Abstract
Importance:
Overuse of medical care is a well-recognized problem.
Objective:
To identify and highlight original research articles published in 2016 that are most relevant to understanding medical overuse or strategies to reduce it. The papers were organized into four categories: overtesting, overtreatment, services to question, and methods to reduce overuse.
Evidence Review:
A structured review of English-language articles on PubMed published in 2016, coupled with examination of tables of contents of high-impact journals to identify articles related to medical overuse in adults. These manuscripts were appraised for their importance to medicine.
Findings:
We reviewed 2252 articles, 1224 of which addressed medical overuse. Of these, 122 were deemed most relevant based on originality, methodologic quality, and number of patients potentially affected. The 10 most influential articles were selected by author consensus. Select findings from the studies include the lack of benefit of transesophageal echocardiography in the workup of cryptogenic stroke, increasing use of CT scans in the ER from 2.2% to 9.4% from 2001 to 2010, and carotid ultrasounds and revascularizations being performed for uncertain or inappropriate indications 95% of the time. Likewise, services for which harms are likely to outweigh benefits include treatment for early stage prostate cancer which provides no mortality benefit but increases absolute risk of erectile dysfunction by 10–30%, oxygen for patients with moderate COPD, surgery for meniscal tear with mechanical symptoms, and nutritional interventions for inpatients with malnutrition. Importantly, we highlighted two methods for reducing overuse: clinician audit and feedback with peer comparison for antibiotic use (reduction in inappropriate antibiotic use from 20% to 4%), and a practical and sensible shared decision-making tool for low risk chest pain (reduction in ER workup from 52% to 37%).
Conclusions and relevance:
The body of empiric work continues to expand related to medical services that are provided for inappropriate or uncertain indications. Engaging patients in conversations aimed at shared decision making, and giving practitioners feedback about their performance relative to peers appear to useful in reducing overuse.
Keywords: Overuse, overdiagnosis, overtreatment, deimplementation
Introduction
This article is the fourth annual update on the burgeoning area of medical overuse,1–3 Over time, empiric work in this area has matured with standardization of terminology, publication of major reviews4 and the elucidation of research agendas related to the appropriate care of both adults and children,5,6 and commencement of an annual update in pediatric overuse.7 Thoughtful attention to overuse within the medical profession has translated into actions by professional societies such as changing the name of low-grade thyroid cancer from “encapsulated follicular variant of papillary thyroid carcinoma (EFVPTC)” to “noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP)”, to emphasize the benign nature of this entity.8 Similarly, articles in the New Yorker9, the New York Times10, and the Atlantic11 reflect the increasing public interest in overuse and inappropriate medical care.
Overuse is defined as care in which potential harms outweigh potential benefits.5,12,13 Overuse can be subdivided into overuse of testing, which can lead to diagnosing disease that would never cause symptoms (“overdiagnosis”), and overtreatment which may be conceptualized as either the provision of therapeutics for which harms outweigh benefits or the treatment of overdiagnosed disease.5,14
This article examines and describes 10 of the most important studies published in 2016 concerning medical overuse in the care of adult patients.
Literature Search and Article Selection Process
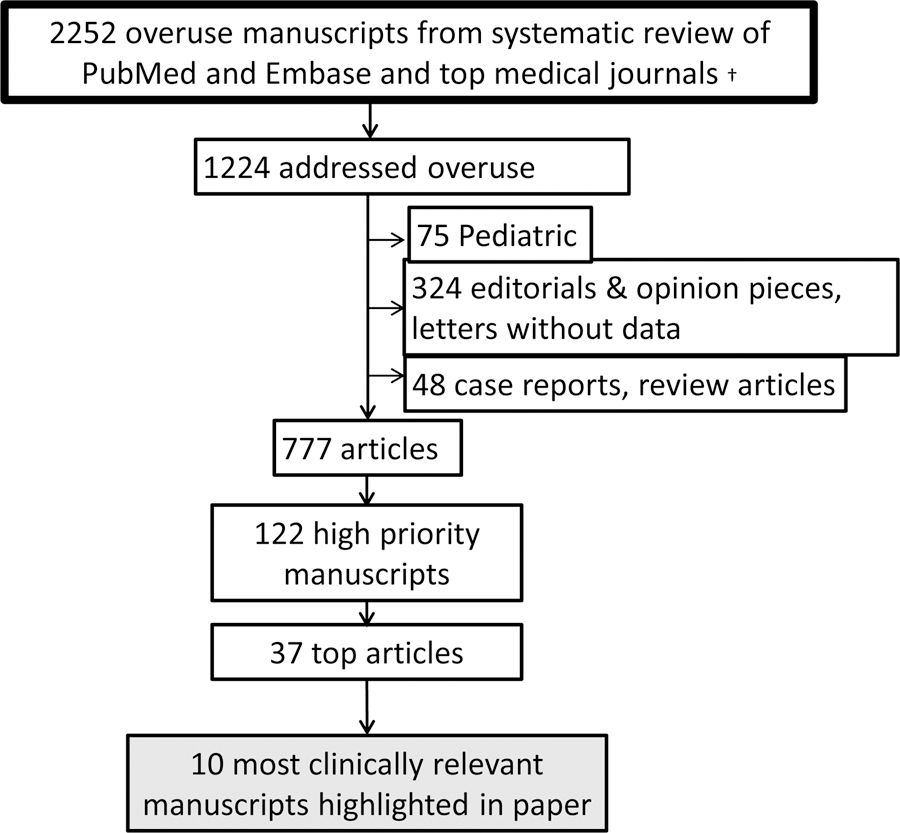
We selected articles through a structured review of studies published in 2016 in PubMed indexed under the Medical Subject Headings term “health services misuse” or with any of the following words in the title: overuse, overtreatment, overdiagnosis, inappropriate, and unnecessary. In EMBASE, we performed a search using the same terms as in PubMed with the additional Emtree term “unnecessary procedure”. We excluded articles with “overuse injury” or “overuse injuries” in the title. Searches were limited to human studies and the English language. One of 4 authors (D.J.M., S.S.D., E.C. and D.K.) reviewed all titles for relevance to medical overuse. One of the same 4 authors reviewed all 2016 titles from 10 major medical journals (Figure) and read abstracts and full journal articles for those of potential relevance; we based our search methodology on the Preferred Reporting Items for systematic reviews and meta-analyses guidelines.15
Figure.
Review Process for All 2016 Titles From 10 Major Medical Journals
† Lancet, BMJ, JAMA, JAMA IM, NEJM, Annals of Internal Medicine, Medical Care, PLoS Med, JGIM, Journal Hospital Medicine
The structured literature review identified 2252 articles, 1224 of which addressed medical overuse. After excluding 75 pediatric articles, 295 editorials or opinion pieces, 29 letters without data, and 48 case reports or review articles, 777 articles remained (See Figure). Of these, 122 (15.7%) were ranked as most relevant by at least 1 of the 3 authors based on quality of methods, magnitude of clinical impact, and number of patients potentially affected (Figure). Using the same criteria, all authors rated these 122 articles. From the 37 most highly rated articles, the 10 most relevant studies were selected by consensus among all authors and are highlighted in this article, organized into the categories of “Overuse of testing”, “Overtreatment”, “Services to question”, and “Methods to reduce overuse”.
Articles
Overtesting
TEE more sensitive than TTE for stroke etiology, without benefitting patients16
Background:
Guidelines for the diagnostic workup of patients with acute ischemic stroke include consideration of echocardiography.17,18 While pooled estimates suggest that transesophageal echocardiography (TEE) has greater sensitivity than transthoracic echocardiography (TTE) for the detection of cardiac causes of stroke19, whether these additional findings impact clinical care is unclear.
Results:
A retrospective cohort study evaluated the findings and impact of TEE in 263 patients over age 50 admitted to a single center with cryptogenic stroke and normal TTE. TEE identified a potential source of embolism in 112 patients (42.6%), most commonly complex aortic plaque (n=44, 16.7%). A single patient (0.4%) had a finding (a left atrial appendage thrombus) that lead to a change in therapy.
Implications:
Although more sensitive than TTE, TEE does not improve the clinical care of patients with acute ischemic stroke of unclear etiology; these findings are consistent with those found in a 2016 meta-analysis.20 As TEE is an invasive procedure requiring sedation, clinicians should generally avoid TEE for the workup of stroke.
Underuse of D-dimer and overuse of CT pulmonary-angiography in suspected pulmonary embolism21
Background:
Diagnostic algorithms in patients with suspected pulmonary embolism (PE) have been widely endorsed; in particular, D-dimer is recommended as the initial test for patients with low to intermediate pre-test probability of PE.22 Despite these recommendations, CT pulmonary angiography (CTPA) use in emergency departments has risen dramatically over time.23
Results:
A retrospective cohort study evaluated the appropriateness of diagnostic testing in 2031 consecutive patients who underwent CTPA at an urban academic hospital, conducting chart review to calculate pre-test probability of PE using standard criteria. About half of CTPAs were performed in the emergency department. Among patients with low pre-test probability for PE (n=1784, 88% of the cohort), CTPA was performed as the initial test in 61%; 78 patients with low pre-test probability and negative D-dimer underwent CTPA. In addition, among patients with high pre-test probability of PE (n=247, 12%), for whom D-dimers are not recommended, 68 (28%) had D-dimers tested.
Implications:
At an academic hospital, there was inconsistent application of the recommended diagnostic algorithm for PE, with overuse of CTPA and both overuse and underuse of D-dimer testing. This inappropriate testing is likely to result in delays, higher costs, and patient harm from unnecessary exposure to radiation and contrast dye. Given the wide availability of CT imaging, clinicians should remain mindful of the importance of clinical assessment, determining pre-test probability and guideline adherence in shaping the diagnostic approach to PE.
CT Scans are Increasingly Performed in Patients with Respiratory Symptoms who have the Least to Gain24
Background:
CT scans can be valuable if they guide management decisions better than other diagnostic strategies.
Results:
An analysis of National Hospital Ambulatory Medical Care Survey data from 2001 through 2010 identified 23,416 emergency department visits for upper respiratory symptoms (e.g. sore throat or nasal congestion) or lower respiratory symptoms (e.g. cough or shortness of breath). From 2001–2002 to 2009–2010, emergency department CT imaging use quadrupled from 2.2% to 9.4%, with the largest increase being among patients with non-acute upper respiratory symptoms. There was no change in antibiotic prescription and hospital admission between the two time periods.
Implications:
Use of CT scans in patients with respiratory symptoms, particularly non-acute symptoms, has increased substantially in emergency departments without improving patient management. CT scans may lead to overdiagnosis of incidental findings and harms from exposure to ionizing radiation, with 1.5–2% of all cancers in the United States attributable to radiation from CT scans.25 Multi-pronged efforts to reverse this trend are required.
Carotid Ultrasounds and Carotid Revascularization in Asymptomatic Patients are frequently for Uncertain or Inappropriate Indications26
Background:
Carotid revascularization (endarterectomy or stenting) is most commonly performed in people with asymptomatic carotid stenosis. The appropriateness of carotid ultrasounds used to detect asymptomatic stenosis is unknown.
Results:
A retrospective cohort study evaluated indications for carotid imaging in 4127 Veterans Health Administration patients aged 65 years or older who underwent carotid revascularization for asymptomatic carotid stenosis between 2005 and 2009. Carotid ultrasounds were deemed appropriate in 5.4%, uncertain in 83.4%, and inappropriate in 11.2% of patients. The most common uncertain indications were carotid bruit and follow-up for established carotid disease. The most common inappropriate indications were dizziness/vertigo, syncope, and change in vision. At 5 years post-carotid revascularization, 28.6% of patients had died.
Implications:
Nearly 95% of carotid ultrasounds for asymptomatic patients who ultimately undergo carotid revascularization are obtained for uncertain or inappropriate indications. There is a need for data to better inform evaluation of carotid bruits and monitoring of known carotid disease to reduce low-value testing and resulting carotid revascularization.
Overtreatment
Aggressive management of prostate cancer associated with erectile dysfunction and incontinence but unchanged mortality27,28
Background:
The optimal therapeutic approach to localized prostate cancer remains uncertain.
Results:
A randomized trial compared radiotherapy, surgery, and active monitoring in 1643 men with localized prostate cancer detected through prostate specific antigen (PSA) screening. Patients were followed for 10 years for prostate specific mortality and patient reported symptoms; about half of the active monitoring group was ultimately treated. The rate of prostate cancer-related death was approximately 1%, with no differences among groups. Metastases and disease progression were more common in the active monitoring group. Patients in the surgical and radiotherapy groups had a 30% and 10% absolute increase, respectively, in the proportion of men with erectile dysfunction (ED) at one year. Incontinence was also more common with surgery.
Implications:
For most men with PSA-detected prostate cancer, active monitoring will lead to better quality of life with no change in mortality compared to radiotherapy or surgery. Patients undergoing surgery and radiation for localized prostate cancer have more ED and incontinence with worse quality of life. By extension, PSA testing should generally be avoided as it is more harmful than beneficial.
Services to question
Supplemental oxygen does not benefit patients with COPD and moderate desaturation29
Background:
Treatment with supplemental oxygen prolongs survival for patients with chronic obstructive pulmonary disease (COPD) and severe desaturations.30 Whether patients with COPD and mild-to-moderate hypoxemia might benefit from supplemental oxygen is unclear.
Results:
This unblinded multicenter randomized trial compared 24-hour supplemental oxygen to no such therapy for patients with stable COPD and moderate resting or exercise-induced desaturation (oxygen saturation 89–93%). After a median of 18 months of follow-up, there was no difference in the primary composite outcome of time to death or first hospitalization for any cause (hazard ratio 0.94, 95% CI 0.79–1.12). No consistent benefit was found for secondary outcomes, including quality of life, depression, anxiety, lung function, or physical status.
Implications:
Supplemental oxygen does not benefit patients with stable COPD and moderate resting or exercise induced desaturation. Limiting use of supplemental oxygen to COPD patients with severe desaturation will protect patients from supplemental oxygen associated harms, lessen risk of tripping, and reduce costs.
No benefit to surgery for meniscal tear, even with mechanical symptoms31
Background:
Osteoarthritis of the knee is highly prevalent among older adults and can lead to substantial disability; mechanical symptoms are often attributed to associated meniscal tears. While arthroscopic surgery for osteoarthritis has little long-term benefit32, partial meniscectomy in patients with meniscal tears has remained controversial33, particularly in patients with mechanical symptoms of the knee (i.e. locking or catching).
Results:
A randomized trial compared long-term mechanical symptoms in 146 patients with degenerative meniscus tears who were randomized to partial meniscectomy (n=70) or sham surgery (n=76). At 1 year, rates of mechanical symptoms did not differ overall (27% in the meniscectomy group vs. 20% in the sham group), including in patients (n=69) with preoperative mechanical symptoms (72% vs. 59%).
Implications:
Surgery does not improve long-term mechanical symptoms in patients with degenerative meniscus tears. These findings are consistent with another 2016 randomized trial that found no difference with partial meniscectomy vs. physical therapy in patients with degenerative meniscal tears.34 The potential harms associated with surgery should lead clinicians to favor conservative management over invasive strategies for this common problem.
Little benefit to nutritional support in medical inpatients35
Background:
Malnutrition is common in medical inpatients. Malnutrition may be associated with morbidity and mortality, but the clinical benefit of nutritional support is not well-understood. Parenteral nutritional support has been shown to lead to harm when used early in critically ill adults.36
Results:
A systematic review and meta-analysis of 22 randomized controlled trials including 3376 patients with malnutrition or at risk for malnutrition compared nutritional interventions (generally oral feeding with or without nutritional counseling or, in 2 cases, enteral feeding) to control (usual care). While intervention group patients had higher caloric intake and weight gain compared to control, there was no difference in mortality (9.8% vs. 10.3%), hospital-acquired infections, functional outcomes, or length of stay. Non-elective readmissions decreased 29% with nutritional interventions.
Implications:
Nutritional support in medical inpatients with or at risk for malnutrition does not positively impact clinically relevant outcomes, including mortality. Nutritional support should generally be avoided.
Methods to reduce overuse
Doctors prescribe fewer inappropriate antibiotics if compared to their peers37
Background:
Up to half of all antibiotic use is inappropriate, exposing patients to the risk of adverse drug events, resistant bacteria, and C. difficile infection without benefit.38
Results:
A cluster randomized trial of 47 practices and 248 physicians in Boston and Los Angeles examined the effect of 3 automated interventions on antibiotic prescribing for acute respiratory tract infections. Clinicians were exposed to 1 of 3 interventions: suggested alternatives, required free-text justification, or emails comparing clinicians to top peer performers. Mean inappropriate antibiotic prescribing rates decreased from 24.1% pre-intervention to 13.1% post-intervention in control practices; the greatest impact was noted in those randomized to peer comparison (from 19.9% to 3.7% pre to post, p <0.01 for a difference compared to control practices).
Implications:
Antibiotic prescribing in outpatients can be improved through clinician feedback of metrics of inappropriate use. This low burden approach to limiting antibiotics should be adopted more broadly.
Shared decision-making in low-risk chest pain using a decision aid leads to less cardiac testing39
Background:
Chest pain is the second most common reason for emergency department visits.40 Advanced cardiac imaging for chest pain patients has more than tripled41 over 10 years and low-risk patients may commonly receive non-invasive testing that could lead to unnecessary downstream hospitalization, invasive testing, and intervention.
Results:
A pragmatic trial at 6 emergency departments included 898 patients with chest pain being considered for admission for cardiac testing. Patients were randomized to use of a decision aid to facilitate shared decision-making or usual care. Compared to usual care, patients with the decision aid were less likely to opt for admission for cardiac testing (37% vs. 52%, p<0.001) or undergo cardiac testing within 30 days (38% vs. 46%, p=0.013), had higher knowledge of their risk for acute coronary syndrome, and were more engaged in the decision-making process. There were no major adverse cardiac events. Mean patient-provider discussion time was 1.3 minutes longer with the decision aid. Clinicians highly recommended and endorsed the decision aid.
Implications:
Patients presenting with low-risk chest pain were more engaged in their management and received less testing when a decision aid tool was employed to facilitate shared decision-making. Similar strategies should be developed and tested in other clinical scenarios.
Conclusions
In 2016, there was a continued expansion of the literature on medical overuse, leading to our reviewing over 1200 articles, compared with 821 in 2015, and 440 from 2014. This expansion in the scope and breadth of scholarship related to overuse may help to bend the healthcare cost curve and promote safer healthcare delivery.
Several themes emerge from our review of the overuse literature from 2016. First, overreliance on high-technology imaging continues apace. The resultant high rates of unnecessary testing leads to overdiagnosis placing patients at risk for adverse events. Such technology often enters into clinical practice without clinical outcome studies to guide appropriate use, suggesting the need for changes in practice or policy to better protect patients against new technologies that are likely to result in net clinical harm. Such policy changes might include an FDA requirement that new technologies and diagnostic tests demonstrate benefits on patient outcomes and not surrogate measures prior to approval42 or a similar move on the part of insurers to limit reimbursement to technologies with demonstrated clinical benefit. Regardless of FDA approval and reimbursement, clinicians should limit use of unproven interventions. In addition, clinicians, particularly primary care physicians, have the power to reduce unnecessary overuse of new technologies by limiting specialist referrals for patients whose conditions does not warrant aggressive invasive management.
Beyond studies demonstrating the lack of benefit or harm with specific types of care such as supplemental home oxygen, meniscal knee surgery or nutritional support for medical inpatients29,31,35, some authors attempted interventions to reduce widely agreed upon unnecessary and harmful care. Shared decision-making, long advocated as a strategy for better quality decisions43, has now emerged as a potential remedy to overuse. Although a shared decision-making tool was helpful in the evaluation of low-risk chest pain, 37% of patients still opted for aggressive management, suggesting the need for other interventions.39 Targeting doctors is another approach for which we found new evidence. For the inappropriate use of antibiotics, it appears that comparing physicians to their high-performing peers is a good way to reduce overuse.37 Future studies should evaluate the impact of these and other interventions in additional clinical situations and test whether they might be complementary.
The continued rapid evolution of the overuse literature is encouraging and exciting. Clear understanding of the best approaches to minimize overuse, coupled with ongoing efforts to identify overused services, will be critical for the medical community as we seek to reduce unnecessary care and optimize value.
Acknowledgements:
DJM had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
DJM has no COIs related to this work. Potential COIs including having received honoraria from Springer for Textbook and journal editing. He has been reimbursed for travel by multiple conferences. He receives research funding from the VA, NIH, CDC and AHRQ. All other authors report no COIs or potential COIs.
No funding organization had any role in this work.
DK’s work on this project was supported in part by a Cancer Center Support Grant from the National Cancer Institute to Memorial Sloan Kettering Cancer Center (P30 CA008748).
SSD is supported by the Department of Veterans Affairs and the Robert Wood Johnson Foundation Clinical Scholars Program.
Dr. Wright receives support as a Miller-Coulson Family Scholar through the Johns Hopkins Center for Innovative Medicine.
References:
- 1.Morgan DJ, Wright SM, Dhruva S. Update on medical overuse. JAMA Intern Med. 2015;175(1):120–124. [DOI] [PubMed] [Google Scholar]
- 2.Morgan DJ, Dhruva SS, Wright SM, Korenstein D. Update on medical practices that should be questioned in 2015. JAMA Intern Med. 2015;175(12):1960–1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morgan DJ, Dhruva SS, Wright SM, Korenstein D. 2016 update on medical overuse: A systematic review. JAMA Intern Med. 2016;176(11):1687–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brownlee S, Chalkidou K, Doust J, et al. Evidence for overuse of medical services around the world. Lancet. 2017. [DOI] [PMC free article] [PubMed]
- 5.Morgan DJ, Brownlee S, Leppin AL, et al. Setting a research agenda for medical overuse. BMJ. 2015;351:h4534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coon ER, Quinonez RA, Moyer VA, Schroeder AR. Overdiagnosis: How our compulsion for diagnosis may be harming children. Pediatrics. 2014;134(5):1013–1023. [DOI] [PubMed] [Google Scholar]
- 7.Coon ER, Young PC, Quinonez RA, Morgan DJ, Dhruva SS, Schroeder AR. Update on pediatric overuse. Pediatrics. 2017;139(2): 10.1542/peds.2016-2797. Epub 2017 Jan 3. [DOI] [PubMed] [Google Scholar]
- 8.Nikiforov YE, Seethala RR, Tallini G, et al. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: A paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol. 2016;2(8):1023–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kolata G. Why ‘Useless’ surgery is still popular. The New York Times. August/3/2016. Accessed 6/15/2016 https://www.nytimes.com/2016/08/04/upshot/the-right-to-know-that-an-operation-is-next-to-useless.html?_r=1.
- 10.Groopman J The most notable medical findings of 2016. The New Yorker. December/29/2016. Accessed 6/15/2017 http://www.newyorker.com/tech/elements/the-most-notable-medical-findings-of-2016.
- 11.Epstein D When evidence says no, but doctors say yes. The Atlantic. February/22/2017. Accessed 6/15/2017 https://www.theatlantic.com/health/archive/2017/02/when-evidence-says-no-but-doctors-say-yes/517368/.
- 12.Welch HG, Schwartz L, Woloshin S. Overdiagnosed: Making people sick in the pursuit of health. Boston, MA: Beacon Press; 2012. [Google Scholar]
- 13.Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of medicine national roundtable on health care quality. JAMA. 1998;280(11):1000–1005. [DOI] [PubMed] [Google Scholar]
- 14.Welch HG, Passow HJ. Quantifying the benefits and harms of screening mammography. JAMA Intern Med. 2014;174(3):448–454. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010;8(5):336–341. [DOI] [PubMed] [Google Scholar]
- 16.Marino B, Jaiswal A, Goldbarg S, Bernardini GL, Kerwin T. Impact of transesophageal echocardiography on clinical management of patients over age 50 with cryptogenic stroke and normal transthoracic echocardiogram. J Hosp Med. 2016;11(2):95–98. [DOI] [PubMed] [Google Scholar]
- 17.European Stroke Organisation (ESO) Executive Committee, ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008;25(5):457–507. [DOI] [PubMed] [Google Scholar]
- 18.Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–2236. [DOI] [PubMed] [Google Scholar]
- 19.Holmes M, Rathbone J, Littlewood C, et al. Routine echocardiography in the management of stroke and transient ischaemic attack: A systematic review and economic evaluation. Health Technol Assess. 2014;18(16):1–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katsanos AH, Giannopoulos S, Frogoudaki A, et al. The diagnostic yield of transesophageal echocardiography in patients with cryptogenic cerebral ischaemia: A meta-analysis. Eur J Neurol. 2016;23(3):569–579. [DOI] [PubMed] [Google Scholar]
- 21.Alhassan S, Sayf AA, Arsene C, Krayem H. Suboptimal implementation of diagnostic algorithms and overuse of computed tomography-pulmonary angiography in patients with suspected pulmonary embolism. Ann Thorac Med. 2016;11(4):254–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raja AS, Greenberg JO, Qaseem A, et al. Evaluation of patients with suspected acute pulmonary embolism: Best practice advice from the clinical guidelines committee of the American College of Physicians. Ann Intern Med. 2015;163(9):701–711. [DOI] [PubMed] [Google Scholar]
- 23.Feng LB, Pines JM, Yusuf HR, Grosse SD. U.S. trends in computed tomography use and diagnoses in emergency department visits by patients with symptoms suggestive of pulmonary embolism, 2001–2009. Acad Emerg Med. 2013;20(10):1033–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drescher FS, Sirovich BE. Use of computed tomography in emergency departments in the United States: A decade of coughs and colds. JAMA Intern Med. 2016;176(2):273–275. [DOI] [PubMed] [Google Scholar]
- 25.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. [DOI] [PubMed] [Google Scholar]
- 26.Keyhani S, Cheng EM, Naseri A, et al. Common reasons that asymptomatic patients who are 65 years and older receive carotid imaging. JAMA Intern Med. 2016;176(5):626–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamdy FC, Donovan JL, Lane JA, et al. 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med. 2016;375(15):1415–1424. [DOI] [PubMed] [Google Scholar]
- 28.Donovan JL, Hamdy FC, Lane JA, et al. Patient-reported outcomes after monitoring, surgery, or radiotherapy for prostate cancer. N Engl J Med. 2016;375(15):1425–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Long-Term Oxygen Treatment Trial Research Group, Albert RK, Au DH, et al. A randomized trial of long-term oxygen for COPD with moderate desaturation. N Engl J Med. 2016;375(17):1617–1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: A clinical trial. nocturnal oxygen therapy trial group. Ann Intern Med. 1980;93(3):391–398. [DOI] [PubMed] [Google Scholar]
- 31.Sihvonen R, Englund M, Turkiewicz A, Jarvinen TL, Finnish Degenerative Meniscal Lesion Study Group. Mechanical symptoms and arthroscopic partial meniscectomy in patients with degenerative meniscus tear: A secondary analysis of a randomized trial. Ann Intern Med. 2016;164(7):449–455. [DOI] [PubMed] [Google Scholar]
- 32.Thorlund JB, Juhl CB, Roos EM, Lohmander LS. Arthroscopic surgery for degenerative knee: Systematic review and meta-analysis of benefits and harms. BMJ. 2015;350:h2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.American Academy of Orthopaedic Surgeons. Treatment of osteoarthritis of the knee. 5/18/2013. Accessed 6/15/17 http://www.aaos.org/cc_files/aaosorg/research/guidelines/treatmentofosteoarthritisofthekneeguideline.pdf.
- 34.Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: Randomised controlled trial with two year follow-up. BMJ. 2016;354:i3740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bally MR, Blaser Yildirim PZ, Bounoure L, et al. Nutritional support and outcomes in malnourished medical inpatients: A systematic review and meta-analysis. JAMA Intern Med. 2016;176(1):43–53. [DOI] [PubMed] [Google Scholar]
- 36.Casaer MP, Mesotten D, Hermans G, et al. Early versus late parenteral nutrition in critically ill adults. N Engl J Med. 2011;365(6):506–517. [DOI] [PubMed] [Google Scholar]
- 37.Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: A randomized clinical trial. JAMA. 2016;315(6):562–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA. 2016;315(17):1864–1873. [DOI] [PubMed] [Google Scholar]
- 39.Hess EP, Hollander JE, Schaffer JT, et al. Shared decision making in patients with low risk chest pain: Prospective randomized pragmatic trial. BMJ. 2016;355:i6165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Niska R, Bhuiya F, Xu J. National hospital ambulatory medical care survey: 2007 emergency department summary. Natl Health Stat Report. 2010;(26)(26):1–31. [PubMed] [Google Scholar]
- 41.Bhuiya FA, Pitts SR, McCaig LF. Emergency department visits for chest pain and abdominal pain: United states, 1999–2008. NCHS Data Brief. 2010;(43)(43):1–8. [PubMed] [Google Scholar]
- 42.Jacoby VL, Subak L, Waetjen LE. The FDA and the vaginal mesh controversy--further impetus to change the 510(k) pathway for medical device approval. JAMA Intern Med. 2016;176(2):277–278. [DOI] [PubMed] [Google Scholar]
- 43.Joosten EA, DeFuentes-Merillas L, de Weert GH, Sensky T, van der Staak CP, de Jong CA. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom. 2008;77(4):219–226. [DOI] [PubMed] [Google Scholar]