Abstract
Background
China has experienced rapid economic growth and reduced poverty, but the associated changes of BMI categories of the Chinese population in recent years are unclear.
Methods
We collected data from two-round cross-sectional National Health Service Surveys (NHSSs) conducted in China in 2013 and 2018. All family members with BMI available from the households sampled in NHSSs were included. We analyzed the standardized prevalence and changes of obesity and overweight by year, age, sex, and urban-rural area, and further identified risk factors for obesity and overweight.
Findings
273,688 individuals were included in 2013 and 25,6304 included in 2018. The standardized prevalence of obesity and overweight in adults were 19.3% (95%CI 19.1–19.4%) in 2013 and 25.6% (95%CI 25.3–25.8%) in 2018, versus 19.4% (95%CI 19·1–19.8%) in children and adolescents in 2013 and 15.8% (95%CI 15.5–16.1%) in 2018. The standardized prevalence of obesity and overweight was 16.9% (95%CI 16.0–17.3%) in young adults aged 19–29 in 2018, 48.2% higher than that in 2013 (11.4% [95%CI 11.0–11.6%]). Although the obesity and overweight prevalence was higher in urban areas, the growth rate in rural areas was 1.8 times higher than that in urban areas. Low education levels, low-income quintiles, marital status, alcohol consumption and former-smoking status were associated with higher obesity and overweight prevalence in adults.
Interpretation
The rapidly increasing prevalence in young adults may lead to the growing chronic disease burden in the future, to the detriment of recent economic gains of rural families.
Funding
National Health Commission of the People's Republic of China.
Keywords: Obesity, Chronic diseases, Prevalence, China
Research in context.
Evidence before this study
The previous studies were either performed in limited number of provinces with a relatively small sample size or targeted specific populations, and none of them reported the most recent national-wide changes of a comprehensive set of BMI categories in China.
Added value of this study
We depicted the most recent changes of BMI categories in the whole population in mainland China. Low education levels, low-income quintiles, marital status, alcohol consumption and former-smoking were associated with higher obesity and overweight prevalence in adults.
Implications of all the available evidence
China is facing a huge double burden of malnutrition as well as the associated health problems when solving the subsistence problem in rural areas. More practical and effective policies should specifically target young adults, especially in rural China.
Alt-text: Unlabelled box
1. Introduction
Obesity and overweight is a major global public health problem [1], and an important preventable risk factor for major non-communicable diseases (NCDs) including cardiovascular diseases, stroke, and certain cancers [2,3], which are the top three causes of adult mortality in China and worldwide [4]. Childhood obesity and overweight are associated with increased risk of elevated lifetime morbidity and premature mortality [5,6]. With this in mind, China started its first National-wide survey of obesity, overweight and underweight in 1959. The prevalence of obesity and overweight remained very low in 1970s and 1980s for the entire population, being only 7.8% for adults and 0.6% for children and adolescents in 1985 [7,8]. Even in the early 1990s, the obesity and overweight prevalence was still very low for adults in China [7,9]. However, some studies performed after the year 2000 have indicated a rapid increase in the prevalence of obesity and overweight in the Chinese population from 1989 to 2014 [10,11].
Socioeconomic developments are apt to bring significant changes in BMI categories in the population. In the process of China's recent economic development, the prevalence of underweight in children and adolescents had certainly decreased, but the prevalence of obesity and overweight had increased, especially in rural areas [12]. Other studies also suggested the obesity prevalence was generally higher in rural areas than in urban areas in the United States [[13], [14], [15]]. At the start of China's rapid economic development and commitment to poverty reduction, the socioeconomic level varied widely across regions. However, the effects of these transformation on BMI categories in recent years was unclear.
National Health Commission (NHC) of the People's Republic of China organized the National Health Services Surveys (NHSSs), which started to record BMI and other demographics of the participants in 2013. The aim here was to show the most recent changes of a comprehensive set of BMI categories extending from underweight to obesity in a large sample of the whole population stratified by age, gender and geographic regions. Moreover, factors related to adults and children and adolescents’ excess bodyweight were investigated while exploring the association between BMI categories and NCDs. In this study, we report the findings of this project during the interval 2013–2018.
2. Methods
2.1. Data source and sample
NHSSs aimed to provide information about Chinese individuals’ health status for policy makers, covering all 31 provinces, autonomous regions, and municipalities in the mainland of China. As described previously [16,17], we performed a multistage stratified cluster sampling method in these surveys. First, we divided mainland China into east, central and west regions. Then we sampled counties from each region stratified by urban and rural areas, and the households from each county to cover 0.02% of the entire population, taking account a 5% nonresponder rate. We sampled 78 counties in urban areas and 78 counties in rural areas in 2013 and 82 counties in urban areas and 74 counties in rural areas in 2018. Second, we selected five streets or townships in each urban or rural county, and then two communities or villages from each street or township, respectively. In each community or village, which typically contained 500–3000 households, we randomly selected 60 households from each of them. Ten standby households in each administrative community or village were also selected, so that we could resort to them in the event of failure to interview the originally selected households, we would move onto one of ten standby households. A total of 93,613 households were selected for survey of 2013 and 94076 for survey of 2018. All members with body weights and heights available were eligible in this study (Fig. 1).
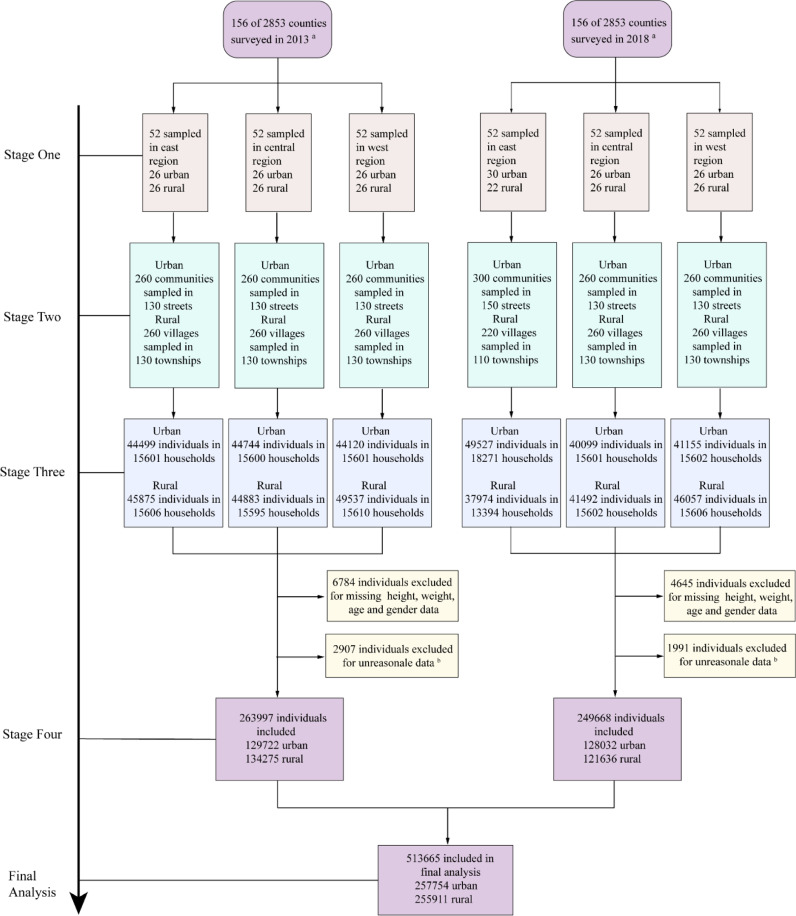
Fig. 1.
Study profile. NHSS=National Health Service Surveys in China. aA multistage stratified cluster sampling method was used in these surveys. The mainland China was first divided into east, central and west regions. We sampled 156 counties each year stratified by region and residence. bUnreasonable data with z scores of height for age <−6.0 or >6.0 (age<19), weight for age <−6.0 or >6.0(age<10), and BMI for age <−6.0 or >6.0(age<19) were excluded from the final analysis. Missing values for height, weight, gender, or age were also excluded in the final analysis.
The NHSS were approved by the institutional review board of the Chinese National Bureau of Statistics. At the last stage of sampling, all selected households would receive a notice describing the purpose and process of the study, and the investigation continued only if they agree to participate. All respondents provided their consents to participate in the survey before the interview.
2.2. Procedure
Local healthcare workers from hospitals in the selected communities or townships were trained to administer the face-to-face interviews based on a structured questionnaire included information about demographic characteristic, socioeconomic characteristic, and health related behavior of participants at both rounds of the survey.
Individuals’ body weight and height were measured with standardised techniques and equipment. For infants and toddlers aged 0–2, the recumbent length was measured instead of standing height. The BMI was calculated as dividing body weight (in kilograms) by squared height or length (in meters). We defined adults with BMI <18,5 kg/m² as underweight, those with BMI ≥25 and <30 kg/m² as overweight, and those with BMI ≥30kg/m² as obese according to the WHO's recommendation [18,19]. For children and adolescents under 18 years old, the criterion for underweight, obesity and overweight were based on the WHO growth standards 2006 for children aged 0–5 [20,21] and the WHO growth standards 2007 for children and adolescents aged 6–18 [21,22].
Former smokers were defined as those who had smoke 100 or more cigarettes during their entire life before having stopped at the time of survey [17]. Current smokers were defined as those who had smoked 100 or more cigarettes and continued smoking [17]. Alcohol consumption was defined as having had one drink containing alcohol in the past 12 months. Physical activity was defined as having done recreational physical activity at least once a week in the past month. To calculate income quartiles, we recorded the total disposable income from household reports of wages, government subsidies received, and any other sources of income. In rural areas, we subtracted business and agricultural investments from the gross income. Self-reported chronic diseases including hypertension, diabetes, ischemic heart disease, cerebrovascular disease, liver and gall bladder disease, chronic respiratory disease, cancer, and gastrointestinal disease were recorded at each round of the survey (Appendixs 1 and 2). The interviewers had to provide relevant medical records from doctors as evidence for diagnosis. Doctors from higher-level health institutions, i.e. Grade-A Tertiary Hospitals in the selected regions supervised the diagnoses, and the investigator filled in the disease code in the questionnaire according to the international Classification of Diseases 10 [17].
2.3. Statistical analysis
All data were documented on a written questionnaire and then double entered into an online system provided by the NHC of the People's Republic of China. Biologically implausible z-scores of height for age <−6.0 or >6.0, weight for age <−6.0 or >6.0, and BMI for age <−6.0 or >6.0 were excluded from the final analysis according to the methods prescribed by WHO AnthroPlus and previous studies [23,24] Records with missing values either for height, weight, gender, or age were also excluded in the final analysis. The analyses were performed separately for adults (age>18 years) and children or adolescents (age ≤18 years). We performed the statistical analysis using SAS 9.4, and consider as significant a two-side P value <0·05. Age and sex standardised prevalence of BMI categories based on the 2010 national census was presented for the overall population and subgroups stratified by geographical regions (east, central, west) and urbanization (urban, rural), as well as by provinces. We combined obesity and overweight together and used Pearson Chi-squared tests to compare the prevalence of the BMI categories across subgroups. We applied Joinpoint models to analyse the percent change of obesity and overweight prevalence as a function of increasing age [17,25].
We then constructed multiple logistic regression models to estimate the odds ratios (ORs) and 95%CI of all recorded variables potentially associated with obesity and overweight. To analyse the influence of family setting on the prevalence of obesity and overweight in children and infants’ obesity, we applied a logistic regression model involving the family factors, such as marital status, education, employment, alcohol consumption, income quartiles, and physical activity. We also constructed multiple logistic regression models to explore the association between BMI categories (obesity and overweight vs. health; underweight vs. health) and the total burden of NCDs or each category of NCD separately from the pooled data of the two-round surveys.
2.4. Role of the funding source
The sponsor of this study had no role in study design, data collection, data analysis, data interpretation and writing of this study. All authors had access to the data and were responsible for the decision to submit the manuscript for publication.
3. Results
A total of 273,688 individuals were interview and measured in 2013 and 256,304 individuals in 2018. Among them, 6784 (2.5%) in 2013 and 4645 (1.8%) in 2018 were excluded due to missing values of either height, weight, gender or age. In addition, 2907 (1.0%) individuals in 2013 and 1991 (0.8%) individuals in 2018 were excluded for reporting unreasonable data. In the end, 257,754 individuals in 2013 and 255,911 individuals in 2018 were included in the final analysis (Fig. 1). The basic characteristics of the individuals of the demographic characteristic, socioeconomic characteristic, and health related behaviors across the survey years are shown in the Appendix 3.
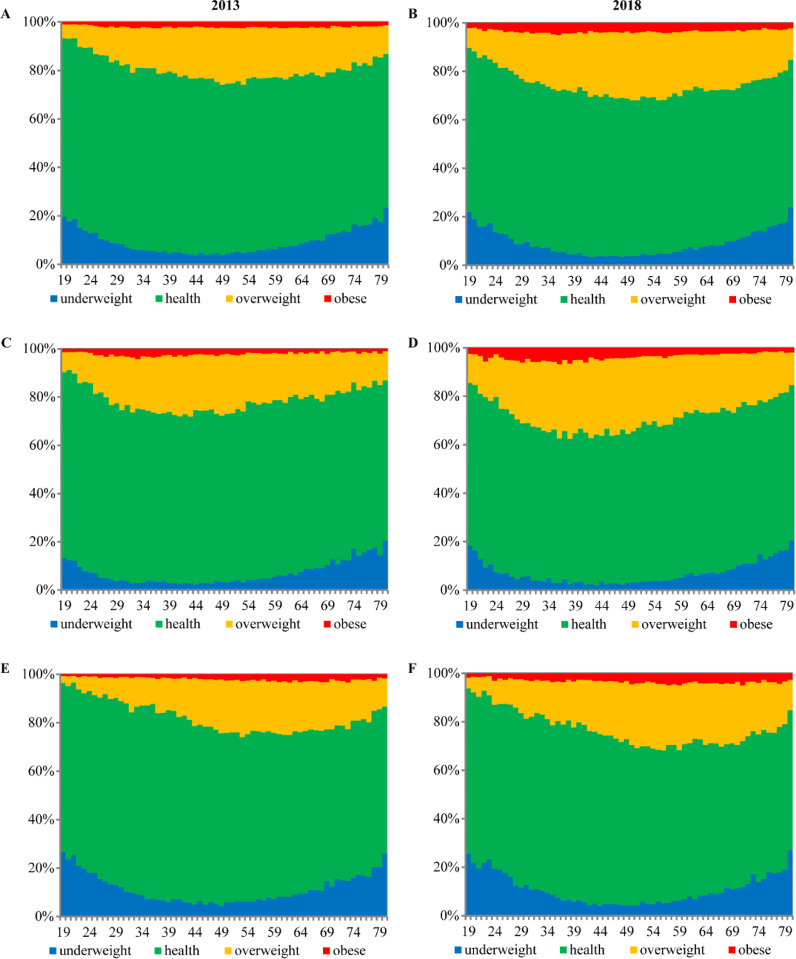
Among all Chinese adults, the standardised prevalence of obesity and overweight was 19.3% (95%CI, 19.1–19.4%) in 2013, and 25.6% (95%CI, 25.3–25.8%) in 2018. Meanwhile, the prevalence of underweight was relatively stable, being 8·4% in 2013 and 8.2% in 2018. Males had a significant higher prevalence of obesity and overweight than females did in both 2013 (22.2% vs 16.7%) and 2018 (29.9% vs 21.8%, both P<0.001). The peak prevalence of obesity and overweight occurred at the age of 40 in the male population, which was 10 years earlier than in the female population. Urban adults had a higher prevalence of obesity and overweight compared with rural adults in both survey years. This prevalence in urban areas was 25.4% higher in 2018 compared to 2013 (26.5% vs 21.4%, P<0.001), and 44·7% in 2018 compared to 2013 in rural area (24.6% vs 17.1%, P<0.001). Adults in east China had the highest prevalence of obesity and overweight (21.5% in 2013 and 27.6% in 2018), while adults in west China had the lowest (16.8% in 2013 and 23.3% in 2018) (Table 1 and Appendix 4). The standardized prevalence of the BMI Category in adult population from 2013 to 2018 in China according to Asian criterion showed the similar pattern of changes (Appendix 5).
Table 1.
Standardised prevalence of BMI Categories in Chinese population in 2013 and 2018.
| BMI Categories 2013 Standardised prevalencea (%, 95%CI) |
BMI Categories 2018 Standardised prevalencea (%, 95%CI) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Underweight | Health | Overweight | Obesity | Underweight | Health | Overweight | Obesity | |
| Adults | 8.4 (8.2-8.5) | 72.3 (72.2-72.6) | 17.2 (17.0-17.4) | 2.1 (2.0-2.1) | 8.2 (8.1-8.4) | 66.2 (66.0-66.5) | 21.9 (21.7-22.1) | 3.7 (3.6-3.8) |
| Age, y | ||||||||
| 19–29 | 13.4 (13.0-13.8) | 75.2 (74.7-75.7) | 9.9 (9.6-10.2) | 1.5 (1.4-1.6) | 14.1 (13.6-14.7) | 69.0 (68.3-69.7) | 13.8 (13.3-14.3) | 3.1 (2.9-3.4) |
| 30–39 | 5.8 (5.5-6.0) | 74.3 (73.8-74.8) | 17.6 (17.2-18.0) | 2.3 (2.1-2.5) | 6.1 (5.9-6.4) | 66.8 (66.2-67.3) | 22.7 (22.2-23.2) | 4.4 (4.2-4.7) |
| 40–49 | 4.3 (4.1-4.5) | 72.3 (71.9-72.7) | 21.2 (20.8-21.6) | 2.3 (2.1-2.4) | 3.7 (3.6-3.9) | 66.1 (65.6-66.6) | 26.3 (25.8-26.7) | 3.9 (3.7-4.1) |
| 50–59 | 5.3 (5.1-5.5) | 70.7 (70.2-71.1) | 21.7 (21.4-22.1) | 2.3 (2.2-2.4) | 4.6 (4.4-4.7) | 64.3 (63.9-64.8) | 27.2 (26.8-27.6) | 3.9 (3.7-4.1) |
| 60–69 | 8.6 (8.3-8.9) | 69.2 (68.7-69.7) | 19.8 (19.4-20.2) | 2.4 (2.2-2.5) | 7.8 (7.5-8.1) | 64.7 (64.2-65.1) | 24.2 (23.8-24.6) | 3.3 (3.2-3.5) |
| ≥70 | 17.4 (16.9-17.8) | 65.7 (65.1-66.3) | 15.1 (14.7-15.6) | 1.8 (1.6-1.9) | 16.7 (16.2-17.1) | 61.9 (61.4-62.5) | 18.7 (18.2-19.2) | 2.7 (2.5-2.9) |
| Sex | ||||||||
| Male | 5.7 (5.6-5.9) | 72.3 (71.9-72.5) | 19.7 (19.4-19.9) | 2.3 (2.2-2.4) | 6.0 (5.8-6.2) | 64.4 (64.1-64.8) | 25.4 (25.1-25.7) | 4.2 (4.0-4.3) |
| Female | 11.0 (10.8-11.2) | 72.5 (72.2-72.8) | 14.7 (14.5-14.9) | 1.8 (1.7-1.9) | 10.6 (10.3-10.8) | 68.0 (67.7-68.3) | 18.3 (18.1-18.6) | 3.1 (3.0-3.3) |
| Residence | ||||||||
| Urban | 8.1 (7.9-8.3) | 70.5 (70.2-70.8) | 18.9 (18.7-19.1) | 2.5 (2.4-2.6) | 7.8 (7.6-8.0) | 65.7 (65.4-66.1) | 22.7 (22.4-23.0) | 3.8 (3.6-3.9) |
| Rural | 8.7 (8.5-8.9) | 74.2 (73.9-74.4) | 15.5 (15.3-15.7) | 1.6 (1.6-1.7) | 8.8 (8.5-9.0) | 66.6 (66.3-67.0) | 21.1 (20.8-21.4) | 3.5 (3.4-3.7) |
| Region | ||||||||
| East | 7.2 (7.0-7.4) | 71.3 (71.0-71.7) | 19.1 (18.7-19.3) | 2.4 (2.3-2.5) | 7.5 (7.3-7.8) | 65.1 (64.7-65.5) | 23.2 (22.9-23.6) | 4.2 (4.0-4.3) |
| Centre | 8.3 (8.0-8.5) | 72.2 (71.9-72.6) | 17.5 (17.2-17.8) | 2.0 (1.9-2.2) | 8.0 (7.7-8.3) | 66.0 (65.5-66.4) | 22.3 (21.9-22.7) | 3.7 (3.6-3.9) |
| West | 9.7 (9.5-9.9) | 73.5 (73.2-73.8) | 15.1 (14.8-15.3) | 1.7 (1.6-1.8) | 9.3 (9.0-9.5) | 67.4 (67.0-67.8) | 20.1 (19.8-20.5) | 3.2 (3.0-3.3) |
| Children and Adolescents | 6.1 (5.9-6.3) | 74.5 (74.1-74.9) | 13.0 (12.7-13.3) | 6.4 (6.2-6.7) | 7.4 (7.2-7.7) | 76.8 (76.4-77.2) | 11.2 (10.9-11.5) | 4.6 (4.4-4.8) |
| Age, y | ||||||||
| 0-5 | 7.4 (7.0-7.8) | 70.6 (69.8-71.4) | 14.2 (13.6-14.8) | 7.8 (7.4-8.3) | 7.9 (7.4-8.3) | 77.3 (76.6-78.0) | 10.1 (9.7-10.6) | 4.7 (4.4-5.1) |
| 6-18 | 5.7 (5.5-6.0) | 73.9 (73.4-74.4) | 13.7 (13.3-14.1) | 6.7 (6.4-7.0) | 8.0 (7.7-8.3) | 72.5 (72.1-73.1) | 13.5 (13.1-13.9) | 6.0 (5.6-6.2) |
| Sex | ||||||||
| Boys | 6.5 (6.2-6.9) | 70.6 (70.0-71.1) | 14.7 (14.3-15.2) | 8.2 (7.9-8.5) | 7.8 (7.5-8.2) | 72.8 (72.2-73.4) | 13.5 (13-13.9) | 5.9 (5.7-6.2) |
| Girls | 5.6 (5.3-5.9) | 79.1 (78.5-79.5) | 10.9 (10.5-11.3) | 4.4 (4.2-4.7) | 7.0 (6.6-7.3) | 81.4 (80.9-81.9) | 8.6 (8.3-9.0) | 3.0 (2.8-3.2) |
| Residence | ||||||||
| Urban | 6.2 (5.8-6.5) | 75.5 (74.9-76.1) | 12.7 (12.2-13.1) | 5.6 (5.4-6.0) | 7.3 (6.9-7.7) | 77.6 (77.0-78.2) | 11.3 (10.8-11.7) | 3.8 (3.6-4.1) |
| Rural | 6.0 (5.8-6.3) | 73.7 (73.2-74.2) | 13.3 (12.9-13.7) | 7.0 (6.7-7.3) | 7.5 (7.2-7.9) | 76.0 (75.4-76.5) | 11.3 (10.9-11.7) | 5.2 (5.0-5.5) |
| Region | ||||||||
| East | 5.7 (5.3-6.1) | 75.4 (74.7-76.1) | 13.2 (12.6-13.8) | 5.7 (5.4-6.1) | 7.3 (6.8-7.8) | 77.5 (76.8-78.2) | 11.2 (10.7-11.8) | 4.0 (3.7-4.3) |
| Centre | 5.9 (5.6-6.3) | 73.3 (72.6-73.9) | 13.9 (13.4-14.5) | 6.9 (6.5-7.3) | 7.3 (6.9-7.8) | 75.5 (74.8-76.2) | 12.4 (11.8-12.9) | 4.8 (4.5-5.1) |
| West | 6.6 (6.2-7.0) | 74.8 (74.1-75.4) | 12.0 (11.6-12.5) | 6.6 (6.3-7.0) | 7.6 (7.2-8.1) | 77.1 (76.4-77.7) | 10.4 (10.0-10.9) | 4.9 (4.6-5.2) |
BMI: Body mass index (calculated as weight in kilograms divided by height in meters squared). For infants and toddlers aged 0–2, the recumbent length was measured instead of height. a The prevalence of different BMI status is standardised by age and sex based on the 2010 national census.
We defined adults with BMI <18.5 kg/m² as underweight, those with BMI ≥25 and <30 kg/m² as overweight, and those with BMI ≥30 kg/m² as obese. We defined individuals aged 0-5 with weight-for-height more than 3 standard deviation (SD) above the WHO Child Growth Standards median as obese, 2SD to 3SD above median as overweight, in the range of 2SD below the median to 2SD above the median as healthy weight, and more than 2SD below the median as underweight. We defined those aged 6–18 with BMI-for-age more than 2SD above the WHO Child Growth Standards median as obese, 1SD to 2SD above the median as overweight, in the range of 2SD below the median to 1SD above the median as healthy weight, and more than 2SD below the median as underweight for children and adolescents aged 6-18.
Values are standardised prevalence and its 95% CI. P values were obtained from Chi-square test for the differences among different BMI categories across subgroups between 2013 and 2018. Test was significant (P <0.001) from Chi-square test across different BMI categories by age, sex, residence, region in 2013 and 2018 separately.
The standardised prevalence of obesity and overweight was declined in children and adolescents, from 19.4% (95%CI, 19.1–19.8%) in 2013 to 15.8% (95%CI, 15·5–16.1%) in 2018 (p<0.001). In the meantime, the standardised prevalence of underweight was 6.1% (95%CI, 5·9–6.3%) in 2013 and 7.4% (95%CI, 7.2–7.7%) in 2018. The height increase exceeded that of weight for children and adolescents during the five-year surveying interval (Appendixs 6 and 7). In 2013, the prevalence of obesity and overweight were higher in boys than that in girls (22.9% vs 15.4%; P<0.001). The prevalence of obesity and overweight in children and adolescents in 2018 showed a similar gender difference. Compared with urban area, the rural children and adolescents showed a higher obesity and overweight prevalence (20·3% vs 18·3 % in 2013 and 16·5% vs 15·1% in 2018; both P<0·001). From east to west, there was declining prevalence of obesity and overweight in children and adolescents from 18·9% (95%CI, 18·3-19·6%) in the east, 20·8% (95%CI, 20·2-21·4%) in central China, and 18·7% (95%CI, 18·1-19·2%) in the west in 2013 to 15·2% (95%CI, 14·6-15·8%) in the east, 17·2% (95%CI, 16·6-17·8%) in central China, and 15·3% (95%CI, 14·8-15·8%) in the east in 2018. Children and adolescents from central China had the highest prevalence of obesity and overweight during the surveying years (Table 1 and Appendix 8).
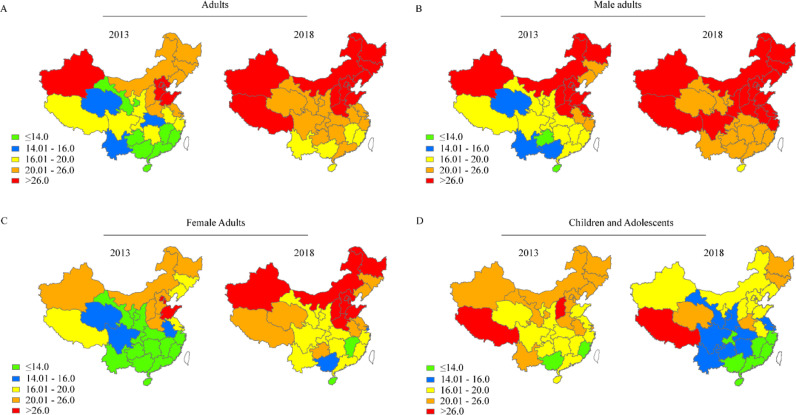
The standardised prevalence of obesity and overweight in adults varied in different provinces of China, ranging from 16·7% (95%CI, 15·4-18·1%) in Hainan province to 38·0% (95%CI, 36·1-39·9%) in Tianjin in 2018. By gender, the prevalence varied from 19·8% in Hainan province to 43·6% in Beijing for males, and from 13·1% in Jiangxi province to 35·0% in Tianjin for females in 2018. The standardised prevalence of obesity and overweight in adults were from 1·7% to 46·2% higher in 2018 than that in 2013 in all provinces in Mainland China. A substantial number of provinces showed a change pattern matching that of the national findings. We also identified three other patterns of obesity and overweight prevalence changes from 2013 to 2018. The first pattern entailed obesity and overweight prevalence well below the national average and a low increased rate, like Shanghai and Jiangsu province in the east region. The second pattern associates obesity and overweight prevalence well below the national average and a rate of increase exceeding the national average, like Guizhou and Qinghai provinces. The third pattern entailed an obesity and overweight prevalence well above the national average with a low rate of increase from 2013 to 2018, like Beijing and Shandong provinces (Fig. 2 and Appendix 9).
Fig. 2.
The geographic distribution of obesity and overweight prevalence in mainland China in 2013 and 2018. A: Prevalence of obesity and overweight in the adult population in 2013 (left) and in 2018 (right) B: Male adult population in 2013 (left) and in 2018 (right). C: Female adult population in 2013 (left) and in 2018 (right). D: Children and Adolescents in 2013 (left) and in 2018 (right). Age- and gender- standardised prevalence of obesity and overweight was calculated for each province in each survey according to the 2010 National population Census. Hong Kong, Macao, and Taiwan were not included in this survey and showed in grey colour. We divided the provinces into five levels according to the quartiles of the obesity and overweight prevalence in total adult population in 2013.
In China, the age and gender specific obesity and overweight prevalence among adults increased sharply in those aged 19–29 years old, then peaked in those aged 30–53 and declined in those aged 54 or older in the two-round surveys. The age specific obesity and overweight prevalence in young adults aged 19–29 was 48.2% higher in 2018 than that in 2013 (16.9% vs 11.4%). By gender, the prevalence was 44.5% higher in 2018 than that in 2013 (28.4% vs 19.5%) among males and 53.7% higher in 2018 than that in 2013 among females (14.5% vs 9.4%) (Fig. 3 and Appendix 10). The prevalence of obesity and overweight peaked at the age of 36 in the rural population, which was 5 years earlier than that of the urban population.
Fig. 3.
Age and gender specific prevalence of underweight, obesity and overweight in adult population in China in 2013 and 2018.
A,B: Age specific prevalence of underweight, obesity and overweight for the adult population in China in 2013 (A) and in 2018 (B).
C,D: Age specific prevalence of underweight, obesity and overweight for male adults in 2013 (C) and in 2018 (D).
E,F: Age specific prevalence of underweight, obesity and overweight for female adults in China in 2013 (E) and in 2018 (F).
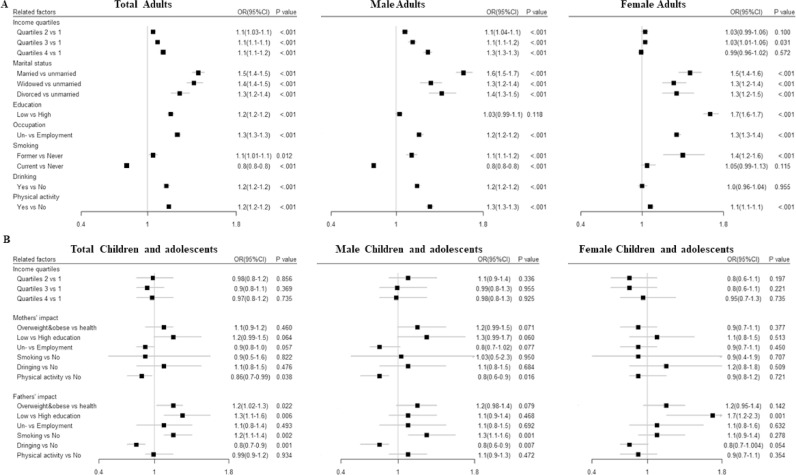
Factors related to BMI status among adults in China are shown in Fig. 4. We found that alcohol consumption was associated with an increased prevalence of obesity and overweight in male adults, with an OR of 1.2(95%CI 1.2–1.2). Besides, the adult males with higher income quintiles tended to have a higher obesity and overweight prevalence. In adult females, lower education levels (junior high school or less) tended to be associated with higher obesity and overweight prevalence compared with those with higher education levels, with an OR of 1.7(95%CI 1.6–1.7). The age-adjusted retired and unemployed people had a higher obesity and overweight prevalence than the employed population, with an OR of 1.3(95%CI 1.3–1.3), 1.2(95%CI 1.2–1.2) for adult males and 1.3(95%CI 1.3–1.4) for adult females. Higher obesity and overweight prevalence were found among those who were married with an OR of 1.5 (95% CI 1.4–1.5), or had physical activity with an OR of 1.2(95%CI 1.2–1.2). The obesity and overweight fathers were related to higher BMI of their children (OR 1.2; 95% CI,1.02–1.3). We also observed that lower education level of the fathers was associated with higher prevalence of obesity and overweight in their children (OR 1.3; 95% CI, 1.1–1.6). Fathers who reported drinking had children with lower BMI (OR 0.8; 95% CI, 0.7–0.9). Finally, boys whose father smoked had a higher risk of obesity and overweight (OR 1.3; 95% CI, 1.1–1.6), but girls did not.
Fig. 4.
Factors related to obesity and overweight in Chinese population. A: Factors related to obesity and overweight in total adult population (left), male adult population (middle) and female adult population (right) in China. B: Factors related to obesity and overweight in children and adolescents (left), boys (middle) and girls (right) in China. Multiple logistic regression models were used to estimate the association between obesity and overweight with all potentially associated variables for total and sex-specific populations. In the adult population, the models included geographical regions, urbanization, income quartiles, sex, age, marital status, education, employment, smoking, alcohol drinking and physical activity. Among children aged 0-5 the models included parental levels of education, employment, smoking, alcohol drinking, and physical activity as well as the family income quartiles, geographical regions, urbanization. The underweight population were not included in these models. Adjusted Odds ratios (ORs) and 95%CI from logistic regression were presented with the Forest plot.
Based on our survey data, the prevalence of chronic diseases increased sharply in both male and female population from 2013 to 2018 (Table 2 and appendix 11). Meanwhile, higher prevalence of chronic diseases was found in obesity and overweight adults compared with normal weight individuals, with an OR of 2.0 (95%CI 2.0–2.0). We observed the highest OR for hypertension (OR 2.5, 95%CI 2.4-2.5), followed by diabetes (OR 1.9, 95%CI 1.9–2·0) and ischemia heart diseases (OR 1.6 95%CI 1.5–1.7). The prevalence of underweight was also associated with certain chronic diseases, i.e. cancer (OR 2.3, 95%CI 2.0–2.6), COPD (OR 2.0, 95%CI 1.8–2.1) and gastrointestinal diseases (OR 1.7, 95%CI 1.6–1.8). Relative to those with normal BMI, liver and gall disease were associate with underweight as well as obesity and overweight, especially for male adults, with an OR of 1.4(95%CI, 1.1–1.6) and 1.3(95%CI, 1.1–1.4) respectively.
Table 2.
Associate between BMI categories and Chronic diseases in adult population.
| Disease | Total population |
Male |
Female |
|||
|---|---|---|---|---|---|---|
| Underweight vs Health OR (95%CI) | Obesity and overweight vs Health OR (95%CI) | Underweight vs Health OR (95%CI) | Obesity and overweight vs Health OR (95%CI) | Underweight vs Health OR (95%CI) | Obesity and overweight vs Health OR (95%CI) | |
| Total | 0.8 (0.80.9) | 2.0 (2.0-2.0) | 0.9 (0.9-0.99) | 2.0 (1.9-2.0) | 0.8 (0.7-0.8) | 1.9 (1.9-2.0) |
| Hypertension | 0.6 (0.5-0.6) | 2.5 (2.4-2.5) | 0.6 (0.5-0.6) | 2.5 (2.4-2.6) | 0.5 (0.5-0.5) | 2.3 (2.3-2.4) |
| Diabetes | 0.5 (0.5-0.6) | 1.9 (1.9-2.0) | 0.5 (0.5-0.6) | 1.8 (1.8-1.9) | 0.5 (0.5-0.6) | 1.9 (1.8-2.0) |
| Ischemic heart disease | 0.9 (0.8-0.96) | 1.6 (1.5-1.7) | 0.8 (0.7-0.9) | 1.7 (1.6-1.8) | 0.9 (0.8-1.0) | 1.5 (1.4-1.6) |
| Cerebrovascular disease | 0.9 (0.8-0.9) | 1.3 (1.2-1.4) | 0.9 (0.8-0.99) | 1.3 (1.2-1.4) | 0.8 (0.7-0.9) | 1.3 (1.2-1.4) |
| Liver and gall disease | 1.1 (0.96-1.2) | 1.2 (1.1-1.3) | 1.4 (1.1-1.6) | 1.3 (1.1-1.4) | 0.9 (0.8-1.1) | 1.2 (1.1-1.3) |
| Chronic respiratory disease | 2.0 (1.8-2.1) | 0.9 (0.9-0.99) | 2.2 (2.0-2.4) | 0.8 (0.7-0.9) | 1.7 (1.5-1.9) | 1.1 (0.99-1.2) |
| Cancer | 2.3 (2.0-2.6) | 0.8 (0.8-0.9) | 3.1 (2.6-3.6) | 0.6 (0.5-0.8) | 1.8 (1.5-2.1) | 1.0 (0.9-1.1) |
| Gastrointestinal disease | 1.7 (1.6-1.8) | 0.7 (0.7-0.8) | 1.7 (1.5-1.8) | 0.7 (0.6-0.7) | 1.7 (1.6-1.9) | 0.7 (0.7-0.8) |
BMI: Body mass index (calculated as weight in kilograms divided by height in meters squared).
Multiple logistic regression models were constructed to explore the association between BMI categories (obesity & overweight vs. health; underweight vs health) and the total non-communicable disease (NCDs) or each NCD respectively from the pooled data of the two-round survey. The regression models presented odds ratios (ORs) and 95%CIs with adjustment for geographical regions, urbanization, sex, age, marital status, education, employment, smoking, drinking, physical activity and family income quartiles
4. Discussion
Our two-round survey depicted the most recent changes and prevalence of BMI categories in the whole population of mainland China. China has achieved huge economic achievements during recent years [16], with the unintended consequence that the prevalence of obesity and overweight increased greatly, by a mean annual rate of 5.8% from 2013 to 2018. Now consisting of 25.6% of the adult population, obesity and overweight now afflicts about 350 million adults in China, which is likely to increase by 15.7 million annually if no interventions are implemented. Meanwhile, there remains a population of 92.0 million underweight population, which we speculate is due to the persistence of malnutrition in some sectors and regions. China is facing a huge double burden of malnutrition.
An escalating global epidemic of obesity and overweight is a severe problem, now involving over 2.1 billion people worldwide [19]. The direct economic loss associated with obesity and overweight is estimated at more than two trillion dollars annually, accounting for 2.8% of the global gross domestic product (GDP) [26]. About two fifths of the worldwide obese population live in the low- and middle-income countries (LMICs) and many LMICs have to face the paradoxically co-existing problems of undernutrition and obesity [27], both of which proved to have close associations with increased risk of certain chronic diseases in our survey. For example, underweight imparted a higher risk of chronic respiratory diseases, while obesity and overweight brought a substantially higher risk of hypertension and diabetes. As one of the largest LMIC, China still has surpassed USA with respect to the number of obese people worldwide, according to our results [18]. The Healthy China 2030 blueprint called for measures to effectively curb the increased BMI [28]. However, our results suggest that reaching this goal shall be challenging.
The persistently higher prevalence of obesity and overweight in urban areas compared to rural areas may be attributed to the urbanization process and urban-rural economic disparity in China, which was similar to the situation reported in other LMIC [29]. Although a lower obesity and overweight prevalence was observed in the rural areas in our study, the rural areas showed a much higher rate of increase in the interval 2013–2018 than did urban areas. Moreover, the prevalence of obesity and overweight peaked some 5 years earlier in rural areas than in urban areas. This phenomenon indicates that resolution of the problem of subsistence living in rural areas now of China, which brought an important transformation of lifestyle and dietary habits. Of particularly, we noticed for the first time a sharp rise of obesity and overweight prevalence in young adults aged 19–29, which was especially pronounced in rural China. Obesity is a major risk factor for various chronic diseases. To make matters worse, excessive weight gain from young to middle adulthood was associated with increased risks of all-cause mortality [30]. Indeed, adiposity has long term harmful consequences, which predicts sharp growth of chronic disease burden and premature death in the future in China. Although China has made great achievements in eliminating poverty, we must not ignore the incident health problems such as obesity and overweight in rural areas. Otherwise, the gains in prosperity enjoyed by the rural population may be undermined by burgeoning adiposity and resultant loss of productivity. The catastrophic health expenses have reportedly increased in rural China in recent years [16]. This rings the alarm to China as well as other LMICs the emergency to adopt “primordial prevention” to mitigate against secondary health burdens due to economic development. Therefore, practical and effective policies for preventing obesity and overweight should specifically target young adults in rural China.
Earlier research showed a sharp increase in obesity and overweight prevalence among Children and adolescents in China between the years 1985 and 2010 [31]. This suggests that children and adolescents are especially vulnerable to social transition. We now report a decrease of BMI categories in children and adolescents aged 0-18 years old in the interval 2013–2018. This improvement in childhood obesity and overweight will likely lead to persistent decrease of obesity at later adulthood [32]. The recent reduction of BMI in children and adolescents may be due to several reasons as follows. First, family factors, including higher family income and mother's education level, may explain the lower obesity and overweight incidence in toddlers and pre-schoolers aged 0–5. Second, enforcement of a physical activities test in schools by the Ministry of Education in 2007 may explain the lower incidence in school aged children [33]. All children in primary and middle school are required to have two hours of physical activities every day. Third, it may due to the implementation of Healthy Lunch Programme in China since 2012 by the State Council of China [34]. Finally, similar to the phenomenon observed in the USA [35], during the past six years, height increased more than weight in school aged youth in China, which led to a decline of BMI value and substantially counteracts the effect of weight gain. For the present, height gains have apparently buffered against BMI increase in the young and adolescents, but this may not hold as the current cohort ages. This remains to be seen, but government policy guidance to ensure adequate physical activity and health food supply at school may be effective interventions for controlling obesity and overweight for children and adolescents.
Obesity and overweight prevalence varied greatly across provinces. The provinces in North China had a much higher obese and overweight prevalence than did provinces in South China, which may be related to the cold weather and eating habits in the North [36]. Shanghai and Jiangsu on east coast, which are the most economically developed regions of China, exhibit with much lower obesity and overweight prevalence as well as a relatively lower rate of increase from 2013 through 2018, indicating that highly developed local economic would enable individuals to eat more healthier foods and get medical supports. This is similar to the high-income countries, such as USA, in which a significantly greater prevalence of obesity and severe obesity in adults are reported in non-metropolitan areas compared with those in metropolitan areas [13]. The finding of significant regional and socioeconomic inequality in obesity and overweight prevalence calls for China may need to implement a regionally tailored health policy for preventing obesity and overweight in rural settings.
Unlike in many other countries [18], the prevalence of obesity and overweight in female was much lower than that of male adults. This may due to prevailing ethos that slenderness is an ideal for women [37]. However, our results showed a more significant increase of obesity and overweight prevalence in female adults than in men. Moreover, female adults with excessive adiposity had a much higher risk of cancer than males [38], which makes an urgent case for mitigating against the increasing adiposity in females in China. Compared with the results from the Nation Nutrition Survey, the prevalence of obesity was lower in our surveys [10]. There may be several reasons for that: first, the Nation Nutrition Survey include higher percentage of urban population, although our study showed higher obesity and overweight prevalence in urban areas than in rural areas [10]. Second, the standardised prevalence of obesity and overweight in adults varied greatly across different provinces of China. During 2913-2018, adults in east China had the highest prevalence of obesity and overweight, followed by adults in central China. However, the Nation Nutrition Survey did not adequately cover regions in Northwest China, where the obesity and overweight prevalence falls below that of the east and central China [10]. The China National Nutrition Surveys (CNNSs), renamed again in 2010 as China National Nutrition and Health Surveillance (CNNHS), were conducted by the Chinese Centre for Disease Control and Prevention in China [39]. The 2010–2013 CNNHS included two surveys: the 2010–2012 CNNHS surveyed 159,101 individuals aged 6 years and above, and the 2013 CNNHS surveyed 44,097 children aged 0–5 years and women who had children aged 0–2 years during the survey period. Finally, 124,787 adults (aged 18 years or old) had physical examinations and 98,042 furnished a complete dataset [39,40] We acknowledged that the prevalence of adult overweight and obesity is lower than according to the CNNHS using the WHO standard. This may be due to the differences of study design and sampling frame between these two studies. But to my understanding, both studies were intended to be nationally representative. In this regard, the problem of adiposity in China could likely be underestimated, which further supports our conclusion that China is indeed facing a severe problem of adiposity. Although the prevalence of adult obesity and overweight is lower than CNNHS according to using the WHO standard, another report suggested that the prevalence of adult obesity and overweight was 45.8% using the Asian criterion [40], which is comparable to prevalence of obesity and overweight of 40.0% in our survey in 2013. In our analysis, we have combined the prevalence of prevalence and obesity together, so the conclusion in our study would not be affected by this difference and could also be generalized.
Our study has some limitations. First, this is a cross-sectional study and the causal relationship between adiposity and a specific factor must be a matter of speculation. For example, the association between physical activity and higher obesity and overweight prevalence in our study stands in contrast to conventional wisdom [41,42], This discrepancy may be related to the fact that people tend to start taking regular exercise when they realized that obesity has greatly affected their health. While demographic, economic factors would usually affect the prevalence of obesity and overweight, the converse was not the case. Thus, the effects of demographic and economic factors on adiposity would not be influenced by the present cross-sectional design. Second, the Physical Activity Questionnaire in our survey did not allow to include physical activity in occupational, household, and transport domains, which are important contributors to total physical activity in developing countries [43,44]. Third, we did not survey the information about dietary factors in our study. In addition, our definition of obesity is based on BMI index, not on measurements of body fat composition. Although BMI and body fat generally have high correlation [45]. The temporal changes observed in BMI may not parallel completely changes in body composition and associated health risks. We excluded the records with biologically implausible height, weight and BMI, and those with missing values for height, weight, gender, or age from the interviewed sample according to the exclusion criteria recommended in the reference. As a result, the selection bias might occur due to this procedure even though the percentage of excluded participants was very low with 3.5% in 2013 and 2.6% in 2018. The prevalence of chronic diseases was underestimated in our survey because these data collected in this study were self-reported and could thus be affected by the recall bias. Moreover, missed diagnosis of NCD, especially in rural areas with medical care hardly being accessible, may also have led to their underestimation. The recall bias may also degrade the validity of health-related behaviors, also leading to underestimation of the contribution of adipose to chronic diseases burden. It is hard to predict whether the association between the demographic factors and the prevalence of obesity and overweight would be biased toward or away from the null effect because, although the very large sample size in our study may protect against this possibility.
In summary, we report the most recent change of obesity and overweight prevalence by age, gender and geography which showed that the prevalence of obesity and overweight was higher among adults in 2018 than that in 2013, with the largest growth rate in young adults aged 19–29. These results call for immediate preventive actions to decrease the potentially alarming impact on the rising NCD epidemics in China. Our study also showed a reduction of obesity and overweight prevalence in children and adolescents, which deserves deeper investigation to understand the reasons and implement early life preventive strategies.
5. Data statement
Although the data is not public available directly, the National Health Commission (NHC) of the People's Republic of China will give a report of these surveying data in certain years, which is publicly available.
Funding
National Health Commission of the People's Republic of China.
Declaration of Competing Interest
We declare that we have no conflicts of interest.
Acknowledgments
We sincerely thank the Centre for Health Statistics Information, National Health Commission of the People's Republic of China, which provided outstanding support in the data collection and analysis of this study.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2020.100521.
Contributor Information
Prof Xiang Luo, Email: flydottjh@163.com.
Prof Wei Wang, Email: wwang@vip.126.com.
Appendix. Supplementary materials
References
- 1.Zheng W, McLerran DF, Rolland B. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364(8):719–729. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Burden of Metabolic Risk Factors for Chronic Diseases C. Lu Y, Hajifathalian K. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383(9921):970–983. doi: 10.1016/S0140-6736(13)61836-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371(9612):569–578. doi: 10.1016/S0140-6736(08)60269-X. [DOI] [PubMed] [Google Scholar]
- 4.Zhou M, Wang H, Zeng X. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–1158. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Griffiths LJ, Parsons TJ, Hill AJ. Self-esteem and quality of life in obese children and adolescents: a systematic review. Int J Pediatr Obes. 2010;5(4):282–304. doi: 10.3109/17477160903473697. [DOI] [PubMed] [Google Scholar]
- 6.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362(6):485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yangfeng WU BZ, Shouqi TAO, Xigui WU, Jun YANG, Ying LI, Liancheng ZHAO, Ganqiang XIE. Prevalence of overweight and obestiy in Chinese middle-aged population: Current status and trend of developement. Chin J Epidemiol. 2002;23(1):5. [PubMed] [Google Scholar]
- 8.Prevention CCfDCa . People's Medical Publishing House Co., Ltd.; 2006. Overweight and obesity prevention and control guide for Chinese adults. [Google Scholar]
- 9.Guansheng Ma YL, Wu Yangfeng, Zhai Fengying, Cui Zhaohui, Hu Xiaoqi, Luan Dechun, Hu Yonghua, Yang Xiaoguang. The prevalence of body overweight and obesity and its changes among Chinese people during 1992 to 2002. Chin J Prev Med. 2002;39(5):5. [PubMed] [Google Scholar]
- 10.CHNS. China Health and Nutrition Surveys. 2019. https://www.cpc.unc.edu/projects/china/data(accessed June 21ST 2020).
- 11.Tian Y, Jiang C, Wang M. BMI, leisure-time physical activity, and physical fitness in adults in China: results from a series of national surveys, 2000-14. Lancet Diabetes Endocrinol. 2016;4(6):487–497. doi: 10.1016/S2213-8587(16)00081-4. [DOI] [PubMed] [Google Scholar]
- 12.Dong Y, Jan C, Ma Y. Economic development and the nutritional status of Chinese school-aged children and adolescents from 1995 to 2014: an analysis of five successive national surveys. Lancet Diabetes Endocrinol. 2019;7(4):288–299. doi: 10.1016/S2213-8587(19)30075-0. [DOI] [PubMed] [Google Scholar]
- 13.Hales CM, Fryar CD, Carroll MD, Freedman DS, Aoki Y, Ogden CL. Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013-2016. JAMA. 2018;319(23):2419–2429. doi: 10.1001/jama.2018.7270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005-2008) J Rural Health. 2012;28(4):392–397. doi: 10.1111/j.1748-0361.2012.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trivedi T, Liu J, Probst J, Merchant A, Jhones S, Martin AB. Obesity and obesity-related behaviors among rural and urban adults in the USA. Rural Remote Health. 2015;15(4):3267. [PubMed] [Google Scholar]
- 16.Meng Q, Xu L, Zhang Y. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379(9818):805–814. doi: 10.1016/S0140-6736(12)60278-5. [DOI] [PubMed] [Google Scholar]
- 17.Wang M, Luo X, Xu S. Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. Lancet Respir Med. 2019;7(1):35. doi: 10.1016/S2213-2600(18)30432-6. [DOI] [PubMed] [Google Scholar]
- 18.Collaboration NCDRF. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–1396. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO. Obesity and overweight. 2019. https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight. (Accessed November 20th 2019).
- 20.WHO . WHO; 2006. WHO Child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development; p. 312. Geneva. [Google Scholar]
- 21.Collaboration NCDRF. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO . WHO; 2009. WHO anthroplus for personal computers manual. Geneva. [Google Scholar]
- 24.Pan L, Freedman DS, Park S, Galuska DA, Potter A, Blanck HM. Changes in obesity among US children aged 2 through 4 years enrolled in WIC during 2010-2016. JAMA. 2019;321(23):2364–2366. doi: 10.1001/jama.2019.5051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 26.Dobbs R.SC, Thompson F., Manyika J., Woetzel J.R., Child P., McKenna S., Spatharou A. McKinsey Global Institute; 2014. Overcoming obesity: an initial economic analysis. [Google Scholar]
- 27.WHO. Controlling the global obesity epidemic. 2019. https://www.who.int/nutrition/topics/obesity/en/(accessed November 20th 2019).
- 28.Agency XN. "Healthy China 2030" blueprint outline. 2016. http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm.
- 29.Collaboration NCDRF. Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature. 2019;569(7755):260–264. doi: 10.1038/s41586-019-1171-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen C, Ye Y, Zhang Y, Pan XF, Pan A. Weight change across adulthood in relation to all cause and cause specific mortality: prospective cohort study. BMJ. 2019;367:l5584. doi: 10.1136/bmj.l5584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guansheng Ma JM, Ma J., Chen F., Chang S., Du S., Sun J., Tang Z., Wang H., Xu H., Ye P., Zhang N. PEOPLE'S MEDICAL PUBLISHING HOUSE Co., Ltd; 2017. Report on childhood obesity in China. [Google Scholar]
- 32.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005;115(1):22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 33.China TCPsGotPsRo . In: The guidline on strengthening the youth sports and building up the youth physique. Council CCPatS, editor. Chinese Communist Party and the State Council; 2007. http://www.gov.cn/jrzg/2007-05/24/content_625090.htm editor. [Google Scholar]
- 34.China TSCotPsRo . In: Implementation of nutrition lunch program me in rural China during the compulsory education period. China TSCotPsRo, editor. The State Council of the People's Republic of China; 2011. http://www.gov.cn/zwgk/2012-06/14/content_2160689.htm editor. [Google Scholar]
- 35.Komlos J, Breitfelder A. Height of US-born non-Hispanic children and adolescents ages 2-19, born 1942-2002 in the NHANES samples. Am J Hum Biol. 2008;20(1):66–71. doi: 10.1002/ajhb.20677. [DOI] [PubMed] [Google Scholar]
- 36.van Marken Lichtenbelt WD, Vanhommerig JW, Smulders NM. Cold-activated brown adipose tissue in healthy men. N. Engl. J. Med. 2009;360(15):1500–1508. doi: 10.1056/NEJMoa0808718. [DOI] [PubMed] [Google Scholar]
- 37.Grogan S. In: Hörschelmann K., Colls R., editors. Contested Bodies of Childhood and Youth. Palgrave Macmillan; London: 2010. [Google Scholar]
- 38.Sung H, Siegel RL, Torre LA. Global patterns in excess body weight and the associated cancer burden. CA Cancer J Clin. 2019;69(2):88–112. doi: 10.3322/caac.21499. [DOI] [PubMed] [Google Scholar]
- 39.He Y, Zhao W, Zhang J. Data resource profile: china national nutrition surveys. Int J Epidemiol. 2019;48(2):368. doi: 10.1093/ije/dyy289. [DOI] [PubMed] [Google Scholar]
- 40.Li Y, Zhao L, Yu D, Wang Z, Ding G. Metabolic syndrome prevalence and its risk factors among adults in China: a nationally representative cross-sectional study. PLoS One. 2018;13(6) doi: 10.1371/journal.pone.0199293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moyer VA, Force USPST. Screening for and management of obesity in adults: U.S. preventive services task force recommendation statement. Ann Intern Med. 2012;157(5):373–378. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- 42.Force USPST, Curry SJ, Krist AH. Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: us preventive services task force recommendation statement. JAMA. 2018;320(11):1163–1171. doi: 10.1001/jama.2018.13022. [DOI] [PubMed] [Google Scholar]
- 43.Bauman AE, Reis RS, Sallis JF. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380(9838):258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 44.Hallal PC, Andersen LB, Bull FC. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 45.Flegal KM, Shepherd JA, Looker AC. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr. 2009;89(2):500–508. doi: 10.3945/ajcn.2008.26847. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.