AJO Episcleritis Scleritis Epidemiology Abstract
Purpose:
To determine the population-based incidence and disease associations of episcleritis and scleritis in a Midwestern US population.
Design:
Population-based retrospective cohort study.
Methods:
All residents of Olmsted County, MN from 2006–2015 were identified using the Rochester Epidemiology Project. 223 episcleritis cases and 77 scleritis cases were identified. We assessed incidence and disease associations of episcleritis and scleritis, as well as scleritis recurrence rates, treatment, and complications.
Results:
The incidence rates for episcleritis and scleritis were 15.39 and 5.54 per 100,000 per year, respectively. Females accounted for 60.1% of episcleritis and 51.9% of scleritis cases. The mean age at diagnosis was 40.2 years for episcleritis and 48.8 years for scleritis. In the episcleritis cases, the incidence in females was higher (p=0.01). There was no significant difference between genders for scleritis incidence (p=0.75). 23.4% of scleritis patients had an associated systemic disease. Patients with systemic disease had a trend towards an increased risk of recurrence, but it was not statistically significant. There was a slightly decreased risk of scleritis recurrence with older age at diagnosis (HR 0.73, p=0.058, 95% CI 0.52 – 1.01). At last follow up, most eyes with scleritis (90.4%) had good visual acuity (better than 20/40), and 92.3% had stable or improved visual acuity.
Conclusion:
The Olmsted County, MN population had a lower incidence of episcleritis and a higher incidence of scleritis compared to previous studies. The population-based results from this study may provide information that is more applicable to a primary eye care setting.
This population-based study reports a lower incidence of episcleritis and higher incidence of scleritis compared to prior studies. Less than 25% of the scleritis patients had an associated systemic disease, and females were not more likely to have scleritis. In comparison to tertiary care center cohorts, the scleritis cases were less severe in terms of treatment required, complications, and recurrences. These findings may provide valuable information that is applicable to a primary eye care setting.
Introduction
Episcleritis and scleritis are ocular inflammatory diseases that differ in terms of associated systemic disease, treatment, and visual outcome. Episcleritis classically presents with eye redness, irritation or mild pain. Most cases are mild, respond to topical anti-inflammatory agents, and do not pose a threat to vision. Scleritis is a painful, potentially vision-threatening inflammation of the sclera that usually requires treatment with nonsteroidal anti-inflammatory drugs (NSAIDs), systemic corticosteroids, and/or systemic immunomodulatory medication. Associated complications can include corneal thinning, glaucoma, cataract, and secondary posterior segment inflammation. Approximately 40–50% of scleritis cases have been reported to have systemic inflammatory causes that are more likely to require systemic immunomodulatory treatment.1
There are few published population-based studies of episcleritis and scleritis. Since cases of episcleritis or scleritis that respond to initial treatment and do not recur are unlikely to be referred to a tertiary care center, a population-based study can provide a more accurate assessment of incidence, disease association and prognosis. This study utilizes the Rochester Epidemiology Project (REP), a medical records linkage system established in 1966 that tracks medical care delivered to residents of Olmsted County, MN using diagnostic and surgical procedure codes.2 The REP captures virtually all of the medical care provided to residents of Olmsted County since the region is relatively isolated from other urban centers and collaborative agreements between local health care providers allowed the creation of a medical records linkage system that covers the entire county population.3 We utilized the REP to conduct a population-based study of the incidences of episcleritis and scleritis in Olmsted County, MN from 2006 to 2015, as well as to assess clinical characteristics, treatment, and complications of scleritis.
Methods
Study Design, Data Source, and Study Population
The Institutional Review Boards of Mayo Clinic and Olmsted Medical Center approved this retrospective cohort study, and the research adhered to the tenets of the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. Participants in the REP database were asked to give authorization for minimal risk research when they are first entered into the medical system in Olmsted County. Since the current study is retrospective and considered minimal risk, the IRBs do not require additional informed consent from the patients included in this study, (waiver of consent was granted by the IRBs.) International Classification of Diseases, 9th and 10th Edition (ICD-9 and −10) codes for ocular inflammation were used to query the REP database to identify all residents of Olmsted County diagnosed with ocular inflammatory disease from January 1, 2006 to December 31, 2015. (Supplemental Tables 1 & 2) Research authorizations were confirmed through the database, and patients who did not grant authorization were excluded from the study. The medical records for all potential cases of episcleritis and scleritis were reviewed to verify the diagnoses on the basis of documented ophthalmic examinations. Demographic data, including age, sex, and self-reported race, was collected and compared to the mid-study Olmsted County population (2010) using the Fisher exact test.
Standard clinical definitions of episcleritis and scleritis were used to confirm the diagnoses. Episcleritis cases had clinical findings of episcleral injection (diffuse, sectoral, or nodular) that blanched with phenylephrine eye drops. Characteristics consistent with scleritis included scleral injection that did not blanche with phenylephrine eye drops, conjunctival chemosis, moderate to severe eye pain, and the absence of significant intraocular inflammation. Cases were excluded if the scleral or episcleral inflammation was surgically-induced, traumatic, or contact lens-related. The majority of patients were diagnosed and treated by ophthalmologists or optometrists who were not specialists in uveitis or anterior segment inflammation.
Medical records were reviewed for evidence of systemic inflammatory or infectious causes of episcleritis and scleritis. Diagnoses of autoimmune thyroid disease, (hypothyroidism, Graves disease, Hashimoto thyroiditis), were also noted. Follow-up visits were reviewed through February 2019 to assess scleritis recurrence, defined as a new episode of scleritis occurring either on or off treatment at least three months after the previously documented activity. In some cases, the patient was not seen when scleritis was quiescent, but the duration between visits with inflammation was greater than three months, and the patient reported a period of inactivity between recurrences.
Medications used to treat scleritis were documented as well as complications attributable to inflammation and/or treatment. Complications included decreased visual acuity (VA), the need for cataract surgery, ocular hypertension (intraocular pressure greater than 24), anterior uveitis, corneal involvement, macular edema, optic disc edema, vitritis, and exudative retinal detachment. Visual acuity (VA) in affected eyes at presentation with scleritis, worst VA, and VA at the last follow up visit was also collected. Decreased VA was defined as a loss of two or more Snellen lines at the last visit.
Statistical Analysis
The overall incidence of episcleritis and scleritis was estimated using the age- and sex-specific population figures for Olmsted County census data from 2006 through 2015. Age was stratified into the following groups by years: 0–14, 15–24, 25–44, 45–64, and 65–110. Population estimates for individual years between census years were determined using linear interpolation. Because approximately 85% of the Olmsted County population is White, incidence rates were also age- and/or gender-adjusted to the 2010 census figures for the U.S. White population so that the data could be compared to national estimates. The 95% confidence intervals (CIs) for the rates were calculated assuming a Poisson error distribution. Trend over age at diagnosis and between genders were investigated using Poisson regression models. The overall risk of recurrence was estimated using the Kaplan-Meier method. To evaluate risk factors for recurrence, a Cox proportional hazards model was completed. Given that we have two eyes in the population from some individuals, a sandwich estimate of the standard error was used in the testing to account for the potential correlation between eyes from the same individual. Overall comparisons between groups were completed with Chi-square tests for categorical variables. Continuous variables were completed using two-sample t-tests.
Results
The Olmsted County mid-study population was 144,248 in 2010 (Figure 1). Initial ICD-9/10 code search revealed 4,253 patients with ocular inflammation diagnoses as well as 233 episcleritis cases and 79 scleritis cases. After chart review, 10 cases of episcleritis and 2 of scleritis were excluded because they lacked research authorization and Olmsted County residency at time of diagnosis. Other reasons for exclusion included a primary diagnosis of uveitis, contact lens-related keratitis and conjunctivitis, and traumatic or post-surgical inflammation. In total, there were 223 confirmed episcleritis cases and 77 confirmed scleritis cases included in this study.
Figure 1:
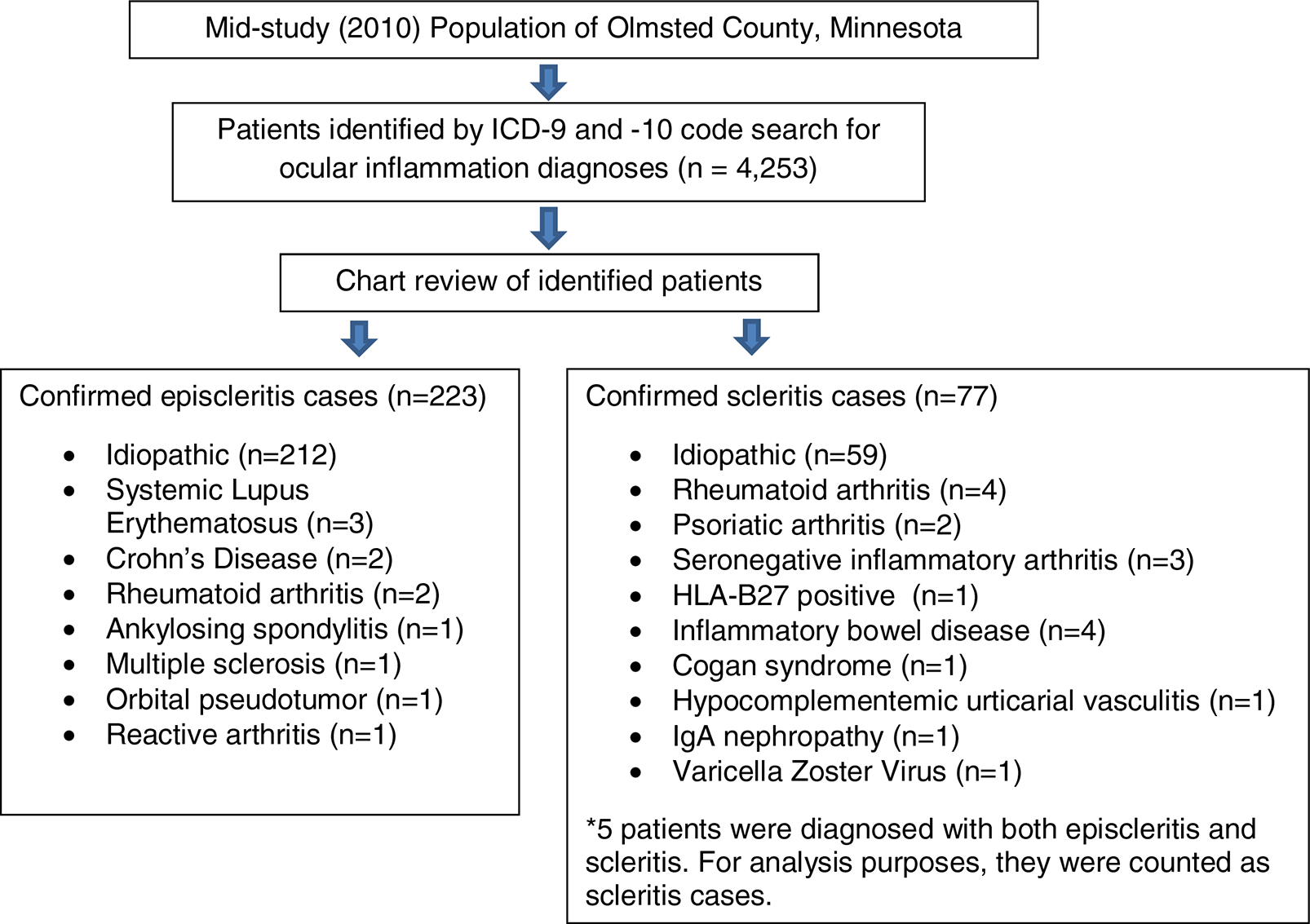
Identification of Episcleritis and Scleritis cases in the Olmsted County population
Female subjects accounted for 60.1% of episcleritis and 51.9% of scleritis cases (Table 1). The mean age at diagnosis was 40.2 years for episcleritis and 48.8 years for scleritis. The majority of episcleritis and scleritis patients were White, 86.5% and 87.0%, respectively, mirroring the composition of Olmsted County (83.4% White in 2010). Compared to the general Olmsted County population, females (p=0.009, 95% CI: 53.3, 66.6) and ages 25–44 years (p<0.001, 95% CI: 36.9, 50.3) were overrepresented in the episcleritis group. Black patients were underrepresented among episcleritis cases (p=0.04). In scleritis cases, patients aged 45–64 years (p=0.02, 95% CI: 28.1, 50.8) were more likely to be affected, but not females (p=0.75, 95% CI: 40.3, 63.5).
Table 1:
Demographics of Episcleritis and Scleritis Cases
| Mid-study (2010) Olmsted County Population | Confirmed Episcleritis Cases | P value | Confirmed Scleritis Cases | P value | Scleritis Cases who are Smokers | |
|---|---|---|---|---|---|---|
| Total | 144,248 | 223 | 77 | 29 (37.7%) (26.9,49.4) | ||
| Mean age | 36.1 | 40.2 | 48.8 | 50.2 | ||
| Female (%) (95% CI) | 73,763 (51.1%) (50.9,51.4) | 134 (60.1%) (53.3,66.6) | 0.009 | 40 (51.9%) (40.3,63.5) | 0.91 | 16 (55.2%) (35.7,73.6) |
| Age category | ||||||
| 0–14 | 30,682 (21.3%) (21.1,21.5) | 19 (8.5%) (5.2,13.0) | <0. 001 | 2 (2.6%) (0.3,9.1) | <0.001 | 0 (0%) (0,11.9) |
| 15–24 | 17,065 (11.8%) (11.7,12.0) | 27 (12.1%) (8.1,17.1) | 0.92 | 3 (3.9%) (0.8,11.0) | 0.03 | 0 (0%) (0,11.9) |
| 25–44 | 40,200 (27.8%) (27.6,28.1) | 97 (43.5%) (36.9,50.3) | <0.001 | 28 (36.4%) (25.7,48.1) | 0.10 | 11 (38.0%) (20.7,57.7) |
| 45–64 | 38,168 (26.5%) (26.2,26.7) | 59 (26.5%) (20.8,32.8) | 1 | 30 (39.0%) (28.1,50.8) | 0.02 | 13 (44.8%) (26.5,64.3) |
| ≥65 | 18,133 (12.5%) (12.4,12.7) | 21 (9.4%) (5.9,14.0) | 0.19 | 14 (18.2%) (10.3,28.6) | 0.17 | 5 (17.2%) (5.9,35.8) |
| Race | ||||||
| Asian | 7,771 (5.4%) (5.3,5.5) | 10 (4.5%) (2.2.8.1) | 0.66 | 4 (5.2%) (1.4,12.8) | 1 | 1 (3.4%) (0.1,17.8) |
| Black | 6,751 (4.7%) (4.6,4.8) | 4 (1.8%) (0.5,4.5) | 0.038 | 3 (3.9%) (0.8,11.0) | 1 | 2 (6.9%) (0.9,22.8) |
| Hispanic | 6,081 (4.2%) (4.1,4.3) | 9 (4.0%) (1.9,7.5) | 1 | 2 (2.6%) (0.3,9.1) | 0.77 | 1 (3.4%) (0.1,17.8) |
| White | 120,348 (83.4%) (83.2,83.6) | 193 (86.5%) (81.4,90.7) | 0.24 | 67 (87.0%) (77.4,93,6) | 0.54 | 24 (82.8%) (64.2,94.2) |
| Other | 3,297 (2.3%) (2.2,2.4) | 7 (3.1%) (1.3,6.4) | 0.36 | 1 (1.3%) (0,7.0) | 1 | 1 (3.4%) (0.1,17.8) |
P values calculated using Fisher exact test comparing cases to Olmsted County population
The overall age- and sex-adjusted incidence of episcleritis was 15.39 (95% CI: 13.36–17.43) per 100,000 per year adjusted for 2010 US white population (Table 2a). Age-adjusted incidence among males with episcleritis was 12.48 (95% CI 9.85–15.10). Age-adjusted incidence among females with episcleritis was 18.21 (95% CI 15.11–21.30). The highest incidence rate (23.78) occurred in patients aged 25–44 years, and the lowest (6.16) was in patients 14 years and younger. In the 25–44 year age group, the incidence rates for females and males were 29.24 and 18.25, respectively. The differences between age groups was statistically significant (p<0.001). The numbers were too low to assess for trends in incidence rates based on ethnicity/race.
Table 2a:
Episcleritis Incidence in Olmsted County, MN by Age and Sex
| N | Rate | 95% CI | N | Rate | 95% CI | |
|---|---|---|---|---|---|---|
| Total | 134 | 18.15 | 15.26–21.56 | 89 | 12.60 | 10.12–15.50 |
| 0–14 | 7 | 4.63 | 1.86–9.54 | 12 | 7.62 | 3.94–13.34 |
| 15–24 | 16 | 18.37 | 10.51–29.76 | 11 | 12.88 | 6.43–23.06 |
| 25–44 | 60 | 29.24 | 22.31–35.72 | 37 | 18.25 | 12.85–25.19 |
| 45–64 | 37 | 19.11 | 13.45–26.37 | 22 | 12.05 | 7.56–18.20 |
| 65+ | 14 | 13.80 | 7.53–23.18 | 7 | 8.98 | 3.60–18.50 |
Incidence rates per 100,000 per year
Overall age and sex adjusted incidence of episcleritis = 15.39 per 100,000 per year (95% CI: 13.36–17.43) adjusted for 2010 US white population.
Males: age adjusted incidence is 12.48 per 100,000 per year (95% CI 9.85–15.10).
Females: age adjusted incidence is 18.21 per 100,000 per year (95% CI 15.11–21.30). Significant difference between genders (p=0.01)
Significant difference across ages (p<0.001).
For scleritis, the overall age- and sex-adjusted incidence was 5.54 (95% CI 4.29–6.79) per 100,000 per year (Table 2b). Age-adjusted incidence was 5.58 (95% CI 3.83–7.29) among males and 5.56 (95% CI 3.83–7.29) among females; this difference was not statistically significant (p=0.75). The overall age- and sex-adjusted scleritis incidence in the total population is slightly lower than the incidence in males and females assessed separately. This result is a function of adjusting the overall incidence to the U.S. white population. The crude overall scleritis incidence does fall between the incidences in males and females. The highest incidence rates occurred in patients 45–64 years (7.98) and 65 years or older (7.80). Children 14 years and younger had the lowest incidence (0.65). There was a statistically different difference in incidence among the age groups, (p<0.001). The numbers were too low to assess for trends in incidence rates based on ethnicity/race.
Table 2b:
Scleritis Incidence in Olmsted County, MN by Age and Sex
| Age | N | Rate | 95% CI | N | Rate | 95% CI |
|---|---|---|---|---|---|---|
| Total | 40 | 5.42 | 3.86–7.36 | 37 | 5.24 | 3,69–7.23 |
| 0–14 | 1 | 0.66 | 0.02–3.68 | 1 | 0.63 | 0.02–3.51 |
| 15–24 | 3 | 3.44 | 0.71–10.04 | 0 | 0 | |
| 25–44 | 14 | 6.82 | 3.72–11.46 | 14 | 6.90 | 3.77–11.59 |
| 45–64 | 15 | 7.75 | 4.34–12.79 | 15 | 8.21 | 4.60–13.55 |
| 65+ | 7 | 6.90 | 2.77–14.21 | 7 | 8.98 | 3.60–14.50 |
Incidence rates per 100,000 per year
Overall age and sex adjusted incidence of scleritis = 5.54 per 100,000 per year adjusted for 2010 US white population (95% CI 4.29–6.79)
Males: age adjusted incidence = 5.58 per 100,000 per year (95% CI 3.75–7.40)
Females: age adjusted incidence = 5.56 per 100,000 per year (95% CI 3.83–7.29) No significant difference between genders (p=0.75).
Significant difference across ages (p<0.001).
The majority of episcleritis (95.1%) and scleritis (76.6%) cases were not associated with systemic inflammatory or infectious causes. Notably, only 2 (0.897%) episcleritis and 4 (5.19%) scleritis patients had the associated diagnosis of rheumatoid arthritis. Twenty-six (11.7%) episcleritis cases and 8 (10.4%) scleritis patients also had a diagnosis of thyroid disease. There were no significant differences between scleritis cases with a systemic disease association versus those that were idiopathic with respect to age (p=0.92), sex (p=0.73), smoking status (p=0.90), and thyroid disease (p=0.91).
Among 77 scleritis patients, 60 (77.9%) cases were classified as diffuse/sectoral, 13 (16.9%) cases were nodular, 3 (3.9%) cases were posterior, and 1 (1.3%) case was necrotizing. Seventy (90.9%) patients had unilateral presentations, 3 were bilateral asynchronous, 1 was bilateral synchronous, and 3 with initial unilateral presentations subsequently developed bilateral synchronous recurrences. Twenty-nine (37.7%) of scleritis patients had a history of smoking. The majority of scleritis cases (81.8%) were managed with oral NSAIDs. Other treatments included corticosteroid eye drops (31.2%), systemic corticosteroids (13.0%), and systemic corticosteroid-sparing immunomodulatory medication (6.5%).
Follow-up visits were available for 67 (87.0%) scleritis cases; the median follow-up was 2.69 years (range: 0.011–11.78 years). There were 84 affected eyes from 77 scleritis patients. Nineteen eyes of 14 patients had recurrences, while 65 eyes from 63 cases had no recurrences. Two eyes from one patient were excluded from the calculation of mean recurrences and five year recurrence rate because the patient had chronic persistent scleritis without clear instances of remission. The five year recurrence rate was 25.5%, and all of the recurrences occurred within three years of initial diagnosis (Figure 2). Among 17 eyes from 13 patients, the mean number of recurrences per eye was 1.87 (range: 1–6).
Figure 2: Risk of Scleritis Recurrence per Eye.

The 5 year recurrence rate is 25.5% among 82 eyes. All of the recurrences occurred within three years.
In the 14 scleritis patients with recurrences, the median follow-up time after initial scleritis diagnosis was 2.71 years (range: 0.071–8.52 years) and the median follow-up per affected eye (19) was 2.63 years (range: 0.44–8.52 years). Patients with no scleritis recurrence had a median follow-up of 1.74 years (range: 0.00–11.78 years), including 10 patients who had no subsequent eye examinations. After excluding the 10 patients with no follow-up, scleritis patients with at least one subsequent visit had a median follow-up of 2.69 years (range: 0.011–11.78 years) and a median follow-up per affected eye (55) of 2.69 years (range 0.011–11.78).
Age, gender, systemic disease, thyroid disease, and smoking were analyzed as risk factors for scleritis recurrence. Increasing patient age (at presentation) was associated with a small decrease in the risk of recurrence: a ten year increase in age decreases the risk 0.73 times (p=0.058, 95% CI 0.52 – 1.01). Patients with systemic disease (35.7%) had an increased risk of recurrence (HR=1.89, 95% CI 0.69 – 5.05), but the difference was not statistically significant (p=0.22). Although 28.6% of patients with recurrent scleritis had a history of smoking, there was no statistically significant difference in recurrence compared to non-smokers (p=0.34). Gender (p=0.22) and thyroid disease (p=0.58) were also not associated with risk of recurrence.
Ocular complications affected 27 (35.1%) scleritis patients, and included anterior uveitis (13%), ocular hypertension (11.7%), vision loss of two or more lines of Snellen acuity (7.8%) between baseline and the last visit (which were 0.011 to 11.8 years apart), corneal involvement (3.9%), exudative retinal detachment (3.9%), and macular edema (2.6%) (Table 3). Among the 77 scleritis cases, 52 of 84 eyes had at least one year of follow-up after initial scleritis presentation. At the time of diagnosis, 49 (94.2%) affected eyes had best corrected Snellen visual acuity (BCVA) of 20/40 or better. Among those with at least one year of follow up, the final visual acuity was better than 20/40 in 47 (90.4%) of affected eyes; only 4 (7.7%) eyes lost two or more lines of Snellen visual acuity compared to baseline. 49 (92.3%) had the same or improved BCVA compared to baseline.
Table 3:
Ocular complications occurring after the diagnosis of scleritis
| Ocular complication | Number of cases (%) |
|---|---|
| Anterior uveitis | 10 (13.0%) |
| Corneal involvement | 3 (3.9%) |
| Macular edema | 2 (2.6%) |
| Optic disc edema | 0 (0%) |
| Vitritis | 1 (1.3%) |
| Exudative detachment | 3 (3.9%) |
| Decreased VA (>2 Snellen lines) | 6 (7.8%) |
| Cataract surgery | 4 (5.2%) |
| Ocular hypertension | 9 (11.7%) |
| Glaucoma surgery | 1 (1.3%) |
Discussion
We report the incidences of episcleritis and scleritis in a Midwestern, predominantly White population that has not been previously studied. In comparison to other population-based studies, this cohort had a lower overall age- and sex-adjusted incidence of episcleritis (15.39 per 100,000 per year) versus 21.7 per 100,000 person-years in the insurance based Pacific Ocular Inflammation Study (POIS) and 41.0 per 100,000 in the Northern California Epidemiology of Uveitis Study (NCEUS).4, 5 The incidence of scleritis in our study was 5.54 per 100,000 per year, slightly higher than POIS and NCEUS (4.1 and 3.4 per 100,000 person-years, respectively).4, 5 These variations in incidence rates may be related to differences racial/ethnic compositions; for example the 2010 Olmsted County MN population was 84% White, 5.4% Asian, and 4.7% Black compared to 27% White, 40% Asian, and 2% Black in the POIS cohort. Due to inadequate statistical power, it was not possible to look for differences in ethnicity and incidence of episcleritis or scleritis in this study.
In this population, the average age at episcleritis diagnosis was 40.2 years, slightly younger than the range of 43 to 47 years reported in the literature.4–7 For scleritis, the average age (48.8 years) was on the younger end of the previously reported range (47 – 59.5 years).4–7 Similar to other reports, episcleritis occurred more frequently in females.5, 61, 4, 6–10
In a notable divergence from previous studies, females were not over-represented among the scleritis cases. This difference may be related to the lower frequency of associated systemic disease.1, 4, 6–10 In this population, 23.4% of scleritis was associated with systemic disease, which is lower than reported in most referral center cohorts. In three tertiary care center studies, 33–39% of scleritis patients had associated systemic disease,6, 7, 11 and 36.0% was reported in a community-based referral practice.8 In the other population-based studies, the association of systemic disease was variable, from 6% of scleritis patients in the NCEUS to 41% in the POIS.4, 5
It is logical that a population-based study would include scleritis cases that are unlikely to be referred to a tertiary care or specialty service, such as those that are less severe, respond to treatment, and are not associated with systemic disease. The findings in this study support this idea. The rate of scleritis recurrence in our study (18%) was lower than the 50% recurrence rate reported by Kempen et al. in a referral center population.12 In our cohort, gender was not associated with increased risk of scleritis recurrence, but the concurrent diagnosis of systemic inflammatory disease showed a trend towards an increased risk of recurrence. Since females are thought to be more likely to develop many autoimmune/inflammatory diseases, they might also be more likely to be referred to a tertiary care center.13
Another indication of the severity of scleritis is the range of medications used for treatment. In this population, scleritis was treated most frequently with oral NSAIDs (81.8%) followed by corticosteroid eye drops (31.2%), systemic corticosteroids (13.0%), and systemic corticosteroid-sparing immunomodulatory medication (6.5%). In contrast, up to two-thirds of scleritis patients in referral center cohorts required treatment with oral corticosteroids and/or systemic immunomodulatory medication.7, 11 In the population-based POIS, more patients were treated with systemic corticosteroids (47.1%) and systemic immunomodulatory medication (35.5%) compared to our cohort (13.0% and 6.5%, respectively).14 However, POIS also had a higher percentage of scleritis patients with rheumatoid arthritis (29.4% versus 5.2% in this population) who are likely to require systemic treatment for the extraocular manifestations of rheumatoid inflammation. The range of treatments utilized in this study may also reflect clinician preference among non-subspecialist ophthalmologists and optometrists who may be less likely to use systemic medications including corticosteroids and immunomodulatory medication.
The frequency of scleritis-related ocular complications in our study was comparable to that of previous population-based studies: 35.1% versus 29.4% in POIS.14 In contrast, 59–85% of scleritis cases had complications in referral center studies.7, 11 Cystoid macular edema was diagnosed in only a small number of patients in this study, although imaging studies were not routinely obtained in the majority of patients. Anterior uveitis occurred in 13% of scleritis patients in this cohort, compared to 11.8% of POIS cases and around 25% in referral center cohorts.5, 6, 14 In contrast, none of the POIS cases developed ocular hypertension,14 whereas the frequency was 11.7% in this cohort, similar to tertiary care centers (10–14%).6, 7, 15 Finally, vision loss in scleritis cases from this population was less common compared to tertiary care centers: 7.7% of affected eyes in our study versus 16–22% in previous studies.6, 7 Jabs et al. defined vision loss as a decrease in best-corrected visual acuity of 2 or more Snellen lines from the initial best-corrected visual acuity and assessed visual acuity data from all visits.7 In contrast, Sainz de la Maza et al. defined vision loss as a decrease in visual acuity of 2 Snellen lines or more at the end of the follow up period, or best-corrected visual acuity of 20/80 or worse (in the worse seeing eye) at presentation.6 This approach would have missed any reductions in visual acuity that occurred between the first and last visits if visual acuity subsequently recovered with treatment. Despite these differences in defining vision loss, it appears that scleritis patients in the general population may be less likely to develop ocular complications in comparison to those seen in a tertiary care center.
Study Limitations
Several limitations of this study must be acknowledged. The majority of the Olmsted County study population is White, so the results may not be generalizable to other populations. In this retrospective study, examination and evaluation data was limited in some cases. Diagnosis coding was utilized to identify potential cases, and review of the medical records was performed to confirm diagnoses; however, the majority of patients were not seen by an ocular inflammatory disease specialist, and a standardized examination and systemic work up was not necessarily performed. Evidence of scleritis recurrence was determined through retrospective chart review, and the timing of follow up visits was not standard, so it may not have been possible to differentiate between true recurrences after remission versus chronic recalcitrant cases. Finally, some cases may have been missed if an Olmsted County resident received eye care from providers outside Olmsted County or from community optometrists who are not associated with the Rochester Epidemiology Project.3 Nonetheless, it is likely that the majority of primary and specialty eye care is captured in this database.
In summary, this study of a predominantly White U.S. population reveals age- and sex-adjusted episcleritis and scleritis incidences of 15.39 and 5.54 per 100,000 per year. Compared to previous studies, the incidence of episcleritis is lower while the incidence of scleritis is slightly higher. Notably, in contrast to other studies, females were not more likely to have scleritis, and the majority of cases were idiopathic (76.6%). Risk of scleritis recurrence was not associated with gender, but it was slightly decreased with increasing age at diagnosis. There was a non-statistically significant trend towards increased risk of recurrence in cases with associated systemic inflammatory disease. The scleritis cases from this predominantly primary eye care setting were less severe in terms of treatment required, complications, and recurrence when compared to tertiary care center cohorts.
The results from our study provide useful information for evaluating and counseling community patients with episcleritis and scleritis. In general, scleritis patients in the general population probably have a lower risk of vision-threatening complications. While there is evidence that scleritis may be less likely to be associated with systemic disease than previously reported in the literature, the patient’s history, risk factors, and review of systems should always be ascertained and used as the basis for determining if additional testing for systemic disease is warranted. Patients with associated systemic disease or severe, recalcitrant inflammation are likely to benefit from evaluation by an ocular inflammation specialist and/or rheumatologist, so early referral to a tertiary care center should be considered.
Supplementary Material
Acknowledgment/Disclosure
Funding/Support: This study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding source had no role in conduct of the research and preparation of the article.
Financial Disclosures: The following authors have no financial disclosures: Timothy T. Xu, Margaret M. Reynolds, David O. Hodge, and Wendy M. Smith.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplemental Material available at AJO.com.
References
- 1.Okhravi N, Odufuwa B, McCluskey P, Lightman S. Scleritis. Surv Ophthalmol 2005;50(4):351–63. [DOI] [PubMed] [Google Scholar]
- 2.Melton LJ 3rd. History of the Rochester Epidemiology Project. Mayo Clin Proc 1996;71(3):266–74. [DOI] [PubMed] [Google Scholar]
- 3.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ 3rd. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clinic proceedings 2012;87(12):1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Homayounfar G, Nardone N, Borkar DS, et al. Incidence of scleritis and episcleritis: results from the Pacific Ocular Inflammation Study. Am J Ophthalmol 2013;156(4):752–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Honik G, Wong IG, Gritz DC. Incidence and prevalence of episcleritis and scleritis in Northern California. Cornea 2013;32(12):1562–6. [DOI] [PubMed] [Google Scholar]
- 6.Sainz de la Maza M, Molina N, Gonzalez-Gonzalez LA, Doctor PP, Tauber J, Foster CS. Clinical characteristics of a large cohort of patients with scleritis and episcleritis. Ophthalmology 2012;119(1):43–50. [DOI] [PubMed] [Google Scholar]
- 7.Jabs DA, Mudun A, Dunn JP, Marsh MJ. Episcleritis and scleritis: clinical features and treatment results. Am J Ophthalmol 2000;130(4):469–76. [DOI] [PubMed] [Google Scholar]
- 8.Raiji VR, Palestine AG, Parver DL. Scleritis and systemic disease association in a community-based referral practice. Am J Ophthalmol 2009;148(6):946–50. [DOI] [PubMed] [Google Scholar]
- 9.Erkanli L, Akova YA, Guney-Tefekli E, Tugal-Tutkun I. Clinical features, prognosis, and treatment results of patients with scleritis from 2 tertiary eye care centers in Turkey. Cornea 2010;29(1):26–33. [DOI] [PubMed] [Google Scholar]
- 10.Ahn SJ, Oh JY, Kim MK, Lee JH, Wee WR. Clinical features, predisposing factors, and treatment outcomes of scleritis in the Korean population. Korean J Ophthalmol 2010;24(6):331–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wieringa WG, Wieringa JE, ten Dam-van Loon NH, Los LI. Visual outcome, treatment results, and prognostic factors in patients with scleritis. Ophthalmology 2013;120(2):379–86. [DOI] [PubMed] [Google Scholar]
- 12.Kempen JH, Pistilli M, Begum H, et al. Remission Of Non-Infectious Anterior Scleritis: Incidence And Predictive Factors. Am J Ophthalmol 2019; pii: S0002–9394(19)30134–5. doi: 10.1016/j.ajo.2019.03.024. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 13.Ji J, Sundquist J, Sundquist K. Gender-specific incidence of autoimmune diseases from national registers. J Autoimmun 2016;69:102–6. [DOI] [PubMed] [Google Scholar]
- 14.Homayounfar G, Borkar DS, Tham VM, Nardone N, Acharya NR. Clinical characteristics of scleritis and episcleritis: results from the pacific ocular inflammation study. Ocul Immunol Inflamm 2014;22(5):403–4. [DOI] [PubMed] [Google Scholar]
- 15.Bin Ismail MA, Lim RHF, Fang HM, et al. Ocular Autoimmune Systemic Inflammatory Infectious Study (OASIS)-report 4: analysis and outcome of scleritis in an East Asian population. J Ophthalmic Inflamm Infect 2017;7(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


