Abstract
This study investigated the diagnostic utility of the Child Behavior Checklist (CBCL) Rule-Breaking Behavior scale to identify children of both sexes with conduct disorder (CD). Participants were derived from four independent datasets of children with and without attention deficit hyperactivity disorder and bipolar-I disorder of both sexes. Participants had structured diagnostic interviews with raters blinded to subject ascertainment status. Receiver operating characteristic (ROC) curves were used to examine the scale’s ability to identify children with and without CD. The sample consisted of 674 participants (mean age of 11.7 ± 3.3 years, 57% male, 94% Caucasian). The interaction to test if CBCL Rule-Breaking Behavior scores identified males and females with CD differently was not significant, thus we performed ROC analysis in the combined group. The ROC analysis of the scale yielded an area under the curve of 0.9. A score of ≥60 on the scale correctly classified 82% of participants with CD with 85% sensitivity, 81% specificity, 48% positive predictive value, 96% negative predictive value. The CBCL Rule-Breaking Behavior scale was an efficient tool to identify children with CD.
Keywords: Child Behavior Checklist (CBCL), rule breaking behavior, conduct disorder, children
Introduction
Conduct disorder (CD) is a childhood onset, prevalent, and morbid psychiatric disorder estimated to affect up to 7% of youth in the United States.1–3 CD is characterized by “a repetitive and persistent pattern of behavior in which the basic rights of others or major age-appropriate societal norms or rules are violated,” as defined in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM 5).4 CD is more prevalent in males than in females,1,5 and frequently co-occurs with other psychiatric disorders.6–8 When CD co-occurs with other psychiatric disorders in the clinical setting the diagnosis of CD may not always be considered due to the higher acuity and therapeutic opportunities for the co-occurring disorders.
Yet, CD is associated with serious complications. Youth with CD are at five times greater risk to develop a substance use disorder (SUD) compared to youth without CD,9 and this risk is even higher in CD youth with comorbid disorders such as attention deficit hyperactivity disorder (ADHD) and bipolar (BP) disorder.10–12 CD in adolescents has also been associated with increased risk for premature death in young adulthood.3 Given the increased morbidity associated with CD increased efforts are needed to help identify children with CD in the clinical setting.
One potential screening method for CD is the Child Behavior Checklist (CBCL), a simple to use, inexpensive, empirically derived, broad band assessment of psychopathology with excellent psychometric properties 13 and norms for both sexes. One of the scales from the CBCL, the Rule-Breaking Behavior scale (previously referred to as the Delinquency scale) bears strong conceptual resemblance to the clinical diagnosis of CD. Questions that contribute to the Rule-Breaking Behavior scale score are similar to those used to diagnose CD, for example, questions about the frequency with which the child lies or cheats, sets fires, and steals at home or outside the home.
Previous research found the Rule-Breaking Behavior scale to be significantly associated with a clinical diagnosis of CD in largely male samples of children with ADHD,14,15 community,16 and psychiatrically referred samples.17–19 However, uncertainties remain as to the optimal cut off point for the CBCL Rule-Breaking Behavior scale, and whether the scale can identify girls with a possible diagnosis of CD with high accuracy. It is particularly important to examine the accuracy of the CBCL Rule-Breaking Behavior scale in the identification of girls with CD because this diagnosis was for many years under recognized and under studied relative to boys.20
The main aim of this study was to identify the optimal cut-off point of the CBCL Rule-Breaking Behavior scale to help identify children of both sexes with a clinical diagnosis of CD. To this end, we applied conditional probability and receiver operating curve (ROC) analysis to a large sample comprised of four data sets of children of both sexes with and without ADHD and BP-I disorder. Children enrolled in these studies were systematically and thoroughly assessed with the same methodology which allowed us to combine the samples to evaluate this research question. Based on the literature and our previous work, we hypothesized that modest elevations of the CBCL Rule-Breaking Behavior scale would predict a structured interview derived diagnosis of CD. To the best of our knowledge this is the largest and most comprehensive evaluation of the diagnostic efficiency of the CBCL Rule-Breaking Behavior scale to help identify children with a clinical diagnosis of CD of both sexes.
Methods
Sample
The sample was derived from four independent studies using identical assessment methodology: 1) and 2) were prospectively controlled family studies of boys and girls 6 to 17 years of age with and without DSM-III-R ADHD (Boys Study: N=140 ADHD and N=120 Controls; Girls Study: N=140 ADHD and N=122 Controls); 21,22 3) was a prospective controlled family study of youth 10 to 18 years of age with (N=105) and without (N=98) DSM-IV pediatric BP-I disorder; 23 and 4) was a prospective family study of youth 6 to 17 years of age of both sexes with active symptoms of DSM-IV BP-I Disorder (N=105).24 The ADHD studies recruited participants from pediatric and psychiatric clinics. The BP disorder studies recruited participants from referrals to the Clinical and Research Programs in Pediatric Psychopharmacology at the Massachusetts General Hospital and through advertisements in the community. Controls were recruited from pediatric clinics, advertisements to hospital personnel and community newspapers, and Internet postings. Potential participants, including controls, were excluded from all four studies if they had been adopted, if their nuclear family was not available for study, if they had major sensorimotor handicaps, autism, inadequate command of the English language, or Full-Scale IQ < 70 (<80 for the ADHD studies). Potential participants were also excluded from the ADHD studies if they had psychosis, and from the BP disorder studies if their BP-I disorder was due solely to a medication reaction. For all four studies parents provided written informed consent to participate. Children and adolescents provided written assent to participate. The Partners Human Research Committee approved these studies.
Assessment Procedures
In all four studies, psychiatric assessments of participants were made with the Kiddie Schedule for Affective Disorders – Epidemiologic Version.25,26 Diagnoses were based on independent interviews with parents and direct interviews with children older than 12 years of age. Data were combined such that endorsement of a diagnosis by either reporter resulted in a positive diagnosis.
Extensively trained and supervised psychometricians with undergraduate degrees in psychology conducted all interviews. For the ADHD studies and the controlled BP disorder study, raters were blind to the ascertainment status of the families. For the BP disorder Family study, raters were blind to the study assignment and whether the subject was a proband or sibling.
To assess the reliability of our overall diagnostic procedures, we computed kappa coefficients of agreement by having experienced, blinded, board-certified child and adult psychiatrists and licensed experienced clinical psychologists diagnose participants from audiotaped interviews made by the assessment staff. Based on 500 assessments from interviews of children and adults, the median kappa coefficient was 0.98 for the ADHD studies and the controlled BP disorder study, and 0.99 for the BP disorder Family study.
Socioeconomic status was measured using the 5-point Hollingshead scale.27 A higher score indicates being of a lower socioeconomic status.
CBCL
The parent of each participant completed the 1991 version of the CBCL for ages 4 to 18 years. The CBCL queries the parent about the child’s behavior in the past six months with a three-point likert scale ranging from “not true” to “very true or often true,” and aggregates this data into behavioral problem t-scores.28 A computer program calculates the t-scores for each scale. Raw scores are converted to gender and age standardized scores (t-scores having a mean of 50 and standard deviation of 10). A minimum t-score of 50 is assigned to scores that fall at percentiles of ≤ 50 on the syndrome scales to permit comparison of standardized scores across scales. T-scores above 70 (2 standard deviations) indicate clinical disorder. Scales include Anxious/Depressed, Withdrawn/Depressed, Somatic Complains, Social Problems, Thought Problems, Attention Problems, Rule-Breaking Behavior, and Aggressive Behavior.
Statistical Analysis
We first compared demographic characteristics between participants with and without CD in each of the studies separately and then in the combined sample using Student’s t-test for continuous outcomes, Pearson’s chi-square test or Fisher’s exact test (for expected counts <5) for binary outcomes, and Wilcoxon rank-sum for ordinal outcomes. Next, we calculated conditional probabilities for each of the studies separately using a conservative cut-off point of >60 (1 standard deviation) for the CBCL Rule-Breaking Behavior scale. We subsequently combined the data from the four studies and subjected them to ROC curves, using a nonparametric approach, to examine the ability of the CBCL Rule-Breaking Behavior t-scores to identify those with and without a structured interview diagnosis of CD. ROC analysis uses each value across the entire range of CBCL scale t-scores as the cutoff for defining a case and compares this classification to the “true” diagnosis, as defined by the clinical interview. The ROC analysis then plots the false positive rate (1-specificity) and the true positive rate (sensitivity) for each CBCL Rule-Breaking Behavior t-score on the x- and y-axis, respectively, to create the ROC curve. Starting in the lower right-hand corner of the plot, each successive point corresponds to an increase in one point in the CBCL Rule-Breaking Behavior t-score. ROC analysis summarizes diagnostic efficiency with the area under the curve statistic. An area under the curve of 0.5 means the test does not predict the disorder in any way, and an area under the curve of 1.0 means the test predicts the disorder perfectly. The area under the curve statistic is useful in that it is equivalent to the Mann-Whitney U-statistic computed from a comparison of the CBCL-Rule Breaking Behavior score between the CD and non-CD groups.29 We used conditional probabilities to examine the diagnostic utility of various cutoff points. For each cutoff, we calculated sensitivity, specificity, the positive predictive value, negative predictive value, and the percent correctly classified. Based on the information from the ROC curve analysis, we used the nearest-to-(0,1) method to calculate the optimal cut-point to identify those with and without CD. This method identifies the cut-point on the ROC curve that is closest to the upper left corner of the graph, i.e. the point plotted at (0,1), representing perfect sensitivity and specificity. All analyses were performed using Stata® (Version 14).
Results
Demographic Characteristics of the Sample
Participants from the four original independent samples were only included in this sample if a CBCL was completed. Table 1 shows the demographic details from the four contributing samples. There were no meaningful demographic differences between children with and without a structured diagnostic interview of CD within each of the four samples. Children with CD were more likely to be male and older when compared to children without CD. No other meaningful sociodemographic differences were identified in socioeconomic status or race (Table 1).
Table 1.
Demographic characteristics of those with and without conduct disorder from the individual studies and all studies combined.
| Boys Attention Deficit Hyperactivity (ADHD) Study | Girls ADHD Study | Bipolar (BP) Disorder Controlled Study | BP Disorder Family Study | All Studies Combined | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No Conduct Disorder N=220 | Conduct Disor der N=31 | No Conduct Disorder N=212 | Conduct Disorder N=8 | No Conduct Disorder N=107 | Conduct Disorder N=52 | No Conduct Disorder N=21 | Conduct Disorder N=23 | No Conduct Disorder N=560 | Conduct Disorder N=114 | Test Statistic | P-Value‡ | |
| Mean ±SD | Mean ±SD | Mean ±SD | Mean ±SD | Mean ±SD | Mean ±SD | Mean ±SD | Mean ±SD | Mean ±SD | Mean ±SD | |||
| Age | 10.9 ± 3.3 | 11.9 ± 3.6 | 11.6 ± 3.2 | 12.9 ± 3.6 | 13.3 ± 2.1 | 14.1 ± 2.4 | 8.8 ± 3.4 | 9.6 ± 3.7 | 11.6 ± 3.2 | 12.5 ± 3.6 | t672=−2.77 | 0.006 |
| Socioeconomic Status† | 1.7 ± 0.8 | 1.9 ± 1.1 | 1.8 ± 0.8 | 2.4 ± 1.3 | 1.7 ± 1.2 | 1.7 ± 1.1 | 1.6 ± 0.9 | 1.9 ± 1.0 | 1.7 ± 0.9 | 1.9 ± 1.1 | z=−1.20 | 0.23 |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |||||
| Male | 220 (100) | 31 (100) | 0 (0) | 0 (0) | 64 (60) | 37 (71) | 18 (86) | 16 (70) | 302 (54) | 84 (74) | χ2=15.11 | <0.001 |
| Caucasian†† | 220 (100) | 31 (100) | 193 (93) | 8 (100) | 86 (84) | 47 (94) | 18 (86) | 20 (87) | 517 (94) | 106 (95) | χ2=0.07 | 0.79 |
Not everyone has Socioeconomic Status (SES) reported. Smaller sample sizes for this measure were: Girls ADHD Study: 219, BP Disorder Controlled Study: 115; Sample size for SES for all studies combined: 629
Not everyone has race reported. Smaller sample sizes for this measure were: Girls ADHD Study: 215; BP Disorder Controlled Study: 152; Sample size for race for all studies combined: 662
There were no significant demographic differences between children with and without a structured diagnostic interview of CD within each of the four samples.
Conditional Probability Analysis
As shown in Table 2, similar values of sensitivity [77%−89%], specificity [75%−86%], and percent correctly classified with CD [80%−86%] were observed in the Boys ADHD study, Girls ADHD study, and BP disorder controlled study using the conservative cut off point of >60 (1 SD) for the CBCL Rule-Breaking Behavior scale. The BP disorder family study had similar sensitivity (87%) to the other studies, but lower specificity (38%) and percent correctly classified (64%).
Table 2.
Sensitivity, specificity, and percent correctly classified using the conservative cut-off of >60 on the Rule-Breaking subscale of the Child Behavior Checklist to identify youth with conduct disorder in each study.
| Sensitivity | Specificity | Correctly Classified | |
|---|---|---|---|
| Boys Attention Deficit Hyperactivity (ADHD) Study (N=251) | 77% | 86% | 85% |
| Girls ADHD Study (N=220) | 88% | 86% | 86% |
| Bipolar (BP) Disorder Controlled Study (N=159) | 89% | 75% | 80% |
| BP Disorder Family Study (N=44) | 87% | 38% | 64% |
ROC Analysis
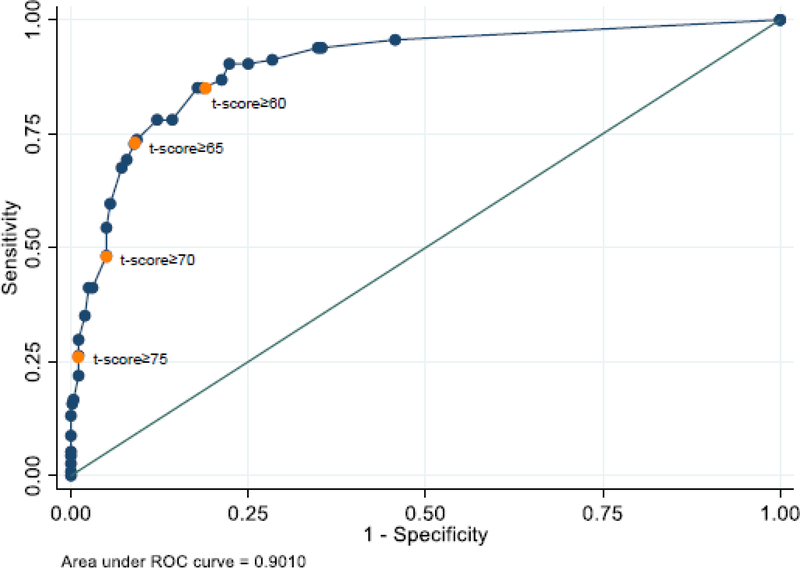
Since all the studies used identical methodology and assessments and had mostly similar conditional probability analysis results, we combined data from the four samples for this analysis to improve statistical power. Thus, our combined sample consisted of 674 participants, of which 114 (16.9%) had conduct disorder. CBCL Rule-Breaking Behavior t-scores ranged from 50 to 87 with a median of 51 and a mean (standard deviation) of 56.5 (8.8). First, we ran a model to test for an interaction between CBCL Rule-Breaking Behavior scores and sex to see if the scores identified males and females with CD differently. This interaction was not significant (z=−0.46, p=0.65) and thus we removed it from our model. Next, we ran a model predicting CD from only the CBCL Rule-Breaking Behavior scale. Figure 1 depicts the combined T-scores from the four studies of the CBCL Rule-Breaking Behavior scale that yielded an area under the curve of 0.9.
Figure 1.
Receiver operating characteristic (ROC) curve of the Child Behavior Checklist Rule Breaking Tscores in subjects from the total sample with and without conduct disorder (N=674).
Further examination of the performance of specific cut off t-scores that correspond to 0.5 SD increases in the CBCL Rule-Breaking Behavior scale to correctly identify participants with a structured diagnostic interview diagnosis of CD showed that a cut-point of 60 had the best properties as determined by the area under the curve with 85% sensitivity, 81% specificity, 48% positive predictive value, 96% negative predictive value, and 82% correctly classified with CD (Table 3). This cut-point has the greatest tradeoff between sensitivity and specificity.
Table 3.
Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and percent correctly classified in the use of the Child Behavior Checklist Rule-Breaking subscale T-scores to to identify youth with conduct disorder in the total sample from all four studies (N=674).
| CBCL Rule | Sensitivity | Specificity | PPV | NPV | Correctly Classified |
|---|---|---|---|---|---|
| Breaking Cut-Point | |||||
| ≥60 | 85% | 81% | 48% | 96% | 82% |
| ≥65 | 73% | 91% | 62% | 94% | 88% |
| ≥70 | 48% | 95% | 66% | 90% | 87% |
| ≥75 | 26% | 99% | 83% | 87% | 87% |
Discussion
ROC analysis using data from children of both sexes showed that a modestly elevated t-score of one standard deviation on the CBCL Rule-Breaking Behavior scale very efficiently identified children with a structured interview diagnosis of CD (area under the curve= 0.9). These results confirm and extend previously reported findings and provide strong evidence that the CBCL Rule-Breaking Behavior scale is a useful tool to identify youth who may have CD in both sexes in the clinical setting.
Our results showing the very high efficiency of the CBCL Rule-Breaking Behavior scale in identifying CD in clinical samples of both sexes extends to females previously reported findings in largely male samples of referred youth with ADHD,15 community,16 and psychiatrically referred samples.17–19 The absence of an interaction effect by sex suggests that sex does not moderate the efficiency of the CBCL Rule-Breaking Behavior scale in identifying children who may have a clinical diagnosis of CD.
Our finding documenting that a modest t-score of 60 (1 standard deviation) on the CBCL Rule-Breaking Behavior scale had the best properties for identifying youth with CD is consistent with our previous work14 in a sample of psychiatrically referred boys with ADHD. It is also consistent with findings reported by Kazdin et al who also found an association between a score of 60 on the CBCL Delinquency/Rule-Breaking Behavior scale and a diagnosis of CD in a sample of psychiatrically referred males.19
However, our conditional probability analysis showing high (81%) specificity associated with a 1 standard deviation elevation on the CBCL Rule-Breaking Behavior scale with a clinical diagnosis of CD is discrepant with the low (7.3%) specificity findings reported by Kazdin et al.19 Although the reasons for the discrepancy are unknown, it may be related to differences in sample composition (psychiatric inpatient versus outpatient and community referrals), as well as differences in assessment methodology (open label clinical diagnosis versus structured diagnostic interview by blinded raters). More work is needed to reconcile these differences.
The high negative predictive value (95%) for the CBCL Rule-Breaking Behavior scale suggests that a clinician can be very confident that a child does not have CD if the scale is not elevated. On the other hand, the modest positive predictive value suggests some children with an elevated CBCL Rule-Breaking Behavior scale will not meet criteria for CD when evaluated clinically. The modest positive predictive value for the CBCL Rule-Breaking Behavior scale supports the need for clinical judgement in weighing the presence or absence of this diagnosis.
Our findings documenting the high efficiency of the CBCL Rule-Breaking Behavior scale in the identification of children of both sexes with a likely clinical diagnosis of CD has important clinical implications. The identification of children with CD can lead to targeted intervention efforts, such as individual or group parent behavioral therapy,30 aimed at mitigating the well-known complication of CD-associated risk for SUD that can benefit the affected youth, their family, and society at large. For youth with CD co-occurring with other psychiatric disorders such as ADHD and BP disorder, the CBCL Rule-Breaking Behavior scale can be an invaluable simple and low-cost tool to alert clinicians to youth who may be at very high risk to develop SUD due to the presence of CD.
Strengths of our study include the large sample size, equal number of participants of both sexes, structured diagnostic interviews, and raters who were blinded to subject ascertainment status and the CBCL t-scores. Our study also needs to be viewed with consideration of some methodologic limitations. Since the sample was largely referred and mostly Caucasian, our findings may not generalize to non-treatment seeking community samples and other ethnic groups. However, the finding do generalize to clinical samples including community and primary care settings. While we focused on the Rule Breaking Behavior scale because of its congruence with the DSM-5 definition of CD, we cannot rule out the possibility that other CBCL scales such as the Aggression scale may have diagnostic utility. Prior research, however, that has examined the Aggression scale and disruptive diagnoses including ODD, CD, and ADHD found high correspondence between the aggression scale and ODD.31,32 Additionally, we do not know whether the CBCL Rule Breaking Behavior scale holds differently for children with ADHD, BP-I, or no diagnosis (i.e. whether there is measurement invariance). Future studies would benefit from performing multi-group confirmatory analysis to evaluate this.
Despite these limitations, our work strongly suggests that modest elevations of the CBCL Rule-Breaking Behavior scale can very efficiently help identify children of both sexes who may have a clinical diagnosis of CD. Such children may benefit from appropriate early intervention strategies to avert the well-documented risks associated with CD.
Summary:
Since conduct disorder (CD) is associated with significant morbidity identification of CD could help guide early intervention strategies to improve prognosis. We evaluated whether the Rule Breaking scale from the parent reported Child Behavior Checklist could identify males and females with CD using a large sample of children (N=674) of both sexes with and without structured interview derived clinical diagnosis of CD. We found that a modestly elevated t-score on the Rule Breaking scale very efficiently identified children with CD. We recommend that clinicians utilize the CBCL Rule-Breaking Behavior scale as a low-cost tool to identify children who may have a clinical diagnosis of CD who might benefit from early referral for mental health services and treatment.
Acknowledgments
Compliance with Ethical Standards:
Funding: This work was supported by 5K12DA00357-17 to Dr. Yule and the MGH Pediatric Psychopharmacology Council. The data used in the current analysis was collected with support from the NIH grants R01HD036317 and R01MH050657 to Dr. Biederman, R01 DA012945 to Dr. Wilens, and 5 R01 MH066237-05 to Dr. Wozniak. The funding sources had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Amy Yule, MD: Dr. Amy Yule received grant support from the Massachusetts General Hospital Louis V. Gerstner III Research Scholar Award from 2014 to 2016. Dr. Yule is currently receiving funding through the American Academy of Child and Adolescent Psychiatry Physician Scientist Program in Substance Abuse 5K12DA000357-17. She was a consultant to the Phoenix House from 2015 to 2017 and is currently a consultant to the Gavin House (clinical services).
Timothy Wilens, MD: Dr. Timothy Wilens receives or has received grant support from the following sources: NIH(NIDA). Dr. Timothy Wilens is or has been a consultant for: Alcobra, Neurovance/Otsuka, and Ironshore. Dr. Timothy Wilens has a published book: Straight Talk About Psychiatric Medications for Kids (Guilford Press); and co/edited books ADHD in Adults and Children (Cambridge University Press), Massachusetts General Hospital Comprehensive Clinical Psychiatry (Elsevier) and Massachusetts General Hospital Psychopharmacology and Neurotherapeutics (Elsevier. Dr. Wilens is co/owner of a copyrighted diagnostic questionnaire (Before School Functioning Questionnaire). Dr. Wilens is Chief, Division of Child and Adolescent Psychiatry and (Co) Director of the Center for Addiction Medicine at Massachusetts General Hospital. He serves as a clinical consultant to the US National Football League (ERM Associates), U.S. Minor/Major League Baseball; Phoenix/Gavin House and Bay Cove Human Services.
Janet Wozniak, MD: Dr. Janet Wozniak received research support from PCORI in 2017–2018. She is the author of the book, “Is Your Child Bipolar” published May 2008, Bantam Books. In 2015–2017, her spouse, Dr. John Winkelman, received an honorarium from Otsuka; royalties from Cambridge University Press and UptoDate; consultation fees from Advance Medical, FlexPharma and Merck; and research support from UCB Pharma, NeuroMetrix, and Luitpold.
Stephen V. Faraone, PhD: Dr. Faraone received income, potential income, travel expenses continuing education support and/or research support from Lundbeck, KenPharm, Rhodes, Arbor, Ironshore, Shire, Akili Interactive Labs, CogCubed, Alcobra, VAYA, Sunovion, Genomind and NeuroLifeSciences in the past year. With his institution, he has US patent US20130217707 A1 for the use of sodium-hydrogen exchange inhibitors in the treatment of ADHD.
Joseph Biederman, MD: Dr. Joseph Biederman is currently receiving research support from the following sources: AACAP, Feinstein Institute for Medical Research, Food & Drug Administration, Genentech, Headspace Inc., Lundbeck AS, Neurocentria Inc., NIDA, Pfizer Pharmaceuticals, Roche TCRC Inc., Shire Pharmaceuticals Inc., Sunovion Pharmaceuticals Inc., and NIH. Dr. Biederman has a financial interest in Avekshan LLC, a company that develops treatments for attention deficit hyperactivity disorder (ADHD); his interests were reviewed and are managed by Massachusetts General Hospital and Partners HealthCare in accordance with their conflict of interest policies. Dr. Biederman’s program has received departmental royalties from a copyrighted rating scale used for ADHD diagnoses, paid by Bracket Global, Ingenix, Prophase, Shire, Sunovion, and Theravance; these royalties were paid to the Department of Psychiatry at MGH. In 2019, Dr. Biederman is a consultant for Akili, Jazz Pharma, and Shire. Through MGH corporate licensing, he has a US Patent (#14/027,676) for a non-stimulant treatment for ADHD, a US Patent (#10245271) on a treatment of impaired cognitive flexibility, and a patent pending (#6½33,686) on a method to prevent stimulant abuse. He received honoraria from the MGH Psychiatry Academy for tuition-funded CME courses. In 2018, Dr. Biederman was a consultant for Akili and Shire; he received honoraria from the MGH Psychiatry Academy for tuition-funded CME courses. In 2017, Dr. Biederman received research support from the Department of Defense and PamLab. He was a consultant for Aevi Genomics, Akili, Guidepoint, Ironshore, Medgenics, and Piper Jaffray; he was on the scientific advisory board for Alcobra and Shire; he received honoraria from the MGH Psychiatry Academy for tuition-funded CME courses
Footnotes
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Written informed consent was obtained from all individual participants’ parents in this study. Written assent was obtained from all children and adolescents included in this study.
Conflicts of Interest:
Maura Disalvo M.P.H., Rachael Lyons B.S., and K.Yvonne Woodworth B.A.: No conflicts of interest at this time.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-5. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 3.Border R, Corley RP, Brown SA, et al. Independent predictors of mortality in adolescents ascertained for conduct disorder and substance use problems, their siblings and community controls. Addiction. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Daignositic and Statistical Manual of Mental Disorders, Fifth Edition. 5 ed. Arlingotn, VA: American Psychiatric Association; 2013. [Google Scholar]
- 5.Nock MK, Kazdin AE, Hiripi E, Kessler RC. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the National Comorbidity Survey Replication. Psychol Med. 2006;36(5):699–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turgay A Treatment of comorbidity in conduct disorder with attention-deficit hyperactivity disorder (ADHD). Essent Psychopharmacol. 2005;6(5):277–290. [PubMed] [Google Scholar]
- 7.Biederman J, Faraone SV, Chu MP, Wozniak J. Further evidence of a bidirectional overlap between juvenile mania and conduct disorder in children. J Am Acad Child Adoles Psychiatry. 1999;38(4):468–476. [DOI] [PubMed] [Google Scholar]
- 8.Whitmore E, Mikulich S, Thompson L, Riggs P, Aarons G, Crowley T. Influences on adolescent substance dependence: conduct disorder, depression, attention deficit hyperactivity disorder, and gender. Drug and Alcohol Dependence. 1997;47:87–97. [DOI] [PubMed] [Google Scholar]
- 9.Groenman AP, Janssen TWP, Oosterlaan J. Childhood Psychiatric Disorders as Risk Factor for Subsequent Substance Abuse: A Meta-Analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(7):556–569. [DOI] [PubMed] [Google Scholar]
- 10.Wilens TE, Gignac M, Swezey A, Monuteaux MC, Biederman J. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry. 2006;45(4):408–414. [DOI] [PubMed] [Google Scholar]
- 11.Wilens TE, Biederman J, Kwon A, et al. Risk of substance use disorders in adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2004;43(11):1380–1386. [DOI] [PubMed] [Google Scholar]
- 12.Wilens T, Biederman J, Martelon M, et al. Further evidence for smoking and substance use disorders in youth with bipolar disorder and comorbid conduct disorder. Journal of Clinical Psychiatry. 2016;79:1420–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Achenbach TM, Howell CT, Quay HC, Conners CK. National survey of problems and competencies among four- to sixteen-year-olds: parents’ reports for normative and clinical samples. Monogr Soc Res Child Dev. 1991;56(3):1–131. [PubMed] [Google Scholar]
- 14.Biederman J, Faraone SV, Doyle A, et al. Convergence of the child behavior checklist with structured interview-based psychiatric diagnoses of ADHD children with and without comorbidity. The Journal of Child Psychology and Psychiatry. 1993;34:1241–1251. [DOI] [PubMed] [Google Scholar]
- 15.Biederman J, Monuteaux MC, Kendrick E, Klein KL, Faraone SV. The CBCL as a screen for psychiatric comorbidity in paediatric patients with ADHD. Arch Dis Child. 2005;90(10):1010–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gould MS, Bird H, Jaramillo BS. Correspondence between statistically derived behavior problem syndromes and child psychiatric diagnoses in a community sample. J Abnorm Child Psychol. 1993;21(3):287–313. [DOI] [PubMed] [Google Scholar]
- 17.Kasius MC, Ferdinand RF, van den Berg H, Verhulst FC. Associations between different diagnostic approaches for child and adolescent psychopathology. J Child Psychol Psychiatry. 1997;38(6):625–632. [DOI] [PubMed] [Google Scholar]
- 18.Edelbrock C, Costello AJ. Convergence between statistically derived behavior problem syndromes and child psychiatric diagnoses. Journal of Abnormal Child Psychology. 1988;16:219–231. [DOI] [PubMed] [Google Scholar]
- 19.Kazdin AE, Heidish IE. Convergence of clinically derived diagnoses and parent checklists among inpatient children. Journal of Abnormal Child Psychology. 1984;12:421–436. [DOI] [PubMed] [Google Scholar]
- 20.Freitag CM, Konrad K, Stadler C, et al. Conduct disorder in adolescent females: current state of research and study design of the FemNAT-CD consortium. Eur Child Adolesc Psychiatry. 2018;27(9):1077–1093. [DOI] [PubMed] [Google Scholar]
- 21.Biederman J, Faraone S, Milberger S, et al. A prospective 4-year follow-up study of attention-deficit hyperactivity and related disorders. Archives of General Psychiatry. 1996;53(5):437–446. [DOI] [PubMed] [Google Scholar]
- 22.Biederman J, Monuteaux M, Mick E, et al. Psychopathology in females with attention-deficit/hyperactivity disorder: A controlled, five-year prospective study. Biological Psychiatry. 2006;60(10):1098–1105. [DOI] [PubMed] [Google Scholar]
- 23.Wilens TE, Biederman J, Adamson JJ, et al. Further evidence of an association between adolescent bipolar disorder with smoking and substance use disorders: a controlled study. Drug Alcohol Depend. 2008;95(3):188–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wozniak J, Petty CR, Schreck M, Moses A, Faraone SV, Biederman J. High level of persistence of pediatric bipolar-I disorder from childhood onto adolescent years: a four year prospective longitudinal follow-up study. J Psychiatr Res. 2011;45(10):1273–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orvaschel H, Puig-Antich J. Schedule for Affective Disorders and Schizophrenia for School-Age Children: Epidemiologic Version. Fort Lauderdale, FL: Nova University; 1987. [Google Scholar]
- 26.Orvaschel H Schedule for Affective Disorder and Schizophrenia for School-Age Children Epidemiologic Version. . Ft. Lauderdale: Nova Southeastern University, Center for Psychological Studies; 1994. [Google Scholar]
- 27.Hollingshead AB. Four factor index of social status. New Haven, CT: Yale University Press; 1975. [Google Scholar]
- 28.Achenbach TM. Manual for the Child Behavior Checklist/ 4–18 and 1991 Profile. Burlington, VT: University of Vermont; 1991. [Google Scholar]
- 29.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. [DOI] [PubMed] [Google Scholar]
- 30.Kaminski JW, Claussen AH. Evidence Base Update for Psychosocial Treatments for Disruptive Behaviors in Children. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53. 2017;46(4):477–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Biederman J, Ball SW, Monuteaux MC, Kaiser R, Faraone SV. CBCL clinical scales discriminate ADHD youth with structured-interview derived diagnosis of oppositional defiant disorder (ODD). J Atten Disord. 2008;12(1):76–82. [DOI] [PubMed] [Google Scholar]
- 32.Hudziak JJ, Copeland W, Stanger C, Wadsworth M. Screening for DSM-IV externalizing disorders with the Child Behavior Checklist: a receiver-operating characteristic analysis. J Child Psychol Psychiatry. 2004;45(7):1299–1307. [DOI] [PubMed] [Google Scholar]