Abstract
Allergic asthma is a public health problem that affects human health and socioeconomic development. Studies have found that the prevalence of asthma has significantly increased in recent years, which has become particularly pronounced in developed countries. With rapid urbanization in China in the last 3 decades, the prevalence of asthma has increased significantly in urban areas. As changes in genetic backgrounds of human populations are limited, environmental exposure may be a major factor that is responsible for the increased prevalence of asthma. This review focuses on environmental components of farms and rural areas that may have protective effects in reducing the development of asthma. Farm and rural related microorganism- and pathogen-associated molecular patterns are considered to be important environmental factors that modulate host's innate and adaptive immune system to induce protection effects later in life. Environmental microbial-related immunotherapy will also be discussed as the future research direction for the prevention of allergic asthma.
Keywords: Asthma, epidemiology, hygiene hypothesis, environmental exposure, house dust mite
INTRODUCTION
Epidemiological studies have confirmed that allergic asthma becomes more prevalent around the world in the past few decades, and the prevalence of asthma is higher in urban areas than in rural areas. The increased occurrence of asthma is often found to be associated with improvement in hygiene conditions of humans. Thirty years ago, the classic “hygiene hypothesis” stated that crowded and unhygienic living conditions will lead to a decrease in the prevalence of asthma as well as in other allergic disorders including eczema and hay fever.1 The unhygienic environment increases the opportunities for children to contact microorganisms at the early stages of life. The advent of this hypothesis has increased research on the role of environmental factors in allergic diseases, especially asthma. Currently, reports on asthma-protective factors in the environment have yielded inconsistent findings. Endotoxin has been found to be associated with protection against asthma as a recent study reported that the prevalence of asthma was lower in Amish children in a high endotoxin environment.2 The mechanisms by which environmental factors regulate allergic asthma have been extensively investigated and the findings further expand our knowledge of the interaction between environmental factors and allergic asthma. The aim of the present review is to summarize the research works in China as well as the findings of research groups from other countries in epidemiological surveys on asthma, environmental microorganism factors, immunoregulation mechanisms, and microbial-related immunotherapy. New research directions on relations between environmental factors and allergic asthma are proposed which are expected to guide future studies.
EPIDEMIOLOGICAL TRENDS OF ALLERGIC ASTHMA
Trends in the prevalence of allergic asthma
Since the 1950s, the global prevalence of allergic asthma has been increasing.3 The International Study of Asthma and Allergies in Childhood analyzed the multicenter survey data on allergic asthma, allergic rhinoconjunctivitis, and eczema at 7-year intervals on average, and the results showed increases in all 3 allergic diseases.4 Generally, the prevalence of asthma is higher in developed countries, while its increasing trend has slowed down in recent years. However, the asthma prevalence showed remarkably increased in the developing countries with rapid economic growth and urbanization.5
In the USA, the prevalence of asthma increased at an annual rate of 1.5% up to 2001, and reached 8.4% in 2010.6 However, it has shown a steady trend since 2008,7 with 8.4% in 2016 and 6.7% in 2018, according to the national survey data.8,9 The prevalence in the UK had also stabilized in recent years (7.2% in 2006 and 6.5% in 2016).10,11 A high asthma prevalence was found in Canada from 14.3% in 2006 to 16% in 2012.12 The rate of school-age children with asthma in Sweden was 2.5%, 5.7%, and 7.1% in 1979, 1991, and 2007, respectively.13 In 2008, 14.9% of children aged 7–11 years in Australia had asthma.14 In Melbourne, the prevalence in 4-year-old children remained high at 13.8% in 2017.15 Singapore showed significantly increased prevalence trend from 5.5% in 1967, to 13.7% in 1987, and 20% in 1994,16,17 and the prevalence continuously went up to 20.7% in 1994 to 27.4% in 2001 for 12- to 15-year-old children.18 Data from National Health Insurance Sharing Service of Korea revealed a 1.4-fold increase from 1.55% to 2.21% between 2002 and 2015 for asthma prevalence, which was more common in elderly population aged ≥ 60 years.19
In China, the prevalence rates of asthma and other allergic diseases have been increasing each year. Pediatric asthma surveys that were conducted in 1990, 2000, and 2010 showed a substantial rise in asthma prevalence in most cities.20,21,22,23 For example, in Beijing, prevalence of asthma in children increased from 0.77% in 1990, to 2.05% in 2000, and to 2.55% in 2010.21,22,23 Shanghai children also demonstrated a similar increasing trend in asthma prevalence from 1.50%, to 3.34%, and to 5.73%, respectively.21,22,23 A survey in school children from Guangzhou also showed increasing prevalence of asthma from 3.9% in 1994, to 4.6% in 2001, and to 6.9% in 2009.24 In 1974, 1985 and 1991, Taiwanese showed their prevalence of asthma at 1.3%, 5.07%, and 5.8%, respectively,25,26 while the prevalence of doctor diagnosed asthma increased dramatically 10 years later at 11.7% in 2001 and 15.7% in 2007.27 In Hong Kong, however, the prevalence of asthma in 6- to 7-year-old children did not change significantly between 1994 (7.8%) and 2001(7.9%).28,29
Difference in the prevalence of asthma between urban and rural populations
In contrast to the high prevalence of asthma in urban areas, asthma is less prevalent in rural regions. Farming and rural environment are proposed to be 2 classic protective factors against asthma in Europe.30,31 Stein et al.2 compared 30 matched Amish children from traditional farms and Hutterite children from modern farms, and found that although both groups had similar genetic backgrounds and lifestyle habits, the prevalence of asthma was 4 to 6 times higher in the Hutterite population than in the Amish population who were exposed to the high endotoxin levels in house dust. Our study showed that the prevalence of asthma in 13- to 14-year-old children from rural Conghua was significantly lower than that in those from urban Guangzhou (3.4% vs. 6.9%).32 The prevalence rated of allergic rhinitis and eczema in the 2 groups of children also showed similar rural-urban differences.32 Similar to the situation observed in southern China, the prevalence of asthma in children from rural regions in northern China was significantly lower than in Beijing city (1.1% vs. 6.3%).30
ENVIRONMENTAL AND MICROBIAL EXPOSURE
Environmental exposure and asthma
Asthma pathogenesis is multifactorial and the most important factors are genetics and environmental factors. Since significant changes in genetic background of humans is less likely to occur within several decades, environmental factors might be the major determinants modulating the prevalence of asthma. The “hygiene hypothesis” proposed in 1989 by Strachan1 suggested that the rapid increase in the prevalence of allergies and autoimmune diseases in humans is due to an overly clean environment. Following the initial “hygiene hypothesis,” many epidemiological studies provided direct evidence for the correlation between the prevalence of asthma and living environmental condition in children and explored the underlying immunological and molecular mechanisms.33,34,35,36 In 1999, Braun-Fahrländer et al.37 first found that the risk of atopic constitution and allergies in children who grew up on farms was significantly lower than those who grew up in non-farm conditions. Subsequently, many epidemiological studies that investigated children asthma on European farms,38,39,40 traditional and modern farms in the USA,2 as well as the studies comparing urban and rural environment32,41,42,43 have validated the protective effect of a farm environment so called “farm effect.”44 In the southern and northern regions of China, we have also found that the agricultural environment and rural house dust endotoxin have protective effects on childhood asthma.30,32 It is generally believed that exposure to the farm environment (particularly traditional farms) early in life has significantly reduced the prevalence of asthma in the children compared with those who are not exposed the farm environment. Due to environment diversity, multiple protective environmental factors were found in different studies. The contact factors included livestock, pets,45 farm crops,38 unpasteurized milk,46,47,48 breastfeeding, farm or village cultivation activities,32,49 and fishing.50 The major findings from these studies are summarized in Table.2,30,32,51,52,53,54,55,56,57
Table. Studies on environmental exposure and allergies in different countries and regions.
| Region | Exposure factor | Sample size (No.) | Sample age (yr) | Main findings | Outcomes (onset of allergy) | Ref. |
|---|---|---|---|---|---|---|
| Asia-Beijing, China | Farm livestock and farming behavior | 7,077 | 13–14 | Contact with farming and livestock has protective effects. | Reduced | 30 |
| Oceania-New Zealand | Traffic at place of residence, drugs, and farm foodstuffs | 24,190 | 6–7; 13–14 | Truck traffic, antibiotics or paracetamol exposure during early life, were positively correlated with eczema. Consumption of milk, seafood, eggs, and have a dog in home, were negatively correlated with eczema. | Reduced | 51 |
| Europe-Turku, Finland and neighboring regions | Indoor pet exposure during the perinatal period | 256 | 0–2 | Fecal Bifidobacterium longum counts in non-wheezing infants who were exposed to pets were significantly higher than those of wheezing infants who were not exposed to pets. | Reduced | 52 |
| Central Europe-Silesia, Poland | Unpasteurized dairy products and activities related to livestock | 1,676 | >5 | Agriculture-related contact significantly decreased in Silesia and the prevalence of allergies drastically increased within a short period of nine years. | Reduced | 53 |
| Northern Europe | Livestock | 11,123 | Mean age: 53 | Subjects who grew up in livestock farms had a lower incidence of asthma (8%) compared to those who grew up in inner cities (11%). | Reduced | 54 |
| Asia-Guangzhou, China | Farming environment and endotoxin levels | 13,251 | 13–14 | Early contact with crops and high levels of environmental endotoxins may protect children from the effects of asthma. | Reduced | 32 |
| North America-USA | Endotoxin levels in homes | 60 | 7–14 | High endotoxin levels in traditional Amish farms was a protective factor for asthma, and innate immunity also played an important role. | Reduced | 2 |
| North America-Canada | Farming environment | 10,941 | 0–11 | The cumulative 14-year asthma incidence in children living in a farming environment was significantly lower than live in non-rural and rural non-farming environments. | Reduced | 55 |
| South America-Cordoba rural areas | Contact with livestock, such as dairy farms | 1,804 | 13–14 | Residency on dairy farms, including periodic livestock contact reduced allergic rhino-conjunctivitis. | Reduced | 56 |
| Africa-Cape Town and Eastern Cape province | Farming exposure, sunlight exposure, pet, antibiotic and probiotic exposure, antihelminth exposure, cigarette smoke and fossil fuel exposure. | 1,736 | 1–3 | Farm animal exposure but not unpasteurized milk is the strongest factor to against allergy. Fermented milk produces has a significant effect in urban cohort but not in rural. | Reduced | 57 |
Microbial exposure and asthma
Among the complex and diverse factors of the living environment that we are exposed, microbes and their chemical compounds might be the key elements that play roles in the modulation of immune responses and the pathogenesis of allergic diseases like asthma. Acinetobacter lwoffii and Lactococcus lactis from farms that can induce T-helper 1 cell (Th1) differentiation and mediate protective effects against allergic airway inflammation.58 Ege et al.59 reported that bacterial and fungal derivatives in house dust had a significant negative correlation with the incidence of asthma in exposed children. In one Finland study, children who grew up in non-farm families showed decreased risk of asthma, but their family bacterial microbiota composition is similar to that of farm families, suggesting that the microbes are accountable for the farm environment-associated protection against development of asthma.60
In addition, high levels of endotoxin in farm and rural environments is related to a low prevalence of asthma and other allergic diseases.61,62,63 Endotoxin is a component of the cell wall of gram-negative bacteria and cyanobacteria.64 A previous study found that the protective effects of endotoxins might be related to the induction of A20 expression in lung epithelial cells.65 Another investigation revealed that endotoxin levels were 6.8 times higher in traditional Amish farms than in modern Hutterite farms and may regulate innate immune pathways in children to prevent the development of asthma.2 In addition to the endotoxins, many pathogen-associated molecular patterns (PAMPs), such as extracellular polysaccharides, muramic acid, and glucans, have been shown to be closely associated with the protective effects of farms.66
Antibiotic exposure during maternal pregnancy or early life67,68,69,70,71 and cesarean delivery57,72,73 can increase the prevalence of asthma in children by affecting the gut microbiota and other mechanisms. Anti-parasitic therapy is also shown to be associated with increased prevalence of asthma.74,75 It was also noted that the prevalence of eczema in children would increase when their mothers accepted deworming treatment during pregnancy, while anthelminthic in children had no significant effect on eczema,76 suggesting that the protective effect of allergies induced by parasite infection might begin in the mother's uterus.
However, it is worthy of noting that some types of microorganisms may have opposite effects on development of asthma. For example, infection with bacterial species like Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis and some virus often aggravates asthma.77,78
ENVIRONMENTAL FACTORS AND IMMUNOLOGICAL REGULATION OF ASTHMA
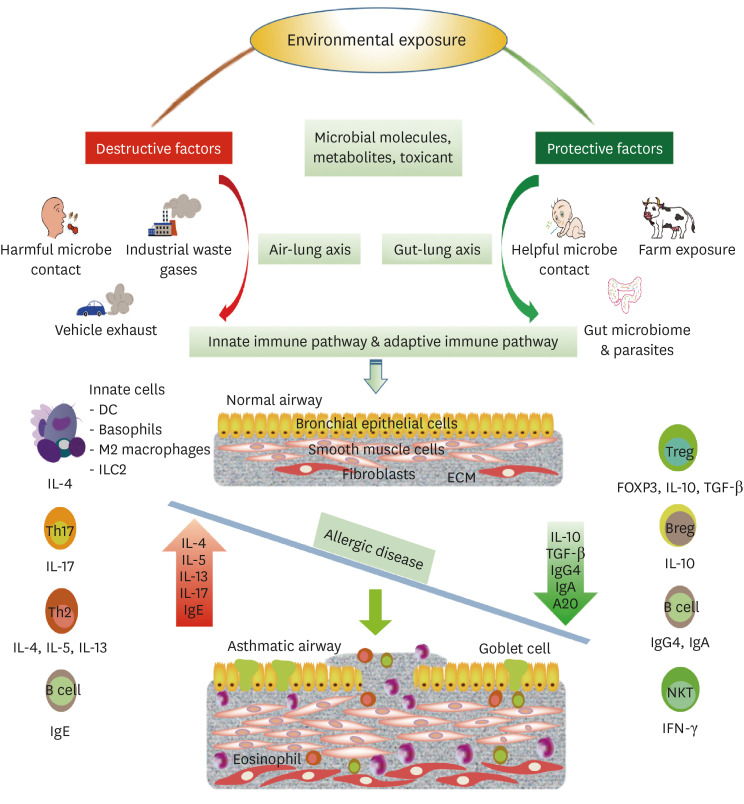
There is still an insufficient understanding of the immunological relationship between the dramatic increase in allergy prevalence and environmental changes. However, in recent years, it has become clear that asthma is a heterogeneous disease in which both innate and acquired immunities are involved. Common factors that promote or inhibit the onset of asthma include allergen exposure and microbial/parasitic infection, oxidative stress as well as environmental and microbial related metabolites. Cells involved in this process include eosinophils, basophils, neutrophils, mast cells, macrophages, dendritic cells (DCs), epithelial cells, natural killer T (NKT) cells, natural helper cells, Th2 cells, T-helper 17 (Th17) cells, group 2 innate lymphoid cells (ILC2), B cells, regulatory T cells (Tregs), and regulatory B cells (Bregs).79 In Figure, we illustrate the environmental factors and immunological regulatory mechanisms involved in the development and prevention of asthma.
Figure. Potential immunological mechanisms by which environmental factors affect allergic asthma. Environmental microbial molecules and metabolites act on innate and adaptive immune pathways through the air-lung axis and/or the gut-lung axis to exert their immunoregulatory effects. Harmful bacteria, viruses, and industrial waste gases, as well as automobile exhaust, can promote airway inflammation through induction of IL-4, IL-5, IL-13, and IL-17 secretion by innate immune cells (e.g., ILC2, airway epithelial cells, DCs, macrophages, and basophils) and adaptive immune cells (e.g., Th17 cells, Th2 cells, and B cells), resulting in airway mucosal damage, smooth muscle hyperplasia, and fibrotic changes. Conversely, protective environmental factors, such as early life contact with helpful microorganisms, gut parasitic worm infection, gut microbiota, and farm exposure, can result in the production of IL-10, TGF-β, IFN-γ, IgA, and IgG4 by innate (toll-like receptors, airway epithelium, DCs, natural killer T cells), and adaptive immune cells (Tregs, Bregs, and B cells) to protect against allergic asthma.
DC, dendritic cell; ILC2, group 2 innate lymphoid cells; ECM, extracellular matrix; IL, interleukin; TGF-β, transformation and growth factor β; Ig, immunoglobulin; IFN-γ, interferon-γ.
Innate immune mechanisms
During human evolution, our immune system is exposed to and interacted with symbiotic surrounding pathogens. The PAMPs on the gut or respiratory microbiota and parasitic worms might be recognized by the pattern recognition receptors on innate immune cells to initiate the immune responses. Study by Lauener et al.80 found that compared with the unexposed children, children with farm exposure had increased CD14/toll-like receptor (TLR) 2 expression levels and that exposure to a farm environment early in life correlates to important regulatory effects on asthma through TLRs. A subsequent study showed that maternal exposure to a microbe-rich environment before delivery resulted in increasing levels of genes expression for the receptors of the innate immune system (i.e. TLR2, TLR4, and CD14) in their children. The underlying mechanism for this phenomenon may be related to the intrauterine environment and/or epigenetic changes.81 TLRs are considered to be key systems in immune response regulation and epithelial cells and DCs play a vital role in linking innate immunity to adaptive immunity. Exposure to appropriate doses of lipopolysaccharide (LPS) weakens signaling pathways required for the production of allergy-related cytokine while retaining double-stranded RNA/DC pathways, thereby activating DCs to promote production of Th1 cytokines but not Th2.82 In addition, LPS exposure will increase the synthesis of the zinc finger protein A20,83 thereby inhibiting airway allergic responses to Dermatophagoides pteronyssinus.82 A prospective study showed that maternal exposure to livestock before delivery resulted in significant increases in TLR5 and TLR9 in umbilical cord blood in children while the risk of atopic dermatitis was significantly reduced.84 Stein et al.2 compared the peripheral blood cell compositions and the phenotypes of 30 traditional farm and modern farm children, and observed that the percentage of eosinophils was decreased in the traditional farm children and that monocytes exhibited an inhibitory phenotype (lower levels of the human leukocyte antigens DR and HLA-DR as well as higher levels of immunoglobulin-like transcript 3, ILT3). In addition, traditional farm dust extracts had significant protective effects in animal models of asthma. In myeloid differentiation primary response gene 88 (MyD88)-deficient mice, this protective effect was drastically reduced. In MyD88- and toll/interleukin-1 receptor domain-containing adaptor inducing IFN-β (TRIF)-deficient mice, this protective effect was completely abolished. These 2 molecules are located at the convergence of multiple immune signaling pathways. These results suggest that environment microbial factors modulate immune response and induce immune suppression allergic asthma through innate immunity.2
It is known that, in addition to endotoxins, diverse microbial products in the environment are effective stimuli for innate immunity.85,86 Invariant NKT (iNKT) cells are able to recognize glycolipid antigens and some PAMPs may directly activate iNKT cells independently of TLRs. House dust extract (HDE) could promote OVA-induced airway inflammation in asthmatic mice through iNKT cells, but the source of iNKT-related antigens in HDE has not yet been identified.87 However, a previous study found that influenza A infection in early life could protect adult mice from allergen-induced airway hyperreactivity (AHR), which was associated with a population of NKT cells, enriched for a CD4-CD8-(DN), T-box transcription factor expressed in T-cells (T-bet)-dependent, and interferon-γ (INF-γ)-secreting subset.88 Chuang et al.89 proposed that early/neonatal infection or antigen stimulation could induce certain NKT subsets, such as CD38hiDN NKT cells, in the lung to produce IFN-γ but not IL-17, IL-4, or IL-13, demonstrating that this NKT subset could directly contact and inhibit CD4+ T cell proliferation, thereby blocking allergen-induced AHR.
Acquired immune mechanisms
Study by Gereda et al.90 demonstrated that persistent environmental endotoxin exposure could induce Th1 immune responses resulting in change in the Th1/Th2 equilibrium, thereby reducing allergen sensitivity and protection of infants from allergen sensitization. Asthmatic mice infected with hookworms or whipworms secrete anti-inflammatory protein-2 (AIP-2) and protein P43 that inhibited costimulatory molecule expression in DCs and Th2 response by binding to IL-13.91,92
Regulatory CD4+ T cells (Tregs) play a vital role at the sensitization stage in the pathogenesis of allergic asthma and contribute to balancing T-cell differentiation and maturation. The functions of effector CD4+ T cells, including Th1, Th2, and Th17 cells, can be regulated by Tregs, which play an important role in the immunoregulation and suppression of asthma.93 Many studies have found a correlation between environmental microbial exposure and Treg differentiation/development. McGuirk and Mills94 and Wilson et al.95 reported that bacteria and helminth infection could facilitate the development of Tregs. Schaub et al.96 found that maternal farm exposure could regulate the immune systems of children, increased the number and functions of Tregs in umbilical-cord blood in newborns, decreased the proliferation of Th2 lymphocytes, and reduced Th2 cytokine levels. They also found that consumption of farm milk by mothers could increase forkhead box P3 (FoxP3) demethylation in their children, thereby reducing their children's risk of asthma during childhood and adulthood. Lluis et al.97,98 reported that during early childhood, farm milk exposure increase FoxP3 demethylation and Treg cell counts through at least 6 different signaling pathways. Our group used a murine gut parasite, Heligmosomoides polygyrus, to investigate the immunoregulation mechanism of gut parasites infection against allergic airway inflammation. It was observed that infection with H. polygyrus induced prominent response of IL-10-producing regulatory B cells (IL-10+ Bregs). These Breg cells were able to promote differentiation and proliferation of IL-10-producing and FoxP3 regulatory CD4+ T cells. Cell transfer and depletion experiments demonstrated that IL-10+Breg, IL-10+Treg and FoxP3+Treg cells participated in the parasite-induced immunosuppression of allergic airway inflammation.99
A birth cohort study showed that contact with livestock or cats during pregnancy could increase secretory immunoglobulin (sIgA) levels in breast milk and reduced atopic dermatitis in their children.100 Many studies have shown that elevated sIgA and transforming growth factor-β (TGF-β) levels in breast milk have protective effects against asthma in children.101,102 TGF-β secreted by Treg cells is a key factor for survival of IgA+ B cells.103 IgA limits the responses of microorganisms to host mucosal immunity.103 These two effects jointly maintain symbiosis with microorganisms in the body, which may be an indirect protective mechanism against allergies.104 Animal experiments have shown that soluble extracts from nematodes can increase IL-10 and TGF-β levels, thereby inhibiting airway inflammation in asthma.105
FUTURE RESEARCH DIRECTIONS
Epidemiological observations provide a mountain of evidence in proving the link between asthma and environmental microbial and parasite exposure.60,106,107,108,109,110 Human fecal bacteria transplantation, probiotic therapy111,112 and parasite immunotherapy76,113 used in clinical trials, and mouse model research114,115 have enhanced our understanding of the interconnection between environmental microbes,116 symbionts,117,118,119,120,121,122,123 and asthma. The available data support the negative correlation between exposure to farms and rural environmental microorganisms in early life and that the incidence of allergic asthma and the specific exposure time window could be critical.110,124 To determine the “best time window” for microbial exposure and to identify the protective microbiome, more cohort observations are needed in the future. Although observational studies help understand the importance of environmental factors in the modulation of allergic asthma, more intervention studies are needed to further elucidate the molecular mechanisms involved in asthma pathogenesis. Animal models are also powerful tolls for the mechanism study of asthma pathogenesis regulated by environmental microorganisms. Furthermore, microbial immunotherapy has been tested as the potential means to protect against allergic asthma; therefor, in-depth studies are needed to characterize the derivatives of symbiotic or infective microorganisms for rational and safe use to control asthma and other allergic diseases.
SUMMARY
It is well established that environmental factors strongly influence the onset and development of asthma and other allergic diseases. The external microorganisms and internal microbiota, and their derivatives have been identified as major components that modulate the immune responses of humans and, in most cases, induce immunosuppression to prevent or alleviate asthma pathogenesis. Research findings have revealed that multiple facets of the immune system are involved in the complex interaction between environmental factors and the prevention of asthma. Further studies on the pathogenesis of allergic asthma, the nature of microorganism derivatives, and immune responses to the bacterial components may result in novel therapies to control and prevent occurrence of allergic asthma in human populations.
ACKNOWLEDGMENTS
This study was supported by the following projects: Key project of National Natural Science Foundation of China-Guangdong joint fund (U1801286); Special funding program for Science and Technology Development of Guangdong Province (Frontier and key technology innovation direction - major science and technology special project) (2017B020226006); Precision Medicine Research Program of National Key Research and Development Project of China (2016YFC0905800); Key program of Science & Technology Specific Project of Guangzhou Science and Innovation Bureau (201607020046).
Footnotes
Disclosure: There are no financial or other issues that might lead to conflict of interest.
References
- 1.Strachan DP. Hay fever, hygiene, and household size. BMJ. 1989;299:1259–1260. doi: 10.1136/bmj.299.6710.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stein MM, Hrusch CL, Gozdz J, Igartua C, Pivniouk V, Murray SE, et al. Innate immunity and asthma risk in amish and hutterite farm children. N Engl J Med. 2016;375:411–421. doi: 10.1056/NEJMoa1508749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robertson CF, Roberts MF, Kappers JH. Asthma prevalence in Melbourne schoolchildren: have we reached the peak? Med J Aust. 2004;180:273–276. doi: 10.5694/j.1326-5377.2004.tb05924.x. [DOI] [PubMed] [Google Scholar]
- 4.Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–743. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 5.Moorman JE, Rudd RA, Johnson CA, King M, Minor P, Bailey C, et al. National surveillance for asthma--United States, 1980–2004. MMWR Surveill Summ. 2007;56:1–54. [PubMed] [Google Scholar]
- 6.Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United States, 2001–2010. Vital Health Stat 3. 2012:1–58. [PubMed] [Google Scholar]
- 7.Akinbami LJ, Simon AE, Rossen LM. Changing trends in asthma prevalence among children. Pediatrics. 2016;137:e20152354. doi: 10.1542/peds.2015-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loftus PA, Wise SK. Epidemiology of asthma. Curr Opin Otolaryngol Head Neck Surg. 2016;24:245–249. doi: 10.1097/MOO.0000000000000262. [DOI] [PubMed] [Google Scholar]
- 9.Hill E, Abboud H, Briggs FB. Prevalence of asthma in multiple sclerosis: a United States population-based study. Mult Scler Relat Disord. 2019;28:69–74. doi: 10.1016/j.msard.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 10.Mukherjee M, Stoddart A, Gupta RP, Nwaru BI, Farr A, Heaven M, et al. The epidemiology, healthcare and societal burden and costs of asthma in the UK and its member nations: analyses of standalone and linked national databases. BMC Med. 2016;14:113. doi: 10.1186/s12916-016-0657-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bloom CI, Saglani S, Feary J, Jarvis D, Quint JK. Changing prevalence of current asthma and inhaled corticosteroid treatment in the UK: population-based cohort 2006–2016. Eur Respir J. 2019;53:1802130. doi: 10.1183/13993003.02130-2018. [DOI] [PubMed] [Google Scholar]
- 12.Karunanayake CP, Amin K, Abonyi S, Dosman JA, Pahwa P. Prevalence and determinants of asthma among aboriginal adolescents in Canada. J Asthma. 2020;57:40–46. doi: 10.1080/02770903.2018.1541354. [DOI] [PubMed] [Google Scholar]
- 13.Hicke-Roberts A, Åberg N, Wennergren G, Hesselmar B. Allergic rhinoconjunctivitis continued to increase in Swedish children up to 2007, but asthma and eczema levelled off from 1991. Acta Paediatr. 2017;106:75–80. doi: 10.1111/apa.13433. [DOI] [PubMed] [Google Scholar]
- 14.Knibbs LD, Cortés de Waterman AM, Toelle BG, Guo Y, Denison L, Jalaludin B, et al. The Australian Child Health and Air Pollution Study (ACHAPS): a national population-based cross-sectional study of long-term exposure to outdoor air pollution, asthma, and lung function. Environ Int. 2018;120:394–403. doi: 10.1016/j.envint.2018.08.025. [DOI] [PubMed] [Google Scholar]
- 15.Peters RL, Koplin JJ, Gurrin LC, Dharmage SC, Wake M, Ponsonby AL, et al. The prevalence of food allergy and other allergic diseases in early childhood in a population-based study: HealthNuts age 4-year follow-up. J Allergy Clin Immunol. 2017;140:145–153.e8. doi: 10.1016/j.jaci.2017.02.019. [DOI] [PubMed] [Google Scholar]
- 16.Chong TM. Pattern of bronchial asthma in Singapore. Singapore Med J. 1972;13:154–160. [PubMed] [Google Scholar]
- 17.Goh DY, Chew FT, Quek SC, Lee BW. Prevalence and severity of asthma, rhinitis, and eczema in Singapore schoolchildren. Arch Dis Child. 1996;74:131–135. doi: 10.1136/adc.74.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang XS, Tan TN, Shek LP, Chng SY, Hia CP, Ong NB, et al. The prevalence of asthma and allergies in Singapore; data from two ISAAC surveys seven years apart. Arch Dis Child. 2004;89:423–426. doi: 10.1136/adc.2003.031112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee E, Kim A, Ye YM, Choi SE, Park HS. Increasing prevalence and mortality of asthma with age in Korea, 2002–2015: a nationwide, population-based study. Allergy Asthma Immunol Res. 2020;12:467–484. doi: 10.4168/aair.2020.12.3.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin J, Wang W, Chen P, Zhou X, Wan H, Yin K, et al. Prevalence and risk factors of asthma in mainland China: The CARE study. Respir Med. 2018;137:48–54. doi: 10.1016/j.rmed.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 21.Chen Y, Wong GW, Li J. Environmental exposure and genetic predisposition as risk factors for asthma in China. Allergy Asthma Immunol Res. 2016;8:92–100. doi: 10.4168/aair.2016.8.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen YZ National Cooperation Group On Childhood Asthma. A nationwide survey in China on prevalence of asthma in urban children. Zhonghua Er Ke Za Zhi. 2003;41:123–127. [PubMed] [Google Scholar]
- 23.National Cooperative Group on Childhood Asthma; Institute of Environmental Health and Related Product Safety, Chinese Center for Disease Control and Prevention; Chinese Center for Disease Control and Prevention. Third nationwide survey of childhood asthma in urban areas of China. Zhonghua Er Ke Za Zhi. 2013;51:729–735. [PubMed] [Google Scholar]
- 24.Li J, Wang H, Chen Y, Zheng J, Wong GW, Zhong N. House dust mite sensitization is the main risk factor for the increase in prevalence of wheeze in 13- to 14-year-old schoolchildren in Guangzhou city, China. Clin Exp Allergy. 2013;43:1171–1179. doi: 10.1111/cea.12157. [DOI] [PubMed] [Google Scholar]
- 25.Tang RB, Tsai LC, Hwang HM, Hwang B, Wu KG, Hung MW. The prevalence of allergic disease and IgE antibodies to house dust mite in schoolchildren in Taiwan. Clin Exp Allergy. 1990;20:33–38. doi: 10.1111/j.1365-2222.1990.tb02772.x. [DOI] [PubMed] [Google Scholar]
- 26.Hsieh KH, Shen JJ. Prevalence of childhood asthma in Taipei, Taiwan, and other Asian Pacific countries. J Asthma. 1988;25:73–82. doi: 10.3109/02770908809071357. [DOI] [PubMed] [Google Scholar]
- 27.Chen BY, Chen CH, Chuang YC, Wu YH, Pan SC, Guo YL. Changes in the relationship between childhood asthma and ambient air pollution in Taiwan: Results from a nationwide survey repeated 5 years apart. Pediatr Allergy Immunol. 2019;30:188–194. doi: 10.1111/pai.12999. [DOI] [PubMed] [Google Scholar]
- 28.Lee SL, Wong W, Lau YL. Increasing prevalence of allergic rhinitis but not asthma among children in Hong Kong from 1995 to 2001 (Phase 3 International Study of Asthma and Allergies in Childhood) Pediatr Allergy Immunol. 2004;15:72–78. doi: 10.1046/j.0905-6157.2003.00109.x. [DOI] [PubMed] [Google Scholar]
- 29.Wong GW, Leung TF, Ko FW. Changing prevalence of allergic diseases in the Asia-pacific region. Allergy Asthma Immunol Res. 2013;5:251–257. doi: 10.4168/aair.2013.5.5.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ma Y, Zhao J, Han ZR, Chen Y, Leung TF, Wong GW. Very low prevalence of asthma and allergies in schoolchildren from rural Beijing, China. Pediatr Pulmonol. 2009;44:793–799. doi: 10.1002/ppul.21061. [DOI] [PubMed] [Google Scholar]
- 31.Wong GW, Mahesh PA, Ogorodova L, Leung TF, Fedorova O, Holla AD, et al. The EuroPrevall-INCO surveys on the prevalence of food allergies in children from China, India and Russia: the study methodology. Allergy. 2010;65:385–390. doi: 10.1111/j.1398-9995.2009.02214.x. [DOI] [PubMed] [Google Scholar]
- 32.Feng M, Yang Z, Pan L, Lai X, Xian M, Huang X, et al. Associations of early life exposures and environmental factors with asthma among children in rural and urban areas of Guangdong, China. Chest. 2016;149:1030–1041. doi: 10.1016/j.chest.2015.12.028. [DOI] [PubMed] [Google Scholar]
- 33.Lambrecht BN, Hammad H. The immunology of the allergy epidemic and the hygiene hypothesis. Nat Immunol. 2017;18:1076–1083. doi: 10.1038/ni.3829. [DOI] [PubMed] [Google Scholar]
- 34.Murrison LB, Brandt EB, Myers JB, Hershey GK. Environmental exposures and mechanisms in allergy and asthma development. J Clin Invest. 2019;129:1504–1515. doi: 10.1172/JCI124612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martikainen MV, Rönkkö TJ, Schaub B, Täubel M, Gu C, Wong GW, et al. Integrating farm and air pollution studies in search for immunoregulatory mechanisms operating in protective and high-risk environments. Pediatr Allergy Immunol. 2018;29:815–822. doi: 10.1111/pai.12975. [DOI] [PubMed] [Google Scholar]
- 36.Sabatel C, Radermecker C, Fievez L, Paulissen G, Chakarov S, Fernandes C, et al. Exposure to bacterial CpG DNA protects from airway allergic inflammation by expanding regulatory lung interstitial macrophages. Immunity. 2017;46:457–473. doi: 10.1016/j.immuni.2017.02.016. [DOI] [PubMed] [Google Scholar]
- 37.Braun-Fahrländer C, Gassner M, Grize L, Neu U, Sennhauser FH, Varonier HS, et al. Prevalence of hay fever and allergic sensitization in farmer's children and their peers living in the same rural community. Clin Exp Allergy. 1999;29:28–34. doi: 10.1046/j.1365-2222.1999.00479.x. [DOI] [PubMed] [Google Scholar]
- 38.Illi S, Depner M, Genuneit J, Horak E, Loss G, Strunz-Lehner C, et al. Protection from childhood asthma and allergy in Alpine farm environments-the GABRIEL Advanced Studies. J Allergy Clin Immunol. 2012;129:1470–7.e6. doi: 10.1016/j.jaci.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 39.MacNeill SJ, Sozanska B, Danielewicz H, Debinska A, Kosmeda A, Boznanski A, et al. Asthma and allergies: is the farming environment (still) protective in Poland? The GABRIEL Advanced Studies. Allergy. 2013;68:771–779. doi: 10.1111/all.12141. [DOI] [PubMed] [Google Scholar]
- 40.Riedler J, Eder W, Oberfeld G, Schreuer M. Austrian children living on a farm have less hay fever, asthma and allergic sensitization. Clin Exp Allergy. 2000;30:194–200. doi: 10.1046/j.1365-2222.2000.00799.x. [DOI] [PubMed] [Google Scholar]
- 41.Marfortt DA, Josviack D, Lozano A, Cuestas E, Agüero L, Castro-Rodriguez JA. Differences between preschoolers with asthma and allergies in urban and rural environments. J Asthma. 2018;55:470–476. doi: 10.1080/02770903.2017.1339800. [DOI] [PubMed] [Google Scholar]
- 42.Schröder PC, Li J, Wong GW, Schaub B. The rural-urban enigma of allergy: what can we learn from studies around the world? Pediatr Allergy Immunol. 2015;26:95–102. doi: 10.1111/pai.12341. [DOI] [PubMed] [Google Scholar]
- 43.Vedanthan PK, Mahesh PA, Vedanthan R, Holla AD, Liu AH. Effect of animal contact and microbial exposures on the prevalence of atopy and asthma in urban vs rural children in India. Ann Allergy Asthma Immunol. 2006;96:571–578. doi: 10.1016/S1081-1206(10)63552-1. [DOI] [PubMed] [Google Scholar]
- 44.Wlasiuk G, Vercelli D. The farm effect, or: when, what and how a farming environment protects from asthma and allergic disease. Curr Opin Allergy Clin Immunol. 2012;12:461–466. doi: 10.1097/ACI.0b013e328357a3bc. [DOI] [PubMed] [Google Scholar]
- 45.Tun HM, Konya T, Takaro TK, Brook JR, Chari R, Field CJ, et al. Exposure to household furry pets influences the gut microbiota of infant at 3–4 months following various birth scenarios. Microbiome. 2017;5:40. doi: 10.1186/s40168-017-0254-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brick T, Schober Y, Böcking C, Pekkanen J, Genuneit J, Loss G, et al. ω-3 fatty acids contribute to the asthma-protective effect of unprocessed cow's milk. J Allergy Clin Immunol. 2016;137:1699–1706.e13. doi: 10.1016/j.jaci.2015.10.042. [DOI] [PubMed] [Google Scholar]
- 47.Kirchner B, Pfaffl MW, Dumpler J, von Mutius E, Ege MJ. MicroRNA in native and processed cow's milk and its implication for the farm milk effect on asthma. J Allergy Clin Immunol. 2016;137:1893–1895.e13. doi: 10.1016/j.jaci.2015.10.028. [DOI] [PubMed] [Google Scholar]
- 48.Waser M, Michels KB, Bieli C, Flöistrup H, Pershagen G, von Mutius E, et al. Inverse association of farm milk consumption with asthma and allergy in rural and suburban populations across Europe. Clin Exp Allergy. 2007;37:661–670. doi: 10.1111/j.1365-2222.2006.02640.x. [DOI] [PubMed] [Google Scholar]
- 49.House JS, Wyss AB, Hoppin JA, Richards M, Long S, Umbach DM, et al. Early-life farm exposures and adult asthma and atopy in the Agricultural Lung Health Study. J Allergy Clin Immunol. 2017;140:249–256.e14. doi: 10.1016/j.jaci.2016.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Park HJ, Kim EJ, Yoon D, Lee JK, Chang WS, Lim YM, et al. Prevalence of self-reported allergic diseases and IgE levels: a 2010 KNHANES analysis. Allergy Asthma Immunol Res. 2017;9:329–339. doi: 10.4168/aair.2017.9.4.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clayton T, Asher MI, Crane J, Ellwood P, Mackay R, Mitchell EA, et al. Time trends, ethnicity and risk factors for eczema in New Zealand children: ISAAC Phase Three. Asia Pac Allergy. 2013;3:161–178. doi: 10.5415/apallergy.2013.3.3.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nermes M, Niinivirta K, Nylund L, Laitinen K, Matomäki J, Salminen S, et al. Perinatal pet exposure, faecal microbiota, and wheezy bronchitis: is there a connection? ISRN Allergy. 2013;2013:827934. doi: 10.1155/2013/827934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sozańska B, Błaszczyk M, Pearce N, Cullinan P. Atopy and allergic respiratory disease in rural Poland before and after accession to the European Union. J Allergy Clin Immunol. 2014;133:1347–1353. doi: 10.1016/j.jaci.2013.10.035. [DOI] [PubMed] [Google Scholar]
- 54.Timm S, Frydenberg M, Janson C, Campbell B, Forsberg B, Gislason T, et al. The urban-rural gradient in asthma: a population-based study in Northern Europe. Int J Environ Res Public Health. 2015;13:E93. doi: 10.3390/ijerph13010093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Parsons MA, Beach J, Senthilselvan A. Association of living in a farming environment with asthma incidence in Canadian children. J Asthma. 2017;54:239–249. doi: 10.1080/02770903.2016.1206564. [DOI] [PubMed] [Google Scholar]
- 56.Han YY, Badellino HA, Forno E, Celedón JC. Rural residence, farming environment, and allergic diseases in Argentinean adolescents. Pediatr Pulmonol. 2017;52:21–28. doi: 10.1002/ppul.23511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Levin ME, Botha M, Basera W, Facey-Thomas HE, Gaunt B, Gray CL, et al. Environmental factors associated with allergy in urban and rural children from the South African Food Allergy (SAFFA) cohort. J Allergy Clin Immunol. 2020;145:415–426. doi: 10.1016/j.jaci.2019.07.048. [DOI] [PubMed] [Google Scholar]
- 58.Debarry J, Garn H, Hanuszkiewicz A, Dickgreber N, Blümer N, von Mutius E, et al. Acinetobacter lwoffii and Lactococcus lactis strains isolated from farm cowsheds possess strong allergy-protective properties. J Allergy Clin Immunol. 2007;119:1514–1521. doi: 10.1016/j.jaci.2007.03.023. [DOI] [PubMed] [Google Scholar]
- 59.Ege MJ, Mayer M, Normand AC, Genuneit J, Cookson WO, Braun-Fahrländer C, et al. Exposure to environmental microorganisms and childhood asthma. N Engl J Med. 2011;364:701–709. doi: 10.1056/NEJMoa1007302. [DOI] [PubMed] [Google Scholar]
- 60.Kirjavainen PV, Karvonen AM, Adams RI, Täubel M, Roponen M, Tuoresmäki P, et al. Farm-like indoor microbiota in non-farm homes protects children from asthma development. Nat Med. 2019;25:1089–1095. doi: 10.1038/s41591-019-0469-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gehring U, Bolte G, Borte M, Bischof W, Fahlbusch B, Wichmann HE, et al. Exposure to endotoxin decreases the risk of atopic eczema in infancy: a cohort study. J Allergy Clin Immunol. 2001;108:847–854. doi: 10.1067/mai.2001.119026. [DOI] [PubMed] [Google Scholar]
- 62.Braun-Fahrländer C, Riedler J, Herz U, Eder W, Waser M, Grize L, et al. Environmental exposure to endotoxin and its relation to asthma in school-age children. N Engl J Med. 2002;347:869–877. doi: 10.1056/NEJMoa020057. [DOI] [PubMed] [Google Scholar]
- 63.Gereda JE, Leung DY, Liu AH. Levels of environmental endotoxin and prevalence of atopic disease. JAMA. 2000;284:1652–1653. doi: 10.1001/jama.284.13.1652. [DOI] [PubMed] [Google Scholar]
- 64.Yen YC, Yang CY, Ho CK, Yen PC, Cheng YT, Mena KD, et al. Indoor ozone and particulate matter modify the association between airborne endotoxin and schoolchildren's lung function. Sci Total Environ. 2020;705:135810. doi: 10.1016/j.scitotenv.2019.135810. [DOI] [PubMed] [Google Scholar]
- 65.Schuijs MJ, Willart MA, Vergote K, Gras D, Deswarte K, Ege MJ, et al. Farm dust and endotoxin protect against allergy through A20 induction in lung epithelial cells. Science. 2015;349:1106–1110. doi: 10.1126/science.aac6623. [DOI] [PubMed] [Google Scholar]
- 66.Heederik D, von Mutius E. Does diversity of environmental microbial exposure matter for the occurrence of allergy and asthma? J Allergy Clin Immunol. 2012;130:44–50. doi: 10.1016/j.jaci.2012.01.067. [DOI] [PubMed] [Google Scholar]
- 67.Lee SY. Can the use of antibiotics alter the susceptibility to allergic diseases? Allergy Asthma Immunol Res. 2018;10:425–427. doi: 10.4168/aair.2018.10.5.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Loewen K, Monchka B, Mahmud SM, 't Jong G, Azad MB. Prenatal antibiotic exposure and childhood asthma: a population-based study. Eur Respir J. 2018;52:1702070. doi: 10.1183/13993003.02070-2017. [DOI] [PubMed] [Google Scholar]
- 69.Russell SL, Gold MJ, Hartmann M, Willing BP, Thorson L, Wlodarska M, et al. Early life antibiotic-driven changes in microbiota enhance susceptibility to allergic asthma. EMBO Rep. 2012;13:440–447. doi: 10.1038/embor.2012.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Han YY, Forno E, Badellino HA, Celedón JC. Antibiotic use in early life, rural residence, and allergic diseases in Argentinean children. J Allergy Clin Immunol Pract. 2017;5:1112–1118.e2. doi: 10.1016/j.jaip.2016.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kim HJ, Lee SH, Hong SJ. Antibiotics-induced dysbiosis of intestinal microbiota aggravates atopic dermatitis in mice by altered short-chain fatty acids. Allergy Asthma Immunol Res. 2020;12:137–148. doi: 10.4168/aair.2020.12.1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Galazzo G, van Best N, Bervoets L, Dapaah IO, Savelkoul PH, Hornef MW, et al. Development of the microbiota and associations with birth mode, diet, and atopic disorders in a longitudinal analysis of stool samples, collected from infancy through early childhood. Gastroenterology. 2020;158:1584–1596. doi: 10.1053/j.gastro.2020.01.024. [DOI] [PubMed] [Google Scholar]
- 73.Lee E, Kim BJ, Kang MJ, Choi KY, Cho HJ, Kim Y, et al. Dynamics of gut microbiota according to the delivery mode in healthy Korean infants. Allergy Asthma Immunol Res. 2016;8:471–477. doi: 10.4168/aair.2016.8.5.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ndibazza J, Mpairwe H, Webb EL, Mawa PA, Nampijja M, Muhangi L, et al. Impact of anthelminthic treatment in pregnancy and childhood on immunisations, infections and eczema in childhood: a randomised controlled trial. PLoS One. 2012;7:e50325. doi: 10.1371/journal.pone.0050325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chico ME, Vaca MG, Rodriguez A, Cooper PJ. Soil-transmitted helminth parasites and allergy: observations from Ecuador. Parasite Immunol. 2019;41:e12590. doi: 10.1111/pim.12590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wammes LJ, Mpairwe H, Elliott AM, Yazdanbakhsh M. Helminth therapy or elimination: epidemiological, immunological, and clinical considerations. Lancet Infect Dis. 2014;14:1150–1162. doi: 10.1016/S1473-3099(14)70771-6. [DOI] [PubMed] [Google Scholar]
- 77.Homaira N, Briggs N, Pardy C, Hanly M, Oei JL, Hilder L, et al. Association between respiratory syncytial viral disease and the subsequent risk of the first episode of severe asthma in different subgroups of high-risk Australian children: a whole-of-population-based cohort study. BMJ Open. 2017;7:e017936. doi: 10.1136/bmjopen-2017-017936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bisgaard H, Hermansen MN, Buchvald F, Loland L, Halkjaer LB, Bønnelykke K, et al. Childhood asthma after bacterial colonization of the airway in neonates. N Engl J Med. 2007;357:1487–1495. doi: 10.1056/NEJMoa052632. [DOI] [PubMed] [Google Scholar]
- 79.Kim HY, DeKruyff RH, Umetsu DT. The many paths to asthma: phenotype shaped by innate and adaptive immunity. Nat Immunol. 2010;11:577–584. doi: 10.1038/ni.1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lauener RP, Birchler T, Adamski J, Braun-Fahrländer C, Bufe A, Herz U, et al. Expression of CD14 and toll-like receptor 2 in farmers' and non-farmers' children. Lancet. 2002;360:465–466. doi: 10.1016/S0140-6736(02)09641-1. [DOI] [PubMed] [Google Scholar]
- 81.Ege MJ, Bieli C, Frei R, van Strien RT, Riedler J, Ublagger E, et al. Prenatal farm exposure is related to the expression of receptors of the innate immunity and to atopic sensitization in school-age children. J Allergy Clin Immunol. 2006;117:817–823. doi: 10.1016/j.jaci.2005.12.1307. [DOI] [PubMed] [Google Scholar]
- 82.Lin TH, Su HH, Kang HY, Chang TH. The interactive roles of lipopolysaccharides and dsRNA/viruses on respiratory epithelial cells and dendritic cells in allergic respiratory disorders: the hygiene hypothesis. Int J Mol Sci. 2017;18:E2219. doi: 10.3390/ijms18102219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yang Z, Zheng Z, Zhu L, Ren X, Li J. Role of A20 in respiratory diseases. Int J Respir. 2018;38:465–468. [Google Scholar]
- 84.Roduit C, Wohlgensinger J, Frei R, Bitter S, Bieli C, Loeliger S, et al. Prenatal animal contact and gene expression of innate immunity receptors at birth are associated with atopic dermatitis. J Allergy Clin Immunol. 2011;127:179–185. doi: 10.1016/j.jaci.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 85.Roy SR, Schiltz AM, Marotta A, Shen Y, Liu AH. Bacterial DNA in house and farm barn dust. J Allergy Clin Immunol. 2003;112:571–578. doi: 10.1016/s0091-6749(03)01863-3. [DOI] [PubMed] [Google Scholar]
- 86.van Strien RT, Engel R, Holst O, Bufe A, Eder W, Waser M, et al. Microbial exposure of rural school children, as assessed by levels of N-acetyl-muramic acid in mattress dust, and its association with respiratory health. J Allergy Clin Immunol. 2004;113:860–867. doi: 10.1016/j.jaci.2004.01.783. [DOI] [PubMed] [Google Scholar]
- 87.Wingender G, Rogers P, Batzer G, Lee MS, Bai D, Pei B, et al. Invariant NKT cells are required for airway inflammation induced by environmental antigens. J Exp Med. 2011;208:1151–1162. doi: 10.1084/jem.20102229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chang YJ, Kim HY, Albacker LA, Lee HH, Baumgarth N, Akira S, et al. Influenza infection in suckling mice expands an NKT cell subset that protects against airway hyperreactivity. J Clin Invest. 2011;121:57–69. doi: 10.1172/JCI44845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chuang YT, Leung K, Chang YJ, DeKruyff RH, Savage PB, Cruse R, et al. A natural killer T-cell subset that protects against airway hyperreactivity. J Allergy Clin Immunol. 2019;143:565–576.e7. doi: 10.1016/j.jaci.2018.03.022. [DOI] [PubMed] [Google Scholar]
- 90.Gereda JE, Leung DY, Thatayatikom A, Streib JE, Price MR, Klinnert MD, et al. Relation between house-dust endotoxin exposure, type 1 T-cell development, and allergen sensitisation in infants at high risk of asthma. Lancet. 2000;355:1680–1683. doi: 10.1016/s0140-6736(00)02239-x. [DOI] [PubMed] [Google Scholar]
- 91.Navarro S, Pickering DA, Ferreira IB, Jones L, Ryan S, Troy S, et al. Hookworm recombinant protein promotes regulatory T cell responses that suppress experimental asthma. Sci Transl Med. 2016;8:362ra143. doi: 10.1126/scitranslmed.aaf8807. [DOI] [PubMed] [Google Scholar]
- 92.Bancroft AJ, Levy CW, Jowitt TA, Hayes KS, Thompson S, Mckenzie EA, et al. The major secreted protein of the whipworm parasite tethers to matrix and inhibits interleukin-13 function. Nat Commun. 2019;10:2344. doi: 10.1038/s41467-019-09996-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ray A, Khare A, Krishnamoorthy N, Qi Z, Ray P. Regulatory T cells in many flavors control asthma. Mucosal Immunol. 2010;3:216–229. doi: 10.1038/mi.2010.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.McGuirk P, Mills KH. Pathogen-specific regulatory T cells provoke a shift in the Th1/Th2 paradigm in immunity to infectious diseases. Trends Immunol. 2002;23:450–455. doi: 10.1016/s1471-4906(02)02288-3. [DOI] [PubMed] [Google Scholar]
- 95.Wilson MS, Taylor MD, Balic A, Finney CA, Lamb JR, Maizels RM. Suppression of allergic airway inflammation by helminth-induced regulatory T cells. J Exp Med. 2005;202:1199–1212. doi: 10.1084/jem.20042572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Schaub B, Liu J, Höppler S, Schleich I, Huehn J, Olek S, et al. Maternal farm exposure modulates neonatal immune mechanisms through regulatory T cells. J Allergy Clin Immunol. 2009;123:774–782.e5. doi: 10.1016/j.jaci.2009.01.056. [DOI] [PubMed] [Google Scholar]
- 97.Lluis A, Depner M, Gaugler B, Saas P, Casaca VI, Raedler D, et al. Increased regulatory T-cell numbers are associated with farm milk exposure and lower atopic sensitization and asthma in childhood. J Allergy Clin Immunol. 2014;133:551–559. doi: 10.1016/j.jaci.2013.06.034. [DOI] [PubMed] [Google Scholar]
- 98.Melnik BC, John SM, Carrera-Bastos P, Schmitz G. Milk: a postnatal imprinting system stabilizing FoxP3 expression and regulatory T cell differentiation. Clin Transl Allergy. 2016;6:18. doi: 10.1186/s13601-016-0108-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gao X, Ren X, Wang Q, Yang Z, Li Y, Su Z, et al. Critical roles of regulatory B and T cells in helminth parasite-induced protection against allergic airway inflammation. Clin Exp Immunol. 2019;198:390–402. doi: 10.1111/cei.13362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Orivuori L, Loss G, Roduit C, Dalphin JC, Depner M, Genuneit J, et al. Soluble immunoglobulin A in breast milk is inversely associated with atopic dermatitis at early age: the PASTURE cohort study. Clin Exp Allergy. 2014;44:102–112. doi: 10.1111/cea.12199. [DOI] [PubMed] [Google Scholar]
- 101.Soto-Ramírez N, Karmaus W, Yousefi M, Zhang H, Liu J, Gangur V. Maternal immune markers in serum during gestation and in breast milk and the risk of asthma-like symptoms at ages 6 and 12 months: a longitudinal study. Allergy Asthma Clin Immunol. 2012;8:11. doi: 10.1186/1710-1492-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Oddy WH, Halonen M, Martinez FD, Lohman IC, Stern DA, Kurzius-Spencer M, et al. TGF-β in human milk is associated with wheeze in infancy. J Allergy Clin Immunol. 2003;112:723–728. doi: 10.1016/s0091-6749(03)01941-9. [DOI] [PubMed] [Google Scholar]
- 103.Cong Y, Feng T, Fujihashi K, Schoeb TR, Elson CO. A dominant, coordinated T regulatory cell-IgA response to the intestinal microbiota. Proc Natl Acad Sci U S A. 2009;106:19256–19261. doi: 10.1073/pnas.0812681106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Alexander KL, Katz J, Elson CO. CBirTox is a selective antigen-specific agonist of the Treg-IgA-microbiota homeostatic pathway. PLoS One. 2017;12:e0181866. doi: 10.1371/journal.pone.0181866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sun S, Li H, Yuan Y, Wang L, He W, Xie H, et al. Preventive and therapeutic effects of Trichinella spiralis adult extracts on allergic inflammation in an experimental asthma mouse model. Parasit Vectors. 2019;12:326. doi: 10.1186/s13071-019-3561-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Olszak T, An D, Zeissig S, Vera MP, Richter J, Franke A, et al. Microbial exposure during early life has persistent effects on natural killer T cell function. Science. 2012;336:489–493. doi: 10.1126/science.1219328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ver Heul A, Planer J, Kau AL. The human microbiota and asthma. Clin Rev Allergy Immunol. 2019;57:350–363. doi: 10.1007/s12016-018-8719-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bannier MA, van Best N, Bervoets L, Savelkoul PH, Hornef MW, van de Kant KD, et al. Gut microbiota in wheezing preschool children and the association with childhood asthma. Allergy. 2019;00:1–4. doi: 10.1111/all.14156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fujimura KE, Sitarik AR, Havstad S, Lin DL, Levan S, Fadrosh D, et al. Neonatal gut microbiota associates with childhood multisensitized atopy and T cell differentiation. Nat Med. 2016;22:1187–1191. doi: 10.1038/nm.4176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Arrieta MC, Stiemsma LT, Dimitriu PA, Thorson L, Russell S, Yurist-Doutsch S, et al. Early infancy microbial and metabolic alterations affect risk of childhood asthma. Sci Transl Med. 2015;7:307ra152. doi: 10.1126/scitranslmed.aab2271. [DOI] [PubMed] [Google Scholar]
- 111.Durack J, Kimes NE, Lin DL, Rauch M, McKean M, McCauley K, et al. Delayed gut microbiota development in high-risk for asthma infants is temporarily modifiable by Lactobacillus supplementation. Nat Commun. 2018;9:707. doi: 10.1038/s41467-018-03157-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Milani C, Duranti S, Bottacini F, Casey E, Turroni F, Mahony J, et al. The first microbial colonizers of the human gut: composition, activities, and health implications of the infant gut microbiota. Microbiol Mol Biol Rev. 2017;81:e00036-17. doi: 10.1128/MMBR.00036-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Croft AM, Bager P, Kumar S. Helminth therapy (worms) for allergic rhinitis. Cochrane Database Syst Rev. 2012:CD009238. doi: 10.1002/14651858.CD009238.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ottman N, Ruokolainen L, Suomalainen A, Sinkko H, Karisola P, Lehtimäki J, et al. Soil exposure modifies the gut microbiota and supports immune tolerance in a mouse model. J Allergy Clin Immunol. 2019;143:1198–1206.e12. doi: 10.1016/j.jaci.2018.06.024. [DOI] [PubMed] [Google Scholar]
- 115.Chua HH, Chou HC, Tung YL, Chiang BL, Liao CC, Liu HH, et al. Intestinal dysbiosis featuring abundance of Ruminococcus gnavus associates with allergic diseases in infants. Gastroenterology. 2018;154:154–167. doi: 10.1053/j.gastro.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 116.Thorsen J, Rasmussen MA, Waage J, Mortensen M, Brejnrod A, Bønnelykke K, et al. Infant airway microbiota and topical immune perturbations in the origins of childhood asthma. Nat Commun. 2019;10:5001. doi: 10.1038/s41467-019-12989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Chiu CY, Cheng ML, Chiang MH, Kuo YL, Tsai MH, Chiu CC, et al. Gut microbial-derived butyrate is inversely associated with IgE responses to allergens in childhood asthma. Pediatr Allergy Immunol. 2019;30:689–697. doi: 10.1111/pai.13096. [DOI] [PubMed] [Google Scholar]
- 118.Lewis G, Wang B, Shafiei Jahani P, Hurrell BP, Banie H, Aleman Muench GR, et al. Dietary fiber-induced microbial short chain fatty acids suppress ILC2-dependent airway inflammation. Front Immunol. 2019;10:2051. doi: 10.3389/fimmu.2019.02051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Uchiyama K, Naito Y, Takagi T. Intestinal microbiome as a novel therapeutic target for local and systemic inflammation. Pharmacol Ther. 2019;199:164–172. doi: 10.1016/j.pharmthera.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 120.Frati F, Salvatori C, Incorvaia C, Bellucci A, Di Cara G, Marcucci F, et al. The role of the microbiome in asthma: the gut-lung axis. Int J Mol Sci. 2018;20:E123. doi: 10.3390/ijms20010123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Anand S, Mande SS. Diet, microbiota and gut-lung connection. Front Microbiol. 2018;9:2147. doi: 10.3389/fmicb.2018.02147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Dzidic M, Abrahamsson TR, Artacho A, Collado MC, Mira A, Jenmalm MC. Oral microbiota maturation during the first 7 years of life in relation to allergy development. Allergy. 2018;73:2000–2011. doi: 10.1111/all.13449. [DOI] [PubMed] [Google Scholar]
- 123.Di Cicco M, Pistello M, Jacinto T, Ragazzo V, Piras M, Freer G, et al. Does lung microbiome play a causal or casual role in asthma? Pediatr Pulmonol. 2018;53:1340–1345. doi: 10.1002/ppul.24086. [DOI] [PubMed] [Google Scholar]
- 124.Arrieta MC, Arévalo A, Stiemsma L, Dimitriu P, Chico ME, Loor S, et al. Associations between infant fungal and bacterial dysbiosis and childhood atopic wheeze in a nonindustrialized setting. J Allergy Clin Immunol. 2018;142:424–434.e10. doi: 10.1016/j.jaci.2017.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]