Abstract
This review explores the hypothesis that a consistent exercise time, especially consistent morning exercise, improves exercise adherence and weight management for individuals with overweight or obesity. We discuss data supporting this premise, identify limitations of current research, and outline directions for future research on exercise timing to more robustly evaluate our thesis.
Keywords: exercise timing, physical activity, circadian rhythms, weight management, habit, obesity, overweight
Summary for Table of Contents:
We discuss the hypothesis that consistent morning exercise improves exercise adherence and weight management among adults with obesity.
INTRODUCTION
Regular physical activity reduces risk of multiple chronic health conditions, including type 2 diabetes and cardiovascular disease. (1) Regular physical activity also assists with healthy weight management among adults with overweight/obesity. While physical activity alone does not typically produce substantial weight loss, physical activity in combination with reduced calorie intake leads to greater weight loss than dietary change alone. (2) A high amount (e.g., 300 min/wk) of moderate-to-vigorous intensity physical activity (MVPA) can also help to protect against weight regain. (3) Furthermore, a high level of cardiorespiratory fitness is associated with lower risk of all-cause mortality among individuals of all weight statuses, (4) highlighting the importance of regular physical activity for enhancing fitness among individuals with obesity independent of changes in body weight. Despite physical activity’s well-established benefits, many adults, and especially those with obesity, do not meet national physical activity recommendations. (5)
There has been a recent surge of interest in how the time of day that exercise is performed within the 24-hour clock (“exercise timing”) impacts a variety of outcomes. For example, numerous studies and recent reviews have examined how exercise timing relates to athletic performance; circadian rhythms; and various aspects of health like metabolic functioning. (6–11) Several reviews have also discussed how exercise timing, relative to meal timing, affects energy intake behaviors and physiological responses to eating (e.g., glycemic control). (12–14) However, less research has considered how exercise timing might be leveraged to (a) facilitate and sustain exercise behavior change, and (b) enhance weight management more broadly. Accordingly, current physical activity guidelines, including those pertaining to physical activity in the context of obesity management, do not address optimal exercise timing.
This review has two overarching objectives. First, we aim to review the small but growing literature on the relation of exercise timing to exercise behavior change and weight management (objective 1). Based on current findings, we propose that exercising at the same time of day—and specifically during the morning—facilitates exercise adherence and improves weight management among adults with overweight/obesity. We draw on findings from several recent studies, as well as theoretical models of exercise behavior, to support this thesis. We also outline a schematic model of how consistent morning exercise might favorably affect weight management. Second, we aim to outline a research agenda to more rigorously evaluate the potential implications of exercise timing for weight management (objective 2). We discuss key limitations of the current literature base and highlight several important avenues for future research. Given that research on exercise timing and weight management is in its infancy, we hope that this discussion—along with our schematic figure—can guide the design of future studies to more robustly evaluate our thesis.
Importantly, this brief review is narrative in nature. While we carefully reviewed the literature to identify relevant articles for inclusion, this review is not exhaustive. Additionally, although we briefly discuss several physiological processes by which exercise timing might affect weight management, we primarily emphasize behavioral pathways through which consistent morning exercise may exert benefit. Given the many biological systems involved in weight regulation, there are undoubtedly additional pathways by which exercise timing could impact weight that we do not discuss (e.g., by impacting cortisol or appetite-regulating hormones). Although beyond this scope of this brief review, we look forward to further research on these topics.
BARRIERS TO REGULAR EXERCISE
Many inactive individuals report intentions to exercise. (15) This is presumably especially true among individuals with obesity who are participating in structured interventions that emphasize and regularly set exercise goals, such as behavioral weight loss programs. While exercise intentions are an important predictor of exercise behavior, (15) a vast body of evidence indicates that it can be difficult to translate health behavior intentions into behavior. High discordance between exercise intentions and behavior has been documented in numerous experimental and correlational studies. (16) In addition, experimentally-induced increases in exercise intentions have modest effects on behavior. (17) While some of the discordance between exercise intentions and behavior may arise from often overlooked yet important nuances of the intention construct (e.g., decisional intention vs. intention strength), (18) individuals may also experience numerous barriers to exercise even when intentions are strong. These include perceived lack of time, waning motivation or low willpower in the moment, competing responsibilities, and low energy. (19) Individuals may also intend to exercise but fail to create a specific exercise plan, thus reducing the likelihood of successful enactment.
CONSISTENT TIMING AS A STRATEGY FOR FOSTERING REGULAR EXERCISE
Potential Mechanisms
There are a number of behaviorally-oriented reasons why exercising at a consistent time, and especially in the morning, could be a useful strategy for overcoming the aforementioned barriers to exercise. These include simplified planning, improved habit formation, and enhanced self-regulation (see Figure).
Figure.
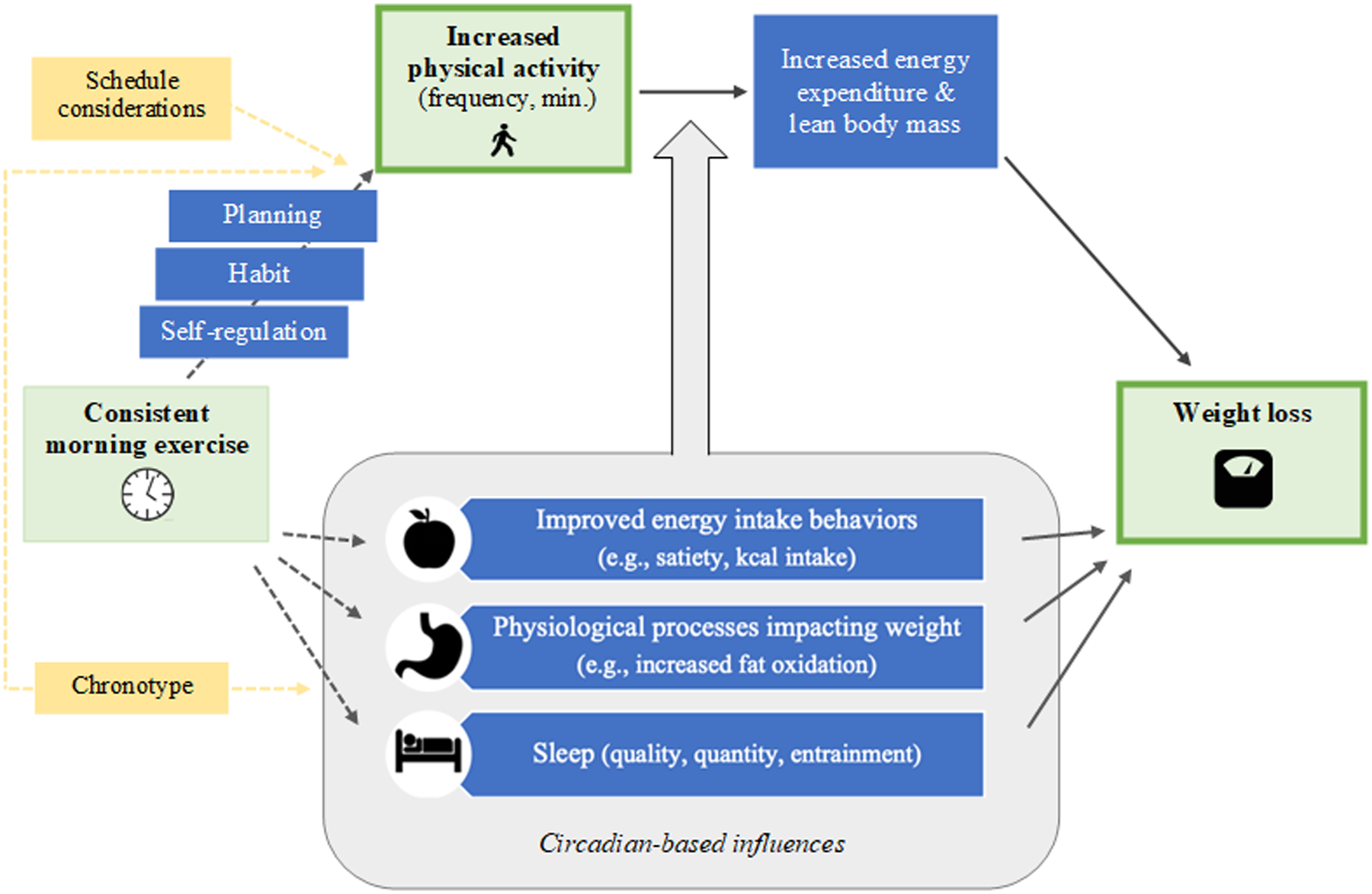
Conceptual model of the hypothesized effect of consistent morning exercise on physical activity levels and weight regulation. Blue boxes depict hypothesized mediators and yellow boxes depict potential moderators. As shown in grey, several processes may be influenced by circadian rhythms. Solid lines depict pathways for which there is strong evidence; dashed lines depict pathways which require further research.
Exercising at a consistent time may help to protect time for exercise, thereby making exercise planning easier and less complex. Planning is an effective time management and behavior change strategy that can help individuals to exercise even when faced with time pressures and competing responsibilities. (20) Many exercise interventions encourage individuals to create action plans for exercise, including plans for when exercise will be performed. For example, interventions may instruct individuals to schedule exercise on their weekly calendar and to treat it as a non-negotiable appointment. While such strategies can be effective, they require recurrent planning week-to-week. Planning may be less likely to occur during busy times. It may also be difficult to find time for exercise if planning occurs at the last minute or if other activities are allowed to fill one’s schedule. Having a consistent, designated exercise time reduces the need for complex planning, thus increasing the chances of exercise occurring. Committing to a consistent exercise time rather than allowing for a temporally variable exercise routine might also reduce the need for coping plans (i.e., plans for how to achieve one’s goal if one’s first-choice plan becomes unrealistic). (21) Consistent morning exercise may be especially effective in reducing planning complexity. Many individuals may have fewer events (e.g., social or work events) scheduled for the morning. This may thus allow individuals to plan on morning as their designated exercise time with fewer arising conflicts and needed coping plans.
Second, exercising at a consistent time may facilitate more frequent exercise via habit formation. Habit can broadly be defined as the process by which a specific context or cue triggers an impulse for a learned behavioral response with little conscious awareness or reflection. (22) As several researchers have recently highlighted, (22–26) exercise is a complex behavior that is unlikely to ever become fully controlled by non-conscious, automatic processes. Moreover, exercise is perhaps best conceptualized not as a single behavior but as multiple sub-actions that are expressed in a “macro” action, or as having distinct stages (e.g., instigation vs. execution). Notwithstanding these important distinctions, there is general agreement that aspects of exercise can be made more habitual and automatic, thus requiring less deliberate motivation and cognitive resources in-the-moment. A stronger exercise habit can help individuals to more efficiently translate their exercise intentions into behavior, and can facilitate exercise when explicit motivation temporarily wanes. (15, 27) Current evidence reveals a strong relation between exercise habit and behavior. (28) The cue-behavior associations that partially drive habit formation can be learned by repeated performance of the target behavior in a consistent context. (29) Consistently exercising at a specific time of day is thus one way to support exercise habit formation. Again, consistent morning exercise may be especially helpful for promoting an exercise habit. Many people have established morning routines, which offer potential cues to link with exercise (e.g., waking up, brushing teeth, then getting dressed for a walk). Physiological processes (e.g., circadian-related elevations in cortisol) may also support improved habit formation in the morning. (30)
Consistent morning exercise may also lead to more effective self-regulation. As the day progresses, self-regulation may become more difficult due to: new and emerging priorities that compete with exercise; lower self-regulatory strength; and incidental affect from other events in the day. These factors can negatively impact both exercise intentions and performance. (31–33) For these reasons, individuals may be most successful with making and enacting exercise intentions early in the day. Indeed, greater exercise intention-behavior concordance has been observed in the morning versus evening. (34)
Current Studies
Data from two studies conducted by our group support the potential benefits of a consistent exercise time, and perhaps specifically morning exercise, for facilitating exercise among adults with overweight/obesity (Table 1). In one study, we assessed the relation of exercise timing to weekly exercise frequency and minutes among physically active successful weight loss maintainers (i.e., individuals who had lost and maintained ≥13.6 kg for ≥1 year and who were performing MVPA on ≥2 days/wk, n=375). (35) Participants first reported whether they tended to exercise at the same time of day. If so, they then provided the start time of each exercise session (if any) for each day in a typical week. Exercise sessions were coded as early morning (4:00–8:59 am), late morning (9:00–11:59 am), afternoon (12:00–4:59 pm), or evening (5:00 pm-3:49 am). Participants were categorized as a temporally consistent exerciser if >50% of their exercise sessions were in a single time period. Participants were categorized as a temporally inconsistent exerciser if they (a) denied having a consistent exercise time, or (b) endorsed a temporally consistent schedule but ≤50% of their reported exercise sessions fell within a single time window. Consistency in cues for exercise and exercise habit strength were assessed via questionnaire. Results revealed that 68% of participants reported a temporally consistent exercise routine. Temporally consistent exercisers performed more exercise (e.g., MVPA on 4.8 vs. 4.4 days/wk, p=.007; 350 vs. 285 MVPA min/wk, p=.03) than temporally inconsistent exercisers. While early morning was the most common exercise time, exercise levels did not differ among temporally consistent exercisers based on the specific time of day (e.g., morning vs. evening) of temporally consistent exercise. Across participants, greater consistency in time-based cues for exercise (i.e., greater consistency in the time of exercise within the 24-hour clock and within one’s daily routine) and a stronger exercise habit related to more exercise days/wk and minutes/wk. These findings provide observational support for the notion that a consistent exercise time may help promote high levels of exercise. These findings also suggest that greater consistency in exercise timing relates to a stronger exercise habit.
Table.
Summary of studies on the effects of exercise timing on exercise adherence and weight change
| Reference | Participants | Design | Exercise Timing Randomized | Exercise Setting | Key Findings | Measured Potential Moderators/ Mediators |
|---|---|---|---|---|---|---|
| Studies evaluating effects on exercise frequency and weekly minutes | ||||||
| Schumacher et al. (2019) | 375 physically active adults in the National Weight Control Registry | Correlational | No | Community | 68% of participants had a consistent exercise time, of whom 48% performed exercise in the early morning (4:00–8:59 am). Temporally consistent exercisers (>50% of exercise sessions/wk at a consistent time of day) performed more exercise than temporally inconsistent exercisers (4.8 vs. 4.4 d/wk, p=.007; 350 vs. 285 min/wk, p=.03; 86% vs. 74% achieving ≥150 min/wk; p=.004). | Exercise habit strength, exercise cue consistency |
| Bond et al. (2017) | 33 adults seeking bariatric surgery participating in a 6-wk preoperative exercise intervention | Secondary analysis from RCT non-specific to Exercise timing | No | Community | At post-tx, a greater % of bouted morning exercise (4:00–11:59 am) related to greater pre- to post-tx increases in exercise (p=.03). A greater proportion of morning exercisers (>50% of exercise in the morning) achieving ≥150 min/wk of exercise than non-morning exercisers (p=.04). | N/A |
| Studies evaluating effects on weight | ||||||
| Chomistek et al. (2016) | 7,157 older women in the Women’s Health Study | Correlational | No | Community | Lower % of accelerometer counts in the morning (before 12:00 pm) related to higher odds of obesity; women in the lowest quartile for morning exercise had 26% higher odds of obesity compared to those in the highest quartile (p=.02). | N/A |
| Willis et al. (2019) | 88 inactive young adults with overweight/obesity participating in the Midwest Exercise Trial-2 | Secondary analysis from RCT non-specific to exercise timing | No | Supervised exercise training | 10-month weight loss was greater among early exercisers (≥50% exercise sessions from 7:00–11:59 am) compared to late exercisers (≥50% exercise sessions from 3:00–7:00 pm) and controls (no supervised exercise; p’s<.001). A greater proportion of early exercisers (vs. late) achieved ≥5% weight loss (p=.007). 10-month weight Δ negatively related to proportion of exercise sessions completed in the early period (p<.001). | Energy intake, energy intake timing, RMR |
| Alizadeh et al. (2017) | 48 inactive women with overweight BMIs in a 6-wk exercise training study on exercise timing | RCT | Yes | Supervised exercise training | Morning exercisers (8:00–10:00 am) had greater 6-wk reductions in weight (p=.04) and BMI (p=.04) compared to afternoon exercisers (2:00–4:00 pm). | Body composition, appetite and eating desire scores, dietary intake |
| Brooker et al. (2019) | 20 inactive adults with overweight/obesity in a 12-wk exercise study assessing the feasibility and acceptability of exercise timing | RCT | Yes | Supervised exercise training + community | The intervention was feasible (e.g., 90% of enrolled participants completed the study; the morning group completed 94% of supervised exercise sessions and the evening group completed 87%) and acceptable (e.g., perceived enjoyment of exercise was similar in the morning [67%] and evening groups [64%]). | Body composition; RMR; energy intake; appetite, food preferences, and eating behaviors; time use; sleep quality; chronotype; exercise enjoyment |
| Di Blasio et al. (2010) | 42 inactive, postmenopausal women with overweight/obesity in a 3-month walking program | Non-randomized trial | No | Supervised exercise training in the community | Δ in body weight did not differ between groups, but the evening group (6:00–8:00 pm) had greater decreases in % fat mass compared to the morning group (7:00–9:00 am; p=.037). Groups also differed in daily kcal distribution (e.g., evening group had greater increases in morning kcal intake and decreases in afternoon intake; p’s<.05). | Body composition, dietary intake |
Note. RCT=randomized controlled trial, BMI=body mass index, RMR=resting metabolic rate
Findings from another study by our group among individuals who were initiating exercise suggest that morning exercise, in particular, might be beneficial for exercise behavior change. (36) Bariatric surgery candidates with severe obesity (n=33) who were enrolled in a 6-wk preoperative exercise program were instructed to identify a specific time in the morning to complete their longest session of daily exercise (i.e., longest daily bout of walking at a moderate intensity). Participants’ exercise timing and bouted MVPA minutes were assessed via accelerometry. We calculated the percentage of participants’ longest MVPA bouts that were performed during the morning (4:00–11:59 am). We also categorized participants as a consistent morning exerciser (>50% of longest MVPA bouts between 4:00–11:59 am) or non-morning exerciser (>50% of longest MVPA bouts 12:00 pm or later). Results indicated that, across participants, a greater percentage of morning exercise at post-intervention related to greater pre- to post-intervention increases in bouted MVPA (β=.40, p=.036). Categorically, morning exercisers (37% of participants) also performed more minutes of bouted MVPA/day (35.8 vs. 22.0 min/d; p=.043) and were more likely to achieve ≥150 MVPA min/wk (64% vs. 26%; p=.044) at post-intervention. Taken together, findings from these two studies provide preliminary support for the hypothesis that a consistent exercise time, and perhaps especially morning exercise, could be leveraged to promote greater exercise among adults with obesity.
EFFECTS OF EXERCISE TIMING ON WEIGHT MANAGEMENT
As discussed above, one way in which exercise timing may impact weight is through facilitating greater exercise frequency and volume. Exercise timing may also influence weight and body composition independently of physical activity levels. While the literature on the relation of exercise timing to weight change among adults with obesity remains limited, results from several studies using a range of designs indicate that morning exercise favorably relates to weight management (Table 1).
Current Studies
Secondary analyses from two larger trials support the potential benefits of morning exercise for weight management. In an ancillary study for the Women’s Health Study, exercise was assessed via accelerometry among >7,100 older women and the proportion of daily accelerometer counts occurring before 12:00 pm was calculated. (37) Results revealed that women in the lowest quartile for morning exercise had 26% higher odds of obesity compared to women in the highest quartile (p=.02). This suggests that women who are less active in the morning may be at higher risk for obesity. The relation of exercise timing to weight change has also been assessed in the context of supervised exercise training. In one study, inactive young adults with overweight/obesity (n=88) who participated in a 10-month exercise program that required supervised exercise on 5 days of the week (the Midwest Exercise Trial-2) were categorized by the time of day of their exercise sessions as follows: early: >50% of sessions between 7:00–11:59 am; late: >50% of sessions between 3:00–7:00 pm; and sporadic: <50% of sessions during either time window. (38) Participants who served as controls were instructed to maintain their exercise levels and did not undergo exercise training. Results revealed that 10-month weight loss was greater in the early group (−7.2%) compared to both the late (−2.1%; p<.001) and control (+0.5%, p<.001) groups. The sporadic group (−5.5%;) also had greater weight loss than the control group (p=.01); mean weight loss did not differ between the early and sporadic groups. A greater proportion of early exercisers (81%) also achieved a clinically meaningful weight loss of >5% compared to late exercisers (36%; p=.007). Additionally, across participants, there was a dose response relationship between the proportion of exercise sessions completed in the morning and 10-month weight change (r=−.039; p<.001). Findings from both of these studies thus suggest morning exercise relates to more favorable weight management.
The observational data from the aforementioned studies indicate that consistent exercise timing, and particularly morning exercise, relate to greater exercise and weight loss. (35, 36, 37, 38) However, given the correlational nature of these findings, it is possible that consistent morning exercise serves as a marker for other factors underlying these improved outcomes (e.g., greater overall conscientiousness, greater commitment to or self-efficacy for behavior change). Results from two small randomized controlled trials that have experimentally assessed the impact of exercise timing on change in body weight and anthropometric characteristics suggest that consistent morning exercise is more than simply a marker for known correlates of successful weight control.
In the first study, 48 women with overweight were randomized to 6 weeks of morning (8:00–10:00 am) or afternoon (2:00–4:00 pm) supervised exercise training (3 days/wk of 30 min. of treadmill running at the ventilatory threshold heart rate). (39) Greater decreases in both weight (p=.04) and BMI (p=.04) were observed among individuals in the morning exercise group compared to the afternoon group. A more recent randomized trial compared the effects of prescribed morning (6:00–9:00 am) versus evening (4:00–7:00 pm) exercise versus a waitlist control on weight change among inactive adults with overweight/obesity (n=20). (40) The intervention lasted 12 wks and used a hybrid design of both supervised and unsupervised exercise (i.e., 50 minutes of supervised exercise on 5 days/wk for the first 4 wks, with the frequency of supervised sessions gradually tapering to 2 days/wk). Given the small n, the primary focus of the trial was on feasibility and acceptability. Results indicated that prescribed exercise timing was both feasible (e.g., study completion rate=90%; adherence to supervised exercise sessions: morning=94%, evening=87%) and acceptable (e.g., perceived enjoyment ratings: morning=67%, evening=64%). The authors also collected data on numerous weight-related outcomes and potential mechanisms of action. Between-group differences in weight change were not assessed due to limited power. Descriptively, mean pre- to post-intervention change in BMI was as follows: morning=−1.5 kg/m2, evening=−1.1 kg/m2.
Although most available data on the effects of exercise timing on weight favor morning exercise, evidence is not unequivocal. For example, in one nonrandomized study, postmenopausal women with overweight/obesity (n=29) participating in a 3-month walking program (with 50% of walking sessions supervised by a trainer) self-selected to walk in the morning (7:00–9:00 am) or evening (6:00–8:00 pm) for 50 min. on 4 days/wk at 55% of their target heart rate. (41) While no differences in weight change were observed between groups, the evening group experienced greater decreases in fat mass relative to the morning group (−1.71 kg vs. −0.24 kg fat mass, respectively; p=.037). Larger randomized controlled trials are thus needed to clarify the effects of exercise timing on weight.
Potential Mechanisms
There are several putative mechanisms, beyond exercise-related energy expenditure, through which consistent exercise timing might impact weight. These include energy intake behaviors, physiological processes involved in body weight regulation, and sleep (Figure). While the literature in most of these areas is heterogeneous and limited, there is presently preliminary support for each of these pathways.
As summarized by Fillon and colleagues, (13) findings from several studies indicate that morning exercise may be more advantageous than exercise later in the day for appetite and eating behavior. For example, in the study by Alizadeh et al. discussed above, the morning exercise group demonstrated greater decreases in fat (p=.049) and carbohydrate intake (p=.04) than the evening group, and there was a trend toward lower total kcal intake in the morning group (p=.06). (39) While not statistically significant, there were also a pattern of lowered energy intake among early exercisers in the study by Willis et al. (e.g., energy intake was 80–230 kcal/day lower among early vs. late exercisers). (38) Results from at least one study of the acute effects of exercise timing on eating among adults with overweight/obesity also indicate a benefit of morning exercise for satiety. (42) However, null effects have been observed in other studies with this population. (43) In addition to impacting total energy intake and dietary composition, it is plausible that exercise timing could impact the timing of eating and/or the length of the eating window. Some data suggest that both earlier timing of kcal intake and a shorter eating window are beneficial for weight regulation. (44, 45) In their secondary analysis, Willis’ and colleagues found that morning and sporadic exercisers consumed a greater proportion of their kcal in the morning compared to those in the non-exercise control group. While no differences in kcal timing were observed between the morning and evening groups, further study of the effect of exercise timing on kcal timing using randomized designs is warranted. (38)
Exercise timing may also influence weight via physiological processes, including greater fat oxidation and various circadian-based processes. Morning exercise, compared to exercise later in the day, may be more likely to be performed in a fasted state. Current evidence suggests that fasted exercise may confer metabolic advantages both during and after exercise (e.g., greater fat oxidation). (46, 47) Although additional research is needed that evaluates the independent and interacting effects of exercise timing and fasting/feeding schedules, morning exercise may positively impact weight partially by affecting fat metabolism.
With regard to circadian-based processes, a steadily-growing evidence base implicates circadian disruption in a variety of health issues (e.g., obesity, diabetes). (48) Exercise has been shown to be an important zeitgeber (time cue) for the human circadian system, helping to regulate and having the ability to phase-shift circadian rhythmicity. As discussed in several recent reviews, (6, 8–10) skeletal muscle is a major organ system that plays a key role in metabolism and many other processes (e.g. cardiovascular functioning). Exercise affects the molecular clocks in—and thus the functioning of—skeletal muscles and other peripheral tissues. Exercise also affects melatonin rhythms, which influence sleep/wake timing. For example, morning exercise has been shown to shift melatonin timing earlier, while exercise in the evening delays melatonin timing. (49) Given its effects on numerous aspects of the circadian system, exercise has the potential to be used strategically to facilitate circadian synchronization and to maximize the health benefits of exercise. While there is growing recognition of this potential, an optimal exercise time from a circadian standpoint has yet to be determined. The impact of exercise timing on physiological processes, like metabolism, is also likely to be influenced by many factors (e.g., exercise type; the individual’s chronotype, i.e., circadian-based propensity to sleep at a particular time during the 24-hour period; aspects of the individual’s health status). Thus, it will be important to comprehensively assess the potential ways in which exercise timing may influence weight via circadian-related processes.
With regard to sleep, numerous studies have evaluated the acute effects of exercise timing (i.e., effects of a single exercise session) on various aspects of sleep. Much of this work has evaluated exercising timing in terms of its relation to bed time rather than clock time. As highlighted in one recent meta-analysis of such studies, at present, there is mixed evidence for how exercise timing impacts sleep. (50) Exercise timing appears not to affect some aspects of sleep (e.g., total sleep time), while exercise shortly before and exercise >8 hrs before bed time positively impacts other aspects (e.g., less time spent in light sleep). As noted above, while some data suggest evening exercise might delay sleep timing, (49) other studies suggest minimal negative effects of evening exercise on sleep. (51) Given this mixed literature, as well as limited research on the chronic effects of differential exercise timing on sleep, additional research is needed.
LIMITATIONS AND FUTURE DIRECTIONS
There are several important limitations of past studies and unanswered questions that warrant further research. First, additional research is needed on the feasibility and acceptability of prescribed exercise timing. Although preliminary data suggest that prescribed exercise timing is both feasible and acceptable, (40) most prior studies on exercise timing either (a) have been secondary analyses, or (b) have examined exercise timing in the context of supervised exercise training studies, in which exercise behavior (e.g., frequency) is highly controlled. Thus, it has yet to be determined whether individuals performing exercise in free-living environments are able and willing to adhere to prescribed exercise timing over the short- or long-term.
Second, there is need for fully-powered, randomized controlled trials that assess the effects of exercise timing on both free-living exercise and weight loss. At present, data on the relation between exercise timing and exercise behavior is correlational. To determine whether exercise timing can be leveraged to causally increase exercise, studies are needed in which adults with obesity are randomized to exercise consistently at a specific time of day and the effect of exercise timing on free-living exercise is assessed. With regard to the impact of exercise timing on weight, two small randomized trials have examined how equal doses of exercise performed consistently at different times of the day impact weight change with promising results. (39, 40) Larger trials of this nature are thus warranted. There is also need for randomized trials that compare the effects of morning exercise, routine exercise prescriptions (i.e., at any convenient time), and a control. Importantly, it will likely be beneficial to examine exercise timing using more circumscribed time windows in these future studies. In past work, the window for defining morning exercise has often been quite broad (e.g., 7:00–11:59 am, 4:00–11:59 am). Particularly as some of the proposed mechanisms underlying morning exercise’s effect on weight (e.g., circadian-related processes) may differ across such a large timeframe, greater precision is needed in future research. For example, studies should differentiate between the effects of early vs. late morning exercise.
In order to more robustly evaluate our thesis and enhance understanding of the effects of exercise timing, it is also important to assess both mediators and moderators in future studies. In this review, we identify several behavioral and physiological pathways through which exercise timing may impact exercise behavior and broader weight regulation. Each of these warrants additional research using sophisticated assessment methods. There are likely also several important moderators of the effects of exercise timing on exercise adherence and weight. For example, from a behavioral perspective, specified exercise timing may best support regular exercise when there is a match between one’s chronotype and exercise schedule. (52) Physiologically, chronotype may also affect the benefits obtained from performing exercise at a particular time. For example, if an individual has a strong evening chronotype, waking up early for morning exercise may be less beneficial if it shortens sleep or if it leads to chronic circadian misalignment. The effects of exercise on peripheral clocks might also be optimized when exercise timing is personalized to individuals’ endogenous rhythms. (9. 10) Additionally, logistical considerations such as one’s work schedule may impact feasible exercise timing. (35) Further, certain aspects of one’s health status (e.g., type 2 diabetes) may influence the effects of exercise timing for a particular individual. (14) While data has been collected on some of these mediators and moderators in past work, (35, 38–41) their effects have not been evaluated among fully powered samples using randomized study designs.
Lastly, future studies should clarify whether the importance of exercise timing differs when individuals are attempting to make versus maintain changes in their exercise and weight. In our study with successful weight loss maintainers, many individuals had been maintaining weight loss for several years and we did not observe a particular advantage of morning exercise for exercise frequency or minutes. (35) It is thus possible that the benefits of consistent morning exercise reduce as exercise becomes integrated into one’s lifestyle. Such possibilities should be evaluated empirically.
IMPLICATIONS AND CONCLUSIONS
The current literature suggests that there are benefits of consistent morning exercise among adults with obesity for both (a) increasing exercise and (b) enhancing weight management. While future studies will be critical for confirming and elucidating the magnitude and precise nature of such benefits, this research area has strong potential to inform future interventions. For example, if the positive effects of consistent morning exercise are confirmed by future data, interventions should encourage and assist individuals in establishing a consistent morning exercise routine. Our conceptual figure can guide the selection and testing of potential intervention techniques (e.g., use of cues) to facilitate development of a such an exercise schedule. We also recognize that individuals may encounter various challenges when trying to implement morning exercise. For example, perceived effort may be greater and aspects of exercise performance may be poorer in the morning compared to later in the day, especially among individuals not identifying as a “morning type.” (53) Morning exercise may also be perceived as less enjoyable, (53) although acceptability data from Brooker et al. challenge this assumption. (40) Logistical barriers (e.g., morning childcare responsibilities) may deter morning exercise for some individuals, and there may be a trade-off between morning exercise and sleep if individuals have difficulty adjusting their bedtimes to accommodate a potentially earlier wake time. (54) Further consideration of this sleep-exercise tradeoff is warranted, although MVPA may be the most potent health-enhancing choice. (54) We hope that this review stimulates interest on the relation of exercise timing to weight management and facilitates research into potential strategies for overcoming these barriers.
In conclusion, current data indicate that consistent exercise timing, and especially consistent morning exercise, could be leveraged to promote more frequent exercise and more effective weight management among adults with overweight/obesity. Several behavioral and physiological pathways may underlie these benefits. Given that exercise timing is a discretionary aspect of exercise that could be targeted in interventions, future research is warranted that more robustly evaluates our thesis and that elucidates moderators and mechanisms of the effects of exercise timing.
Key Points:
Physical activity levels tend to be low among adults with obesity, and, in general, many individuals who intend to exercise have difficulty translating these intentions into behavior.
Recent data suggest that the time of day that exercise is performed within the 24-hour clock (“exercise timing”) may be able to be leveraged to facilitate exercise behavior change and enhance weight management among adults with obesity.
Consistent exercise timing, and especially consistent morning exercise, may facilitate greater exercise levels by enhancing planning, fostering an exercise habit, and/or improving self-regulation.
Morning exercise may also enhance weight loss independently of daily physical activity levels. Several behavioral and physiological processes (e.g., modified energy intake behaviors, circadian influences) may underlie such effects.
Potential implications for intervention, current limitations, and directions for future research to more robustly evaluate our thesis are discussed.
Funding:
T32 HL076134 (Schumacher; Wing-PI); R01 DK108579 (MPIs: Bond & Thomas).
Footnotes
Disclosures: The authors declare no conflict of interest.
References
- 1.Rhodes RE, Janssen I, Bredin SS, Warburton DE, Bauman A. Physical activity: Health impact, prevalence, correlates and interventions. Psychol Health. 2017;32(8):942–75. [DOI] [PubMed] [Google Scholar]
- 2.Johns DJ, Hartmann-Boyce J, Jebb SA, Aveyard P. Diet or exercise interventions vs combined behavioral weight management programs: a systematic review and meta-analysis of direct comparisons. J Acad Nutr Diet. 2014;114(10):1557–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Church TS. The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014;56(4):441–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, Blair SN. Fitness vs. fatness on all-cause mortality: a meta-analysis. Prog Cardiovasc Dis. 2014;56(4):382–90. [DOI] [PubMed] [Google Scholar]
- 5.Zenko Z, Willis EA, White DA. Proportion of adults meeting the 2018 Physical Activity Guidelines for Americans according to accelerometers. Front Public Health. 2019;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duglan D, Lamia KA. Clocking in, working out: circadian regulation of exercise physiology. Trends Endocrinol Metab. 2019. [DOI] [PMC free article] [PubMed]
- 7.Grgic J, Lazinica B, Garofolini A, Schoenfeld BJ, Saner NJ, Mikulic P. The effects of time of day-specific resistance training on adaptations in skeletal muscle hypertrophy and muscle strength: A systematic review and meta-analysis. Chronobiol Int. 2019;36(4):449–60. [DOI] [PubMed] [Google Scholar]
- 8.Lewis P, Korf HW, Kuffer L, Groß JV, Erren TC. Exercise time cues (zeitgebers) for human circadian systems can foster health and improve performance: a systematic review. BMJ Open Sport & Exercise Medicine. 2018;4(1):e000443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gabriel BM, Zierath JR. Circadian rhythms and exercise—re-setting the clock in metabolic disease. Nat Rev Endocrinol. 2019;15(4):197–206. [DOI] [PubMed] [Google Scholar]
- 10.Hower IM, Harper SA, Buford TW. Circadian rhythms, exercise, and cardiovascular health. J Circadian Rhythms. 2018;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teo SY, Kanaley JA, Guelfi KJ, Marston KJ, Fairchild TJ. The effect of exercise timing on glycemic control: A randomized clinical trial. Med Sci Sports Exerc. 2020;52(2),323–334. [DOI] [PubMed] [Google Scholar]
- 12.Parr EB, Heilbronn LK, Hawley JA. A Time to Eat and a Time to Exercise. Exerc Sport Sci Rev. 2020;48(1):4–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fillon A, Mathieu M, Boirie Y, Thivel D. Appetite control and exercise: Does the timing of exercise play a role? Physiol Behav. 2019:112733. [DOI] [PubMed] [Google Scholar]
- 14.Heden TD, Kanaley JA. Syncing exercise with meals and circadian clocks. Exerc Sport Sci Rev. 2019;47(1):22–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rhodes RE, Bruijn GJ. How big is the physical activity intention–behaviour gap? A meta-analysis using the action control framework. Br J Health Psychol. 2013;18(2):296–309. [DOI] [PubMed] [Google Scholar]
- 16.Rhodes RE, Yao CA. Models accounting for intention-behavior discordance in the physical activity domain: a user’s guide, content overview, and review of current evidence. Int J Behav Nutr Phy. 2015;12(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rhodes RE, Dickau L. Experimental evidence for the intention–behavior relationship in the physical activity domain: A meta-analysis. Health Psychol. 2012;31(6):724. [DOI] [PubMed] [Google Scholar]
- 18.Rhodes RE, Rebar AL. Conceptualizing and defining the intention construct for future physical activity research. Exerc Sport Sci Rev. 2017;45(4):209–16. [DOI] [PubMed] [Google Scholar]
- 19.McIntosh T, Hunter DJ, Royce S. Barriers to physical activity in obese adults: a rapid evidence assessment. J Res Nurs. 2016;21(4):271–87. [Google Scholar]
- 20.Carraro N, Gaudreau P. Spontaneous and experimentally induced action planning and coping planning for physical activity: A meta-analysis. Psychol Sport Exerc. 2013;14(2):228–48. [Google Scholar]
- 21.Schwarzer KR. Coping planning as an intervention component: A commentary. Psychol Health. 2016;31(7):903. [DOI] [PubMed] [Google Scholar]
- 22.Hagger MS. Habit and physical activity: Theoretical advances, practical implications, and agenda for future research. Psychol Sport Exerc. 2018.
- 23.Phillips LA. Challenging assumptions about habit: A response to Hagger (2019). Psychol Sport Exerc. 2019.
- 24.Gardner B, Rebar AL, Lally P. ‘Habitually deciding’or ‘habitually doing’? A response to Hagger (2019). Psychol Sport Exerc. 2019:101539. [Google Scholar]
- 25.Hagger MS. Redefining habits and linking habits with other implicit processes. Psychol Sport Exerc. 2020;46:101606. [Google Scholar]
- 26.Rhodes RE, Rebar AL. Physical activity habit: Complexities and controversies. The psychology of habit: Springer; 2018. p. 91–109. [Google Scholar]
- 27.Rebar AL, Rhodes RE, Gardner B. How we are misinterpreting physical activity intention–behavior relations and what to do about it. Int J Behav Nutr Phy. 2019;16(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rebar AL, Dimmock JA, Jackson B, Rhodes RE, Kates A, Starling J, et al. A systematic review of the effects of non-conscious regulatory processes in physical activity. Health Psychol Rev. 2016;10(4):395–407. [DOI] [PubMed] [Google Scholar]
- 29.Kaushal N, Rhodes RE. Exercise habit formation in new gym members: a longitudinal study. J Behav Med. 2015;38(4):652–63. [DOI] [PubMed] [Google Scholar]
- 30.Fournier M, d'Arripe-Longueville F, Rovere C, Easthope CS, Schwabe L, El Methni J, et al. Effects of circadian cortisol on the development of a health habit. Health Psychol. 2017;36(11):1059. [DOI] [PubMed] [Google Scholar]
- 31.Rebar AL, Dimmock JA, Rhodes RE, Jackson B. A daily diary approach to investigate the effect of ego depletion on intentions and next day behavior. Psychol Sport Exerc. 2018;39:38–44. [Google Scholar]
- 32.Rhodes RE, Quinlan A, Mistry CD. Do other goals influence physical activity? A systematic review examining the relationship between other goals and physical activity behavior. Prev Med. 2016;91:306–17. [DOI] [PubMed] [Google Scholar]
- 33.Kerrigan SG, Schumacher L, Manasse SM, Loyka C, Butryn ML, Forman EM. The association between negative affect and physical activity among adults in a behavioral weight loss treatment. Psychol Sport Exerc. 2019. [DOI] [PMC free article] [PubMed]
- 34.Bailey KJ, Jung ME. The early bird gets the worm! Congruency between intentions and behavior is highest when plans to exercise are made for the morning. J Appl Biobeh Res. 2014;19(4):233–47. [Google Scholar]
- 35.Schumacher LM, Thomas JG, Raynor HA, Rhodes RE, O’Leary KC, Wing RR, et al. Relationship of consistency in timing of exercise performance and exercise levels among successful weight loss maintainers. Obesity. 2019;27(8):1285–91. [DOI] [PubMed] [Google Scholar]
- 36.Bond DS, Raynor HA, Thomas JG, Unick J, Webster J, Ryder B, et al. Greater adherence to recommended morning physical activity is associated with greater total intervention-related physical activity changes in bariatric surgery patients. J Phys Act Health. 2017;14(6):492–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chomistek AK, Shiroma EJ, Lee I-M. The relationship between time of day of physical activity and obesity in older women. J Phys Act Health. 2016;13(4):416–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Willis EA, Creasy SA, Honas JJ, Melanson EL, Donnelly JE. The effects of exercise session timing on weight loss and components of energy balance: midwest exercise trial 2. Int J Obes. 2019:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alizadeh Z, Younespour S, Rajabian Tabesh M, Haghravan S. Comparison between the effect of 6 weeks of morning or evening aerobic exercise on appetite and anthropometric indices: a randomized controlled trial. Clin Obes. 2017;7(3):157–65. [DOI] [PubMed] [Google Scholar]
- 40.Brooker PG, Gomersall SR, King NA, Leveritt MD. The feasibility and acceptability of morning versus evening exercise for overweight and obese adults: A randomized controlled trial. Contemp Clin Trials. 2019;14:100320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Di Blasio A, Di Donato F, Mastrodicasa M, Fabrizio N, Di Renzo D, Napolitano G, et al. Effects of the time of day of walking on dietary behaviour, body composition and aerobic fitness in post-menopausal women. J Sports Med Phys Fitness. 2010;50(2):196–201. [PubMed] [Google Scholar]
- 42.Alizadeh Z, Mostafaee M, Mazaheri R, Younespour S. Acute effect of morning and afternoon aerobic exercise on appetite of overweight women. Asian J Sports Med. 2015;6(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Larsen P, Marino F, Melehan K, Guelfi KJ, Duffield R, Skein M. Evening high-intensity interval exercise does not disrupt sleep or alter energy intake despite changes in acylated ghrelin in middle-aged men. Exp Physiol. 2019. [DOI] [PubMed]
- 44.Allison KC, Goel N. Timing of eating in adults across the weight spectrum: Metabolic factors and potential circadian mechanisms. Physiol Behav. 2018;192:158–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rynders CA, Thomas EA, Zaman A, Pan Z, Catenacci VA, Melanson EL. Effectiveness of intermittent fasting and time-restricted feeding compared to continuous energy restriction for weight loss. Nutrients 2019;11(10):2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vieira AF, Costa RR, Macedo RCO, Coconcelli L., Kruel LFM. Effects of aerobic exercise performed in fasted v. fed state on fat and carbohydrate metabolism in adults: a systematic review and meta-analysis. Br J Nutr. 2016;116(7):1153–1164. [DOI] [PubMed] [Google Scholar]
- 47.Aird TP, Davies RW, Carson BP. Effects of fasted vs fed-state exercise on performance and post-exercise metabolism: A systematic review and meta-analysis. Scand J Med Sci Sports. 2018;28(5):1476–1493. [DOI] [PubMed] [Google Scholar]
- 48.Reutrakul S, Knutson KL. (2015 Consequences of circadian disruption on cardiometabolic health. Sleep Med Clin. 2015;10(4):455–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Youngstedt SD, Elliott JA, Kripke DF. Human circadian phase–response curves for exercise. J Physiol. 2019;597(8):2253–2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38(3):427–49. [DOI] [PubMed] [Google Scholar]
- 51.Stutz J, Eiholzer R, Spengler CM. Effects of evening exercise on sleep in healthy participants: A systematic review and meta-analysis. Sports Med. 2019;49(2):269–87. [DOI] [PubMed] [Google Scholar]
- 52.Hisler GC, Phillips AL, Krizan Z. Individual differences in diurnal preference and time-of-exercise interact to predict exercise frequency. Ann Behav Med. 2016;51(3):391–401. [DOI] [PubMed] [Google Scholar]
- 53.Vitale JA, Weydahl A. Chronotype, physical activity, and sport performance: a systematic review. Sports Med. 2017;47(9):1859–68. [DOI] [PubMed] [Google Scholar]
- 54.Chaput J-P, Carson V, Gray C, Tremblay M. Importance of all movement behaviors in a 24 hour period for overall health. Int J Environ Res Public Health. 2014;11(12):12575–81. [DOI] [PMC free article] [PubMed] [Google Scholar]


