Abstract
Objectives:
This study investigated the effect of cervical flexor muscles fatigue on neck proprioception and postural stability.
Methods:
Forty-five male and female subjects were evaluated pre, immediate after induction of fatigue, and after recovery. Isometric neck flexor muscle endurance test (NET) was used for the induction of cervical flexor muscle fatigue. Cervical proprioception was assessed by cervical joint position error test (JPET) via overhead laser pointer while postural stability was assessed by using (a) biodex balance system measuring “Overall stability index (OSI), Anterior/ posterior (A/P) index and medial/ lateral (M/L) index”, (b) multidirectional reach test.
Results:
There was a significant decrease in cervical proprioception (cervical joint position error test) and postural stability (biodex balance system & multidirectional reach test) immediate post-induction of fatigue compared with both before induction of fatigue & after recovery from fatigue (p<0.001).
Conclusion:
Subjects suffering from cervical muscles fatigue are vulnerable to have a significant effect on neck proprioception and postural instability as it impaired the cervical proprioception sense & postural stability. Therefore, our study provides information for the clinicians and patients to avoid overload fatigue of the cervical muscles because it affects overall postural balance, neck proprioception & righting reaction.
Keywords: Cervical Fatigue, Joint Position Error, Neck Flexors, Postural Stability, Proprioception
Introduction
Muscle fatigue is defined as an activity-induced reduction in the capacity of the muscle to deliver power or force whether or not the task can be sustained. It is usually referred to as the decreased reaction of muscle for repetitive stimulus[1]. The adjustment in the position of head may cause an imbalance in the course of action of musculoskeletal framework, pressure in neck-extensor muscles, and neck-flexor muscle weakness[2]. Extreme exhausting & fatigued exercises influence both power and position coordinating the postural assignments[3].
The cervical flexors, essentially the deep neck flexors (DNF) (longus capitis, longus colli, rectus capitis), are proposed to help in stabilizing the cervical spine during gross neck developments[4]. Cervical overhead loads can lead to pressure pain in upper trapezius muscle[5]. The impact of muscle fatigue goes past the capacity to react to the continuous somatosensory input feedback and reaches out to one’s capacity to utilize motor strategies in circumstances of tactile sensory conflict[6].
Fatigue (central and peripheral) is impacted by a complex integration of physiological, tactile and mental criticism feedback, the components that add to bring about an inner perturbation which produces a weakness in the coordination of movement and postural stability[6]. Peripheral fatigue caused mainly by inner changes in the real muscles (motor units) during exercise, as the muscles become exhausted and unfit to keep delivering a similar degree of power[6]. The aggregation of lactic acid after exhausting fatiguing activities leads to firing of group III and IV of the muscle spindle afferents which are delicate to metabolites substances that accumulated inside the muscles. These afferent impulses considered as affection in the central nervous system (CNS) which leads to a reduction in neural drive and more decrease in firing rate of the motor unit, Ia from muscle spindle, Ib from Golgi tendon organ, and small diameter afferents which acts as a defensive mechanism. This contributes to the Central type of fatigue[7].
Peripheral fatigue is the primary driver of cervical exhaustion as the peripheral muscle fatigue considered to have a greater intensity than the central type of fatigue. Peripheral exhaustion fatigue shows up when consumption of vitality stores happens, or disability of the muscle contractile system is achieved during the activity and exercise[8].
The muscle spindles intensity is higher in the deep profound & small intrinsic cervical muscles than in other cervical muscles which represent their significant role in proprioception, hence proposed that fatigue of these muscles could affect stability & balance because of the tonic gamma motor neurons activation due to development of muscle contraction metabolites[8].
Inputs of Cervical proprioception give significant somatosensory feedback impacting postural balance. The adjustment in the postural control was brought about by the mistaken proprioceptive message delivered by a continuous voluntary sustained contraction[9]. Proprioception of the axial muscles, as additionally of the cervical muscles, has an incredible body-arranging impact during locomotion & stable position[10]. The sensory-motor system of the neck has a significant job in the postural control[11], as the neck proprioception has a significant role for ideal neck execution in exercises[11].
Postural instability may result from disturbed integration of the proprioception & somatosensory framework, which is constrained by the neural tract in the spinal cord[12]. The postural control impairment caused by diminished input of cervical proprioceptive and maladaptive changes in the central process of sensorimotor coordination[13]. Deficiencies of sensorimotor incorporation have been identified with impeded neck proprioception[14]. Neck proprioception impairment may influence postural control & balance[15], as the posture appears to greatly affect the sensorimotor capacity of the cervical spine[16].
The primary cause of altered postural stability following neck muscle exhaustion fatigue after isometric contraction seems to be proprioceptive conflicts[8], and as appeared in past investigations, the fatigue of postural muscles, for example, cervical, lumbar and lower extremity muscles decreases the effectiveness of postural mechanism to a more prominent degree than non-postural muscles[17].
However, along these lines, the goals of this research were to explore the impact of cervical flexor muscle fatigue on neck proprioception and postural stability, after induction of neck fatigue by isometric neck flexor muscle endurance test (NET). This research study relies upon the cervical joint position error test (JPET) to survey the cervical proprioception in clinical practice and the assessment of postural stability by using: (a) Biodex balance system measuring “Overall stability index (OSI), Anterior/ posterior (A/P) index and medial/ lateral (M/L) index”, and (b) multidirectional reach test.
Materials and methods
This study was conducted at the Faculty of Physical Therapy, Cairo University as a descriptive cross-sectional study, repeated measures (full details including ethical approval are available under the institutional ethical committee of faculty of physical therapy, Cairo University, Egypt number P.T.REC/012/002299, and clinical trials.gov ID NCT03998280.
Subjects
Forty-five participants were assessed from both sexes. All the subjects received written & verbal information about the study and gave written consent to sign before the beginning of the study. The anonymity and confidentiality were assured, and all the procedures were performed in compliance with relevant laws and institutional guidelines. The subjects were included in the study if they: (i) had age ranging from 18 to 40 years old, (ii) had a normal cervical range of motion within 80° to 90° of flexion, 70° of extension, 20° to 45° of lateral flexion, and 80° to 90° of rotation to both sides[18]. (iii) had normal muscle strength for cervical neck flexors according to group manual muscle test[19], (iv) had body mass index (BMI) ranged from (18.5 to 24.9) Kg/m2. The subjects were excluded from the study if they: (i) had a history of pathological trauma to the cervical, thoracic or lumbar spine, upper extremity, lower extremity or rib cage, (ii) had spine with any surgical intervention (iii) had any orthopedic, musculoskeletal or neurological disorders around cervical region or Spinal postural deformities as hyper kyphosis & scoliosis (iv) had vestibular impairment (e.g. vertigo).
Sample size
Sample size calculation was performed using G*POWER statistical software (version 3.1.9.2; Franz Faul, Universitat Kiel, Germany)[20] and revealed that the appropriate sample size for this study is n=45. Calculations: F tests- MANOVA: Repeated measures, within factors, α=0.05, power=0.95 and medium effect size=.25.
Methods
Induction of cervical flexor muscle fatigue using isometric neck flexor muscle endurance test (NET)
An isometric neck muscle endurance test (NME test) was conducted by instructing the subject to hold the static neck and head position in a position until fatigue & exhaustion occurred, then the total time (s) of endurance was calculated[21]. The NME test was performed for the profound deep neck flexors (Rectus Capitus Anterior, Rectus Capitus Lateralis, Longus Capitus, Longus Colli) Until exhaustion in all subjects occurred[22].
The subjects starting position was in a supine, crock-lying position, with the hands laying on the abdomen (Figure 1). The Subject maintained a chin in isometrically in a maximally tucked position, then the subject lifted the head and neck around 2.5 cm from resting position, While in this position, a line was drawn across 2 approximated skin folds along the subject’s anterior-lateral neck by the therapist, and the therapist’s fingers were under the subject’s head at the most posterior aspect of the occiput (Figure 1).
Figure 1.
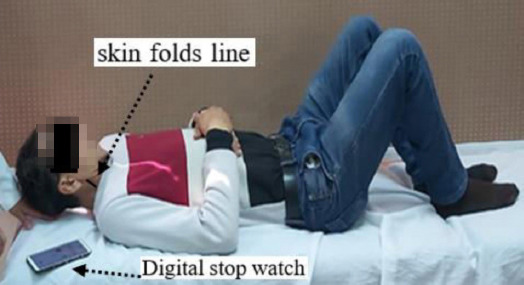
Isometric neck flexor muscle endurance test for induction of cervical flexor fatigue. The subject elevated his head up with the therapist’s hand under his head. The neck arrow points to the skin-folds line drawn by the therapist and the small arrow points to the digital stopwatch for measuring the time of fatigue.
The induction fatigue test was finished when the subject was demonstrating fatigue if one of the following four criteria were met: (1) the neck drawn lines over the skin folds no longer overlays each other & separated because of a loss of chin folds, (2) the therapist noted that the subject raised his or her head & there was never again kept in touch with the therapist’s fingers, (3) the subject’s head laid on the tester’s fingers for more than one second, (4) inability of the subject to continue. The therapist recorded time to terminate as the holding time in seconds using a digital stopwatch[23]. The average of three times measurements was taken, and the result was recorded. For the induction of exhaustion or fatigue, the subject had to maintain for 60 to 63.73 seconds for males and 38 to 45 seconds for females[24-25].
Evaluation procedures
All the evaluation procedures were conducted in the early morning before the exhausting daily routine activities, besides all the participants were allowed to rest for a while before starting the evaluation, and all the measurements were applied in the three following conditions: (1) before induction of fatigue, (2) immediate after fatigue induction through the isometric neck muscle endurance test (NME test), and (3) post-recovery after 15 minutes of fatigue induction, according to the fatigue development protocols of cervical muscles[26-27].
Assessment of cervical proprioception using cervical joint position error test (JPET)
The Joint Position Sense Error (JPSE) is considered the mainly essential measure to clinically operationalize cervical proprioception[10-28]. Cervical Joint Position Error (JPE), is the ability to relocate the head to a beginning position following a dynamic active cervical range of motion. It was found that a laser strategy for assessing JPSE had a good test-retest reliability and a strong correlation for measuring JPSE[29-30].
The subject was asked to sit with back support & the foot was placed supported on the floor with knee and hip at 90o. The Target paper of the test was fixed on the wall about 90 cm from the subject’s seat & it was adjusted according to the height of the subject. The laser pointer was fixed on the highest point of the subject head (Figure 2). The subject was asked to fix his/her head at the center of target paper, initially with opened eyes to become familiar with the test, then the subject was asked to move his/her head in four directions to the right, left, upward & downward as much as he/she could and to attempt to return to the beginning point, then with closed eyes, the subject was asked to move his/her head in the four previous directions then to return to the starting position. The points of which subject reached in all four directions were detected by the colored stickers. Then the distance between the starting center point and the point which subject reached was measured using a ruler by the therapist (Figure 2). The normal relocation is within 7 cm or less than 4.5 degrees (horizontal) from the starting point, and abnormal error is considered more than 7 cm or more than 4.5 degrees (horizontal) from starting point[31].
Figure 2.
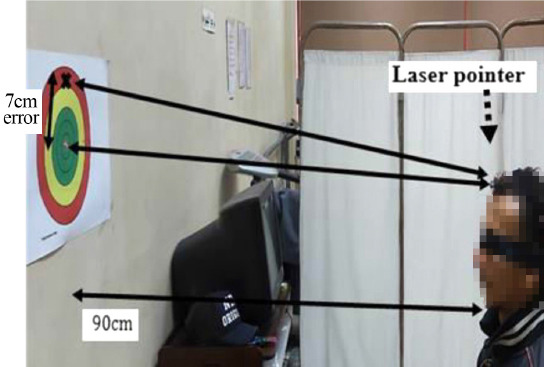
The Cervical Joint Position Sense Error test. A subject with a blindfolded seated in front of the target paper with a distance of 90 cm. The large arrows represent the two laser points on the target paper (starting point & relocation point) and the small arrow on the target paper represents the error distance between these two points (7 cm).
Assessment of postural stability by using (a) biodex balance system (b) multidirectional reach test:
(a) Biodex balance system
The subject’s ability to keep up body posture while standing on the unstable tilting platform was evaluated using the biodex balance system. The postural stability test emphasized on subject’s ability to maintain the center of balance. The data generated from this test was in the form of a balanced index which includes: a) Overall stability index (OSI), b) Anterior / posterior (A/P) index & c) medial/ lateral (M/L) index. The subjects were instructed to stand up on the foot platform, grasp the support handles at the beginning of the test, then try to maintain center position on the platform through keeping the cursor on the visual feedback screen. Additional test trials (second and third) were performed with closed eyes and the mean was calculated.
(b) Multidirectional reach test
Multidirectional reach test (MDRT) is an assessment method used to evaluate the limits of stability of individuals in four directions “forward, backward, right and left”. It measures the individual’s ability to reach, with the feet stationary subsequently shifting the center of gravity (COG) to the limits of the base of support (BOS). The MDRT is a valid and reliable clinical measure for limits of stability[32]. Without moving the feet or taking a step, the subject was asked to reach by his \her arm beside a wall as much as possible in the previous four directions then the therapist measured the distance between starting and ending points by using the tape measurement. The normal Scores of the multi-directional reach test for individuals with age ranging from (20 to 39) years are as follow: forward reach (28 cm); backward reach (17 to 18 cm); leftward reach (17 to 21 cm) and rightward reach (18 to 20 cm)[33].
Statistical analysis
Descriptive statistics in the form of mean, standard deviation, minimum, maximum, range, median and frequency were conducted for expression of the subject characteristics and measured variables of the study group. MANOVA with repeated measures was conducted for comparison of JPE, postural stability indices and multidirectional reach test between the three test conditions. The level of significance for all statistical tests was set at p<0.05. All statistical analysis was conducted through the statistical package for social studies (SPSS) version 25 for windows (IBM SPSS, Chicago, IL, USA).
Results
Subject characteristics
Forty-five subjects, 21 (47%) females and 24 (53%) males participated in this study. Table 1 showed the subject characteristics of the study group. The cervical range of motion (ROM) of the subjects was within normal values as shown in (Table 2). The median (25th, 75th percentiles) of the cervical muscle strength grade of the subjects was (4,5). 25 (55.7%) subjects had grade 4 and 20 (44.3 %) subjects had grade 5.while The mean±SD of fatigue time of the subjects was 52.44±19.98 seconds with a minimum of 23 seconds and a maximum of 100 seconds, also (Table 3) demonstrates the values of fatigue time in seconds between males and females subjects.
Table 1.
Descriptive statistics for the age, weight, height, and BMI of the study group.
| X̄±SD | Minimum | Maximum | Range | |
|---|---|---|---|---|
| Age (years) | 27.57±8.16 | 18 | 49 | 31 |
| Weight (kg) | 67.84±11.21 | 44 | 90 | 46 |
| Height (cm) | 165.26±9 | 145 | 183 | 38 |
| BMI (kg/m2) | 24.6±2.93 | 19.3 | 33 | 13.7 |
X̄, Mean; SD, Standard deviation
Table 2.
Descriptive statistics for the cervical ROM of the study group.
| Cervical ROM (degrees) | X̄±SD | Minimum | Maximum | Range |
|---|---|---|---|---|
| Flexion | 86.7±4.28 | 78 | 93 | 15 |
| Extension | 69.67±2.2 | 63 | 73 | 10 |
| Right rotation | 87.16±3.7 | 80 | 93 | 13 |
| Left rotation | 87.3±3.67 | 80 | 93 | 13 |
| Right side bending | 34.4±7.73 | 20 | 46 | 26 |
| Left side bending | 34.62±7.66 | 20 | 45 | 25 |
X̄, Mean; SD, Standard deviation.
Table 3.
Descriptive statistics for fatigue time of the study group.
| Fatigue time (seconds) | X̄±SD | Minimum | Maximum | Range |
|---|---|---|---|---|
| Study group | 52.44±19.98 | 23 | 100 | 77 |
| Males | 62.87±21.51 | 23 | 100 | 77 |
| Females | 40.52±8.15 | 30 | 55 | 25 |
X̄, Mean; SD, Standard deviation
Effect of cervical flexor fatigue on JPE, postural stability, and multidirectional reach test
There was a significant effect of fatigue on JPE, postural stability indices and multidirectional reach test (F=79.09, p=0.001) as follow.
Effect of cervical flexor fatigue on Proprioceptive JPE test
There was a significant increase in JPE in extension, flexion, right and left rotation in fatigue condition compared with that in no fatigue and recovery conditions (p<0.001), and there was a significant increase in JPE in recovery condition compared with no fatigue condition (p<0.001) (Table 4).
Table 4.
Comparison of Cervical JPE, postural stability and multidirectional reach between no fatigue, fatigue and recovery conditions.
| No fatigue | Fatigue | Recovery | p-value | |||
|---|---|---|---|---|---|---|
| X̄±SD | X̄±SD | X̄±SD | No fatigue vs fatigue | No fatigue vs recovery | Fatigue vs recovery | |
| Cervical JPE (cm) | ||||||
| Extension | 2.95±1.36 | 7.81±2.7 | 3.63±1.6 | 0.001 | 0.001 | 0.001 |
| Flexion | 2.96±1.45 | 8.66±2.97 | 3.76±1.8 | 0.001 | 0.001 | 0.001 |
| Right rotation | 3.6±1.58 | 9.45±3.1 | 4.25±1.6 | 0.001 | 0.001 | 0.001 |
| Left rotation | 4.16±2.03 | 9.44±3 | 4.92±2.2 | 0.001 | 0.001 | 0.001 |
| Postural stability | ||||||
| OSI | 3.68±1.46 | 6.78±2.53 | 3.67±1.54 | 0.001 | 1 | 0.001 |
| (M/L) index | 2.26±0.86 | 3.86±1.61 | 2.31±0.89 | 0.001 | 0.08 | 0.001 |
| (A/P) index | 3.09±1.53 | 5.7±2.52 | 3.24±1.67 | 0.001 | 0.07 | 0.001 |
| Multidirectional reach | ||||||
| Forward | 28.91±3.3 | 24.64±4 | 29.24±2.6 | 0.001 | 0.65 | 0.001 |
| Backward | 18.62±1.64 | 15.73±1.97 | 18.4±1.7 | 0.001 | 1 | 0.001 |
| Right | 19.64±1.38 | 15.97±1.81 | 19.84±1.4 | 0.001 | 1 | 0.001 |
| Left | 17.53±2.54 | 15.17±2.27 | 17.4±1.26 | 0.001 | 1 | 0.001 |
X̄, Mean; SD, Standard deviation; p-value, a Probability value; JPE, Joint position error; OSI, overall stability index; (M/L) index, medial/ lateral stability index; (A/P) index, Anterior / posterior stability index.
Effect of cervical flexor fatigue on Postural stability
There was a significant increase in OSI, (M/L) index and (A/P) index in the fatigue condition compared with that in no fatigue and recovery conditions (p<0.001), while there was no significant difference in OSI, (M/L) index, and (A/P) index between no fatigue and recovery conditions (p>0.05) (Table 4).
Effect of cervical flexor fatigue on Multidirectional reach test
There was a significant decrease in forward, backward, right and left reach in fatigue condition compared with that in no fatigue and recovery conditions (p<0.001), while there was no significant difference in multidirectional reach between no fatigue and recovery conditions (p>0.05) (Table 4).
Discussion
This study showed that there is an effect of the cervical flexor muscle fatigue on neck proprioception and postural stability, immediately after induction of fatigue using isometric neck flexor muscle endurance test (NET) compared with no fatigue & after recovery conditions. The assessment methods were: cervical joint position error test via overhead laser pointer, Biodex balance system, and multi-directional reach test.
The finding of the present study were in concurrence with an examination done by Naderifar et al[34] who revealed that there is a significant relationship between muscle fatigue and proprioception, as the study assessed the impact of neck fatigue on the stability and neck proprioception. The outcomes demonstrated that neck muscle fatigue prompts changes in the sensory receptors of the neck muscles and proprioception, thereby increasing postural instability so there is a significant correlation between neck muscle fatigue and postural stability.
Postural control and stability requires a complex organization of many senses that are related by the central nervous system (CNS) to numerous muscles that act as the multi-connected musculoskeletal system, also the input from the vestibular and visual systems are in conjunction with the muscle spindle afferent information from the cervical muscles that are essential for cervical proprioceptive acuity[35].
Vuillerme et al[15] investigated the impacts of cervical muscular fatigue on the stability of the posture under numerous tactile & sensory conditions and verified that the center of foot pressure displacement expanded due to fatigue of neck muscle in the absence of vision. Their outcomes demonstrated that there is a correlation between impaired postural stability & neck muscle fatigue.
Gardas et al[36] also revealed that the cervical muscle exhaustion & fatigue delivered a significant disturbance on balance as the outcomes indicated diminished functional reach in multidirectional reach test (MDRT) in all four directions post fatigue induction by measuring: forward, right lateral and Left lateral (p<0.0001). Multi-directional reach test reproduces the everyday capacity of a person. It was performed to find whether fatigue has an impact on the daily functions of the person. As the examination demonstrated that the exhaustion of the cervical muscle prompts postural instability.
Vuillerme[37] reported that there is a decline in the proprioceptive capacities of the muscles immediately after muscle fatigue. The absence of proprioception through deficiencies of activation in mechanoreceptors is considered the negative impact of muscle fatigue. In this case, fatigue is defined by the inability to produce an expected movement or force. This fatigue may happen every day because of normal daily activities and the central nervous system (CNS) compensates for this muscle fatigue frequently utilizing the visual feedback.
Consequences of a past trial by Pinsault and Vuillerme[38] investigated the effects of cervical muscular fatigue on joint position sense and found that the joint position sense of cervical region, which evaluated through the relocation test of the cervical to the neutral head position, was diminished by muscular fatigue. Absolute and variable errors were utilized to survey the cervical joint repositioning accuracy and consistency, respectively. Less accurate and less consistent repositioning performances were observed in pos-fatigue compared with the non-fatigue condition.
In a previous study by Mousavi et al[39] who reported that anticipatory muscle activity & the neck proprioception were tested before and after maintaining static neck flexion to produce fatigue then the measurement of neck proprioception was assessed as each participant was asked to practice ten trials of the relocation test for the cervical after active neck rotation to both sides. Following the flexion, the absolute and variable errors in head relocation significantly increased (p<0.05). The results of this examination recommended that a maintained static neck flexion until induction of fatigue can prompt affection of the feed-forward control and neck proprioception because of neuro-muscular& mechanical alterations that may be a risk factor for cervical spine injury & pain.
Domenech et al[21] likewise found that the profound deep Neck flexor (DNF) endurance test (the head lift strategy) is a non-instrumented cost-effective method & a reliable tool for measuring DNF endurance time in a clinical setting. Neck flexor endurance time that causes fatigue was significantly lower in females (mean=38.43 seconds, P<0.001) than males (mean=63.73 seconds), this normative value can be utilized as a baseline for designing an exercise program for the treatment of neck pain & to improve DNF endurance.
Previous studies have shown that the fatigue of cervical flexor muscle negatively affects visual acuity & postural stability, due to the fact that the cervical afferents assume a significant job in giving proprioceptive information in a combination of the mechanoreceptors of the cervical region, as in the neck’s upper region, there is a high density of small muscles providing neck proprioception entrances. The neck sensory-motor system has a significant role in postural stability[40]. For future studies, it would be beneficial to assess the effect of cervical muscle flexor fatigue in patients with cervical pathological problems and to assess the effect of trunk muscle fatigue on lumbar spine proprioception and postural stability.
Conclusion
Based on the findings of this study, we can conclude that cervical muscle flexor fatigue decreases neck proprioception and postural stability, so preventing overload cervical fatigue should be considered in the management of patients with cervical problems especially that suffer from postural instability.
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Yiou E, Caderby T, Hussein T. Adaptability of anticipatory postural adjustments associated with voluntary movement. World journal of orthopedics. 2012;3(6):75. doi: 10.5312/wjo.v3.i6.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kang KW, Kang DW, Kwon GY, Kim HB, Noh KM, Baek GH, Kim HH. The impact of head repositioning accuracy and proprioception on cervical stabilization exercise in healthy adults. Physical Therapy Rehabilitation Science. 2015;4(1):49–54. [Google Scholar]
- 3.Allen TJ, Proske U. Effect of muscle fatigue on the sense of limb position and movement. Experimental Brain Research. 2006;170(1):30–38. doi: 10.1007/s00221-005-0174-z. [DOI] [PubMed] [Google Scholar]
- 4.Kim JY, Kwag K Il. Clinical effects of deep cervical flexor muscle activation in patients with chronic neck pain. Journal of physical therapy science. 2016;28(1):269–273. doi: 10.1589/jpts.28.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shin S, An D, Oh J, Yoo W. Changes in pressure pain in the upper trapezius muscle, cervical range of motion, and the cervical flexion - relaxation ratio after overhead work. Industrial health. 2012;50(6):509–515. doi: 10.2486/indhealth.2012-0009. [DOI] [PubMed] [Google Scholar]
- 6.Taylor JL, Amann M, Duchateau J, Meeusen R, Rice CL. Neural contributions to muscle fatigue:from the brain to the muscle and back again. Medicine and science in sports and exercise. 2016;48(11):2294. doi: 10.1249/MSS.0000000000000923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kristjansson E, Treleaven J. Sensorimotor function and dizziness in neck pain:implications for assessment and management. journal of orthopaedic &sports physical therapy. 2009;39(5):364–377. doi: 10.2519/jospt.2009.2834. [DOI] [PubMed] [Google Scholar]
- 8.Luan H, Gdowski MJ, Newlands SD, Gdowski GT. Convergence of vestibular and neck proprioceptive sensory signals in the cerebellar interpositus. Journal of Neuroscience. 2013;33(3):1198–1210. doi: 10.1523/JNEUROSCI.3460-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duclos C, Roll R, Kavounoudias A, Mongeau JP, Roll JP, Forget R. Postural changes after sustained neck muscle contraction in persons with a lower leg amputation. Journal of Electromyography and Kinesiology. 2009;19(4):e214–e222. doi: 10.1016/j.jelekin.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 10.Pettorossi VE, Schieppati M. Neck proprioception shapes body orientation and perception of motion. Frontiers in human neuroscience. 2014;8:895. doi: 10.3389/fnhum.2014.00895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reddy RS, Alahmari KA. Cervical proprioception evaluation using cervical range of motion device:A narrative review. Saudi Journal of Sports Medicine. 2015;15(2):127. [Google Scholar]
- 12.Haddas R, Lieberman I, Boah A, Arakal R, Belanger T, Ju KL. Functional balance testing in cervical spondylotic myelopathy patients. Spine. 2019;44(2):103–109. doi: 10.1097/BRS.0000000000002768. [DOI] [PubMed] [Google Scholar]
- 13.Taylor HH, Murphy B. The effects of spinal manipulation on central integration of dual somatosensory input observed after motor training:a crossover study. Journal of manipulative and physiological therapeutics. 2010;33(4):261–272. doi: 10.1016/j.jmpt.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 14.De Pauw J, van der Velden K, Cox R, Truijen S, Cras P, Mercelis R, De Hertogh W. Measuring disability in patients with cervical dystonia according to the international classification of functioning, disability and health. OTJR:occupation, participation and health. 2017;37(3):132–140. doi: 10.1177/1539449217697043. [DOI] [PubMed] [Google Scholar]
- 15.Vuillerme N, Pinsault N. Experimental neck muscle pain impairs standing balance in humans. Experimental brain research. 2009;192(4):723–729. doi: 10.1007/s00221-008-1639-7. [DOI] [PubMed] [Google Scholar]
- 16.Alshahrani A, Aly SM, Abdrabo MS, Asiri FY. Impact of smartphone usage on cervical proprioception and balance in healthy adults. Biomedical Research J. 2018;29(12):2547–2552. [Google Scholar]
- 17.Kent-Braun JA, Fitts RH, Christie A. Skeletal muscle fatigue. Compr Physiol. 2012;2(2):997–1044. doi: 10.1002/cphy.c110029. [DOI] [PubMed] [Google Scholar]
- 18.Bogduk N, Mercer S. Biomechanics of the cervical spine. I:Normal kinematics. Clinical biomechanics. 2000;15(9):633–648. doi: 10.1016/s0268-0033(00)00034-6. [DOI] [PubMed] [Google Scholar]
- 19.Cuthbert SC, Goodheart GJ. On the reliability and validity of manual muscle testing:a literature review. Chiropractic &osteopathy. 2007;15(1):4. doi: 10.1186/1746-1340-15-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1:Tests for correlation and regression analyses. Behavior research methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 21.Domenech MA, Sizer PS, Dedrick GS, McGalliard MK, Brismee J-M. The deep neck flexor endurance test:normative data scores in healthy adults. PM&R. 2011;3(2):105–110. doi: 10.1016/j.pmrj.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 22.Edmondston S, Björnsdóttir G, Pálsson T, Solgård H, Ussing K, Allison G. Endurance and fatigue characteristics of the neck flexor and extensor muscles during isometric tests in patients with postural neck pain. Manual therapy. 2011;16(4):332–338. doi: 10.1016/j.math.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 23.Oksanen A, Pöyhönen T, Metsähonkala L, Anttila P, Hiekkanen H, Laimi K, Salminen JJ. Neck flexor muscle fatigue in adolescents with headache - An electromyographic study. European Journal of Pain. 2007;11(7):764–772. doi: 10.1016/j.ejpain.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Häkkinen A, Nikander R. Isometric endurance test of the cervical flexor muscles e Reliability and normative reference values. Journal of Bodywork &Movement Therapies. 2017;30:1e5. doi: 10.1016/j.jbmt.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 25.Painkra JP, Kumar S, Anwer S, Kumar R, Nezamuddin M, Equebal A. Reliability of an assessment of deep neck flexor muscle endurance test:A cross-sectional study. International Journal of Therapy and Rehabilitation. 2014;21(5):227–231. [Google Scholar]
- 26.Gosselin G, Fagan MJ. Effects of cervical muscle fatigue on the perception of the subjective vertical and horizontal. Springer Plus. 2014;3(1):78. doi: 10.1186/2193-1801-3-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zreiqat MM. Morgantown, West Virginia: West Virginia University; 2014. Post fatigue changes in the stability of cervical spine [Dissertation on the internet] avaialble from https://researchrepository.wvu.edu/etd/313 . [Google Scholar]
- 28.Strimpakos N. The assessment of the cervical spine. Part 1:Range of motion and proprioception. Journal of bodywork and movement therapies. 2011;15(1):114–124. doi: 10.1016/j.jbmt.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Stanton TR, Leake HB, Chalmers KJ, Moseley GL. Evidence of impaired proprioception in chronic, idiopathic neck pain:systematic review and meta-analysis. Physical therapy. 2016;96(6):876–887. doi: 10.2522/ptj.20150241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roren A, Mayoux-Benhamou M-A, Fayad F, Poiraudeau S, Lantz D, Revel M. Comparison of visual and ultrasound based techniques to measure head repositioning in healthy and neck-pain subjects. Manual therapy. 2009;14(3):270–277. doi: 10.1016/j.math.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 31.Treleaven J, Jull G, LowChoy N. The relationship of cervical joint position error to balance and eye movement disturbances in persistent whiplash. Manual therapy. 2006;11(2):99–106. doi: 10.1016/j.math.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 32.Newton RA. Validity of the multi-directional reach test:a practical measure for limits of stability in older adults. The Journals of Gerontology Series A:Biological Sciences and Medical Sciences. 2001;56(4):M248–-M252. doi: 10.1093/gerona/56.4.m248. [DOI] [PubMed] [Google Scholar]
- 33.Tantisuwat A, Chamonchant D, Boonyong S. Multi-directional reach test:an investigation of the limits of stability of people aged between 20-79 years. Journal of physical therapy science. 2014;26(6):877–880. doi: 10.1589/jpts.26.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Naderifar H, Minoonejad H, Barati AH, Lashay A. Effect of a neck proprioceptive neuromuscular facilitation training program on body postural stability in elite female basketball players. Journal of Rehabilitation Sciences &Research. 2018;5(2):41–45. [Google Scholar]
- 35.Khanna P, Kapoor G, Zutshi K. Balance deficits and recovery timeline after different fatigue protocols. Indian Journal of Physiotherapy and Occupational Therapy. 2008;2(3):42–54. [Google Scholar]
- 36.Gardas S, Nerurkar A, Yardi S. Effect of cervical muscle fatigue on postural stability. International Journal of Physiotherapy and Research. 2017;5(4):2289–92. [Google Scholar]
- 37.Vuillerme N, Nougier V, Prieur J-M. Can vision compensate for a lower limbs muscular fatigue for controlling posture in humans?Neuroscience letters. 2001;308(2):103–106. doi: 10.1016/s0304-3940(01)01987-5. [DOI] [PubMed] [Google Scholar]
- 38.Pinsault N, Vuillerme N. Degradation of cervical joint position sense following muscular fatigue in humans. Spine. 2010;35(3):294–297. doi: 10.1097/BRS.0b013e3181b0c889. [DOI] [PubMed] [Google Scholar]
- 39.Mousavi-Khatir R, Talebian S, Toosizadeh N, Olyaei GR, Maroufi N. Disturbance of neck proprioception and feed-forward motor control following static neck flexion in healthy young adults. Journal of Electromyography and Kinesiology. 2018;41:160–167. doi: 10.1016/j.jelekin.2018.04.013. [DOI] [PubMed] [Google Scholar]
- 40.Okhravi SM, Zavveyeh MK, Kalantari KK, Baghban AA, Karimi MT. A study on the effects of general fatigue on head and neck proprioception in healthy young adults. Ortopedia, traumatologia, rehabilitacja. 2015;17(1):1–6. doi: 10.5604/15093492.1143513. [DOI] [PubMed] [Google Scholar]


