Abstract
COVID-19 has been disturbing human society with an intensity never seen since the Influenza epidemic (Spanish flu). COVID-19 and Influenza are both respiratory viruses and, in this study, we explore the relations of COVID-19 and Influenza with atmospheric variables and socio-economic conditions for tropical and subtropical climates in Brazil. Atmospheric variables, mobility, socio-economic conditions and population information were analyzed using a generalized additive model for daily COVID-19 cases from March 1st to May 15th, 2020, and for daily Influenza hospitalizations (2017–2019) in Brazilian states representing tropical and subtropical climates. Our results indicate that temperature combined with humidity are risk factors for COVID-19 and Influenza in both climate regimes, and the minimum temperature was also a risk factor for subtropical climate. Social distancing is a risk factor for COVID-19 in all regions. For Influenza and COVID-19, the highest Relative Risks (RR) generally occurred in 3 days (lag = 3). Altogether among the studied regions, the most important risk factor is the Human Development Index (HDI), with a mean RR of 1.2492 (95% CI: 1.0926–1.6706) for COVID-19, followed by the elderly fraction for both diseases. The risk factor associated with socio-economic inequalities for Influenza is probably smoothed by Influenza vaccination, which is offered free of charge to the entire Brazilian population. Finally, the findings of this study call attention to the influence of socio-economic inequalities on human health.
Keywords: Climate, Respiratory diseases, SARS-CoV-2, Transmission diseases, Virus
1. Introduction
The COVID-19 pandemic has been destructive to human lives, economy and social relations around the world. In just a few months, it quickly spread to all countries and killed more than 900,000 people, consuming tens of millions of jobs (Worldometer website). COVID-19 is caused by SARS-CoV-2, which can be transmitted by two main ways: Contact (surface contact, i.e. fomites and contact with a contaminated person) and by air, via droplets and aerosol (Kutter et al., 2018; Doremalen et al., 2020; Setti et al., 2020; Stadnytskyi et al., 2020; Tellier et al., 2019; World Health Organization, 2020). Influenza, another respiratory virus, has also caused tens of thousands of deaths worldwide each year. The Influenza virus, which can also cause Severe Acute Respiratory Syndrome (SARS), has forms of transmission similar to COVID-19, although there is no consensus on the relevance of each mode (Brankston et al., 2007; Killingley and Nguyen-Van-Tam, 2013; Krammer et al., 2018; Kutter et al., 2018; Lee, 2007; Tellier, 2006). Therefore, the transmission of both is susceptible to climate conditions and, in the case of Influenza, seasonality is already described in the literature (Alonso et al., 2007; Carleton and Meng, 2020; Li et al., 2015; Moriyama et al., 2020; Petrova and Russell, 2018; Russell et al., 2008; Shaman and Kohn, 2009; Shimmei et al., 2020; Sobral et al., 2020).
The world pandemic caused by COVID-19 has demanded a huge effort of the scientific community to identify the relevant factors and their associations with virus transmission. As the virus spreads to new areas, more studies are required to understand the disease under the socio-economic and climate conditions of different countries, especially those in Africa and South America (Belser, 2020; Marson and Ortega, 2020; Wilder-Smith et al., 2020). Besides social distancing, the influence of climate variables on SARS-CoV-2 spread capacity has already been explored by some studies (Ma et al., 2020; Qi et al., 2020; Tobías and Molina, 2020; Wang et al., 2020a; Xie and Zhu, 2020), as well as other factors (Domingo and Rovira, 2020; Sarmadi et al., 2020; Urrutia-Pereira et al., 2020). However, the relations of climate variables were based only on subtropical regions, which makes the pandemic view somewhat early and narrow.
Even for Influenza, only a few studies were conducted in tropical regions and a deep investigation of its relation with environmental variables is still needed (Alonso et al., 2007; Krammer et al., 2018). However, such previous studies can provide important insights on COVID-19. For COVID-19, some studies analyzed the influence of temperature, humidity and rainfall (Auler et al., 2020; Prata et al., 2020; Rodrigues et al., 2020; Tenório; Lansac-tôha, 2020) for some Brazilian cities.
Some factors cannot be ignored to address the spread of respiratory viruses as SARS-CoV-2 and Influenza. For instance, the effects of population age, hygiene measures, social distancing, socio-economic conditions and climate. Therefore, in this study, we investigated the associations of COVID-19 cases and the number of hospital admissions by Influenza with atmospheric variables, social distancing and socio-economic conditions for different climate regions in Brazil. Besides, we compare the results of both diseases, aiming to establish a robust relation between Influenza and COVID-19.
2. Methods
2.1. Data and region
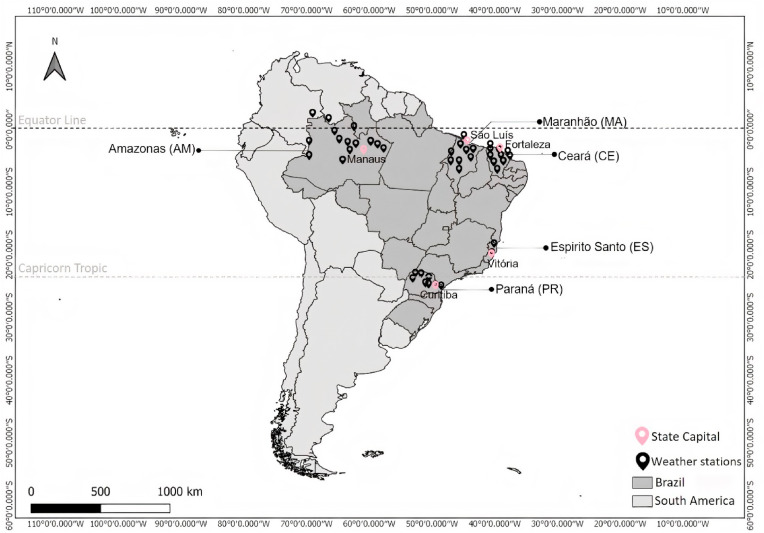
Brazil is the unique huge country that extends from the Equator to the subtropics (5° 16′19'' N and 3° 45′07'' S, with an area of 8,516,000 km2) and thus has different climate zones (Fig. 1 ). The socio-economic conditions also show wide variations inside the country; thus, it is a perfect area to study the influence of these factors on the dissemination of COVID-19 and Influenza, two respiratory viruses with similarities in the modes of transmission. In addition, the inherent bias associated with the data record can be minimized using the information of the same country, mainly for COVID-19, which is a new disease. Another important feature used was to choose regions that do not represent the main gates for people and goods entering the country. The only exception was the state of Amazonas, the home of the Manaus Free Trade Zone. However, we kept the region in the study, since it is a very particular tropical area, where the main city of Manaus is surrounded by the largest tropical forest in the world. The Amazonas state has a low population density (2.23 inhabitants km−2), but 51% of the population is living in the capital Manaus.
Fig. 1.
Geographical position of Brazilian states and meteorological stations.
Five Brazilian states representing different climate regimes were chosen (Fig. 1). The state of Amazonas (AM) has a tropical rainforest climate, with annual average temperature and rainfall of 27.4 °C and 2145 mm, respectively. This type of climate is classified as Af (tropical without a dry season), following the Köppen climate classification (Alvares et al., 2013). Maranhão (MA) and Ceará (CE) have a tropical savanna climate, predominantly Aw (tropical with a dry winter) and As (tropical with a dry summer), respectively. They have a similar annual pattern of rainfall and temperature, with low-temperature variations during the year, but with well-defined seasonality for the monthly rainfalls. For both states, the rainy season occurs between February and May, while the driest period occurs between August and November. Espírito Santo (ES), located in Southeast Brazil, has also a tropical savanna climate (Aw) in most of its area, but with monthly rainfall not changing significantly over the year, as in MA and CE. There is no well-defined dry season and only a slightly rainy period from November to January. The state of Paraná (PR) has well-defined seasons (summer, fall, winter and spring), with humid subtropical (Cfa and Cfb) oceanic climates, without a dry season. Curitiba is the main city of the state, and the average temperature and monthly rainfall are 17.1 °C and 130 mm (climate-data website).
The meteorological data were compiled from the National Institute of Meteorology stations (Instituto Nacional de Meteorologia - INMET, see supplementary material), which consisted of the average daily maximum and minimum temperature (°C), rainfall (mm), relative humidity (%), wind speed (m s−1) and insolation (hours), from January 1st, 2017 to May 15th, 2020 (INMET website). As the wind speed is not available for all stations, it was not included in the final regression analysis. By the way, no statistical significance was found for this variable in our analysis.
The period of investigation is from March 1st to May 15th, 2020, for COVID-19. For Influenza, we analyzed daily data of hospital admissions from 2017 to 2019, in order to have a complete view of the seasonality and to provide insights for COVID-19 that do not yet have a complete annual cycle. Besides, we also performed a regression analysis for Influenza for the same period of the year used for COVID-19 during the years of 2017–2019 to support the comparison of both diseases. Daily data on the number of hospital admissions by Influenza reported in the International Classification of Diseases (ICD) as J09-J11 were compiled on May 05th and 25th, 2020 from the online public Single System of Health Department of Informatics (DATASUS website). Influenza is recorded as follows: code J09 to the avian influenza virus; code J10 to identified influenza virus and their subtypes, and code J11 to influenza cases with no identified virus. The daily COVID-19 cases and deaths were obtained from the Brazilian Ministry of Health for all states (Ministry of Health website). Daily data on 2020 hospitalizations by influenza is not available yet at DATASUS.
Mobility restrictions imposed by COVID-19 were implemented at different levels of intensity and on different dates across Brazil. The poor governance of the pandemic was in part due to the polemic and controversial speeches of the Brazilian president. The president's speech against the WHO recommendations (The Lancet, 2020) forced the Federal Court of Justice to determine (on April 08) that the competence to adopt or to maintain measures during the COVID-19 pandemic should be shared between the three levels of government: federal, state and municipal administrations. However, only the last two moved to do something in their own way, without any coordination or effort from the Ministry of Health. As a measure of the recognized effect of social distancing on COVID-19 dissemination, we used the Community Mobility Reports trends, an indicator provided by Google (Google covid19 website). This mobility reports show the relative percentual changes in the averaged categorized places concerning baseline days (Jan 3rd – Feb 6th, 2020), named as mobility. These data present a good linear correlation with a similar product provided by Apple.
As socio-economic indicators, we used: access to clean water supply, the elderly fraction (≥60 years old), and the Human Development Index (HDI) which, in summary, is a measure of three key dimensions related to development: income, education and health. The number of tests performed was also considered in the regression analysis. The indicators were obtained from the Brazilian Institute of Geography and Statistics and the Ministry of Regional Development (IBGE and SNIS websites). Table 1 shows the values of these variables for each state, besides information concerning the population, Case Fatality Rate (CFR), and the number of Intensive Care Units (ICU) available for the studied states.
Table 1.
Variables used in the regression analysis: Socio-economic indicators (access to clean water supply, elderly fraction and HDI) and COVID-19 tests. Besides, Population; Case Fatality Rate (CFR) and Number of Intensive Care Units (ICU).
| States | HDI | Access to clean Water (%) | Elderly ≥ 60 y (%) | aTests/100,000 inhab. | Population (2019) | CFR (%) | bICU/100,000 inhab. |
|---|---|---|---|---|---|---|---|
| AM | 0.733 | 81.1 | 7.3 | 852 | 4,240,210 | 7.2 | 10.6 |
| CE | 0.735 | 59.0 | 12.0 | 707 | 9,178,363 | 6.6 | 10.9 |
| ES | 0.772 | 81.2 | 14.1 | 625 | 4,138,657 | 4.2 | 19.4 |
| MA | 0.687 | 56.4 | 9.4 | 320 | 7,121,156 | 4.6 | 9.6 |
| PR | 0.792 | 94.4 | 15.1 | 172 | 11,538,518 | 5.6 | 21.2 |
State Health Secretariat reports (Brasil.io website). Note that, in general, the Health Secretariat is testing only when the patients have symptoms.
ICU number from public and private system (Ministry of Health website).
2.2. Statistical analysis
A descriptive analysis of atmospheric variables and health data was performed. A Generalized Additive Model for Location, Scale and Shape (GAMLSS), combined with the negative binomial distribution, a distribution belonging to the exponential family (Hastie and Robert, 1990; Wedderburn, 1974; Stasinopoulos et al., 2018), were used to investigate the potential influence of the atmospheric and socio-economic variables on COVID-19 cases and Influenza hospitalizations, as well to determine the most important variables among those analyzed. The model systematic part is given by:
where, xji are the explanatory variables from j = 1, 2, …,6; and from time (day) from i = 1, …,n: maximum and minimum temperatures, relative humidity, rainfall frequency, insolation and social distancing measured by mobility (only for COVID-19). Rainfall was added to the model as a binary variable (0 without rain, 1 with rain), since the interest was to observe the effect of its occurrence and not of intensity. HDI is the Human Development Index, water corresponds to the percentage of homes with access to clean water supply in the state, elderly is the fraction of the population aged ≥60 years, and test is the number of tests done per 100,000 inhabitants. These variables allowed to observe the scenarios between each studied Brazilian state since the socio-economic and population characteristics are quite variable.
After contamination, there is a latency period of the virus in the organism. The incubation period for viruses is quite variable; in general, the interval between exposure and the onset of symptoms varies from 2 to 7 days (Lauer et al., 2020; Lessler et al., 2009; O'Shea et al., 2019; Wang et al., 2020b). Therefore, for this study, lags from 0 to 7 days were considered. Exposure-response curves were also plotted at lag 3 (3 days of interval between exposure and the onset of symptoms and their notification in this study), using the Distributed Lag Non-linear Model (DLNM), with reference values centered on the median of the variable (Gasparrini, 2011). Finally, the values of Relative Risks (RR), at 95% confidence (CI), were calculated for each variable in the states. Statistical analyses were performed using the software R 3.6.1.
3. Results and discussion
3.1. Statistical analysis - COVID-19
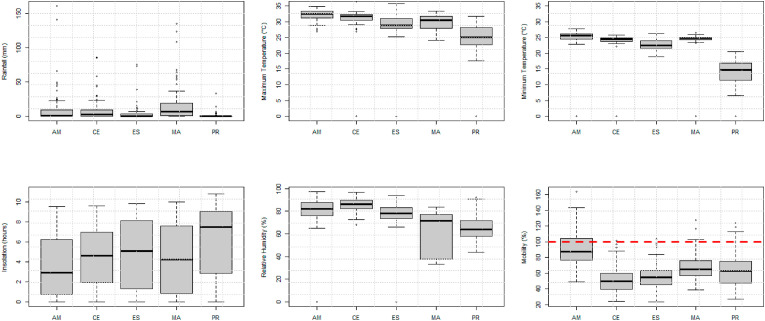
Fig. 2 shows the boxplot of continuous daily explanatory variables for the period of investigation, from March 1st to May 15th, 2020. Although AM recorded the two highest rainfall values, one of which over 150 mm of rainfall, the highest average rainfall was observed in the state of MA. The highest temperatures were recorded in Northern and Northeastern states, which were also those with the highest percentage of relative humidity (mean above 75%). The state of PR, with the lowest temperatures and humidity, presented the most dispersed values for maximum and minimum temperatures. In terms of relative humidity, the greatest dispersion was observed for MA. Insolation was significantly higher for PR, around 8 h, which is almost the double of the average for the other states.
Fig. 2.
Boxplot of atmospheric variables and mobility from March 1st to May 15th, 2020.
The social distancing proposed by the local authorities reduced urban mobility by up to 50%, comparing with the baseline (Jan 3rd – Feb 6th, 2020). The reduction in mobility was not significant, but much worse for AM, where the adhesion to social distancing was lower and mobility was reduced by only 20% in the studied period.
Although the regions are markedly different in their climates, atypical weather conditions were observed in the short period of meteorological data analyzed. Rainfall was above average across much of North and Northeastern Brazil (AM, MA, and CE). For example, Manaus had 446.3 mm and São Luis 657.8 mm in March, which is respectively about 50% and 80% higher than the expected rainfall for the month. On the other hand, the atmospheric conditions were drier and warmer across Southern Brazil. In the largest city of PR (Curitiba), the rainfall and minimum temperature in March were 13.8 mm and 16 °C, respectively, which is significantly different from expected mean values (125 mm and 13.6 °C). These atypical meteorological conditions may have an influence on the spread of COVID-19.
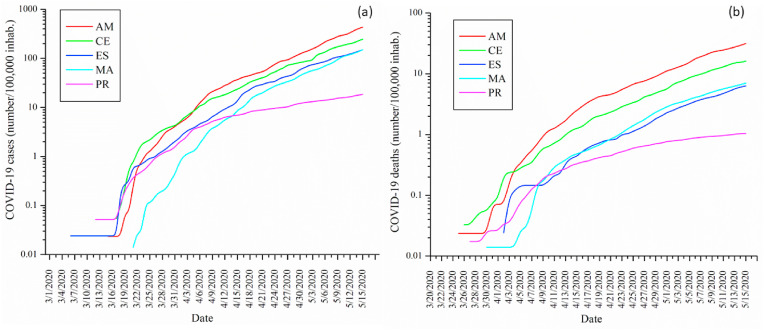
Fig. 3 shows the curve of confirmed COVID-19 cases and deaths in the states. The first cases were registered in ES (March 03rd) and PR (March 12th), and MA was the last state to be reached by the virus on March 21st. A similar behavior was observed among states until around April 05th, with a clear change in the curve of PR from around this date. The curves of deaths also presented the same profile observed for the cases, except for ES at the first 10–12 days of the pandemic, probably due to. The CFR values presented in Table 1 are higher when compared to statistics reported to other countries (Banerjee et al., 2020; Verity et al., 2020). Despite the sub-notification, the number of infected people is lower in PR, which is the most populous of all analyzed states in this study. Also, PR is a neighbor of São Paulo, which is by far the state with the highest number of cases in Brazil (see supplementary material to have a complete view of data – Fig. S1).
Fig. 3.
Prevalence of COVID-19 (number/100,000 inhabitants) cases (a) and deaths (b) for the Brazilian states.
The RR calculated for COVID-19 cases is shown in Table 2 . The variables that present risks to COVID-19 are in bold, as well as the most significant lags for the set of variables. Insolation and the rainfall frequency are not important variables in the set of all variables. The minimum temperature is a risk factor only for PR, which has a subtropical climate. These results suggest that minimum and maximum temperatures in this type of climate are a risk factor for cases of COVID-19. Previous studies conducted in China pointed out that high temperature and humidity reduce the transmission of COVID-19 (i.e., low temperature is a risk factor) (Ma et al., 2020; Wang et al., 2020a,b; Xie and Zhu, 2020).
Table 2.
Relative Risks (RR) and Confidence Interval (CI) at 95% for COVID-19 cases.
| AM RR (CI 95%) |
CE RR (CI 95%) |
ES RR (CI 95%) |
MA RR (CI 95%) |
PR RR (CI 95%) |
|
|---|---|---|---|---|---|
| Rain | 1.1376 (0.9619–1.2080) | 0.9464 (0.9201–1.0688) | 1.0326 (0.9668–1.0632) | 0.9749 (0.9384–1.4619) | 0.9803 (0.9523–1.5782) |
| Tmin | 0.9800 (0.9094–1.0561) | 1.0244 (0.9371–1.1198) | 0.9808 (0.96542–1.0000) | 0.9857 (0.9151–1.0619) | 1.0324 (1.0000–1.0949) |
| Tmax | 1.0918 (0.9121–1.3070) | 1.1091 (1.0423–1.1803) | 1.2192 (1.0973–1.3548) | 1.1684 (1.0795–1.2645) | 1.0155 (1.0120–1.0631) |
| Inso | 0.9564 (0.9723–1.2645) | 0.9380 (0.9806–1.0911) | 0.9849 (0.9771–1.0010) | 0.9975 (0.9471–1.0507) | 1.0742 (0.9868–1.1693) |
| RH | 1.0086 (1.0075–1.0313) | 0.9668 (0.8874–1.0534) | 1.0665 (1.0238–1.1109) | 0.9760 (0.9583–0.9942) | 1.0457 (1.0167–1.0756) |
| Mob. | 1.0221 (1.0013–1.0434) | 1.0445 (1.0168–1.2264) | 1.0320 (1.0111–1.0533) | 1.0095 (1.0085–1.1911) | 1.0357 (1.0141–1.0578) |
| lag1 | 0.9941 (0.9927–0.9956) | 0.9949 (0.9939–0.9959) | 0.9944 (0.9934–0.9953) | 0.9870 (0.9833–0.9908) | 0.9796 (0.9698–0.9895) |
| lag2 | 1.0005 (0.9995–1.0015) | 0.9997 (0.9993–1.0000) | 1.0005 (1.0000–1.0008) | 1.0009 (0.9987–1.0029) | 0.9979 (0.9883–1.0076) |
| lag3 | 1.0015 (1.0007–1.0023) | 1.0010 (1.0005–1.0013) | 1.0007 (1.0005–1.0010) | 1.0036 (1.0013–1.0060) | 1.0067 (0.9951–1.0184) |
| lag4 | 1.0017 (0.9999–1.0034) | 1.0013 (1.0001–1.0026) | 1.0003 (0.9993–1.0013) | 1.0035 (1.0005–1.0066) | 1.0119 (1.0002–1.0238) |
| lag5 | 0.9992 (0.9982–1.0001) | 0.9996 (0.9994–0.9999) | 0.9997 (0.9995–1.0000) | 0.9978 (0.9959–0.9997) | 0.9820 (0.9725–0.9917) |
| lag6 | 1.0018 (1.0007–1.0029) | 1.0013 (1.0009–1.0017) | 1.0012 (1.0009–1.0016) | 1.0008 (0.9993–1.0023) | 1.0162 (1.0047–1.0278) |
| lag7 | 0.9979 (0.9965–0.9993) | 0.9988 (0.9981–0.9996) | 1.0004 (0.9997–1.0012) | 0.9953 (0.9913–0.9993) | 0.9888 (0.9785–0.9992) |
| HDI | 1.2492 (1.0926–1.6706) | ||||
| Elderly | 1.0966 (1.0556–1.0788) | ||||
| Water | 1.0151 (0.9597–1.0738) | ||||
| Tests | 1.0044 (1.0030–1.0057) | ||||
Rain = Rainfall frequency, Tmin = minimum temperature (oC); Tmax = Maximum temperature (oC); Inso. = insolation (h); RH = Relative Humidity (%); Mob = Mobility (%); HDI= Human Development Index; Elderly = fraction of the population aged ≥ 60 years old (%); Water = homes with access to clean water supply (%); Tests = Number of tests performed per 100,000 inhabitants.
Unlike other studies (Mecenas et al., 2020; Sajadi et al., 2020; Wang et al., 2020a,b; Xie and Zhu, 2020), in Brazil, higher temperatures combined with humidity represented more risks for the spread of the virus. For Brazil, Prata et al. (2020) suggested that temperature had a negative linear relationship with the number of confirmed cases, while our results indicate an opposite relation. This means that higher temperatures, as observed in tropical regions, combined with high humidity, can favor the transmission while, in subtropical regions, both minimum and maximum temperatures, together with humidity, are risk factors. Auler et al. (2020) found that higher mean temperatures influenced the COVID-19 transmission rate and intermediate relative humidity favored COVID-19 transmission, a result that is in agreement with this study. However, we analyzed a broader scope of meteorological and socio-economic variables. Other aspects that should be taken into consideration are the methods and the different periods of analysis.
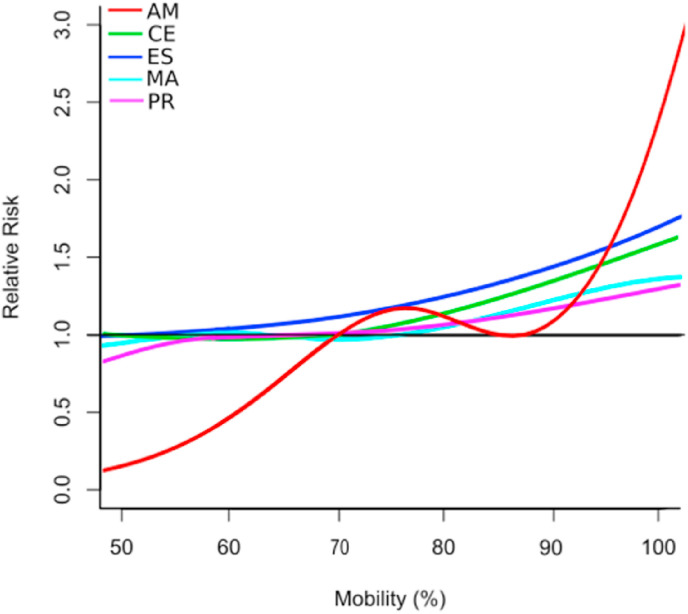
Social distancing, measured by mobility changes in this study, also presented a well-marked RR for all states, which corroborates the influence of social distancing measures as recommended by the WHO and already observed for Brazil (Aquino et al., 2020; Tenório and Lansac-tôha, 2020; Valenti et al., 2020). The comparison of the exposure-response curves of mobility and RR at lag 3 is presented in Fig. 4 . For CE, ES, MA and PR, exposure-response curves of mobility and RR present a similar behavior. Without any reduction in mobility (100% on the mobility axis of Fig. 4), the cases could be increased by 60% (RR 1.5993, 95% CI: 1.2010–2.1551), 73% (RR 1.7301, 95% CI: 1.2459–2.5872), 40% (RR 1.3996, 95% CI: 1.1109–1.6459), and 30% (RR 1.2993, 95% CI: 1.0904–1.6020), respectively, for CE, ES, MA, and PR. For AM, the curve shows an abrupt risk increase after 90% mobility, indicating the expressive importance of this variable in the number of cases in this state, and a potential risk increase of 140% (RR 2.4012, 95% CI: 1.3507–3.4819) without any reduction in mobility. In the supplementary material, we present the curves for each state (Fig. S2) with a CI of 95% that reflects the behavior of population in relation to social distancing in each state.
Fig. 4.
Exposure-response curves of mobility (%) and Relative Risks (RR) for states at lag 3.
In all states analyzed in this study, a one-week interval was observed between exposure and the onset of COVID-19 notifications, but shorter intervals, usually 3 days, were also observed. This time lag estimated here is in the set of variables and it is the interval between the exposure and the notification. The first symptoms after exposure to SARS-CoV-2 normally occur after 2–7 days, but it can extend up to 14 days, which is considered the quarantine time for COVID-19 (Jiang et al., 2020; Lauer et al., 2020).
Socio-economic conditions (HDI) proved to be the most important risk factor among the states. This suggests a difficulty for people to understand the importance of hygiene measures and social distancing on the spread of COVID-19. In addition, the index indirectly measures the difficulty that people have to keep social distancing due to the daily need to search for resources for their livelihood. Therefore, income and education levels are the main relevant factors.
The access to the health care system is another important factor related to socio-economic conditions that can also help explain the high number of deaths in AM, CE, and MA, the states with less ICU available by inhabitant (see Table 1). The fraction of elderly, one additional information captured by the HDI, is also an important risk factor, as already noticed and documented by Health Systems around the world (Banerjee et al., 2020; Wang et al., 2020; Verity et al., 2020). The elderly are the most vulnerable group to COVID-19.
3.2. Statistical analysis – influenza
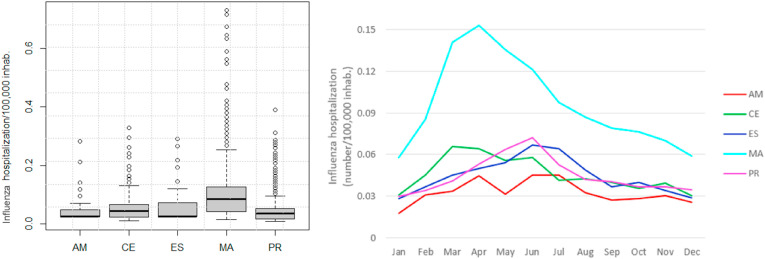
The statistical description of atmospheric variables from 2017 to 2019 is presented in the supplementary material (Fig. S3). The prevalence of Influenza hospitalizations (ICD J09-J11) is presented in Fig. 5 . The state of MA presented the highest prevalence of Influenza. For MA and CE, a peak of prevalence is observed in March/April, which differs from PR and ES, with a peak in May/June, and AM, with a peak not clear. The prevalence of Influenza in Brazil is quite variable, and the fatality rate is 0.4/100,000 inhabitants (for 2019), according to the Brazilian Ministry of Health. This variation is dependent on several factors, including climate conditions, which show wide variations across Brazil. Influenza presents a well-defined seasonality (Fig. 5 and Fig. S4), as observed for other parts of the world. However, it is not possible to attribute the same association to climate, as observed in other parts of the world.
Fig. 5.
State prevalence of daily Influenza (number of hospitalization/100,000 inhabitants) for 2017–2019. In the left panel, box plots comparing prevalence among states. In the right, the average annual profile for each state.
Table 3 presents the Influenza RR and CI for the analyzed variables. As mentioned before, the wind speed was previously analyzed, and the results indicate that this variable is not significant. Maximum temperature and humidity are the main atmospheric risk factors for hospital admissions by influenza in all analyzed climate regimes. Besides, CE and ES also presented significant RR for minimum temperature and insolation (protective effect), while PR for rainfall frequency.
Table 3.
Relative Risks (RR) and Confidence Interval (CI) at 95% for hospital admissions due to Influenza.
| AM RR (CI 95%) |
CE RR (CI 95%) |
ES RR (CI 95%) |
MA RR (CI 95%) |
PR RR (CI 95%) |
|
|---|---|---|---|---|---|
| Rain | 1.2417 (0.9522–1.6192) | 1.1205 (0.9928–1.2646) | 1.0202 (0.9179–1.1338) | 1.0212 (0.9025–1.1554) | 0.9795 (0.9728–0.9887) |
| Tmin | 1.0960 (0.9936–1.2089) | 0.9613 (0.9273–0.9966) | 0.9896 (0.9526–1.0281) | 1.0088 (0.9988–1.0298) | 0.9888 (0.9692–1.0097) |
| Tmax | 1.0771 (1.0154–1.1425) | 1.0646 (1.0258–1.1049) | 1.0461 (1.0112–1.0823) | 1.0090 (1.0078–1.0254) | 1.0204 (1.0028–1.0384) |
| Inso | 1.0257 (0.96264–1.0928) | 0.9630 (0.9375–0.9893) | 0.9696 (0.9502–0.9894) | 1.0043 (0.9841–1.0249) | 0.9974 (0.9518–1.0025) |
| RH | 1.0294 (1.010–1.0492) | 1.0016 (1.0009–1.0115) | 1.0003 (1.0001–1.0022) | 1.0155 (1.0088–1.0222) | 1.0013 (1.0006–1.0021) |
| lag1 | 0.9261 (0.9823–1.0418) | 0.9830 (0.9697–0.9966) | 0.9906 (0.9768–1.0047) | 0.9891 (0.9813–0.9970) | 0.9818 (0.9722–0.9915) |
| lag2 | 0.9838 (0.9739–0.9952) | 0.9703 (0.9568–0.9840) | 0.9748 (0.9609–0.9888) | 0.9792 (0.9717–0.9867) | 1.0136 (1.0035–1.0236) |
| lag3 | 1.1441 (1.0492–1.2476) | 1.0743 (1.0613–1.0875) | 1.0894 (1.0758–1.1032) | 1.0580 (1.0502–1.0659) | 1.0207 (1.0109–1.0306) |
| lag4 | 1.0657 (0.9666–1.1749) | 0.9979 (0.9844–1.0115) | 0.9997 (0.9858–1.0139) | 0.9793 (0.9708–0.9880) | 0.9958 (0.9858–1.0060) |
| lag5 | 0.9791 (0.9688–0.9903) | 0.9648 (0.9517–0.9781) | 0.9607 (0.9472–0.9744) | 0.9731 (0.9655–0.9808) | 0.9824 (0.9727–0.9922) |
| lag6 | 0.9879 (0.9786–0.9893) | 0.9900 (0.9781–1.0021) | 0.9949 (0.9822–1.0078) | 0.9976 (0.9910–1.0042) | 0.9854 (0.9757–0.9951) |
| lag7 | 1.2104 (1.1071–1.3233) | 0.9877 (0.9754–1.0002) | 0.9908 (0.9780–1.0037) | 0.9907 (0.9834–0.9982) | 1.0031 (0.9935–1.0128) |
| HDI | 0.9657 (0.9309–1.0398) | ||||
| Elderly | 1.7152 (1.6742–1.7574) | ||||
| Water | 1.0170 (1.0122–1.0219) | ||||
Rain = Rainfall frequency, Tmin = minimum temperature (oC); Tmax = Maximum temperature (oC); Inso. = insolation (hours); RH = Relative Humidity (%); Mob. = Mobility (%); HDI= Human Development Index; Elderly = fraction of the population aged over 60 years old (%); Water = homes with access to clean water supply (%).
The results do not indicate HDI as an important factor when comparing the states, although clean water supply is a risk factor, indicating that other socio-economic inequalities should be explored, besides those measured by HDI. An important aspect for all Brazilian states is the annual influenza vaccination program of the Brazilian Unified Health System (SUS, http://www.saude.gov.br/sistema-unico-de-saude), that provides free influenza vaccine for vulnerable groups (elderly > 60 years old, pregnant women, children under 5 years old, chronic patients, health workers and indigenous population). Therefore, the vaccine is a protective factor for the population, independently of income, which can explain this result for HDI. On the other hand, age is the most important risk factor for influenza, as demonstrated by an RR of 1.7151 (95% CI: 1.6742–1.7574).
The set of variables presented a pronounced RR at lag 3 for hospitalization due to Influenza, which is in agreement with the latency time for the virus (Lessler et al., 2009; O'Shea et al., 2019).
The regression analysis performed from March 1st to May 15th of years 2017–2019 for Influenza provide similar results of those obtained using the total daily data from 2017 to 2019 (Table 3), with the elderly as the most important factor, with significant RR for temperature and humidity, and no significant RR for HDI (see Table S2). The rainfall and minimum temperature were risk factors in AM, which is consistent with the year station and the annual prevalence of Influenza.
3.3. COVID-19 versus influenza
Comparing socio-economic characteristics, HDI showed statistical significance for COVID-19 and Influenza, and Amazonas was the state with the highest significance for this variable (see the p-value in Table S3). The percentage of elderly people was statistically more significant in MA for COVID-19 while, for influenza, it was PR. In the case of access to clean water supply, the highest statistical significance was observed in the state of CE for both influenza and COVID-19. The two states with the lowest number of tests per 100,000 inhabitants, MA and PR, showed higher significance (α = 0.001).
HDI and the elderly are important factors for COVID-19 cases, while the elderly fraction is remarkably the main factor for Influenza in the set of variables and states. As previously argued, this difference may be due to the Influenza vaccination provided by SUS every year for vulnerable groups. As the vaccine is free and is systematically provided by SUS, the existing inequalities measured by HDI are not highlighted in Influenza, in an opposite way of what happens in the case of COVID-19, for which no vaccine is available yet. However, other inequalities such as access to clean water supply is a risk factor.
Temperature and Humidity are factors significantly associated with both diseases, which suggests that seasonality may be a factor attributable to both viruses. This explains the high number of cases in the tropical climate.
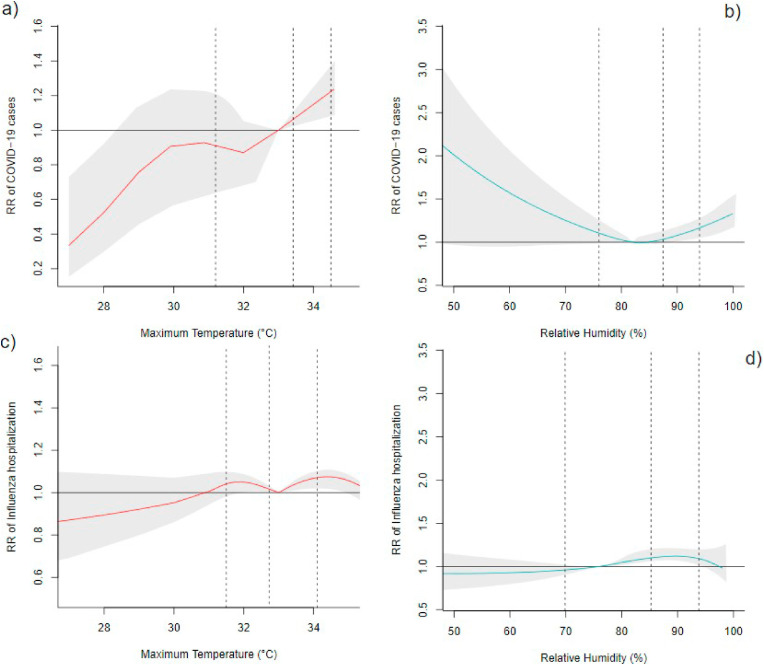
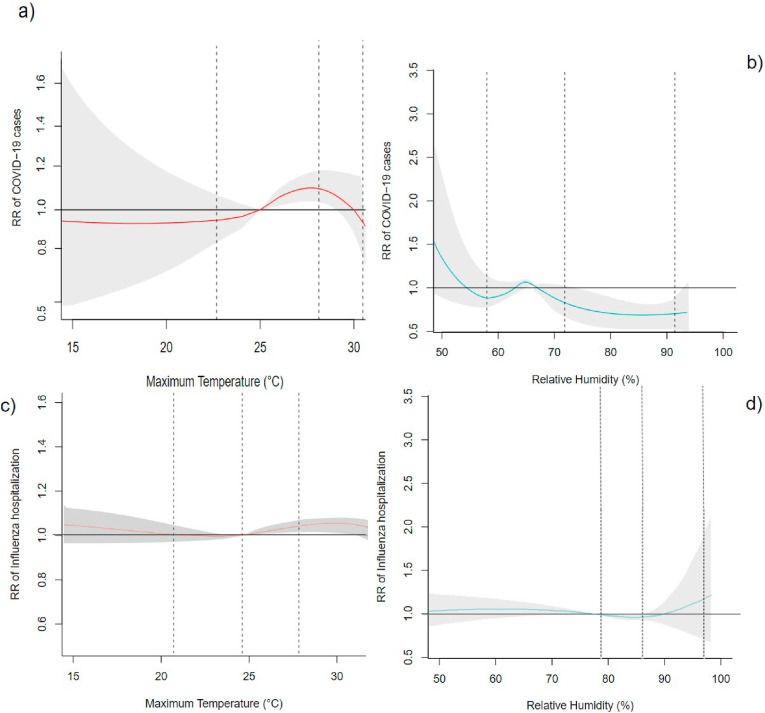
The exposure-response curves for COVID-19 and Influenza at lag 3 for maximum temperature and relative humidity for AM (tropical climate) and PR (subtropical climate) are presented in Fig. 6, Fig. 7 , respectively.
Fig. 6.
Exposure-response curves of maximum temperature (°C) and relative humidity (%) and their RR at lag 3 for AM (tropical climate). a) and b) for COVID-19 cases and c) and d) for Influenza hospitalizations. Vertical lines mean the 25th, 75th, and 99th percentiles.
Fig. 7.
Exposure-response curves of maximum temperature (°C) and relative humidity (%) and their RR at lag 3 for PR (subtropical climate). a) and b) for COVID-19 cases and c) and d) for Influenza hospitalizations. Vertical lines mean the 25th, 75th, and 99th percentiles.
Temperature presents similarities in the risks for COVID-19 (Fig. 6 a and b) and Influenza (Fig. 6 c and d), with a risk factor above percentile 75th for both diseases. Humidity is also observed in having the same way, as can be seen on exposure-response curves for AM (Fig. 6). The same result is observed in the case of PR for both diseases. However, for humidity, these similarities in the curves are not so clear, but the risk is around the mean (Table 2, Table 3) and a protective factor is observed between 25th and 75th percentiles for influenza and 75th and 99th percentiles for COVID-19. Anyway, it is important to note that the COVID-19 period in PR presented atypical meteorological conditions (drier) concerning the climatology of the corresponding period.
From the discussed results, a few similarities can be highlighted between Influenza and COVID-19, considering the results of regression analysis and exposure-response curves performed for Influenza from 2017 to 2019, besides the results for the restricted period (March 1st to May 15th, 2017–2019) presented in Table S2 and Fig. S5 in the supplementary material. Both diseases are caused by viruses with equal modes of transmission and both can cause SARS and present seasonality; temperature and humidity are the main related atmospheric variables. Therefore, we believe that COVID-19 also has a similar annual cycle like Influenza, with tropical regions presenting a different cycle than subtropical regions, since the variability of temperature and humidity is significantly different between these regions.
4. Conclusions
In this study, we evaluated the influence of atmospheric and socio-economic conditions on the spread of COVID-19 and Influenza in tropical and subtropical states in Brazil. COVID-19 presented a different epidemiological profile in tropical and subtropical Brazilian climates. Seasonality showed similarities with the behavior of Influenza in previous years. Despite the relevance of social distancing, indicated in this study by mobility, the climate had an important influence on both COVID-19 and Influenza suggesting that, for the tropical region (AM, MA, and CE), COVID-19 arrived in a favorable time. This favorable climate condition, identified by an abnormal rainy season that influenced humidity, was observed mainly in AM and MA and may have contributed to a large number of cases. On the other hand, COVID-19 arrived in unfavorable periods and atypical meteorological conditions for PR state, i.e. under much drier and sunnier conditions than normal, with several hours of solar radiation that contributed to the control of COVID-19 spread in the state.
Age is the most important risk factor for influenza, while for COVID-19 the HDI is the most important factor to explain the differences among regions in the number of COVID-19 cases followed by age and social distancing.
Finally, the dataset has limitations associated with sub notifications of cases and deaths by COVID-19. Similar limitations can be extended to the social distancing measure, analyzed through the mobility changes since it cannot represent with accuracy how far people are staying away from each other. Besides, hospital admission for influenza obtained from SUS cannot represent the total population, as well as the data available for COVID-19 that is yet limited to a few months, which can influence the results. However, we believe that these results can be extended to other similar regions and call attention to the influence of socioeconomic inequalities on the spread of the pandemic.
Credit author statement
Leila D. Martins: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Iara da Silva: Data curation, Formal analysis, Methodology, Visualization, Wellington V. Batista: Data curation, Maria F. Andrade: Methodology, Writing - review & editing, Edmilson D. Freitas: Writing - review & editing, and Jorge A. Martins: Conceptualization, Methodology; Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to acknowledge the organizations and Institutes for providing the dataset. We would also like to thank the Brazilian National Council for Scientific and Technological Development (Conselho Nacional de Desenvolvimento Científico e Tecnológico - CNPq), process grant No. 306862/2018-2.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.110184.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- Alonso W.J., Viboud C., Simonsen L., Hirano E.W., Daufenbach L.Z., Miller M.A. Seasonality of influenza in Brazil: a traveling wave from the amazon to the subtropics. Am. J. Epidemiol. 2007;165:1434–1442. doi: 10.1093/aje/kwm012. [DOI] [PubMed] [Google Scholar]
- Alvares C.A., Stape J.L., Sentelhas P.C., De Moraes Gonçalves J.L., Sparovek G. Köppen’s climate classification map for Brazil. Meteorol. Z. 2013;22:711–728. doi: 10.1127/0941-2948/2013/0507. [DOI] [Google Scholar]
- Aquino E.M.L., Silveira I.H., Pescarini J.M., Aquino R., Souza-Filho J.A. Social distancing measures to control the COVID-19 pandemic : potential impacts and challenges in Brazil 2423–2446. Ciência e Saúde Coletiva. 2020;25:2423–2446. doi: 10.1590/1413-81232020256.1.10502020. [DOI] [PubMed] [Google Scholar]
- Auler A.C., Cássaro F.A.M., da Silva V.O., Pires L.F. Evidence that high temperatures and intermediate relative humidity might favor the spread of COVID-19 in tropical climate: a case study for the most affected Brazilian cities. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.139090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee A., Pasea L., Harris S., Gonzalez-Izquierdo A., Torralbo A., Shallcross L., Noursadeghi M., Pillay D., Sebire N., Holmes C., Pagel C., Wong W.K., Langenberg C., Williams B., Denaxas S., Hemingway H. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020;395:1715–1725. doi: 10.1016/s0140-6736(20)30854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belser J.A. Assessment of SARS-CoV-2 replication in the context of other respiratory viruses. Lancet. Respir. Med. 2020;2600:7–8. doi: 10.1016/S2213-2600(20)30227-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brankston G., Gitterman L., Hirji Z., Lemieux C., Gardam M. Transmission of influenza A in human beings. Lancet Infect. Dis. 2007;7:257–265. doi: 10.1016/S1473-3099(07)70029-4. [DOI] [PubMed] [Google Scholar]
- Brasil io. https://brasil.io/dataset/covid19/caso/ Available at: the website.
- Carleton T., Meng K.C. medRxiv; 2020. Causal Empirical Estimates Suggest COVID-19 Transmission Rates Are Highly Seasonal. 2020.03.26.20044420. [DOI] [Google Scholar]
- Climate-data https://pt.climate-data.org/america-do-sul/brasil Available at: the website webpage.
- DATASUS Department of Informatics of Single system of health. http://www2.datasus.gov.br/DATASUS/ Available at: the website, Accessed on May 05 and 25, 2020.
- Domingo J.L., Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ. Res. 2020;187:109650. doi: 10.1016/j.envres.2020.109650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doremalen N. van, Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., Wit E., Munster V.J. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020;382(16) doi: 10.1056/NEJMc2004973. 0-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A. Distributed lag linear and non-linear models in R: the package dlnm. J. Stat. Software. 2011;43:1–20. doi: 10.18637/jss.v043.i08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Google covid19 COVID-19 community mobility reports. https://www.google.com/covid19/mobility/ Available at: the website webpage.
- Hastie T., Robert T. Generalized additive models 1 Introduction 2 Smoothing methods and generalized addi- tive models. Prev. Med. (Baltim). 1990;43 [Google Scholar]
- IBGE Instituto Brasileiro de Geografia e Estatística. https://www.ibge.gov.br/cidades-e-estados/sp/panorama.html Available at: the website.
- INMET Instituto Nacional de Meteorologia, Banco de Dados Meteorológicos para Ensino e Pesquisa. http://www.inmet.gov.br/portal/index.php?r=bdmep/bdmep Available at: the website.
- Jiang X., Rayner S., Luo M.H. Does SARS-CoV-2 has a longer incubation period than SARS and MERS? J. Med. Virol. 2020;92:476–478. doi: 10.1002/jmv.25708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killingley B., Nguyen-Van-Tam J. Routes of influenza transmission. Influenza other respi. Viruses. 2013;7:42–51. doi: 10.1111/irv.12080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krammer F., Smith G.J.D., Fouchier R.A.M., Peiris M., Kedzierska K., Doherty P.C., Palese P., Shaw M.L., Treanor J., Webster R.G., García-Sastre A. Influenza. Nat. Rev. Dis. Prim. 2018;4:1–21. doi: 10.1038/s41572-018-0002-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutter J.S., Spronken M.I., Fraaij P.L., Fouchier R.A., Herfst S. Transmission routes of respiratory viruses among humans. Curr. Opin. Virol. 2018;28:142–151. doi: 10.1016/j.coviro.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R., Azman A.S., Reich N.G., Lessler J. The incubation period of coronavirus disease 2019 (CoVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee R.V. Transmission of influenza A in human beings. Lancet Infect. Dis. 2007;7:760–761. doi: 10.1016/S1473-3099(07)70270-0. [DOI] [PubMed] [Google Scholar]
- Lessler J., Reich N.G., Brookmeyer R., Perl T.M., Nelson K.E., Cummings D.A. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect. Dis. 2009;9:291–300. doi: 10.1016/S1473-3099(09)70069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Rao Y., Sun Q., Wu X., Jin J., Bi Y., Chen J., Lei F., Liu Q., Duan Z., Ma J., Gao G.F., Liu D., Liu W. Identification of climate factors related to human infection with avian influenza A H7N9 and H5N1 viruses in China. Sci. Rep. 2015;5:1–9. doi: 10.1038/srep18094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S., Yan J., Niu J., Zhou J., Luo B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marson F.A.L., Ortega M.M. Covid-19 in Brazil. Pulmonology. 2020;26(4):241–256. doi: 10.1016/j.pulmoe.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mecenas P., Bastos R., Vallinoto A., Normando D. medRxiv; 2020. Effects of Temperature and Humidity on the Spread of COVID-19: A Systematic Review. 2020.04.14.20064923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health Ministério da Saúde. https://covid.saude.gov.br/https://covid-insumos.saude.gov.br/paineis/insumos/painel_leitos.php Available at: the website, Accessed on May 05 and 25, 2020.
- Moriyama M., Hugentobler W.J., Iwasaki A. Seasonality of respiratory viral infections. Annu. Rev. Virol. 2020;7:1–19. doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- O'Shea H., Blacklaws B.A., Collins P.J., McKillen J., Fitzgerald R. Elsevier Ltd; 2019. Viruses Associated with Foodborne Infections, Reference Module in Life Sciences. [DOI] [Google Scholar]
- Petrova V.N., Russell C.A. The evolution of seasonal influenza viruses. Nat. Rev. Microbiol. 2018;16:47–60. doi: 10.1038/nrmicro.2017.118. [DOI] [PubMed] [Google Scholar]
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci. Total Environ. 2020;729:138862. doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., Xiao S., Shi R., Ward M.P., Chen Y., Tu W., Su Q., Wang W., Wang X., Zhang Z. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728:138778. doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues W., Prata D.N., Camargo W. medRxiv; 2020. Regional Determinants of the Expansion of Covid-19 in Brazil. 2020.04.13.20063925. [DOI] [Google Scholar]
- Russell C.A., Jones T.C., Barr I.G., Cox N.J., Garten R.J., Gregory V., Gust I.D., Hampson A.W., Hay A.J., Hurt A.C., De Jong J.C., Kelso A., Klimov A.I., Kageyama T., Komadina N., Lapedes A.S., Lin Y.P., Mosterin A., Obuchi M., Odagiri T., Osterhaus A.D.M.E., Rimmelzwaan G.F., Shaw M.W., Skepner E., Stohr K., Tashiro M., Fouchier R.A.M., Smith D.J. The global circulation of seasonal influenza A (H3N2) viruses. Science. 2008;320:340–346. doi: 10.1126/science.1154137. [DOI] [PubMed] [Google Scholar]
- Sajadi M.M., Habibzadeh P., Vintzileos A., Shokouhi S., Miralles-Wilhelm F., Amoroso A. Temperature and latitude analysis to predict potential spread and seasonality for COVID-19. SSRN Electron. J. 2020;6–7 doi: 10.2139/ssrn.3550308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarmadi M., Marufi N., Kazemi Moghaddam V. Association of COVID-19 global distribution and environmental and demographic factors: an updated three-month study. Environ. Res. 2020;188 doi: 10.1016/j.envres.2020.109748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Borelli M., Palmisani J., Di Gilio A., Torboli V., Fontana F., Clemente L., Pallavicini A., Ruscio M., Piscitelli P., Miani A. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: first evidence. Environ. Res. 2020;188:109754. doi: 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaman J., Kohn M. Absolute humidity modulates influenza survival, transmission, and seasonality. Proc. Natl. Acad. Sci. U.S.A. 2009;106:3243–3248. doi: 10.1073/pnas.0806852106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimmei K., Nakamura T., Ng C.F.S., Hashizume M., Murakami Y., Maruyama A., Misaki T., Okabe N., Nishiwaki Y. Association between seasonal influenza and absolute humidity: time-series analysis with daily surveillance data in Japan. Sci. Rep. 2020;10:7764. doi: 10.1038/s41598-020-63712-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SNIS Sistema Nacional de Informações sobre Saneamento, Ministério do Desenvolvimento Regional. http://snis.gov.br/diagnostico-anual-agua-e-esgotos Available at: the website.
- Sobral M.F.F., Duarte G.B., da Penha Sobral A.I.G., Marinho M.L.M., de Souza Melo A. Association between climate variables and global transmission oF SARS-CoV-2. Sci. Total Environ. 2020;729:3–6. doi: 10.1016/j.scitotenv.2020.138997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadnytskyi V., Bax C.E., Bax A., Anfinrud P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc. Natl. Acad. Sci. Unit. States Am. 2020;202006874 doi: 10.1073/pnas.2006874117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stasinopoulos M.D., Rigby R.A., Bastiani F. De. vol. 18. 2018. pp. 1–26. (GAMLSS : A Distributional Regression Approach). [DOI] [Google Scholar]
- Tellier R. Review of aerosol transmission of influenza A virus. Emerg. Infect. Dis. 2006;12:1657–1662. doi: 10.3201/eid1211.060426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellier R., Li Y., Cowling B.J., Tang J.W. Recognition of aerosol transmission of infectious agents: a commentary. BMC Infect. Dis. 2019;19:1–9. doi: 10.1186/s12879-019-3707-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenório M., Lansac-tôha F.M. 2020. Social Distancing and Movement Constraint as the Most Likely Factors for COVID-19 Outbreak Control in Brazil Social Distancing and Movement Constraint as the Most Likely Factors for COVID-19 Outbreak Control in Brazil. [Google Scholar]
- The Lancet COVID-19 in Brazil: “so what? Lancet. 2020;395:1461. doi: 10.1016/S0140-6736(20)31095-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobías A., Molina T. Is temperature reducing the transmission of COVID-19 ? Environ. Res. 2020;186:109553. doi: 10.1016/j.envres.2020.109553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urrutia-Pereira M., Mello-da-Silva C.A., Solé D. COVID-19 and air pollution: a dangerous association? Allergol. Immunopathol. 2020;10–13 doi: 10.1016/j.aller.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenti V.E., Menezes P.D.L., Carolina A., Abreu G. De, Vieira N.A., Garner D.M. Social distancing measures could have reduced estimated deaths related to COVID-19 in Brazil. 2020;30:164–169. [Google Scholar]
- Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N., Cuomo-Dannenburg G., Thompson H., Walker P.G.T., Fu H., Dighe A., Griffin J.T., Baguelin M., Bhatia S., Boonyasiri A., Cori A., Cucunubá Z., FitzJohn R., Gaythorpe K., Green W., Hamlet A., Hinsley W., Laydon D., Nedjati-Gilani G., Riley S., van Elsland S., Volz E., Wang H., Wang Y., Xi X., Donnelly C.A., Ghani A.C., Ferguson N.M. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect. Dis. 2020;3099:1–9. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Tang K., Feng K., Lv W. High temperature and high humidity reduce the transmission of COVID-19. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3551767. [DOI] [Google Scholar]
- Wang W., Tang J., Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J. Med. Virol. 2020;92:441–447. doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Li-sheng, Yi-ru Wang, Ye Da-wei, Li Qing-quan. Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence. Int. J. Antimicrob. Agent. 2020;55:105948. doi: 10.1016/j.ijantimicag.2020.105948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wedderburn R.W.M. Quasi-likelihood functions , generalized linear models , and the Gauss — Newton method. Biometrika. 1974;61:439–447. [Google Scholar]
- Wilder-Smith A., Chiew C.J., Lee V.J. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect. Dis. 2020;20:e102–e107. doi: 10.1016/S1473-3099(20)30129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization W. Modes of transmission of virus causing COVID-19 : implications for IPC precaution recommendations. Sci. Br. 2020:1–3. doi: 10.1056/NEJMoa2001316.5. [DOI] [Google Scholar]
- Worldometer https://www.worldometers.info/coronavirus/ Available at: the website webpage.
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.