Abstract
Purpose
Robotic nipple-sparing mastectomy (RNSM) may allow for more precise anatomic dissection and improved cosmetic outcomes over conventional open nipple-sparing mastectomy; however data about the feasibility and safety of the procedure is limited. The aim of this study is to present and discuss peri-operative surgical outcomes and early oncologic follow-up data on consecutive patients undergoing RNSM from June 2014 to January 2019.
Methods
Women underwent RNSM and immediate robotic breast reconstruction through an axillary incision at a single institution. Peri-operative data, complications at 3 months postoperatively, pathological data, and adjuvant therapies were recorded. Local recurrence free survival, disease free survival and overall survival were analyzed.
Results
Seventy-tree women underwent 94 RNSM procedures. Indications were invasive breast cancer in 39 patients, ductal carcinoma in situ in 17 patients, and BRCA mutation in 17 patients. Mean surgery time was 3 hours and 32 minutes. One-step reconstruction with implant occurred in 89.4% of procedures. The rate of complications requiring re-operation was 4.3%. The rate of flap or nipple necrosis was 1.1% The median follow up was 19 months (range: 3.1–44.8). No local recurrences occurred. The overall survival at 12 months, 24 or 60 months was 98% (95% CI 86–100%).
Discussion
We observed low complication rate in 94 consecutive RNSM procedures demonstrating the procedure is technically feasible and safe. We found no early local failures at 19 months follow-up. Long-term follow-up is needed to confirm oncologic safety. Future clinical trials to study the advantages and disadvantages of RNSM are warranted.
Keywords: Breast cancer, robotic mastectomy, nipple-sparing mastectomy, conservative mastectomy, risk-reducing surgery, breast reconstruction, robotic surgery, cancer BRCA
Introduction
Nipple-sparing mastectomy is increasingly performed for the treatment and prevention of breast cancer and has acceptable oncologic outcomes in appropriately selected patients [1–4]. The challenge of nipple-sparing mastectomy is achieving adequate exposure to perform precise dissection in areas that are remote from the skin incision. Robotic nipple-sparing mastectomy (RNSM) was developed in order to allow for enhanced visualization of tissue planes and better access to areas that are difficult to reach through conventional open nipple-sparing mastectomy incisions. Utilizing an incision off the breast in the mid-axillary line, the aim of RNSM was to achieve superior technical and cosmetic results while maintaining the same oncologic principles of standard mastectomy (i.e. anatomic dissection planes and removal of breast en-bloc) [5–14].
We first described our technique of robotic nipple sparing mastectomy (RNSM) and immediate robotic reconstruction (IRBR) at the European Institute of Oncology in Milan [5–8] in 2014. Since that time, we have continued to study the advantages and disadvantages of RNSM through enrollment into prospective and randomized trials at our institution. We published feasibility and safety data on our first consecutive 29 RNSM and IRBR procedures where we determined the procedure was technically feasible and safe [7]. The success in our early series justified a randomized prospective trial comparing RNSM with open classical technique. This trial fully accrued and has already been closed [15]. We await long-term follow-up data for this trial but will be years for data maturation. The aim of the current study is to analyze the perioperative data, postoperative complications and early oncologic outcomes of consecutive patients undergoing RNSM and IRBR between June 2014 and January 2019.
Methods
Women age >18 who were candidates for nipple-sparing mastectomy and immediate breast reconstruction and had RNSM with IRBR were enrolled into a prospective institutional registry from June 2014 to January 2019. Indications for RNSM were invasive breast cancer, ductal carcinoma in situ (DCIS) or BRCA mutation carriers. All patients had negative preoperative assessment of nipple-areola complex, with absence of skin involvement and with low probability to have positivity of nipple-areola complex tissue intra-operative frozen section. Additionally, all patients had breast volume ≤ Bra C, no heavy smoking (defined as >20 cigarettes/day), and were low and intermediate risk for anesthesia (ASA Scale).
Previous thoracic radiation therapy for any reason, inflammatory breast cancer, skin involvement, pre-operative diagnosis (radiological or cytological) of nipple-areola complex disease, pregnancy, patients with psychiatric, addictive, or any disorder, which compromises ability to give informed consent for participation in this study, uncontrolled diabetes mellitus, and high risk for anesthesia, were exclusion criteria.
The protocol for this prospective study was approved by the scientific directorate board. Before the operation, all patients gave their signed informed consent for RNSM and IRBR according to the established regulations.
The surgical procedure of RNSM and IRBR was previously published [6–7] and minimal technical modifications during the assessment of surgical technique were meticulously recorded to allow understanding of possible effect on outcomes.
All procedures were carried out using the da Vinci Xi Surgical System® (Intuitive Surgical, Sunnyvale, CA) except for 5 procedures completed with the da Vinci Si Surgical System® (Intuitive Surgical, Sunnyvale, CA).
Operation time, length of hospitalization and number of complications were recorded. Complications were recorded at specific time points and included all complications up to 3 months post-operatively. Major complications included re-operations or implant loss. Minor complications included subcutaneous emphysema due to carbon dioxide insufflation, minor infections, necrosis, delayed wound healing, eschar/erythema to nipple or skin flap, and seroma.
Data was collected on patient age, body mass index (BMI), breast cancer characteristics (including tumor size, histologic sub-type, grade, and nodal status) and adjuvant therapy (including receipt of radiotherapy, endocrine therapy, chemotherapy and monoclonal antibodies).
Local recurrence free survival, disease free survival and overall survival were analyzed.
Patients’ characteristics, operation parameters, and complications were presented using contingency tables. Continuous variables were represented by their mean, median and range. Follow-up was calculated from the date of surgery to the date of last follow-up, the date of death, or the date of diagnosis of a second primary cancer, whichever occurred first. Only first events that occurred during the median follow up were considered for analysis. All analyses were carried out with the SAS software version 9.4 (Cary, NC).
Results
A total of 73 women between June 2014 and January 2019 underwent 94 RNSMs and IRBR procedures. Indications for procedure was invasive breast cancer in 39 patients, DCIS in 17 patients and BRCA mutation carriers without cancer diagnosis in 17 patients
Mean age was 42 years. Patient demographics and pre-operative parameters are listed in Table 1.
Table 1.
Patient demographics/pre-operative parameters
| N=73 | |
|---|---|
| Age: (years) | |
| Mean | 42 |
| Median | 42 |
| Range | (24–59) |
| BMI: kg/m2 | |
| Mean | 20.5 |
| Median | 20.5 |
| Range | (16.4–24.4) |
| Menopausal status: | |
| Premenopausal | 54 (74.0%) |
| Postmenopausal | 13 (17.8%) |
| Perimenopausal | 6 (8.2%) |
| Ptosis of the breast: | |
| 0 | 23 (31.5%) |
| 1 | 15 (20.5%) |
| 2 | 24 (32.9%) |
| 3 | 5 (6.8%) |
| Missing | 6 (8.2%) |
| Smoking history: | |
| Never smoker | 58 (79.5%) |
| Past smoker | 9 (12.3%) |
| Current smoker | 6 (8.2%) |
| Family History of BC: | |
| No | 30 (41.1%) |
| Yes | 43 (58.9%) |
In the 39 patients with invasive cancer, mean tumor size was 1.7 cm. A majority of patients had estrogen receptor positive (34/39, 87.2%) cancers without HER2 over-expression (HER2 negative in 35/39 patients (89.7%). All tumor characteristics are listed in Table 2. In patients were the sentinel node biopsy was indicated, micrometastases were found in in 4 (4.3%) and macrometastases in 7 (7.5%). In the 7 patients with macrometatasasis, axillary dissection was performed through the robotic access incision, but using standard open technique.
Table 2.
Pathological data
| Robotic N=94 | |
|---|---|
| Histological examination | |
| Ca ductal | 30 (31.9%) |
| Ca lobular | 6 (6.4%) |
| Infiltrating other | 3 (3.2%) |
| In situ | 21 (22.3%) |
| Negative (prophylactic) | 34 (36.2%) |
| Pathological staging, dimension (cm) | |
| Mean | 1.7 |
| Median (range) | 1.6 (0.14–4.9) |
| Pathological staging, pT | |
| pT1a | 4 (4.3%) |
| pT1b | 2 (2.2%) |
| pT1c | 20 (21.5%) |
| pT2 | 13 (14.0%) |
| pTis | 21 (22.6%) |
| pT0 | 33 (35.5%) |
| Pathological staging, pN | |
| pNX | 34 (36.2%) |
| pN (SentNeg) | 49 (52.1%) |
| pN1mi | 4 (4.3%) |
| pN1a | 4 (4.3%) |
| pN2a | 2 (2.1%) |
| pN3a | 1 (1.1%) |
| Pathological staging, Grading | |
| G1 | 6 (6.4%) |
| G2 | 18 (19.1%) |
| G3 | 13 (13.8%) |
| Not available | 2 (2.1%) |
| Not applicable | 55 (58.5%) |
| Margins (oncologic patients) | |
| Negative | 56 (100%) |
| Positive | 0 (0%) |
| Biological characteristics of 39 invasive carcinoma | N=39 |
| ER | |
| Negative | 5 (12.8%) |
| Positive | 34 (87.2%) |
| PgR | |
| Negative | 7 (17.9%) |
| Positive | 32 (82.1%) |
| Ki-67 | |
| <20 | 15 (38.5%) |
| ≥20 | 24 (61.5%) |
| PVI | |
| Negative | 35 (89.7%) |
| Positive | 4 (10.3%) |
| HER2 | |
| 0/+/++ | 35 (89.7%) |
| Overexpressed (+++ or FISH+) | 4 (10.3%) |
Margins were negative in all oncological cases
Mean surgery time was of 3 hours and 32 minutes (Table 3). All patients received retropectoral implant-based reconstruction. One step reconstruction with implant occurred 89.4% of cases, the remaining received reconstruction with tissue expander. The mean length of hospital stay (admission to discharge) was 2 days.
Table 3.
Peri-operative data
| Number of procedures: | N=94 |
|---|---|
| Mastectomy procedure time (h:min) | |
| Mean | 1:57 |
| Median (range) | 2:00 (0:47–3:50) |
| Reconstruction procedure time (h:min) | |
| Mean | 1:35 |
| Median (range) | 1:15 (0:24–3:12) |
| Reconstruction, n (%) | |
| Prosthesis | 84 (89.4%) |
| Expander | 10 (10.6%) |
| Length of hospital stay- admission to discharge (days) | |
| Mean | 2 |
| Median (range) | 2 (1–8) |
| Duration of drainage (days) | |
| Mean | 11 |
| Median (Range) | 9 (4–40) |
| Drainage (ml) | |
| Mean | 180 |
| Median (Range) | 150 (40–700) |
Complications were defined as any post-operative event through 90 days. Minor and major complications were recorded as listed in methods section. Seroma was the most frequent event and occurred in 5 patients (5.3%) (Table 4). Infection occurred in 2 patients (2.1%). Both patients were treated with antibiotics and one of two patients required explant of implant. Hematoma requiring re-operation occurred in 2 cases (2.1%).. Necrosis, erythema, and axillary web syndrome was found in 1 case respectively (1.1%). One patient required removal of implant at almost 3 months during chemotherapy for implant exposure.
Table 4.
Complications thru’ 90 days
| Procedures: | N=94 | N=94 |
|---|---|---|
| Total N (%) | Requiring Reoperation N (%) | |
| Infection | 2 (2.1%) | 1 (1.1%)* |
| Hematoma/Hemorrhage | 4 (4.3%) | 2 (2.1%) |
| Necrosis | 1 (1.1%) | - |
| Axillary web syndrome | 1 (1.1%) | - |
| Implant exposure | 1 (1.1%) | 1 (1.1%)* |
| Eschar | 4 (4.3%) | - |
| Seroma | 5 (5.3%) | - |
| Erythema | 1 (1.1%) | - |
| *Total loss of Implant | 2 (2.1%) | |
One explant of implant for infection, 1 implant removed for implant exposure at almost 3 months during chemotherapy.
Considering the 39 invasive breast cancer patients, radiotherapy was received in 5 (5.3%) patients. Chemotherapy was administered in 13 patients (33.3%) patients. Among the 34 patients with ER+ disease, endocrine therapy was recommended in 100% of cases (87.2% of total patients. Among the 4 patients with HER2 overexpressed, 3 underwent trastuzumab therapy (Table 5).
Table 5.
Proposed adjuvant treatment and follow up
| N=39 | |
|---|---|
| N of subjects requiring radiation therapy | 5 (12.8%) |
| N of subjects requiring chemotherapy | 13 (33.3%) |
| N of subjects requiring monoclonal antibody | 3 (7.7%) |
| N of subjects requiring hormonal therapy | 34 (87.2%) |
| Follow-up for 56 patients, months | |
| Mean | 20.0 |
| Median (Range) | 19.0 (3.1–44.8) |
The median follow up for the 56 oncologic patients was 19 months (range: 3.1–44.8) and mean follow up was 20 months (Table 5).
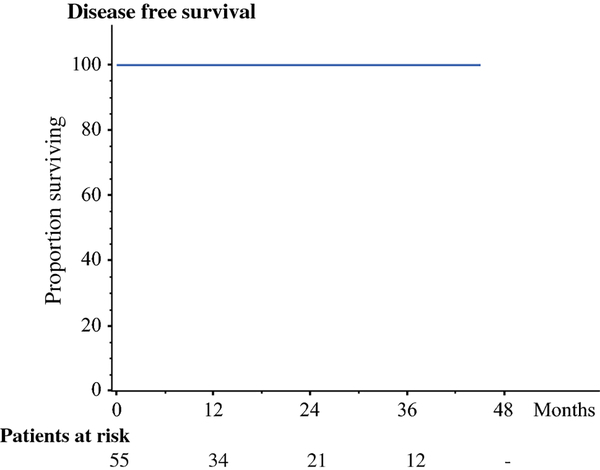
No patients were lost at follow up. No local recurrences occurred (Figure 1). One woman received neo-adjuvant treatment with Carboplatinum, NAB-Paclitaxel and immunotherapy with Atezolizumab for triple negative sub-type. This patient was oligometastatic (bone only) at the time of surgery. This patient died after 4 months for brain metastasis. The disease free survival (excluding the patient who died) was 100% (Figure 2). Considering all oncologic patients (DCIS and infiltrating carcinoma), the overall survival at 12 months was 98% (95% CI 86–100%) and remained constant after 20, 24 or 60 months (Figure 3).
Figure 1.
Local recurrence free survival. No patients lost at follow up.
Figure 2.
Disease free survival. No patients lost at follow up. One patient with metastatic disease excluded from disease free survival analysis.
Figure 3.
Overall survival. No patients lost at follow up. Overall survival at 12 months, 20 months, 24 months or 60 months is 98% (95%CI 86–100%)
Discussion
In 94 prospectively studied, consecutive robotic nipple-sparing mastectomy (RNSM) procedures with immediate robotic breast reconstruction (IRBR) performed for treatment of breast cancer or prevention of breast cancer, we had technical success of the operation in all cases and very low complication rate. Major complications of re-operation and loss of implant occurred in only 4 cases (4%) and minor complications requiring only observation for resolution occurred in an additional 13% of patients. This rate is acceptable and similar to our larger single center experience on 1989 patients underwent open nipple-sparing mastectomy and reconstructions [3] as well as large restrospective studies evaluating post-operative outcomes of conventional open technique [16].
The technical advantages of the robotic system compared to the standard open technique are related to enhanced visualization as well as incision placement. The robotic arms and camera allow for superior vision of tissue planes and higher precision dissections as the robotic arms provide access at angles that are not possible with the retractors used in open surgery. In our experience, this allows for a more complete and anatomic dissection of the breast.
The robot allows for incision placement outside of the breast in the mid-axillary line. This offers cosmetic benefit but more importantly, may have vascular advantages. The vascular supply to the nipple after NSM relies on small vessels that traverse subcutaneous tissue from larger branching vessels off the internal mammary, anterior intercostal and lateral thoracic arteries with less reliance on branches from the axillary artery or posterior intercostal branches [17]. Options for open nipple sparing mastectomy are the inframammary fold or a lateral extension off the nipple which threaten these branches more than an incision placed in the mid-axillary line. This may contribute for our low rate of necrosis and no total nipple loss events.
Furthermore, it is equally conceivable that the minimal countertraction of 8 mmHg insufflation as compared to manual retraction in an open procedure may also contribute to the low skin and nipple areola complex necrosis rates.
Despite technical or cosmetic advantages that the robot may afford, the most important outcome is oncologic outcome. We recognize this is essential to study long-term in any future study utilizing the robot for mastectomy. However, there is no reason to think that oncologic outcomes would be worse if careful technique is utilized. This is because both open and robotic procedures follow the same oncologic principles. They use anatomic dissection along tissue-planes to remove the breast specimen completely en-bloc. The specimen is then subjected to the same orientating protocol and pathologic analysis in both procedures. In fact, with the enhanced visualization and access to areas harder to reach with the open technique, it is plausible that the robot may offer superior oncologic outcomes.
To provide preliminary data on oncologic safety, our study presents our short-term follow-up of all consecutively performed RNSM performed over a 5 year period with median follow-up 19 months. The local relapse rate, disease free survival rate and overall survival were in line with previous evaluation on nipple sparing mastectomy larger series [3]. We acknowledge that most of the patients enrolled in this trial could be considered as low-risk in terms of prognosis although they were all young patients. Besides the relative small median tumor size, the vast majority of patients were ER+ pattern and the nodal involvement was limited.
As more centers perform RNSM with immediate breast reconstruction as part of prospective trials, it is important to ensure that local and distant recurrence rates are closely followed and remain within acceptable limits. In the meantime, our early data does offer insight that it is safe for larger trials to continue to study the technology.
Synopsys.
Robotic mastectomy is conceived to reduce morbidity and improve cosmetic outcomes reducing the negative impact of a devastating surgery. This study report feasibility, safety and oncologic outcome. We found no local failures at 19 months follow-up.
Acknowledgments
We thank the IEO.CCM Foundation for supporting the study.
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Competing Interests:
The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Jakub JW, Peled AW, Gray RJ, et al. Oncologic Safety of Prophylactic Nipple-Sparing Mastectomy in a Population With BRCA Mutations: A Multi-institutional Study. JAMA Surg. 2018. February 1;153(2):123–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith BL, Tang R, Rai U, et al. Oncologic Safety of Nipple-Sparing Mastectomy in Women with Breast Cancer. J Am Coll Surg. 2017. September;225(3):361–365. [DOI] [PubMed] [Google Scholar]
- 3.Galimberti V, Morigi C, Bagnardi V, et al. Oncological Outcomes of Nipple-Sparing Mastectomy: A Single-Center Experience of 1989 Patients. Ann Surg Oncol. 2018. December;25(13):3849–3857. [DOI] [PubMed] [Google Scholar]
- 4.Botteri E, Gentilini O, Rotmensz N, et al. Mastectomy without radiotherapy: outcome analysis after 10 years of follow-up in a single institution. Breast Cancer Res Treat. 2012. August;134(3):1221–8. [DOI] [PubMed] [Google Scholar]
- 5.Toesca A, Manconi A, Peradze N, et al. 1931 Preliminary report of robotic nipple-sparing mastectomy and immediate breast reconstruction with implant. Eur J Cancer 2015;51(Suppl 3):S309 [Google Scholar]
- 6.Toesca A, Peradze N, Galimberti V, et al. Robotic Nipple-Sparing Mastectomy and Immediate Breast Reconstruction with Implant: First Report of Surgical Technique. Ann Surg 2017;266(2):e28–e30. Epub 2015. [DOI] [PubMed] [Google Scholar]
- 7.Toesca A, Peradze N, Manconi A, et al. Robotic nipple-sparing mastectomy for the treatment of breast cancer: Feasibility and safety study. Breast. 2017. February;31:51–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toesca A, Peradze N, Manconi A, Nevola Teixeira LF. Reply to the letter to the editor “Robotic-assisted Nipple Sparing Mastectomy: A feasibility study on cadaveric models” by Sarfati B et al. J Plast Reconstr Aesthet Surg 2017. April;70(4):558–560. [DOI] [PubMed] [Google Scholar]
- 9.Sarfati B, Struk S, Leymarie N, et al. Robotic Prophylactic Nipple-Sparing Mastectomy with Immediate Prosthetic Breast Reconstruction: A Prospective Study. Ann Surg Oncol. 2018. September;25(9):2579–2586. [DOI] [PubMed] [Google Scholar]
- 10.Struk S, Qassemyar Q, Leymarie N, et al. The ongoing emergence of robotics in plastic and reconstructive surgery. Ann Chir Plast Esthet. 2018. April;63(2):105–112. [DOI] [PubMed] [Google Scholar]
- 11.Sarfati B, Honart JF, Leymarie N, Rimareix F, Al Khashnam H, Kolb F. Robotic da Vinci Xi-assisted nipple-sparing mastectomy: First clinical report. Breast J. 2018. May;24(3):373–376. [DOI] [PubMed] [Google Scholar]
- 12.Selber JC. Robotic Nipple-Sparing Mastectomy: The Next Step in the Evolution of Minimally Invasive Breast Surgery. Ann Surg Oncol. 2019. January;26(1):10–11. [DOI] [PubMed] [Google Scholar]
- 13.Park HS, Kim JH, Lee DW, et al. Gasless Robot-Assisted Nipple-Sparing Mastectomy: A Case Report. J Breast Cancer. 2018. September;21(3):334–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai HW, Wang CC, Lai YC, et al. The learning curve of robotic nipple sparing mastectomy for breast cancer: An analysis of consecutive 39 procedures with cumulative sum plot. Eur J Surg Oncol. 2019. February;45(2):125–133. [DOI] [PubMed] [Google Scholar]
- 15.NCT 03440398
- 16.Frey JD, Choi M, Salibian AA, Karp NS. Comparison of Outcomes with Tissue Expander, Immediate Implant, and Autologous Breast Reconstruction in Greater Than 1000 Nipple-Sparing Mastectomies. Plast Reconstr Surg. 2017. June;139(6):1300–1310. [DOI] [PubMed] [Google Scholar]
- 17.O’Dey Dm, Prescher A, Pallua N. Vascular reliability of nipple-areola complex-bearing pedicles: an anatomical microdissection study. Plast Reconstr Surg. 2007. April 1;119(4):1167–77. [DOI] [PubMed] [Google Scholar]