Abstracta
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by a newly discovered coronavirus. Epidemiological and clinical features of patients with COVID-19 have been examined but socio-economic aspects have been less studied. This study aimed to identify the role of the human development index (HDI) in the incidence and mortality rates of COVID-19 worldwide. Information on the incidence and mortality rates of COVID-19 was obtained from the Worldometer and data about the HDI 2019 were obtained from the World Bank database. Correlations between incidence, mortality rates and HDI parameters were assessed using linear regression. We calculated the concentration index to measure socio-economic inequality in COVID-19-related mortality and incidence. A linear regression analysis showed a direct significant correlation between the incidence and mortality rate of COVID-19 and HDI at the global level. The concentration index was positive for incidence rate (0.62) and mortality rate (0.69) of COVID-19, indicating the higher concentration of the rates among groups with high HDI. The high incidence and mortality rates of COVID-19 in countries with high and very high HDI are remarkable and should be the top priority for interventions by global health policy-makers. Health programmes should be provided to reduce the burden of this disease in regions with high incidence and mortality rates of COVID-19.
Keywords: Coronavirus disease 2019, human development index, incidence, inequality, mortality
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by a newly discovered coronavirus. By June 2020, the disease had infected more than 6 million people and killed nearly 380 000 people [1]. Most people infected with the new coronavirus will experience mild to moderate respiratory illness and recover without requiring special treatment [2]. Older people and those with underlying medical problems like cardiovascular disease, diabetes, chronic respiratory disease and cancer are more likely to develop serious illness [[3], [4], [5]]. Based on various research, this disease is associated with complications such as encephalopathy, thromboembolism, acute myocarditis, rhabdomyolysis, renal failure, heart failure, shock and multi-organ failure [[5], [6], [7], [8]].
Although the aetiology has been widely studied, many aspects of the disease are still unknown and socio-economic aspects have been less studied. This study aimed to assess the association of specific elements of the Human Development Index (HDI) (life expectancy at birth, education, gross national income per 1000 capita) with morbidity and mortality from COVID-19, and to examine the socio-economic inequality in global mortality from and incidence of COVID-19.
Materials and methods
This ecological study used data sets regarding the incidence and mortality rates per 1 million people of COVID-19 and the HDI. Data about incidence and mortality rate of COVID-19 for the years 2019 and 2020 were obtained from the WHO. Data about the HDI 2019 and its components were extracted from the World Bank database for 189 countries.
The HDI is a statistical tool used to measure a country's overall achievement in its social and economic dimensions. The social and economic dimensions of a country are based on the health of its people, their level of education attainment and their standard of living. HDI has several main components that include: life expectancy at birth, mean years of schooling and gross national income per capita. The range of this index is between 0 and 1. In this research, the HDI values of countries were used to classify their socio-economic status.
Data analysis was restricted to countries for which both epidemiological data from the WHO database and the HDI were available. A linear regression model was used for assessment of the HDI effect on COVID-19 mortality and incidence rates. Multiple linear regressions were exempt due to extreme collinearity of predictors. In the regression model, the β coefficient is the degree of change in mortality and incidence rates from COVID-19 for every 1-unit change in the HDI. The level of 0.05 was considered as statistical significance.
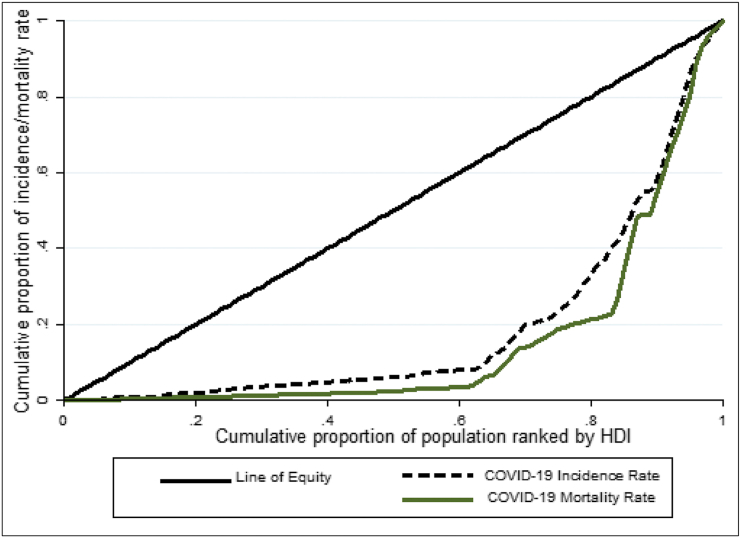
Socio-economic inequality was measured using the concentration index. This is one of the best measures of inequalities in social groups with a natural ordering. A concentration curve was used to measure the concentration index, where the cumulative percentage of mortality or incidence from COVID-19 (y-axis) was plotted against the cumulative percentage of countries ranked by their socio-economic status (x-axis) beginning with the poorest socio-economic status on the left, and ending with the richest socio-economic status on the right.
Data were analysed using Stata software version 14 (StataCorp, College Station, TX, USA).
Results
Results from linear regression models that examined the association between HDI and its components and the incidence and mortality rates from COVID-19 are presented in Table 1. This model determined that increasing mean life expectancy at birth, mean years of schooling, gross national income and HDI significantly increased the COVID-19 incidence and mortality rates (p 0.001).
Table 1.
Effect of HDI components on COVID-19 incidence and mortality rates
| Variables | COVID-19 incidence rate |
COVID-19 mortality rate |
||||
|---|---|---|---|---|---|---|
| β | 95% CI | p value | β | 95% CI | p value | |
| Life expectancy at birth | 117.28 | 72.12–162.44 | 0.001 | 6.65 | 3.53–9.76 | 0.001 |
| Mean years of schooling | 208.23 | 91.06–325.41 | 0.001 | 13.83 | 6.24–21.44 | 0.001 |
| Gross national income | 0.06 | 0.04–0.07 | 0.001 | 0.002 | 0.001–0.003 | 0.001 |
| HDI | 5830.52 | 3609.51–8051.53 | 0.001 | 317.11 | 164.15–470.08 | 0.001 |
COVID-19, coronavirus disease 2019; HDI, Human Development Index.
Fig. 1 shows concentration curves for the outcome measures analysed in this research. The horizontal axis represents the cumulative percentage of the population ranked by HDI with the origin as the lowest human development index. The cumulative percentage of incidence and mortality rate from COVID-19 corresponding to the cumulative percentage of HDI is recorded on the vertical axis. The positive value of the concentration index and the placement of the concentration curve below the equality line indicate that death and incidence rates of COVID-19 are more concentrated in countries with high socio-economic status. Concentration index and 95% CI were 0.63 (0.52–0.74) for incidence rate of COVID-19 and 0.69 (0.56–0.83) for COVID-19 mortality rate.
Fig. 1.
Concentration curve for measuring socio-economic inequality in incidence and mortality rate from COVID-19 ranked by Human Development Index in World (2020).
Discussion
In this research, we consider the HDI as an indicator of the socio-economic status of countries and examined its effect on the incidence and mortality rates of COVID-19. The results of this ecological study indicated that with increasing HDI and its components, both incidence and mortality rates of COVID-19 increased. In contrast, the concentration index showed a higher concentration of morbidity and mortality of COVID-19 in countries with higher socio-economic status.
The high incidence rate in countries with higher HDI can be attributed to the effective health-care system for early detection of disease and widespread implementation of screening programmes to diagnose the disease in these countries; these will identify asymptomatic and subclinical forms of disease. In countries with low HDI, poor access to diagnostic devices leads to a low value for incidence of infection. However, the disease registration and reporting systems in low-income countries are not of good quality, which leads to under-reporting of diseases.
One of the components of HDI is life expectancy at birth. Increasing life expectancy is equivalent to increasing the elderly population. The results of various studies have shown that the highest incidence and mortality in COVID-19 occurs in the elderly population, which is consistent with the results of our research. In explaining the relationship between aging and incidence/mortality from this infection, it can be said that older people are more likely to progress to severe cases of the disease and their immune system is less able to cope with severe cases and infectious challenges [[9], [10], [11]].
A linear regression model showed that with increasing mean years of schooling the incidence and death rate for COVID-19 also increased. With increasing level of health literacy and awareness of early symptoms of Disease and early detection, the incidence will increase.
There were some limitations in our study. First, in this ecological study, exposure is at an aggregate level so we have to be careful about interpreting the results and avoid ecological fallacy. Ecological fallacy has been described as the bias that may happen because a relationship observed among variables on an aggregate level does not represent with confidence the association that exists at an individual level. The inability to control the influence of confounding variables is the second limitation of ecological studies. For these limitations, ecological studies rarely provide a powerful examination of a causal hypothesis, but they usually serve to make hypotheses.
In conclusion, according to this study, the high incidence and mortality rates of COVID-19 in countries with high and very high HDI are remarkable, which should be the top priority of interventions for global health policy-makers. Also, health programmes should be provided to reduce the burden of this disease in regions with high incidence and mortality rates of COVID-19.
Author contributions
FSH contributed to the study concept and design, acquisition, analysis and interpretation of data, and to drafting of the manuscript. SKH contributed to the study concept and design.
Conflicts of interest
The authors declare that there are no conflicts of interest to report for this work.
Acknowledgements
This study (ID: IR.UMSHA.REC.1399.347) was funded by the Vice-Chancellor of Research and Technology of Hamadan University of Medical Sciences. The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Olivares F., Munoz D., Fica A., Delama I., Alvarez I., Navarrete M. Covid-19 in Chile. The experience of a regional reference center. Preliminary report. medRxiv. 2020 doi: 10.4067/S0034-98872020001101577. [DOI] [PubMed] [Google Scholar]
- 2.Zhang W., Zhao Y., Zhang F., Wang Q., Li T., Liu Z. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): the experience of clinical immunologists from China. Clin Immunol. 2020:108393. doi: 10.1016/j.clim.2020.108393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emami A., Javanmardi F., Pirbonyeh N., Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8(1) [PMC free article] [PubMed] [Google Scholar]
- 4.Jordan R.E., Adab P., Cheng K. Covid-19: risk factors for severe disease and death. BMJ. 2020 doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 5.Mehra M.R., Desai S.S., Kuy S., Henry T.D., Patel A.N. Cardiovascular disease, drug therapy, and mortality in COVID-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2007621. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 6.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19–associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020:201187. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeng J.-H., Liu Y.-X., Yuan J., Wang F.-X., Wu W.-B., Li J.-X. First case of COVID-19 complicated with fulminant myocarditis: a case report and insights. Infection. 2020 doi: 10.1007/s15010-020-01424-5. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jin M., Tong Q. Rhabdomyolysis as potential late complication associated with COVID-19. Emerg Infect Dis. 2020;26:10–3201. doi: 10.3201/eid2607.200445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi K.W., Chau T.N., Tsang O., Tso E., Chiu M.C., Tong W.L. Outcomes and prognostic factors in 267 patients with severe acute respiratory syndrome in Hong Kong. Ann Intern Med. 2003;139:715–723. doi: 10.7326/0003-4819-139-9-200311040-00005. [DOI] [PubMed] [Google Scholar]
- 10.Hong K.-H., Choi J.-P., Hong S.-H., Lee J., Kwon J.-S., Kim S.-M. Predictors of mortality in Middle East respiratory syndrome (MERS) Thorax. 2018;73:286–289. doi: 10.1136/thoraxjnl-2016-209313. [DOI] [PubMed] [Google Scholar]
- 11.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]