Abstract
Purpose
Chronic cough is a prevalent condition in the community and may pose considerable impairment to quality of life (QoL). However, its disease burden remains largely undefined in the general population. The present study investigated the relationship between chronic cough and health-related QoL in a Korean nationwide population database, with an emphasis on clinical conditions which may confound the impact of cough.
Methods
This study analyzed cross-sectional datasets of adults (aged ≥ 40 years) in the Korean National Health and Nutrition Examination Survey 2010–2016. Health-related QoL was assessed using the 3-level EuroQoL 5-dimension component (EQ-5D-3L) index score. The presence of chronic cough and other conditions were defined using structured questionnaires.
Results
The prevalence of chronic cough was 3.48% ± 0.17% among adults aged ≥ 40 years. The overall EQ-5D-3L index score was significantly lower in subjects with than without chronic cough (0.79 ± 0.01 vs. 0.86 ± 0.00, P < 0.001). In subgroup analyses by age and sex, chronic cough had a notably large impact on QoL in women aged ≥ 65 years (vs. those without chronic cough: 0.55 ± 0.04 vs. 0.70 ± 0.01, P < 0.001), although the mean difference in the scores exceeded the minimally important difference score of 0.05 in all subgroups. In multivariate analyses, chronic cough was significantly associated with QoL, independent of confounders including depression, arthritis, asthma, and chronic obstructive pulmonary disease. In dimension analyses, chronic cough was more associated with anxiety/depression, pain/discomfort, and usual activities than with self-care or mobility in the EQ-5D.
Conclusions
The present study demonstrated significant associations between chronic cough and health-related QoL in a nationwide large general adult population aged ≥ 40 years, which were independent of clinical confounders. The impact of chronic cough was greater in women aged ≥ 65 years. These findings indicate a considerable burden of chronic cough in the general population and warrant further investigations to assess the disease burden of chronic cough in a global scale.
Keywords: Cough, quality of life, population surveillance, nutrition surveys, burden of disease, cross-sectional studies, patient health questionnaire, epidemiology
INTRODUCTION
Cough is a physiological reflex to protect the lower airways from aspiration and irritation.1 However, cough is a common medical problem, being the single most frequent symptom for which patients seek medical care.2,3,4 Chronic cough, usually defined as lasting 8 or more weeks, is also highly prevalent, affecting about 10% of the general adult population,5 and is frequently difficult to treat.6,7,8,9 Chronic cough can have a significant effect on quality of life (QoL) in affected individuals in their physical, mental, and social aspects of life.10,11,12,13,14
The disease burden of chronic cough, however, remains largely undefined, presumably because it was perceived not as a clinical entity, but as a consequent symptom from other medical conditions.9 In previous studies of the global burden of disease, only whooping cough, but not chronic cough, was assessed.15 This is a major knowledge gap, given a recent paradigm shift in chronic cough (defining it as a clinical syndrome presenting as chronic cough)9,16,17 and also successful clinical trials with novel antitussives targeting cough reflex pathways.18
Unlike in clinic-based studies,10,11,12,13,14 however, there is only limited evidence for the impact of chronic cough in the general population. Investigation of randomly recruited persons from the general population would enable the comparative analyses of health-related QoL status across different medical conditions. In the literature, several general population studies have reported significant associations between chronic cough and health-related QoL19,20,21,22,23,24,25,26; however, they did not test the independency of such relationships from confounding medical conditions, such as asthma, chronic obstructive pulmonary disease (COPD), or depression. These are frequently comorbid in patients with chronic cough and may influence the QoL status.27,28,29 In addition, the relative impact of chronic cough, compared to other chronic conditions, has not been examined in the general population. Although the impact of cough has been assessed in subgroups of patients with respiratory conditions, such as chronic cough, asthma, bronchiectasis, and COPD, that study was performed on patients evaluated in a specialist cough clinic, with a relatively small number of patients, about 20–30, in each disease subgroup.29
The present study therefore investigated the relationship between chronic cough and health-related QoL in the Korean general adult population, with emphasis on chronic medical conditions which may confound the impact of chronic cough.
MATERIALS AND METHODS
Study population
The present study analyzed cross-sectional datasets of subjects in the Korean National Health and Nutrition Examination Survey (KNHANES) 2010–2016. The KNHANES is an annual nationwide survey of major health and disease information in the Korean general population. The details of the KNHANES are described online at https://knhanes.cdc.go.kr/knhanes/eng/. Of the 56,632 subjects originally enrolled in the KNHANES 2010–2016, 30,021 aged ≥ 40 years, who responded to the EuroQoL questionnaire, a generic tool for measuring health-related QoL, and to a question on the presence of chronic cough (“Have you had cough on most days for 3 months or more during the past year?”) were included in the present study. Only adults aged ≥ 40 years were included as the question on chronic cough was not administered to younger subjects in the KNHANES 2010–2016. The study protocol was approved by the Institutional Review Board at the Korea Centers for Disease Control and Prevention. All participants were fully informed of the protocol and provided written informed consent.
Parameters
Health-related QoL was assessed by measuring the 3-level EuroQoL 5-dimension component (EQ-5D-3L) index score. This score was calculated from subject ratings of 5 dimensions: mobility, self-care, usual activities (work, study, housework, family and leisure activities), pain/discomfort, and anxiety/depression (https://euroqol.org/). Each dimension has 3 levels of response (no problems, some problems, and extreme problems/unable to). The index scores range from less than 0 (where 0 is a health state equivalent to death; and negative values indicate a health state worse than death) to 1 (perfect health). The minimally important difference (MID) in the EQ-5D-3L index score was defined as 0.05.30
QoL status in subjects with chronic cough was compared to that in subjects diagnosed with other common chronic physical and mental conditions, including asthma, COPD, allergic rhinitis, angina/myocardial infarction (MI), stroke, hypertension, diabetes mellitus, dyslipidemia, arthritis (osteoarthritis and rheumatoid arthritis), and depression. They were selected on the basis of the literature about their impact on QoL or frequent overlaps with chronic cough.27,28,31,32 The presence of each of these chronic conditions was defined using the combination of physician diagnostic history and current disease status (i.e., “Have you ever been diagnosed with [a specific disease] by a physician?”, followed by “Do you still have [that specific disease]?”). Because allergic rhinitis was assessed only in the KNHANES 2013–2015, it was included only in a sensitivity analysis.
Demographic parameters analyzed in this study included subject age, sex, smoking status, body mass index (BMI), educational level, household income, and occupation. Smoking status was classified as “never” for participants who had never smoked or had smoked fewer than 100 cigarettes; as “former” for those who had stopped smoking for at least 6 months, but had smoked more than 100 cigarettes; and as “current” for those who smoked at the time of the study or had quit within the past 6 months. BMI was calculated as body weight divided by height squared (kg/m2). Occupation was categorized using the Korean Standard Classification of Occupation, with managers, professionals, clerks, service/sales workers, unemployed individuals, retired persons, and students and housewives classified as “white collar”; and with workers in agriculture, forestry, fisheries, craft and related trades, plant and machine operators, assemblers, and simple laborers classified as “blue collar.”33 Household income was categorized as low or high based on the fiftieth percentile in each survey population.
Statistical analysis
To obtain unbiased national estimates representing the general Korean adult population, the KNHANES sampling weights were adjusted to account for a complex sample design. Sampling was applied to strata at the level of primary sampling units and households. Missing rates for variables were generally ≤ 5%. Missing data were assumed to be missing completely at random and were regarded as valid in all analyses.
Categorical variables are summarized as weighted percentages ± standard errors (SEs) and continuous variables as weighted means ± SEs. Subjects with and without chronic cough in each EQ-5D-3L dimension response were compared by weighted χ2 tests with design-based F statistics. The relationship between chronic cough (vs. no chronic cough) and EQ-5D-3L index score was determined by linear regression analyses. Demographic and clinical parameters associated with chronic cough or EQ-5D-3L index score in univariate analyses (with P values < 0.05) were included in multivariate linear regression analyses. Determinants of each EQ-5D dimension value were analyzed by logistic regression; in each dimension, level 1 (no problems) served as the reference, and level 2 (some problems) and level 3 (extreme problems) were merged to “some or extreme problem.” Interactions in multivariate regression analyses were considered between chronic cough and chronic airway diseases (asthma, COPD, and allergic rhinitis). Sensitivity analyses were also considered to explore the confounding effects of major confounders. Two-sided P values < 0.05 were considered statistically significant. All statistical analyses were performed using Stata 15.1 statistical software (Stata Corp., College Station, TX, USA).
RESULTS
Baseline characteristics
The weighted prevalence of chronic cough among the study subjects (aged ≥ 40 years) was 3.48% ± 0.17%. The mean duration of cough among subjects with chronic cough was 7.76 ± 0.46 years, and the proportion of subjects with cough duration ≤ 1 year was 32.48% ± 2.09% among those with chronic cough (Supplementary Fig. S1). Baseline characteristics are summarized in Table 1. Compared to subjects without chronic cough, those with chronic cough were significantly older and more likely to be men, current smokers, and to have asthma, COPD, allergic rhinitis, arthritis and depression.
Table 1. Weighted characteristics of the study subjects (aged ≥ 40 years) in the KNHANES 2010–2016.
| Characteristics | No chronic cough | Chronic cough | P value | |
|---|---|---|---|---|
| Prevalence (%) | 96.52 ± 0.17 | 3.48 ± 0.17 | - | |
| Age (yr) | 55.89 ± 0.12 | 57.27 ± 0.55 | 0.012 | |
| Cough duration (yr) | - | 7.76 ± 0.46 | - | |
| Men (%) | 47.64 ± 0.36 | 60.80 ± 2.22 | < 0.001 | |
| Smoking history (%) | < 0.001 | |||
| Never | 56.26 ± 0.40 | 39.43 ± 2.26 | ||
| Former | 23.66 ± 0.35 | 17.56 ± 1.67 | ||
| Current | 20.08 ± 0.37 | 43.01 ± 2.40 | ||
| BMI category (%) | 0.350 | |||
| < 18.5 kg/m2 | 1.62 ± 0.11 | 1.97 ± 0.51 | ||
| 18.5–24.9 kg/m2 | 60.71 ± 0.42 | 57.10 ± 2.09 | ||
| 25.0–29.9 kg/m2 | 33.29 ± 0.41 | 36.40 ± 2.02 | ||
| ≥ 30 kg/m2 | 4.38 ± 0.18 | 4.52 ± 0.94 | ||
| Educational level (%) | 0.005 | |||
| Elementary school | 26.46 ± 0.50 | 32.78 ± 1.99 | ||
| Middle school | 14.5 ± 0.32 | 16.13 ± 1.62 | ||
| High school | 33.93 ± 0.47 | 29.97 ± 2.17 | ||
| University | 25.11 ± 0.58 | 21.11 ± 1.90 | ||
| Low household income (%) | 50.08 ± 0.62 | 53.45 ± 2.30 | 0.152 | |
| Blue collar occupation (%) | 31.48 ± 0.59 | 33.22 ± 2.29 | 0.448 | |
| Medical conditions (%) | ||||
| Asthma | 1.41 ± 0.10 | 11.74 ± 1.39 | < 0.001 | |
| COPD* | 0.19 ± 0.04 | 3.04 ± 0.71 | < 0.001 | |
| Allergic rhinitis† | 8.49 ± 0.30 | 13.16 ± 1.76 | 0.009 | |
| Diabetes mellitus | 9.37 ± 0.24 | 11.94 ± 1.37 | 0.109 | |
| Hypertension | 25.66 ± 0.41 | 26.27 ± 1.96 | 0.769 | |
| Dyslipidemia | 12.22 ± 0.28 | 11.81 ± 1.58 | 0.771 | |
| Angina/MI | 2.26 ± 0.12 | 3.25 ± 0.78 | 0.132 | |
| Stroke | 3.48 ± 1.78 | 2.92 ± 0.97 | 0.590 | |
| Arthritis | 13.45 ± 0.31 | 18.6 ± 1.72 | < 0.001 | |
| Depression | 2.46 ± 0.14 | 4.85 ± 0.91 | 0.003 | |
Categorical variables are summarized as weighted percentages ± SEs and continuous variables as weighted means ± SEs.
KNHANES, Korean National Health and Nutrition Examination Survey; BMI, body mass index; COPD, chronic obstructive pulmonary disease; MI, myocardial infarction; SE, standard error.
*A COPD patient was defined as one who required current treatment; other medical conditions in this table indicate a diagnostic history and current disease; †Allergic rhinitis was assessed only in the KNHANES 2013–2015 study.
Chronic cough and health-related QoL
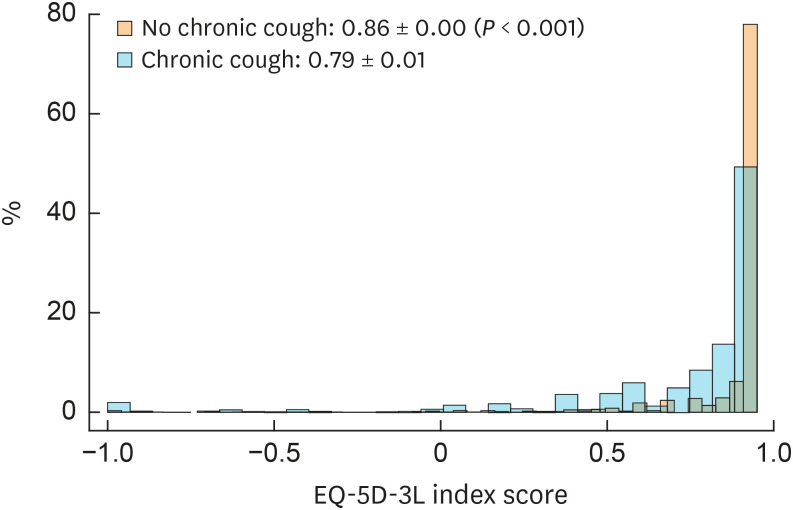
The overall EQ-5D-3L index score was significantly lower in subjects with than without chronic cough (0.79 ± 0.01 vs. 0.86 ± 0.00, P < 0.001; Fig. 1), with its exceeding the defined MID score of 0.05.30 The EQ-5D-3L index score did not differ by cough duration (≤ 1 year: 0.80 ± 0.02 vs. > 1 year: 0.79 ± 0.02; Supplementary Fig. S2). The score also did not differ by the presence of chronic phlegm within patients with chronic cough (chronic cough without phlegm: 0.80 ± 0.02 vs. chronic cough with phlegm: 0.79 ± 0.02; Supplementary Table S1).
Fig. 1. Histograms of EQ-5D-3L index scores in subjects with and without chronic cough (aged ≥ 40 years) in the KNHANES 2010–2016.
EQ-5D-3L, 3-level EuroQoL 5-dimension component; KNHANES, Korean National Health and Nutrition Examination Survey.
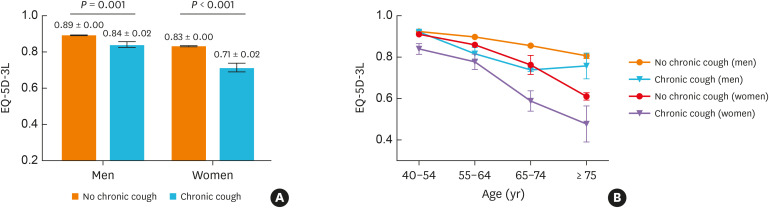
Subgroup analyses showed that EQ-5D-3L index scores were significantly lower in both men and women with than without chronic cough, although the mean difference in score was greater for women (0.71 ± 0.02 vs. 0.83 ± 0.00; P < 0.001) than for men (0.84 ± 0.02 vs. 0.89 ± 0.00; P = 0.001) (Fig. 2A). When further sub-grouped by age, the mean difference in score was greater for elderly women (aged ≥ 65 years) than other age and sex subgroups (Fig. 2B). Among elderly women, the mean score difference was 0.15 (chronic cough: 0.55 ± 0.04 vs. no chronic cough: 0.70 ± 0.01; P < 0.001).
Fig. 2. EuroQoL EQ-5D-3L index scores in subjects according to the presence of chronic cough (aged ≥ 40 years) classified by (A) gender and (B) sex-age subgroups in the KNHANES 2010–2016. The scores are presented as weighted means ± standard errors.
EQ-5D-3L, 3-level EuroQoL 5-dimension component; KNHANES, Korean National Health and Nutrition Examination Survey.
Given the greater impairment in QoL score in elderly women with chronic cough than in elderly men with chronic cough, their baseline characteristics were compared (Supplementary Table S2). Compared to elderly men with chronic cough, elderly women with chronic cough had significantly lower frequencies of smoking history and COPD, but had higher BMI and more arthritis and depression.
Multivariate analyses of the relationships between chronic cough and EQ-5D-3L index score
Univariate linear regression analyses identified several demographic and clinical parameters as being significantly associated with EQ-5D-3L index scores, including subject age, sex, smoking history, BMI category, level of education, household income, occupation, depression, asthma, COPD, and chronic cough (Supplementary Table S3).
In multivariate linear regression analyses adjusted for confounders (please see Methods for confounder selection), chronic cough was significantly associated with EQ-5D-3L index score, independently of demographic factors (correlation coefficient, −0.058; 95% confidence interval [95% CI], −0.082 to −0.034; P < 0.001; model 1 in Table 2). In additional adjustment for comorbidities, including arthritis, depression, asthma, or COPD, the relationship between chronic cough and EQ-5D-3L index score remained significant (correlation coefficient, −0.037; 95% CI, −0.059 to −0.015; P = 0.001; adjusted models 2 in Table 2). In a sensitivity analysis with further adjustment for allergic rhinitis to model 2 (in the KNHANES 2013–2015 population), the impact of chronic cough on QoL remained significant (correlation coefficient, −0.041; 95% CI, −0.066 to −0.017; P = 0.001; Table not shown). In separate regression analyses, there were no significant interactions between chronic cough and airway diseases (asthma, COPD, or allergic rhinitis) (all P > 0.05; Table not shown).
Table 2. Multivariate linear regression analyses of factors associated with EQ-5D-3L index scores in the KNHANES 2010–2016.
| For EQ-5D-3L index score | Model 1* | Model 2† | |||
|---|---|---|---|---|---|
| Coefficient (95% CI) | P value | Coefficient (95% CI) | P value | ||
| Age (yr) | −0.004 (−0.004 to −0.003) | < 0.001 | −0.002 (−0.003 to −0.002) | < 0.001 | |
| Woman (vs. man) | −0.055 (−0.066 to −0.043) | < 0.001 | −0.031 (−0.043 to −0.021) | < 0.001 | |
| Smoking history | |||||
| Never smoker | Reference | Reference | |||
| Ex-smoker | −0.016 (−0.027 to −0.004) | 0.010 | −0.012 (−0.023 to −0.000) | 0.041 | |
| Current smoker | −0.037 (−0.050 to −0.025) | < 0.001 | −0.034 (−0.045 to −0.022) | < 0.001 | |
| BMI category (kg/m2) | |||||
| < 18.5 | −0.032 (−0.061 to −0.003) | 0.031 | −0.035 (−0.064 to −0.007) | 0.015 | |
| 18.5–24.9 | Reference | Reference | |||
| 25.0–29.9 | −0.014 (−0.020 to −0.007) | < 0.001 | −0.003 (−0.009 to 0.003) | 0.332 | |
| ≥ 30 | −0.062 (−0.082 to −0.042) | < 0.001 | −0.040 (−0.058 to −0.022) | < 0.001 | |
| Educational level | |||||
| Elementary school | Reference | Reference | |||
| Middle school | 0.074 (0.062 to 0.086) | < 0.001 | 0.063 (0.052 to 0.075) | < 0.001 | |
| High school | 0.093 (0.081 to 0.105) | < 0.001 | 0.076 (0.065 to 0.086) | < 0.001 | |
| University | 0.098 (0.086 to 0.110) | < 0.001 | 0.078 (0.067 to 0.089) | < 0.001 | |
| Low household income (vs. high household income) | −0.035 (−0.042 to −0.029) | < 0.001 | −0.031 (−0.037 to −0.025) | < 0.001 | |
| Blue collar occupation (vs. white collar occupation) | 0.031 (0.023 to 0.038) | < 0.001 | 0.027 (0.020 to 0.034) | < 0.001 | |
| Arthritis (vs. no arthritis) | - | - | −0.130 (−0.145 to −0.116) | < 0.001 | |
| Depression (vs. no depression) | - | - | −0.182 (−0.222 to −0.142) | < 0.001 | |
| Asthma (vs. no asthma) | - | - | −0.076 (−0.120 to −0.032) | 0.001 | |
| COPD‡ (vs. no COPD) | - | - | −0.030 (−0.116 to 0.056) | 0.497 | |
| Diabetes mellitus (vs. no diabetes mellitus) | - | - | −0.025 (−0.041 to −0.010) | 0.001 | |
| Hypertension (vs. no hypertension) | - | - | −0.013 (−0.022 to −0.003) | 0.011 | |
| Dyslipidemia (vs. no dyslipidemia) | - | - | −0.011 (−0.025 to 0.002) | 0.089 | |
| Angina/MI (vs. no angina/MI) | - | - | −0.056 (−0.086 to −0.027) | < 0.001 | |
| Stroke (vs. no stroke) | - | - | −0.131 (−0.182 to −0.080) | < 0.001 | |
| Chronic cough (vs. no chronic cough) | −0.058 (−0.082 to −0.034) | < 0.001 | −0.037 (−0.059 to −0.015) | 0.001 | |
EQ-5D-3L, 3-level EuroQoL 5-dimension component; KNHANES, Korean National Health and Nutrition Examination Survey; 95% CI, 95% confidence interval; BMI, body mass index; COPD, chronic obstructive pulmonary disease; MI, myocardial infarction.
*Adjusted for age, sex, smoking, BMI category, education level, household income, and occupation; †Adjusted for age, sex, smoking, BMI category, education level, household income, occupation, arthritis, depression, asthma, COPD, hypertension, dyslipidemia, angina/MI, and stroke; ‡COPD requiring current treatment.
Given the frequent overlaps of depression with chronic cough and its major impact on QoL,28 we conducted sensitivity analysis excluding subjects with depression or arthritis. However, the overall findings were in line with those of the primary analyses; the EQ-5D-3L index score was similarly lower in subjects with chronic cough than in those without (Supplementary Fig. S3A and B), and the impact of chronic cough on QoL remained significant in multivariate analyses, independently of confounders (Supplementary Table S4).
Chronic cough and EQ-5D dimensions
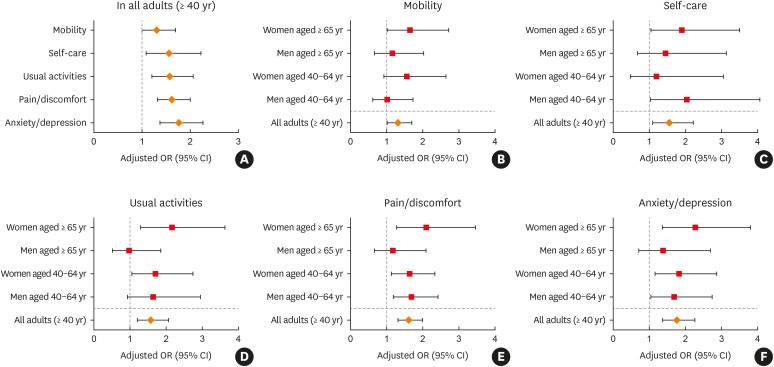
Dimension analysis found that subjects with chronic cough scored significantly lower on all 5 dimensions of the EQ-5D. However, design-based F values were higher for anxiety/depression, usual activities, and pain/discomfort than for mobility and self-care (Table 3). In multivariate logistic regression analyses adjusted for demographic and clinical confounders, chronic cough was significantly associated with all 5 dimensions, but more strongly with anxiety/depression (odds ratio [OR], 1.77; 95% CI, 1.38–2.27; P < 0.001), pain/discomfort (OR, 1.62; 95% CI, 1.32–2.00; P < 0.001), and usual activities (OR, 1.58; 95% CI, 1.21–2.07; P = 0.001) (Fig. 3A). The associations were weaker, or just marginal for self-care (OR, 1.56; 95% CI, 1.09–2.23; P = 0.016), or mobility (OR, 1.31; 95% CI, 1.01–1.70; P = 0.042) (Fig. 3A).
Table 3. Responses to the EQ-5D-3L health-related quality of life questionnaire and index scores in subjects with and without chronic cough (aged ≥ 40 years) in the KNHANES 2010–2016.
| Dimension | No chronic cough | Chronic cough | Design-based F value | P value | |
|---|---|---|---|---|---|
| Mobility | 20.36* | < 0.001* | |||
| No problems (%) | 84.40 ± 0.35 | 76.37 ± 1.98 | |||
| Some problems (%) | 15.09 ± 0.34 | 21.39 ± 1.91 | |||
| Extreme problems (%) | 0.51 ± 0.06 | 2.23 ± 0.66 | |||
| Self-care | 12.98* | < 0.001* | |||
| No problems (%) | 96.34 ± 0.16 | 92.13 ± 1.11 | |||
| Some problems (%) | 3.54 ± 0.16 | 7.48 ± 1.08 | |||
| Extreme problems (%) | 0.13 ± 0.03 | 0.38 ± 0.28 | |||
| Usual activities | 26.20* | < 0.001* | |||
| No problems (%) | 91.12 ± 0.27 | 82.36 ± 1.65 | |||
| Some problems (%) | 8.26 ± 0.26 | 16.53 ± 1.62 | |||
| Extreme problems (%) | 0.62 ± 0.06 | 1.12 ± 0.41 | |||
| Pain/discomfort | 25.06* | < 0.001* | |||
| No problems (%) | 75.97 ± 0.38 | 63.40 ± 2.14 | |||
| Some problems (%) | 21.83 ± 0.36 | 31.63 ± 2.10 | |||
| Extreme problems (%) | 2.19 ± 0.12 | 4.97 ± 0.92 | |||
| Anxiety/depression | 28.29* | < 0.001* | |||
| No problems (%) | 89.41 ± 0.27 | 79.83 ± 1.76 | |||
| Some problems (%) | 9.89 ± 0.25 | 18.95 ± 1.73 | |||
| Extreme problems (%) | 0.69 ± 0.07 | 1.22 ± 0.39 | |||
| EQ-5D-3L index score | 0.86 ± 0.00 | 0.79 ± 0.01 | - | < 0.001 | |
Categorical variables are summarized as weighted percentages ± standard errors (SEs) and continuous variables as weighted means ± SEs.
EQ-5D-3L, 3-level EuroQoL 5-dimension component; KNHANES, Korean National Health and Nutrition Examination Survey; SE, standard error.
*Calculated by χ2 tests.
Fig. 3. Associations between chronic cough and each EQ-5D dimension score in the KNHANES 2010–2016. (A) Domain scores in all adults (≥ 40 years), and (B-F) each domain score according to age and sex. In each dimension, level 1 (no problems) served as the reference, and level 2 (some problems) and level 3 (extreme problems) were merged to “some or extreme problem.” ORs were calculated from multivariate logistic regressions adjusted for age, sex, smoking, body mass index, education level, household income, occupation, arthritis, depression, asthma, chronic obstructive pulmonary disease, hypertension, dyslipidemia, angina/myocardial infarction, and stroke.
EQ-5D, EuroQoL 5-dimension component; KNHANES, Korean National Health and Nutrition Examination Survey; OR, odds ratio; CI, confidence interval.
In subgroup analyses by age and sex, F values were generally greater in all 5 dimensions among women than among men (Supplementary Table S5). Multivariate logistic regression confirmed this, but particularly elderly women (aged ≥ 65 years) had significant impairments across all 5 dimensions, albeit having less problems with mobility and self-care (Fig. 3B-F). However, women aged 40–64 years showed significant problems with anxiety/depression, pain/discomfort, and usual activities, but not with self-care and mobility dimensions (Fig. 3B-F).
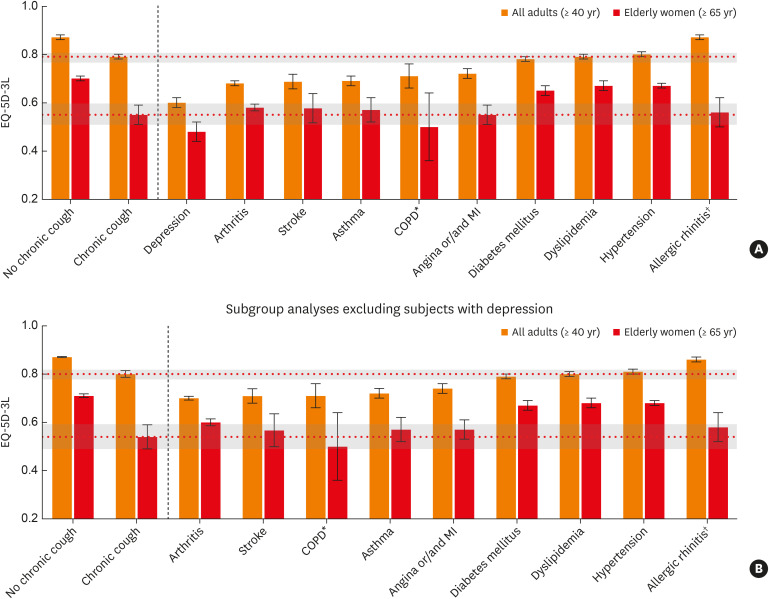
EQ-5D-3L index scores of subjects with different chronic medical conditions
For comparison, EQ-5D-3L index scores were assessed across different chronic medical conditions. In all subjects, the EQ-5D-3L index score of chronic cough (0.79 ± 0.01) was similar to those of diabetes mellitus, dyslipidemia, and hypertension, but was higher than those for depression, arthritis, asthma, COPD, and angina/MI (Fig. 4A). Because the EQ-5D-3L index score for chronic cough was lower in women aged ≥ 65 years than in the other subgroups (0.55 ± 0.04), EQ-5D-3L index scores for other chronic conditions were further assessed in this subgroup (Fig. 4A); comparable EQ-5D-3L index scores were observed in women aged ≥ 65 years with arthritis, stroke, asthma, angina/MI, and allergic rhinitis. Overall, depression showed the lowest QoL score among the chronic conditions examined. In subgroup analyses excluding subjects with depression, the relative impact of chronic cough on QoL was similar to that in the entire study population (Fig. 4B).
Fig. 4. EQ-5D-3L index scores according to the presence of chronic diseases among subjects in all adult subjects (aged ≥ 40 years) and elderly women (aged ≥ 65 years) in the KNHANES 2010–2016. (A) Entire sample analyses and (B) subgroup analyses excluding subjects with depression. Horizontal dotted lines and grey boxes indicate the mean score and standard error margins of the EQ-5D-3L index score in subjects with chronic cough. Vertical dotted lines are positioned to differentiate chronic cough from other chronic conditions. Error bars indicate standard error in the EQ-5D-3L index scores in each chronic condition. Conditions other than chronic cough were sorted by EQ-5D-3L index score (low to high) in all adult dataset (≥ 65 years).
EQ-5D, EuroQoL 5-dimension component; KNHANES, Korean National Health and Nutrition Examination Survey; COPD, chronic obstructive pulmonary disease.
*COPD was defined as a condition requiring current treatment; other medical conditions in this figure indicate a diagnostic history and current disease. †Allergic rhinitis was assessed only in the KNHANES 2013–2015 study.
DISCUSSION
This general population analysis found that chronic cough is significantly associated with health-related QoL among adults aged ≥ 40 years, independent of demographic and clinical confounders including depression, arthritis, asthma, and COPD. The mean difference in the EQ-5D-3L index score exceeded the defined MID score of 0.0530 in all age/sex subgroups examined (Fig. 2B). However, chronic cough had a notable impact on QoL in women aged ≥ 65 years (vs. those without chronic cough: 0.55 ± 0.04 vs. 0.70 ± 0.01), indicating that this is the most susceptible age/sex subgroup warranting active interventions for the treatment of chronic cough.
Health-related QoL status is influenced by a variety of demographic and clinical factors, and it may become worse with aging, particularly among women,31,34 as also shown in the present KNHANES analyses. Furthermore, chronic cough is frequently comorbid with respiratory and non-respiratory diseases,27,35 making the cough-related QoL data difficult to interpret, although we think that comorbidity is part of a disease, either in terms of the pathophysiology or causal relationships. Depression is frequently associated with chronic cough12,28,36,37; however, depression in patients with chronic cough is likely to be a consequence of cough, because it significantly improves with cough resolution.28 However, depression is considered as a major confounder in the present study, because it is a part of EQ-5D dimension score and also its implication may be different from that in specialist cough clinics. Therefore, we examined the associations between chronic cough and QoL in several ways, including multivariate analyses, dimension analyses, and sensitivity analyses excluding subjects with depression.
Our findings may not be surprising, as chronic cough was significantly associated with impaired health-related QoL in several general population studies.19,20,21,22,23,24,26 However, no previous studies in general populations had adjusted for clinical confounding factors, such as depression, asthma, and COPD. As discussed above, depression is a major confounder to be considered when testing the relationships between chronic cough and QoL using generic health-related QoL measures. Therefore, the results of this study are a valuable addition to the literature of the subject, confirming the impact of chronic cough on health-related QoL.
In this study, chronic cough had a greater impact on health-related QoL in women aged ≥ 65 years than in the other age and sex subgroups. In normative studies, it is known that health-related QoL is generally worse in elderly women.34 However, the mean EQ-5D-3L index score was particularly lower in elderly women with than without chronic cough, or than men with, showing the largest mean difference in the score (0.15) (Fig. 2). In addition, the EQ-5D-3L index scores in these subjects with chronic cough were comparable to those in subjects with other major chronic conditions, but only second to depression among chronic medical conditions examined in this study. This greater impact of chronic cough in older women may be one of the major reasons for an older female predominance commonly found in cough clinics in many countries.38,39 Heightened cough sensitivity in women may underlie poorer cough-related QoL or more presentation of women to the specialist cough clinics.40 In tussigen inhalation cough challenge studies, there is a consistently enhanced cough sensitivity in women than in men.38,39,41,42 In our recent clinic-based study of Korean patients with chronic cough, the number of cough triggers and cough-related laryngeal sensations, as measured using the Cough Hypersensitivity Questionnaire (CHQ), was significantly higher in women than in men, and the CHQ score significantly correlated with poorer cough-specific QoL.43 In the KNHANES 2010–2016, there were no items specific for cough sensitivity because the survey focuses on the general aspects of health and diseases. However, compared to men counterparts, elderly women with chronic cough more frequently had depression and arthritis, but not respiratory comorbidities, such as asthma, COPD, or allergic rhinitis (Supplementary Table S2), indicating that the impact of chronic cough on QoL was less likely dependent on these respiratory diseases.
This age/sex-specific finding in the QoL may also be attributed to urinary incontinence, which is a more frequent complication of coughing in older women, as previously suggested by a specialist clinic-based study in the USA.44 However, urinary incontinence was not included in the KNHANES 2010–2016 study protocols, and thus its impact could not be directly assessed in this study. Although 3 dimensions of the EQ-5D-3L usual activities, anxiety/depression, and pain/discomfort were more affected by chronic cough in this subgroup, a previous study found that none of these dimensions were specifically associated with urinary incontinence.45
Unlike the female predominance observed in chronic cough patients visiting specialist clinics,38 chronic cough is reportedly more prevalent in men than in women in many general population studies,46 including the present analysis. As none of previous general population studies assess cough-related healthcare utilization and reasons for seeking (or not seeking) medical care for cough, no conclusion can be drawn now. However, the QoL status related to chronic cough was worse in women than in men, suggesting that the impact on QoL may be a factor driving the healthcare visit in subjects with chronic cough. We propose that further population-based studies should address major issues in cough epidemiology,46 including the sex disparity in patient profiles between the community and clinics.
The present analyses need to be discussed with regard to the population norms of the EQ-5D index score. The normative values for Korea, which were obtained from face-to-face interviews on a random sample of the South Korean residential registry in 2007, are 0.960 (in 45–54 years), 0.909 (in 55–64 years), 0.888 (in 65–74 years), and 0.958 (in total [18–74 years]; the normative values in aged ≥75 years were not reported).34 In the present analyses of the KNHANES 2010–2016 dataset, the scores in subjects with chronic cough were 0.88 ± 0.01 (in 40–54 years), 0.76 ± 0.04 (in 55–64 years), and 0.68 ± 0.04 (in aged 65–74 years), which are considerably lower than the normative values.34
In dimension analyses, chronic cough was particularly more associated with anxiety/depression, pain/discomfort and usual activities than self-care or mobility (Fig. 3). Although 5 dimensions are rather categorical than indicative of a specific problem, our findings are in line with those of previous studies on QoL in patients with chronic cough. In 2 landmark studies in constructing cough-specific QoL questionnaires, chronic cough was associated with diverse adverse outcomes, encompassing physical, mental, and psychosocial domains.10,11 In the study by French et al.,10 a substantial proportion of adverse effects was explained by cough-causing exhaustion, the need for reassurance that nothing is serious, the inability to go to the movies, and spouses not being able to tolerate cough. Also, in before-and-after treatment data, psychosocial dysfunction was more significantly associated with cough than physical impairment.10
Several limitations need to be considered while interpreting our findings. First, the observational nature of this cross-sectional study limits causal inference between chronic cough and QoL impairment. Secondly, chronic cough was defined by period prevalence, not by point prevalence, which is prone to recall bias. In addition, it used 3 months as the cutoff, which is longer than the cutoff recommended in the clinical guidelines (8 weeks).6,7,8 However, it is the most common definition used in epidemiological studies.46 The point prevalence of chronic cough using 8 weeks as the cutoff duration (current chronic cough) was measured only in the KNHANES 2010–2012 surveys47; of note, the EQ-5D-3L index score in subjects with current chronic cough in the 2010–2012 study population is 0.79 ± 0.02 (vs. 0.86 ± 0.00 in subjects without current cough; Supplementary Table S6), which is consistent with the main findings using the period prevalence definition (0.79 ± 0.01 vs. 0.86 ± 0.00; Fig. 1). Thirdly, the cough duration in subjects with chronic cough was 7.76 ± 0.46 years, which is relatively longer than those reported in clinic-based studies in Korea.39,43 Thus, the present study population may represent more persistent or treatment-refractory cough patients, and the impact of chronic cough might have been overestimated, even though they were recruited by random sampling of nationwide populations. However, the EQ-5D-3L index score did not differ between patients with chronic cough ≤ 1 year and > 1 year (0.80 ± 0.02 vs. 0.79 ± 0.02; Supplementary Fig. S2). In our view, cough duration is difficult to define particularly when self-reported, as cough frequently waxes and wanes over time within a single patient rather than persists continuously, which is more problematic to measure in patients with cough persisting for longer than 1 year. Further studies are warranted to validate existing tools to capture chronic cough in large population-based epidemiological studies. Fourthly, the present analyses were confined to adults aged ≥ 40 years, and thus the impact of cough in Korean younger adults remains unclear. Fifthly, the presence of chronic diseases, such as asthma, COPD, and depression, was defined by a self-reported history of physician diagnosis combined with current disease activity. They are therefore prone to recall and misclassification biases, with no ability to differentiate among degrees of clinical severity. Finally, the definition of chronic cough was not based on a physician diagnosis, unlike those of chronic medical conditions compared. Therefore, our comparative analyses (Fig. 3) have an explorative nature. However, the lack of a physician diagnosis of chronic cough in study protocols is inherent to current diagnostic classification systems. The 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) does not include a diagnostic code for chronic cough, with R05 used to classify “cough” as a symptom. Chronic cough, however, represents a pathophysiologic state that deviates from the protective role of cough, suggesting that chronic cough should be recognized as a disease entity in the ICD system.9,48,49
This study has strength that it has demonstrated significant associations between chronic cough and health-related QoL in a nationwide large general adult population (aged ≥ 40 years), which were independent of clinical confounding conditions. The greatest impact of chronic cough on QoL was observed in women aged ≥ 65 years, suggesting that this age/sex subgroup is the most susceptible to chronic cough and may warrant active intervention. These findings suggest that there is a considerable burden of chronic cough in the general population and warrant further investigations to precisely assess the disease burden of chronic cough in a global scale.
Footnotes
Disclosure: There are no financial or other issues that might lead to conflict of interest.
SUPPLEMENTARY MATERIALS
Weighted prevalence and EQ-5D-3L index score of chronic cough and chronic phlegm
Comparison of weighted demographic and clinical parameters according to sex and chronic cough in the elderly (age ≥ 65 years)
Univariate linear regression analyses of factors associated with EQ-5D-3L index scores in the KNHANES 2010–2016
Multivariate linear regression analyses of factors associated with EQ-5D-3L index scores among subjects without depression or arthritis in the KNHANES 2010–2016
Responses to the EQ-5D-3L questionnaire in subjects with and without chronic cough, according to age and sex
Prevalence and EQ-5D-3L index score of current chronic and non-chronic cough in the KNHANES 2010–2012 surveys
Histogram of cough duration in adults with chronic cough (aged ≥ 40 years).
EuroQoL EQ-5D-3L index scores according to cough duration.
EuroQoL EQ-5D-3L index scores in subjects without depression or arthritis, classified by (A) sex and (B, C) age and gender subgroups. The scores are presented as weighted means ± standard errors.
References
- 1.Canning BJ, Chang AB, Bolser DC, Smith JA, Mazzone SB, McGarvey L, et al. Anatomy and neurophysiology of cough: CHEST Guideline and Expert Panel report. Chest. 2014;146:1633–1648. doi: 10.1378/chest.14-1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schappert SM. National Ambulatory Medical Care Survey: 1991 summary. Adv Data. 1993;29:1–16. [PubMed] [Google Scholar]
- 3.Morice AH. Epidemiology of cough. Pulm Pharmacol Ther. 2002;15:253–259. doi: 10.1006/pupt.2002.0352. [DOI] [PubMed] [Google Scholar]
- 4.Cho SH, Lin HC, Ghoshal AG, Bin Abdul Muttalif AR, Thanaviratananich S, Bagga S, et al. Respiratory disease in the Asia-Pacific region: cough as a key symptom. Allergy Asthma Proc. 2016;37:131–140. doi: 10.2500/aap.2016.37.3925. [DOI] [PubMed] [Google Scholar]
- 5.Song WJ, Chang YS, Faruqi S, Kim JY, Kang MG, Kim S, et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J. 2015;45:1479–1481. doi: 10.1183/09031936.00218714. [DOI] [PubMed] [Google Scholar]
- 6.Morice AH, Fontana GA, Sovijarvi AR, Pistolesi M, Chung KF, Widdicombe J, et al. The diagnosis and management of chronic cough. Eur Respir J. 2004;24:481–492. doi: 10.1183/09031936.04.00027804. [DOI] [PubMed] [Google Scholar]
- 7.Irwin RS, French CL, Chang AB, Altman KW CHEST Expert Cough Panel. Classification of cough as a symptom in adults and management algorithms: CHEST guideline and expert panel report. Chest. 2018;153:196–209. doi: 10.1016/j.chest.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Song DJ, Song WJ, Kwon JW, Kim GW, Kim MA, Kim MY, et al. KAAACI evidence-based clinical practice guidelines for chronic cough in adults and children in Korea. Allergy Asthma Immunol Res. 2018;10:591–613. doi: 10.4168/aair.2018.10.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morice AH, Millqvist E, Bieksiene K, Birring SS, Dicpinigaitis P, Domingo Ribas C, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J. 2020;55:1901136. doi: 10.1183/13993003.01136-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.French CL, Irwin RS, Curley FJ, Krikorian CJ. Impact of chronic cough on quality of life. Arch Intern Med. 1998;158:1657–1661. doi: 10.1001/archinte.158.15.1657. [DOI] [PubMed] [Google Scholar]
- 11.Birring SS, Prudon B, Carr AJ, Singh SJ, Morgan MD, Pavord ID. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ) Thorax. 2003;58:339–343. doi: 10.1136/thorax.58.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chamberlain SA, Garrod R, Douiri A, Masefield S, Powell P, Bücher C, et al. The impact of chronic cough: a cross-sectional European survey. Lung. 2015;193:401–408. doi: 10.1007/s00408-015-9701-2. [DOI] [PubMed] [Google Scholar]
- 13.Hulme K, Dogan S, Parker SM, Deary V. ‘Chronic cough, cause unknown’: a qualitative study of patient perspectives of chronic refractory cough. J Health Psychol. 2019;24:707–716. doi: 10.1177/1359105316684204. [DOI] [PubMed] [Google Scholar]
- 14.Kang SY, Won HK, Lee SM, Kwon JW, Kim MH, Jo EJ, et al. Impact of cough and unmet needs in chronic cough: a survey of patients in Korea. Lung. 2019;197:635–639. doi: 10.1007/s00408-019-00258-9. [DOI] [PubMed] [Google Scholar]
- 15.GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morice AH, Millqvist E, Belvisi MG, Bieksiene K, Birring SS, Chung KF, et al. Expert opinion on the cough hypersensitivity syndrome in respiratory medicine. Eur Respir J. 2014;44:1132–1148. doi: 10.1183/09031936.00218613. [DOI] [PubMed] [Google Scholar]
- 17.Song WJ, Chung KF. Exploring the clinical relevance of cough hypersensitivity syndrome. Expert Rev Respir Med. 2020;14:275–284. doi: 10.1080/17476348.2020.1713102. [DOI] [PubMed] [Google Scholar]
- 18.Abdulqawi R, Dockry R, Holt K, Layton G, McCarthy BG, Ford AP, et al. P2X3 receptor antagonist (AF-219) in refractory chronic cough: a randomised, double-blind, placebo-controlled phase 2 study. Lancet. 2015;385:1198–1205. doi: 10.1016/S0140-6736(14)61255-1. [DOI] [PubMed] [Google Scholar]
- 19.Ford AC, Forman D, Moayyedi P, Morice AH. Cough in the community: a cross sectional survey and the relationship to gastrointestinal symptoms. Thorax. 2006;61:975–979. doi: 10.1136/thx.2006.060087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Voll-Aanerud M, Eagan TM, Wentzel-Larsen T, Gulsvik A, Bakke PS. Changes in respiratory symptoms and health-related quality of life. Chest. 2007;131:1890–1897. doi: 10.1378/chest.06-2629. [DOI] [PubMed] [Google Scholar]
- 21.Voll-Aanerud M, Eagan TM, Wentzel-Larsen T, Gulsvik A, Bakke PS. Respiratory symptoms, COPD severity, and health related quality of life in a general population sample. Respir Med. 2008;102:399–406. doi: 10.1016/j.rmed.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 22.Adams RJ, Appleton SL, Wilson DH, Taylor AW, Ruffin RE. Associations of physical and mental health problems with chronic cough in a representative population cohort. Cough. 2009;5:10. doi: 10.1186/1745-9974-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Voll-Aanerud M, Eagan TM, Plana E, Omenaas ER, Bakke PS, Svanes C, et al. Respiratory symptoms in adults are related to impaired quality of life, regardless of asthma and COPD: results from the European community respiratory health survey. Health Qual Life Outcomes. 2010;8:107. doi: 10.1186/1477-7525-8-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ternesten-Hasséus E, Larsson S, Millqvist E. Symptoms induced by environmental irritants and health-related quality of life in patients with chronic cough - A cross-sectional study. Cough. 2011;7:6. doi: 10.1186/1745-9974-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Song WJ, Morice AH, Kim MH, Lee SE, Jo EJ, Lee SM, et al. Cough in the elderly population: relationships with multiple comorbidity. PLoS One. 2013;8:e78081. doi: 10.1371/journal.pone.0078081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wheaton AG, Ford ES, Thompson WW, Greenlund KJ, Presley-Cantrell LR, Croft JB. Pulmonary function, chronic respiratory symptoms, and health-related quality of life among adults in the United States--National Health and Nutrition Examination Survey 2007-2010. BMC Public Health. 2013;13:854. doi: 10.1186/1471-2458-13-854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet. 2008;371:1364–1374. doi: 10.1016/S0140-6736(08)60595-4. [DOI] [PubMed] [Google Scholar]
- 28.Dicpinigaitis PV, Tso R, Banauch G. Prevalence of depressive symptoms among patients with chronic cough. Chest. 2006;130:1839–1843. doi: 10.1378/chest.130.6.1839. [DOI] [PubMed] [Google Scholar]
- 29.Polley L, Yaman N, Heaney L, Cardwell C, Murtagh E, Ramsey J, et al. Impact of cough across different chronic respiratory diseases: comparison of two cough-specific health-related quality of life questionnaires. Chest. 2008;134:295–302. doi: 10.1378/chest.07-0141. [DOI] [PubMed] [Google Scholar]
- 30.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35:1095–1108. doi: 10.1097/00005650-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Park B, Ock M, Lee HA, Lee S, Han H, Jo MW, et al. Multimorbidity and health-related quality of life in Koreans aged 50 or older using KNHANES 2013-2014. Health Qual Life Outcomes. 2018;16:186. doi: 10.1186/s12955-018-1016-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee SE, Lee JH, Kim HJ, Lee BJ, Cho SH, Price D, et al. Inhaled corticosteroids and placebo treatment effects in adult patients with cough: a systematic review and meta-analysis. Allergy Asthma Immunol Res. 2019;11:856–870. doi: 10.4168/aair.2019.11.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Statistics Korea. Korean Standard Classification of Occupations (KSCO) Daejeon: Statistics Korea; 2007. [Google Scholar]
- 34.Janssen MF, Szende A, Cabases J, Ramos-Goñi JM, Vilagut G, König HH. Population norms for the EQ-5D-3L: a cross-country analysis of population surveys for 20 countries. Eur J Health Econ. 2019;20:205–216. doi: 10.1007/s10198-018-0955-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kang SY, Kim GW, Song WJ, Chang YS, Cho SH. Chronic cough in Korean adults: a literature review on common comorbidity. Asia Pac Allergy. 2016;6:198–206. doi: 10.5415/apallergy.2016.6.4.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McGarvey LP, Carton C, Gamble LA, Heaney LG, Shepherd R, Ennis M, et al. Prevalence of psychomorbidity among patients with chronic cough. Cough. 2006;2:4. doi: 10.1186/1745-9974-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sohn KH, Song WJ, Kim SH, Jang HC, Kim KW, Chang YS. Chronic cough, not asthma, is associated with depression in the elderly: a community-based population analysis in South Korea. Korean J Intern Med (Korean Assoc Intern Med) 2019;34:1363–1371. doi: 10.3904/kjim.2018.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morice AH, Jakes AD, Faruqi S, Birring SS, McGarvey L, Canning B, et al. A worldwide survey of chronic cough: a manifestation of enhanced somatosensory response. Eur Respir J. 2014;44:1149–1155. doi: 10.1183/09031936.00217813. [DOI] [PubMed] [Google Scholar]
- 39.Song WJ, Kim JY, Jo EJ, Lee SE, Kim MH, Yang MS, et al. Capsaicin cough sensitivity is related to the older female predominant feature in chronic cough patients. Allergy Asthma Immunol Res. 2014;6:401–408. doi: 10.4168/aair.2014.6.5.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang MS, Jee YK. How to apply the concept of cough hypersensitivity in clinical practice? Allergy Asthma Immunol Res. 2019;11:589–592. doi: 10.4168/aair.2019.11.5.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fujimura M, Kasahara K, Kamio Y, Naruse M, Hashimoto T, Matsuda T. Female gender as a determinant of cough threshold to inhaled capsaicin. Eur Respir J. 1996;9:1624–1626. doi: 10.1183/09031936.96.09081624. [DOI] [PubMed] [Google Scholar]
- 42.Kastelik JA, Thompson RH, Aziz I, Ojoo JC, Redington AE, Morice AH. Sex-related differences in cough reflex sensitivity in patients with chronic cough. Am J Respir Crit Care Med. 2002;166:961–964. doi: 10.1164/rccm.2109061. [DOI] [PubMed] [Google Scholar]
- 43.Won HK, Kang SY, Kang Y, An J, Lee JH, Lee SM, et al. Cough-related laryngeal sensations and triggers in adults with chronic cough: symptom profile and impact. Allergy Asthma Immunol Res. 2019;11:622–631. doi: 10.4168/aair.2019.11.5.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.French CT, Fletcher KE, Irwin RS. Gender differences in health-related quality of life in patients complaining of chronic cough. Chest. 2004;125:482–488. doi: 10.1378/chest.125.2.482. [DOI] [PubMed] [Google Scholar]
- 45.Davis S, Wailoo A. A review of the psychometric performance of the EQ-5D in people with urinary incontinence. Health Qual Life Outcomes. 2013;11:20. doi: 10.1186/1477-7525-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Song WJ, Chang YS, Faruqi S, Kang MK, Kim JY, Kang MG, et al. Defining chronic cough: a systematic review of the epidemiological literature. Allergy Asthma Immunol Res. 2016;8:146–155. doi: 10.4168/aair.2016.8.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kang MG, Song WJ, Kim HJ, Won HK, Sohn KH, Kang SY, et al. Point prevalence and epidemiological characteristics of chronic cough in the general adult population: the Korean National Health and Nutrition Examination Survey 2010-2012. Medicine (Baltimore) 2017;96:e6486. doi: 10.1097/MD.0000000000006486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McGarvey L, Gibson PG. What is chronic cough? Terminology. J Allergy Clin Immunol Pract. 2019;7:1711–1714. doi: 10.1016/j.jaip.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 49.Song WJ, Morice AH. Cough hypersensitivity syndrome: a few more steps forward. Allergy Asthma Immunol Res. 2017;9:394–402. doi: 10.4168/aair.2017.9.5.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Weighted prevalence and EQ-5D-3L index score of chronic cough and chronic phlegm
Comparison of weighted demographic and clinical parameters according to sex and chronic cough in the elderly (age ≥ 65 years)
Univariate linear regression analyses of factors associated with EQ-5D-3L index scores in the KNHANES 2010–2016
Multivariate linear regression analyses of factors associated with EQ-5D-3L index scores among subjects without depression or arthritis in the KNHANES 2010–2016
Responses to the EQ-5D-3L questionnaire in subjects with and without chronic cough, according to age and sex
Prevalence and EQ-5D-3L index score of current chronic and non-chronic cough in the KNHANES 2010–2012 surveys
Histogram of cough duration in adults with chronic cough (aged ≥ 40 years).
EuroQoL EQ-5D-3L index scores according to cough duration.
EuroQoL EQ-5D-3L index scores in subjects without depression or arthritis, classified by (A) sex and (B, C) age and gender subgroups. The scores are presented as weighted means ± standard errors.