Abstract
Background And Methods:
In this study, we surveyed 761 psychiatric hospital staff (69% women, 71% full-time, 56% nursing) regarding their exposure to trauma in the workplace; symptoms of post-traumatic stress disorder (PTSD), depression, and anxiety; help seeking; and perceived barriers for help seeking.
Results:
Significant proportions of staff met the screening cutoffs for probable PTSD (16%), depression (20%), and anxiety (16%). Comorbidity was high, with approximately half of those meeting the screening cutoff for PTSD also meeting the cutoffs for depression or anxiety. Only PTSD symptoms were uniquely associated with exposure to trauma in the workplace, but both PTSD and depression symptoms significantly predicted help seeking. Staff who met one or more screening cutoffs perceived more barriers to help seeking such as difficulty with accessing services.
Conclusion:
Implications for supporting psychiatric staff exposed to trauma are discussed.
Keywords: psychiatric staff, workplace trauma, PTSD symptoms, help seeking, perceived barriers to support
Abstract
Contexte et méthodes:
Dans cette étude, nous avons interrogé 761 employés d’un hôpital psychiatrique (69% de femmes, 71% à temps plein, 56% du personnel infirmier) au sujet de leur exposition aux traumatismes en milieu de travail, des symptômes de troubles de stress post-traumatique (TSPT), de dépression ou et d’anxiété, de la recherche d’aide et d’obstacles perçus à cette recherche.
Résultats:
Des proportions significatives du personnel atteignaient les seuils de dépistage d’un TSPT probable (16%), de la dépression (20%), et de l’anxiété (16%). La comorbidité était élevée, car environ la moitié de ceux qui atteignaient le seuil de dépistage du TSPT atteignaient également les seuils de la dépression ou de l’anxiété. Seuls les symptômes du TSPT étaient uniquement associés à l’exposition à un traumatisme en milieu de travail, mais les symptômes du TSPT comme de la dépression prédisaient significativement la recherche d’aide.
Conclusion:
Les employés qui atteignaient un ou plusieurs seuils de dépistage percevaient plus d’obstacles à la recherche d’aide, comme la difficulté d’accéder aux services. Les implications du soutien au personnel psychiatrique exposé aux traumatismes sont discutées.
Post-traumatic stress disorder (PTSD) is a serious mental health disorder that can result in debilitating symptoms that involve reexperiencing and reliving a traumatic event; avoiding activities, people, or thoughts related to the traumatic event; and hyperarousal and reactivity that can cause serious distress or impairment in functioning.1 In health care settings, potentially traumatic events can include violence or threats of violence, especially if serious injury is caused or the worker feared for his or her life, but can also include less critical events including disturbing patient behavior such as chronic screaming.2,3,4 Workplace trauma can affect both the staff member who was directly affected and other staff who witnessed the event or intervened.5
Nurses may be particularly at risk of violence exposure at work, for example, nurses accounted for 31% of all workplace violence claims in British Columbia, even though they represented less than 5% of the province’s total workforce.6 In a study of 107 hospital emergency care workers, 22% of respondents reported clinically significant PTSD symptoms, and 8% met the criteria for PTSD or acute stress disorder (similar to PTSD but shorter duration of symptoms).7
Violence against health care workers is even more common in psychiatric settings; Gerberich et al.8 reported an annual assault rate of 13% in the Minnesota Nurses’ Study, with psychiatric nurses having twice the odds of being assaulted. In a recent survey of 219 psychiatric staff in Ontario, 24% self-reported PTSD symptoms that met a screening cutoff for probable PTSD.4 PTSD symptoms are associated with lower job satisfaction and compassion fatigue,9 reduced productivity,2 and increased risk of patient falls, medication errors, and lower quality of health care.10 The results of workplace trauma can affect employers in the form of absenteeism, poorer worker performance, long-term disability claims, and return-to-work difficulties.
PTSD and Other Mental Disorders
There is substantial evidence that PTSD can be comorbid with other mental health problems, especially mood and anxiety disorders, based on meta-analyses of community and psychiatric samples.11,12,13 We are unaware of any published research that has examined psychiatric comorbidity among psychiatric workers with PTSD or probable PTSD.
Interventions aimed at reducing workplace violence exposure14 or strengthening employee resilience15 may be less effective if they do not account for comorbidity.16 Therefore, it is important to examine other mental disorders in the context of workplace-related PTSD.
Help Seeking and Barriers to Accessing Help for PTSD
Barriers to accessing help can delay recovery and return to work. In a survey of 2,219 adult workers across job sectors in Ontario, 38% were currently experiencing depression, and over 50% of those affected individuals did not recognize their need for help,17 a major barrier to accessing mental health care.18 A further 20% of workers who wanted help did not seek it because of attitudinal barriers (e.g., fear of what others would think) or structural barriers (e.g., lack of accessible services). Mojtabai et al.18 found that attitudinal barriers were much more prominent than structural barriers in both initiating and continuing treatment. The most commonly reported barrier to help seeking, as documented by Alden,7 was concern about the opinions of coworkers and potential career damage.
Present Study
We conducted this study to determine the prevalence of PTSD, depression, and anxiety symptoms among psychiatric staff exposed to workplace trauma. We asked questions about help seeking and perceived attitudinal and structural barriers. We hypothesized that PTSD, depression, and anxiety would be related to workplace trauma exposure, with larger effects for direct exposure and for exposure to violence. We predicted that symptoms would, in turn, be related to help seeking, with those reporting more symptoms being more likely to seek formal supports. We predicted that many staff would report barriers to accessing formal supports, with not identifying a need for help as one of the major barriers.
Method
Participants
Survey participants were 761 psychiatric hospital staff (69% women, 71% full-time, 56% nursing, and 62% of all eligible staff). Almost half (46%) had worked for more than 10 years in mental health. We intentionally did not ask about participant characteristics such as age, relationship status, or specific allied health discipline because this could potentially identify individual participants in smaller units, and we were concerned this might inhibit survey recruitment or retention.
Measures
Workplace trauma exposure
We asked participants about direct and indirect exposure to assaults, threats, and other violence in the workplace per DSM-5: physical assault by patient, no physical injury; physical assault by patient, resulting in injury or death; injured while physically restraining patient; sexual assault by patient; threat of death or serious injury to staff; threat of death or serious injury to staff’s family; violent or accidental death; and suicide (or near fatal attempt). For each of these kinds of events, the participants responded: It happened to me directly, I responded to the code or call for help, I witnessed it, I learned about it happening to a close colleague/friend at work, I was repeatedly exposed to details about it as part of my job, or does not apply to me. A total exposure score (range 0 to 8) was created by summing the number of these types of events. A total direct exposure score was created by summing the number of events to which participants responded, “It happened to me directly” (possible range 0 to 7; excluding “violent or accidental death”).
We also asked participants to respond to the following question: “In the past year, while at work, how often were you exposed to the following behaviors by patients”: Damaging the room, drinking from the toilet, eating harmful nonfood items, elopement, flooding the room, hoarding, physically resisting care, screaming constantly, self-injury with or without suicidal intent, public sexual behavior, smearing feces, wandering, verbal abuse/threats, and physical violence.4 Participants responded on a 7-point scale from “Never” to “Every day.”
PTSD symptoms
Trauma symptoms were assessed using the PTSD Checklist-5 (PCL-5).19 Participants were asked to consider their most stressful workplace experience when completing this measure. The PCL-5 has 20 self-report items rated 0 (“not at all”) to 4 (“extremely”) according to how much the participant had been bothered by each symptom over the past month. A cutoff score of 33 has optimal efficiency for identifying probable PTSD.20
Depression and anxiety
Depression and anxiety were measured using the Patient Health Questionnaire and Generalized Anxiety Disorder Questionnaire measures (PHQ-9 and GAD-7).21 These self-report scales ask respondents how much they were bothered by symptoms during the past 2 weeks, using ratings on a scale from 0 (“Not at all”) to 3 (“Nearly every day”). The PHQ-9 measures depression with 9 items about emotional, cognitive, and other symptoms (e.g., “Feeling tired or having little energy”). The GAD-7 measures anxiety with 7 items (e.g., “Trouble relaxing”). Scores of 10 or higher indicate a positive screening result for depression (PHQ-9) or anxiety (GAD-7).
Help seeking
We created a measure of help seeking. First, we asked whether there was a time in the past 12 months when participants felt that they “needed help for PTSD or other mental health problems related to workplace trauma” on a 5-point scale labeled from “Not at all” to “Extremely.” We then asked about their use of resources for their “own mental health care” in the past 12 months, such as accessing information about mental illness, therapy, medical treatment, employment counselling, or addiction treatment, based on categories used in previous research,17 as well as engaging in self-help.
Barriers
We also asked about participants’ reasons for not using resources, within the barrier categories identified by Mojtabai et al.18 Attitudinal barriers include perceptions of symptom seriousness and perceived stigma (e.g., “You thought you could handle the problem without treatment,” “You didn’t want others to find out that you needed treatment”). Structural barriers include practical concerns (e.g., “You did not know where to go to get services,” “You didn’t have time”). Participants checked all the barriers that applied to them. We also asked participants to check which sources of support they would consider using and invited them to suggest other types of support.
Procedure
We surveyed staff working on inpatient psychiatric units at 3 psychiatric hospitals providing both forensic and nonforensic services in both urban and rural areas. All staff working with inpatients were eligible to participate in our survey. The majority of eligible staff were nursing staff, which included registered nurses, practical nurses, and patient care assistants. Other direct care providers included psychiatrists and allied health professionals such as social workers or psychologists. Nonclinical staff who routinely interacted with inpatients also participated, including clinical managers, security, housekeeping, and nutrition services. The research protocols were reviewed and approved by the research ethics boards of the participating hospitals.
We invited staff to participate in an online survey through e-mail invitations. Survey participation was also promoted through posters, staff newsletters, and postcards distributed during shift changes. Staff also participated at in-person meetings; these participants accessed the online survey using provided tablets or completed paper surveys. We gave in-person participants a card listing hospital- and community-based sources of support for trauma-related concerns, and all participants were offered a $10 gift card as a token of thanks.
Results
Workplace Trauma Exposure
Direct trauma exposure was reported by two-thirds (67%) of participants. Indeed, most (96%) participants reported one or more direct or indirect exposures, where indirect exposures included responding to an incident, witnessing the incident, having a close friend at work experience the trauma, or being repeatedly exposed to details of the trauma as part of work.
PTSD, Depression, and Anxiety
The means, standard deviations, and proportions of the sample meeting cutoff scores on the PTSD, depression, and anxiety screening measures are reported in Table 1. The same results for the public safety personnel surveyed by Carleton et al. are also reported for comparison purposes. Approximately 1 in 6 participants met the PTSD screening cutoff score of at least 33. One in 5 participants met the depression cutoff score. One in 6 participants met the cutoff score for anxiety. Almost a third (29%) of the sample met screening cutoffs for probable PTSD, depression, or anxiety. Over half of those with probable PTSD also met the cutoff score for depression (57%) or anxiety (50%).
Table 1.
Screening Results for Participants in Current Study Compared to Carleton et al.’s Survey of Public Safety Personnel.
| Current Study | Carleton et al. (2018) | |||||||
|---|---|---|---|---|---|---|---|---|
| Measures | N (n) | % | M | SD | N (n) | % | M | SD |
| PCL-5 | 761 (118) | 16 | 15.40 | 16.19 | 5,620 (1,304) | 23 | 21.27 | 18.80 |
| PHQ-9 | 754 (150) | 20 | 5.44 | 5.55 | 5,375 (1,419) | 26 | 6.54 | 5.86 |
| GAD-7 | 752 (120) | 16 | 4.75 | 5.06 | 5,241 (975) | 19 | 5.25 | 5.01 |
Note. PCL-5 = PTSD Checklist-5. PHQ-9 = Personal Health Questionnaire for depression. GAD-7 = Generalized Anxiety Disorder Questionnaire.
As predicted, exposure to threatened or actual serious physical injury, death, or sexual violence was significantly related to PTSD, r(759) = 0.40, P < 0.001, depression, r(752) = 0.24, P < 0.001, and anxiety symptoms, r(750) = 0.22, P < 0.001, with a larger association for PTSD symptoms. In a regression analysis, PTSD symptoms were significantly and uniquely related to trauma exposure, β = 0.429, in contrast to depression or anxiety, β = −0.038 and −0.001, respectively, model R 2 = 0.164, F = 48.75, P < 0.001.
Help Seeking and Barriers
The majority (443, 58%) of participants reported they did not need help in the past year. Perceived need for help was strongly and positively correlated with total scores on all 3 symptom measures, the PCL-5, r(757) = 0.73; the PHQ-9, r(751) = 0.55; and the GAD-7, r(749) = 0.50; for all measures P < 0.001. In a regression analysis, 42.6% of variance in help seeking was explained when entering PTSD, depression, and anxiety scores: PTSD, β = 0.490, t = 15.74, P < 0.001, and depression scores, β = 0.265, t = 7.52, P < 0.001, were significant, whereas anxiety scores were not, β = 0.014, t = 0.39, P = 0.70.
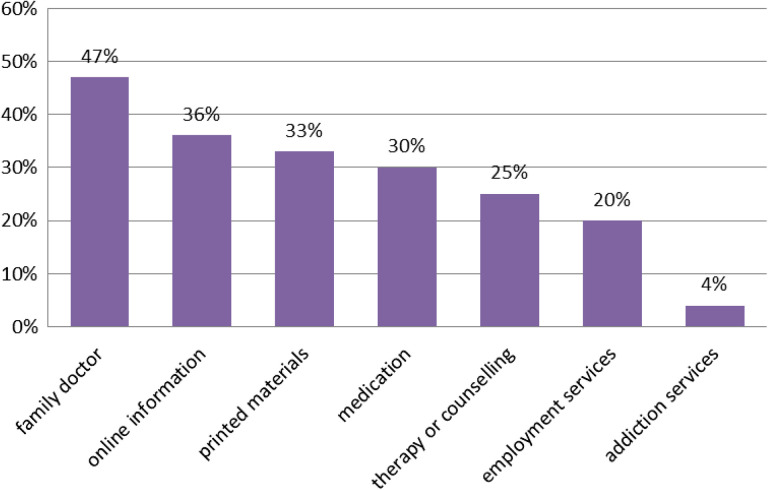
Help seeking through formal supports is illustrated in Figure 1. The majority (62%) of the sample did not seek any formal support. One in 5 (22%) sought one formal support, and 16% sought 2 to 5 formal supports. The most common source of formal support was seeing a family doctor (47%). Eighty-six staff (11%) suggested other types of support.
Figure 1.
Formal supports used in past 12 months.
We next examined help seeking among those who met any cutoff for probable PTSD, depression, or anxiety. Use of supports was higher in this subsample, with 4 in 5 (79%) using from 1 to 8 supports (M = 2.63, SD = 2.16). Seeing a family doctor was again the most common support, used by two-thirds, followed by accessing online information, printed materials, and medication, used by approximately half of this subsample.
A majority (423, 56%) of the whole sample reported one or more attitudinal barriers to seeking support (see Table 2). Fewer participants (288, 38%) reported one or more structural barriers to seeking support. We then compared the attitudinal and structural barriers perceived by those meeting a cutoff for probable PTSD, depression, or anxiety and found that those who met a cutoff perceived significantly more barriers, with large effect sizes ranging from 2.42 (did not know where to get services) to 4.79 (no transportation, too far away, or inconvenient hours).
Table 2.
Reported Barriers to Help Seeking.
| Barrier | Staff Meeting Any Cutoff (N = 222), % | Other Staff (N = 537), % | Total Sample (%) | χ2 | OR | 95% CI |
|---|---|---|---|---|---|---|
| Attitudinal | ||||||
| You thought you could handle the problem without treatment | 65.3 | 41.5 | 48.5 | 35.58 | 2.65 | 1.92 to 3.67 |
| You didn’t think treatment would help. | 23.9 | 8.9 | 13.3 | 30.37 | 3.20 | 2.08 to 4.90 |
| You were concerned that getting mental health treatment or counseling might cause your neighbors or community to have a negative opinion of you. | 15.3 | 6.0 | 8.7 | 17.32 | 2.85 | 1.71 to 4.76 |
| You were concerned that getting mental health treatment or counseling might have a negative effect on your job. | 30.2 | 10.1 | 15.9 | 47.47 | 3.87 | 2.59 to 5.78 |
| You didn’t want others to find out that you needed treatment. | 32.4 | 10.4 | 16.9 | 54.24 | 4.12 | 2.78 to 6.12 |
| You were concerned that the information you gave the counselor might not be kept confidential. | 17.1 | 6.0 | 9.2 | 23.36 | 3.26 | 1.98 to 5.37 |
| You were concerned that you might be committed to a psychiatric hospital or might have to take medicine. | 8.1 | 2.0 | 3.8 | 15.70 | 4.22 | 1.96 to 9.09 |
| Structural | ||||||
| You had no health care coverage, and you couldn’t afford the cost. | 21.2 | 8.0 | 11.9 | 26.04 | 3.08 | 1.97 to 4.83 |
| Your health insurance does not pay enough for mental health treatment or counseling. | 34.7 | 12.1 | 18.7 | 52.66 | 3.86 | 2.64 to 5.63 |
| You did not know where to go to get services | 12.2 | 5.4 | 7.4 | 10.51 | 2.42 | 1.40 to 4.20 |
| You didn’t have time (because of job, childcare, or other commitments). | 46.4 | 16.8 | 25.4 | 72.75 | 4.30 | 3.04 to 6.09 |
| You had no transportation, or treatment was too far away, or the hours were not convenient. | 6.8 | 1.5 | 3.0 | 14.83 | 4.79 | 2.00 to 11.47 |
Note. N = 759. OR = odds ratio. CI = confidence interval. All χ2 tests were significant, P = 0.001 or lower. All odds ratios were significant.
Gender
Most of our sample (751/761) identified as men or women. We previously reported that men had more trauma exposures than women and scored higher on the PCL-5.22 Here, gender was significantly related to meeting the screening cutoffs for probable PTSD, χ2(1) = 11.21, P < 0.001, but not depression, χ2(1) = 2.49, P = 0.115, or anxiety, χ2(1) = 0.51, P = 0.474. Men were significantly less likely than women to use formal supports, t(503.24) = −2.82, P = 0.005, though neither group was likely to use formal supports (M = 0.47 vs. 0.66). Men were significantly more likely than women to identify attitudinal barriers, M = 1.25 versus 0.91, t(365.39) = 3.22, P = 0.001, but did not differ when it came to structural barriers, M = 0.56 versus 0.71, t(749) = −1.74, P = 0.08.
Discussion
Participating psychiatric hospital staff reported significant levels of PTSD symptoms, with 16% meeting the cutoff for probable PTSD on the PTSD Checklist. Similar proportions of the sample met the screening cutoffs for depression (20%) and anxiety (16%). Over half of those who met the probable PTSD cutoff also met the screening cutoff for depression or anxiety. In short, workplace trauma exposure was common in this sample and so were mental disorder symptoms. PTSD symptoms were more strongly related to workplace trauma exposure than were depression or anxiety symptoms, and only PTSD symptoms were uniquely correlated with trauma exposure when PTSD, depression, and anxiety symptoms were entered into a regression analysis.
Almost half (42%) of the sample said they needed help for their mental health, and this was positively correlated with mental health symptoms. PTSD and depression symptoms, but not anxiety symptoms, uniquely and significantly explained help seeking. We would not expect participants with few or no symptoms to seek help, so focusing on the subsample that met a cutoff for PTSD, depression, or anxiety revealed that 4 in 5 of this subsample sought help from at least one source of support. The most common formal support was seeing a family doctor. However, staff meeting screening cutoffs also reported substantially more barriers to help seeking. This finding suggests that reducing stigma and other barriers, and concomitantly increasing the availability and appeal of evidence-based supports, could help staff cope with their workplace exposures. Employers and other stakeholders concerned about workers, such as unions and professional organizations, could help staff by reducing barriers to care. Organizational climate is a relatively overlooked but potentially important factor in mental health disclosure,23 such that barrier reduction could include staff–management relations and employer policies and procedures for supporting staff with mental health disorders.
Limitations
There were a number of limitations in this study. First, the survey was voluntary, and so staff may have selected themselves for participation because of their workplace exposures or mental health concerns. This selection could have both increased and decreased the prevalence and comorbidity rates we found because we might expect some participants who had concerns would be more willing to participate in the survey, but we might also expect that the most adversely affected staff avoided the survey or were not at work at the time.
Another limitation is that the survey was entirely self-report; we did not attempt to connect surveys to workplace records regarding incidents, time off work due to workplace injury, or other collateral information. Therefore, the results of our survey might be affected by socially desirable responding, recall bias, and other self-report effects. We attempted to mitigate this limitation by excluding surveys with evidence of incomplete, inconsistent, or careless responding. A total of 88 participants were removed for these reasons.
We did not ask about participant characteristics such as age, relationship status, or specific discipline because we thought some participants would be less likely to complete the survey if they were concerned about their privacy from the research team, who are also staff at these hospitals. There might only be a single male psychologist in their 40s in a hospital, for example, and so it would be easy to identify this individual through triangulation of responses.
The cross-sectional nature of our survey data cannot establish a causal link between trauma exposure and mental health symptoms. For example, participants might have experienced mental health symptoms as a result of events outside the workplace or may have been experiencing mental health symptoms before any workplace trauma exposures. However, the wording of our questions about help seeking and perceived barriers allowed us to link these factors to workplace trauma exposures.
Finally, our survey focused on patient-related exposures. Although assaults by patients (or visitors) are by far the most common form of workplace violence in health care settings, accounting for 85% of workplace violence incidents, workplace assaults can also be committed by other staff, former staff, or someone the worker knows personally who comes to the workplace (e.g., an ex-spouse).24
Future Directions
In a previous study examining these survey data, we found that trauma exposure extends beyond violence or threats of violence and can include chronic patient behavior such as yelling, smearing feces, drinking from toilet, or room damage.22 Further research on workplace trauma exposure beyond violence and threats of violence would add to our understanding of PTSD in the workplace.
We collected qualitative data through 1:1 interviews and focus groups conducted after the surveys. We plan to analyze these data to see how they can help contextualize and enrich our quantitative understanding of workplace trauma exposure and help seeking. Of particular interest are the questions we asked staff about the policies or practices that could better help staff.
Ideally, we could reduce trauma exposure in the first place. More work is needed on effective patient violence prevention and early intervention to reduce the likelihood of workplace exposures to violence and threats of violence.25 More rigorous evaluations of interventions are particularly needed, given most interventions are studied using weak designs, resulting in inconclusive findings.26
Acknowledgments
We thank the administration of our participating hospitals and partners from the Ontario Public Service Employees Union (OPSEU), the Ontario Nurses’ Association (ONA), and the Registered Nursing Association of Ontario (RNAO) for their support and participation in activities described in this report. We thank all the research participants and Rebecca Harris for research assistance.
Authors’ Note: The views, findings, opinions, and conclusions expressed herein do not necessarily represent the views of WorkSafeBC, the Government of Ontario, or our partner organizations.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: This research was supported by funds from WorkSafeBC through their Innovation at Work program and the Ontario Ministry of Labour, Training and Skills Development through their Research for the Workplace program.
ORCID iD: Nicole C. Rodrigues  https://orcid.org/0000-0003-2570-7259
https://orcid.org/0000-0003-2570-7259
References
- 1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed Washington, (DC): American Psychiatric Association; 2013. [Google Scholar]
- 2. Gates DM, Gillespie GL, Succop P. Violence against nurses and its impact on stress and productivity. Nurs Econ. 2011;29(2):59–66. [PubMed] [Google Scholar]
- 3. Speroni KG, Fitch T, Dawson E, Dugan L, Atherton M. Incidence and cost of nurse workplace violence perpetrated by hospital patients or patient visitors. J Emerg Nurs. 2014;40(3):218–228. [DOI] [PubMed] [Google Scholar]
- 4. Hilton NZ, Ham E, Dretzkat A. Psychiatric hospital workers’ exposure to disturbing patient behavior and its relation to post-traumatic stress disorder symptoms. Can J Nurs Res. 2017;49(3):118–126. [DOI] [PubMed] [Google Scholar]
- 5. Alden LE, Regambal MJ, Laposa JM. The effects of direct versus witnessed threat on emergency department healthcare workers: implications for PTSD criterion A. J Anxiety Disord. 2008;22(8):1337–1346. [DOI] [PubMed] [Google Scholar]
- 6. Alden LE. Factors that predict return-to-work in workers with PTSD. British Columbia, Canada: WorkSafe BC; 2012. [updated 2012 Jan; accessed 2019 May 17] https://www.worksafebc.com/en/resources/about-us/research/factors-that-predict-return-to-work-in-workers-with-ptsd?. [Google Scholar]
- 7. Alden LE. Posttraumatic stress disorder in hospital emergency room personnel. British Columbia, Canada: WorkSafe BC; 2005. [updated 2005 Nov; accessed 2019 May 17] https://www.worksafebc.com/en/resources/about-us/research/post-traumatic-stress-disorder-in-hospital-emergency-room-personnel?. [Google Scholar]
- 8. Gerberich SG, Church TR, McGovern PM, et al. Risk factors for work-related assaults on nurses. Epidemiology. 2005;16(5):704–709. [DOI] [PubMed] [Google Scholar]
- 9. Lauvrud C, Nonstad K, Palmstierna T. Occurrence of post traumatic stress symptoms and their relationship to professional quality of life (ProQoL) in nursing staff at a forensic psychiatric security unit: a cross-sectional study. Health Qual Life Outcomes. 2009;7(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Karanikola M, Giannakopoulou M, Mpouzika M, Kaite CP, Tsiaousis GZ, Papathanassoglou EDE. Dysfunctional psychological responses among intensive care unit nurses: a systematic review of the literature. Revista Esc Enferm USP. 2015;49(5):847–857. [DOI] [PubMed] [Google Scholar]
- 11. Rytwinski NK, Scur MD, Feeny NC, Youngstrom EA. The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis. J Trauma Stress. 2013;26(3):299–309. [DOI] [PubMed] [Google Scholar]
- 12. Spinhoven P, Penninx BW, van Hemert AM, de Rooij M, Elzinga BM. Comorbidity of PTSD in anxiety and depressive disorders: prevalence and shared risk factors. Child Abuse Negl. 2014;38(8):1320–1330. [DOI] [PubMed] [Google Scholar]
- 13. Carleton RN, Afifi TO, Turner S, et al. Mental disorder symptoms among public safety personnel in Canada. Can J Psychiatry. 2018;63(1):54–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wassell JT. Workplace violence intervention effectiveness: a systematic literature review. Saf Sci. 2009;47(8):1049–1055. [Google Scholar]
- 15. Robertson IT, Cooper CL, Sarkar M, Curran T. Resilience training in the workplace from 2003 to 2014: a systematic review. J Occup Organ Psychol. 2015;88(3):533–562. [Google Scholar]
- 16. McKee SA. Concurrent substance use disorders and mental illness: bridging the gap between research and treatment. Can Psychol. 2017;58(1):50–57. [Google Scholar]
- 17. Dewa CS, Hoch JS. Barriers to mental health service use among workers with depression and work productivity. J Occup Environ Med. 2015;57(7):726–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mojtabai R, Olfson M, Sampson NA, et al. Barriers to mental health treatment: results from the national comorbidity survey replication. Psychol Med. 2011;41(8):1751–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–498. [DOI] [PubMed] [Google Scholar]
- 20. Wortmann JH, Jordan AH, Weathers FW, et al. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess. 2016;28(11):1392–1403. [DOI] [PubMed] [Google Scholar]
- 21. Kroenke K, Spitzer RL, Williams JB, Löwe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345–359. [DOI] [PubMed] [Google Scholar]
- 22. Hilton NZ, Ham E, Rodrigues NC, Kirsh B, Chapovalov O, Seto MC. Contribution of critical events and chronic stressors to PTSD symptoms among psychiatric workers. Psychiatr Serv. 2019. doi: 10.1176/appi.ps.201900226. [DOI] [PubMed] [Google Scholar]
- 23. Dobson KS, Szeto A, Knaak S, et al. Mental health initiatives in the workplace: models, methods and results from the mental health commission of Canada. World Psychiatry. 2018;17(3):370–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. International Association for Healthcare Security and Safety—Foundation. 2019 Healthcare Crime Survey (Report No. IAHSS-F CS-19); 2019. [Google Scholar]
- 25. Rice ME, Harris GT, Varney GW, Quinsey VL. Violence in institutions: understanding, prevention, and control. Ashland (OH: ): Hogrefe & Huber Publishers; 1989. [Google Scholar]
- 26. Runyan CW, Zakocs RC, Zwerling C. Administrative and behavioral interventions for workplace violence prevention. Am J Prev Med. 2000;18(4):116–127. [DOI] [PubMed] [Google Scholar]