Abstract
BACKGROUND
Nonmelanoma skin cancer is the most common cancer in the United States with significant quality of life impact.
OBJECTIVE
To assess the utility of a highly immersive virtual reality (VR) experience in the context of outpatient skin cancer surgery as a means to minimize patient-reported feelings of anxiety or pain. The authors also sought to assess the effects on patient-reported overall satisfaction.
MATERIALS AND METHODS
Patients completed a pre-VR experience survey after completion of their first Mohs surgery layer, followed by a 10-minute VR experience, and a post-VR experience survey. Differences in the pre-VR survey and post-VR survey were compared using the chi-square test. The anxiety scores were compared using a t-test.
RESULTS
In all but 2 questions, there was a trend toward improvement of the anxiety-related sensations after completion of the VR experience. There were statistically significant differences for 4 questions: “Are you currently feeling unable to relax” (p = .0013), “are you currently feeling fear of the worst happening” (p < .0001), “are you currently feeling terrified or afraid” (p = .0046), and “are you currently feeling nervous” (p < .0001).
CONCLUSION
Virtual reality experiences during the Mohs surgical day significantly improved measures of anxiety and patient satisfaction.
Nonmelanoma skin cancer (NMSC) is the most common cancer in the United States with more than 5 million estimated cases per year, outnumbering all other cancers combined and with rates continuing to climb.1–7 In addition to potential mortality in advanced and high-risk cases, the quality of life (QOL) impact on patients is substantial.8 In a small sample of 52 patients with NMSC, 31% indicate moderate to severe QOL impairment due to physical symptoms of the disease and its treatment.9 In a larger cohort of 211 patients with NMSC, worries centered on risk of future skin cancers and scar size.9 Furthermore, the majority of NMSC is removed from the head and neck region and is therefore highly visible, potentially resulting in embarrassment and/or emotional trauma.10,11 In addition, patients with skin cancer commonly undergo surgical procedures while awake under local anesthesia. Thus, although Mohs surgery is overall well tolerated, there exists a wide spectrum of experiences and multiple factors that influence patient anxiety and satisfaction. These factors include patient demographics (age, sex, and race), socioeconomic variables (education status, income, and marital status), health status (physical health, mental health, skin-related QOL, and worry), tumor characteristics (size, type, location, and invasiveness), smoking status, psychiatric diagnoses, and previous experience with disease.12,13 Despite the high overall survival rates in NMSC, a significant proportion of patients report unmet supportive care needs and experience heightened anxiety and distress levels that may worsen during idle time before their Mohs procedure and between Mohs layers.9,13
Proof of concept using virtual reality (VR) experiences to mitigate stressful health care experiences has already been demonstrated in various settings, including in the context of venipuncture, pain secondary to burn injuries, post-traumatic stress disorder, wound care, chemotherapy, dental procedures, and routine medical procedures. In general, these studies have shown notable improvement in pain, anxiety, and general levels of distress.14–24,31 Specifically, a 2004 study evaluating the efficacy of VR to reduce pain associated with subcutaneous venous port access reported a significant difference between the VR group and control group, while another study reported significant reductions in pain associated with burn injury debridement.22 In another study of patients in a pediatric nephrology clinic, results demonstrated significantly lower pain and stress intensity in the VR group relative to controls. In a study focused on preoperative anxiety, the authors reported a statistically significant improvement in the group that received the VR experience.25
The VR sector has experienced tremendous growth in recent years with rapidly expanding technology applications.26,27 In the past, widespread use of VR has been limited by numerous factors including but not limited to cost and size of equipment.26,27 The new generation of VR head-mounted displays, however, is reasonably priced, smaller in size, and available to the general public, improving the practicality of use in diverse settings, including the outpatient dermatology and surgical setting.26,27
In this prospective study, the authors sought to expand the applications of VR technology in health care through evaluation of the experience of patients undergoing Mohs surgery for skin cancer. Specifically, the authors assessed the utility of a highly immersive VR experience in the context of outpatient skin cancer surgery as a means to minimize patient-reported feelings of anxiety or pain. The authors also sought to assess the effect of VR on patient-reported overall satisfaction.
Patients and Methods
Population and Study Design
The study was approved by the University of Southern California Institutional Review Board. Patients undergoing Mohs micrographic surgery at this clinic from July 2017 to January 2018 were recruited for participation in this prospective interventional study at the beginning of their surgical day. A signed consent form was obtained from each participant that was willing to participate. Patients were excluded if they were unwilling to participate, had a bandage interfering with placement of VR headset, were non-English speaking, had a psychiatric condition affecting ability to accurately complete the survey, or had a reported history of a seizure disorder. The type of skin cancer for which the patient was being treated was recorded. After the first Mohs surgery layer was removed, patients completed a pre-VR experience survey. After completion of the pre-VR survey, participants participated in a 10-minute VR experience. Immediately after the experience, patients completed a post-VR survey.
Instruments
The pre-VR survey asked patients to rate their general health and subjectively endorse a series of symptoms induced by anxiety such as numbness, tingling, wobbliness in legs, dizziness, and rapid heart rate. Answer choices included “not at all,” “mildly—but it doesn’t bother me much,” “moderately—it’s unpleasant, but I can stand it,” and “severely—I can barely stand it.” These questions were taken from the previously published and validated Beck Anxiety Inventory (BAI), a 21-item scale that serves as the most widely used instrument for detecting anxiety. The authors used scores of components relevant to their patient population. Components were used rather than the BAI in its entirety due to the medical setting in which the survey was used relative to the psychiatric setting in which the survey was validated. Beck Anxiety Inventory questions relevant to skin cancer surgery were used, and select questions that were more general in nature were excluded from data collection and subsequent analyses. Differences between pre-VR and post-VR answers were analyzed. Questions regarding history of anxiety and current health status were also included in the surveys in addition to questions regarding patients’ subjective experience with the VR headsets. Patients were also asked to self-report technology savvy on a scale of 1 to 10, with 1 representing the lowest level of technology proficiency and 10 representing the highest.
Equipment
There were 2 types of VR headsets used in the study. The first headset was a Google Daydream headset (Figure 1). Using this headset, patients viewed a series of 3 videos that ran for a total of approximately 10 minutes. All patients watched all 3 videos. The 3 videos were chosen for their relatively relaxing nature and minimal sensory stimulation. They comprised an experience at Joshua Tree National Park, a video of the 1962 moon landing, and an equestrian piece in which the viewer watched a horse and rider complete choreography. The second headset was a Vive VR headset (Figure 2). In this headset, patients viewed TheBlu, an underwater experience comprising passive viewing of wales, jellyfish, and other sea creatures. The alternate Vive experience was titled Tilt Brush, in which the patients painted 3-dimensional artwork (Figure 3). The patients were randomized to either of the 2 available headsets and in the case of the Vive, alternated between the 2 available experiences. Thus, patients did not pick VR experiences, but rather, it was randomly assigned.
Figure 1.
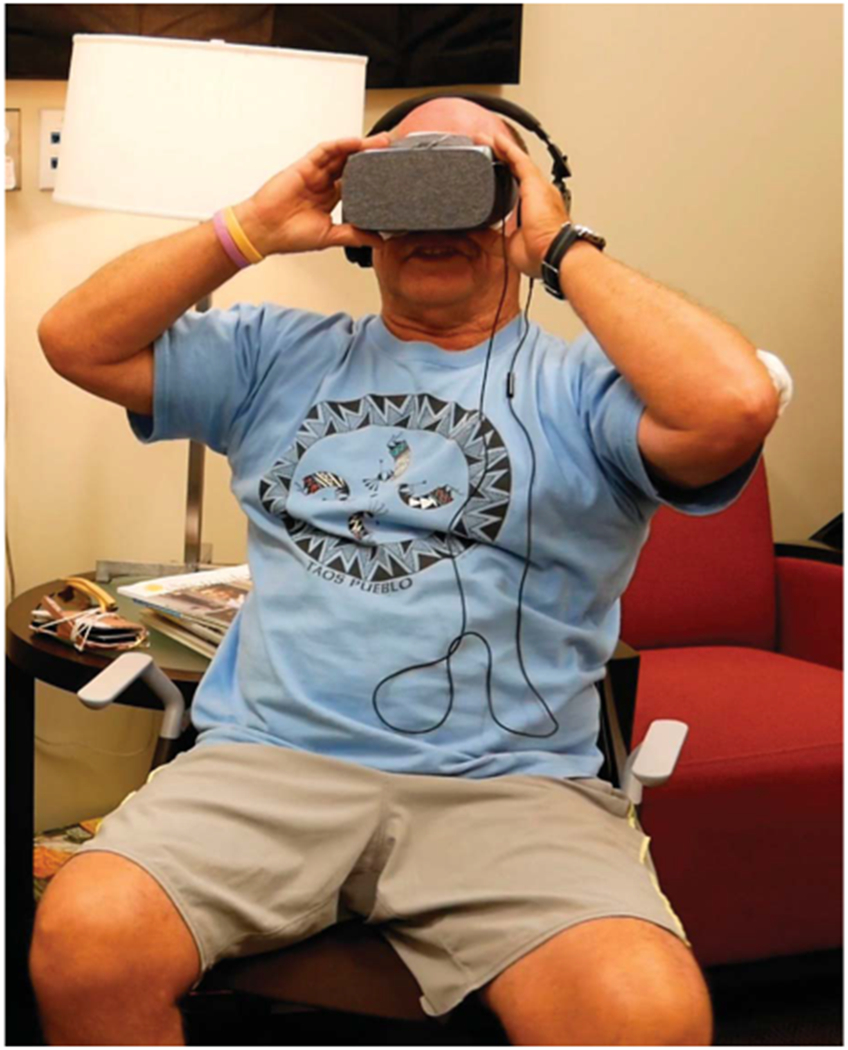
Volunteer patient in the Daydream headset.
Figure 2.

Volunteer patient in a Vive VR headset. VR, virtual reality.
Figure 3.

Volunteer patient beginning a Tilt Brush 3D painting experience.
Statistical Analysis
Analytic procedures were conducted using SAS Version 9.4. Differences in the pre-VR survey and post-VR survey were compared using the chi-square test. The anxiety scores were compared using a t-test.
Results
Baseline Characteristics
A total of 133 consecutive patients were approached during study recruitment. Sixteen declined participation, 2 of whom declined after completion of the presurvey. Of the 117 patients who agreed to participate, 109 completed the study in its entirety (Table 1). Of those who completed the study, the average age of patients was 63.15 years (SD 16.26). There were slightly more male participants with 65 (59.6%) men and 44 (40.4%) women.
TABLE 1.
Demographic Characteristics of Patients Participating in Virtual Reality to Improve the Experience of Mohs Procedure
| Patient Recruitment | ||
| Number approached | 133 | 100.0% |
| Number declined | 16 | 12.0% |
| Survey completion | ||
| Completed presurvey | 119 | 100.0% |
| Completed postsurvey | 113 | 95.0% |
| Completed both | 109 | 83.2% |
| Patient Characteristics | Mean | SD |
|---|---|---|
| Age | 63.15 | 16.26 |
| n | % | |
| Sex | ||
| Male | 65 | 59.6 |
| Female | 44 | 40.4 |
| Cancer type | ||
| Basal cell carcinoma | 74 | 67.9 |
| Squamous cell carcinoma | 26 | 23.9 |
| Other | 9 | 8.3 |
| History of anxiety | ||
| Yes | 22 | 20.2 |
| No | 87 | 79.8 |
| Current health | ||
| Excellent | 25 | 22.9 |
| Very good | 58 | 53.2 |
| Fair | 24 | 22.0 |
| Poor | 2 | 1.8 |
Seventy-four patients (67.9%) were undergoing Mohs surgery for removal of basal cell carcinoma, while 26 (23.9%) were undergoing surgery for squamous cell carcinoma, and 9 patients (8.3%) were undergoing Mohs surgery for other types of cutaneous tumors. The majority of patients did not have a history of anxiety (87, 79.8%) and most patients self-reported their health at the time of participation to be excellent (25, 22.9%) or very good (58, 53.2%) (Table 1).
Background Virtual Reality Experience
Regarding previous technology and VR use, most patients self-reported their technology savvy as intermediate, with most of the scores falling between a 5 and 8 on a scale of 1 to 10 with a 1 corresponding to the least technology savvy and 10 corresponding to the most. The majority of patients had neither previously used VR technology (77.1%) nor played video games (72.5%). The type of VR headset used by patients was approximately split with 50.5% of patients using the Daydream headset, 40.4% using the Vive headset, and the remainder not specifying which headset was used.
Anxiety-Related Questions
In all but 2 questions, there was a trend toward improvement of the anxiety-related sensation after completion of the VR experience. There were statistically significant differences for 4 questions: “Are you currently feeling unable to relax” (p = .0013), “are you currently feeling fear of the worst happening” (p < .0001), “are you currently feeling terrified or afraid” (p = .0046), and “are you currently feeling nervous” (p < .0001) (Table 2). Furthermore, the difference between a mean of the score of all anxiety-related questions taken from the BAI in the pre-VR versus post-VR surveys demonstrated a strongly significant difference between pre-VR and post-VR surveys (p < .0001) (Table 2). This significance was maintained in subgroup analyses when broken down by sex, age (≤65 years old and >65 years old), and headset type (Table 2). There were no statistically significant differences in patient satisfaction and pain measures between presurvey and postsurvey measures (Table 2).
TABLE 2.
VR Presurvey and Postsurvey Responses n = 109
|
Pre-VR Response |
Post-VR Response |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Weighted Score of Components (Similar to BAI) | Mean | SD | Mean | SD | p* | ||||
| Anxiety-related questions | |||||||||
| Overall | 4.66 | 4.24 | 1.84 | 2.83 | <.0001 | ||||
| Sex | |||||||||
| Male | 4.97 | 4.57 | 2.11 | 2.96 | <.0001 | ||||
| Female | 4.20 | 3.71 | 1.45 | 2.62 | <.0001 | ||||
| Age | |||||||||
| ≤65 (n = 57) | 5.14 | 4.88 | 2.05 | 3.16 | <.0001 | ||||
| >65 (n = 52) | 4.13 | 3.38 | 1.62 | 2.43 | <.0001 | ||||
| VR headset | |||||||||
| Vive | 4.68 | 4.48 | 1.75 | 2.61 | <.0001 | ||||
| Daydream | 4.55 | 4.10 | 1.96 | 2.93 | <.0001 | ||||
|
Pre-VR Response |
Post-VR Response |
||||||||
| Measures | Responses | n | % | n | % | p* | |||
| Anxiety-related questions | |||||||||
| Any wobbliness in your legs? | Not at all | 88 | 80.7 | 94 | 86.2 | 0.7344 | |||
| Mildly–it doesn’t bother me much | 17 | 15.6 | 12 | 11.0 | |||||
| Moderately–it’s unpleasant, but I can stand it | 3 | 2.8 | 2 | 1.8 | |||||
| Severely–I can barely stand it | 1 | 0.9 | 1 | 0.9 | |||||
| Unable to relax? | Not at all | 71 | 65.1 | 86 | 78.9 | 0.0013 | |||
| Mildly–it doesn’t bother me much | 28 | 25.7 | 20 | 18.3 | |||||
| Moderately–it’s unpleasant, but I can stand it | 10 | 9.2 | 2 | 1.8 | |||||
| Severely–I can barely stand it | 0 | 0.0 | 1 | 0.9 | |||||
| Fear of the worst happening? | Not at all | 62 | 56.9 | 94 | 86.2 | <.0001 | |||
| Mildly–it doesn’t bother me much | 31 | 28.4 | 8 | 7.3 | |||||
| Moderately–it’s unpleasant, but I can stand it | 11 | 10.1 | 3 | 2.8 | |||||
| Severely–I can barely stand it | 1 | 0.9 | 0 | 0.0 | |||||
| Faint, dizzy, or lightheaded? | Not at all | 86 | 78.9 | 91 | 83.5 | 0.5960 | |||
| Mildly–it doesn’t bother me much | 16 | 14.7 | 14 | 12.8 | |||||
| Moderately–it’s unpleasant, but I can stand it | 4 | 3.7 | 2 | 1.8 | |||||
| Severely–I can barely stand it | 1 | 0.9 | 0 | 0.0 | |||||
| Your heart is pounding or racing? | Not at all | 92 | 84.4 | 99 | 90.8 | 0.1718 | |||
| Mildly–it doesn’t bother me much | 12 | 11.0 | 7 | 6.4 | |||||
| Moderately–it’s unpleasant, but I can stand it | 3 | 2.8 | 1 | 0.9 | |||||
| Severely–I can barely stand it | 0 | 0.0 | 0 | 0.0 | |||||
| Terrified or afraid? | Not at all | 86 | 78.9 | 102 | 93.6 | 0.0046 | |||
| Mildly–it doesn’t bother me much | 17 | 15.6 | 6 | 5.5 | |||||
| Moderately–it’s unpleasant, but I can stand it | 5 | 4.6 | 0 | 0.0 | |||||
| Severely–I can barely stand it | 0 | 0.0 | 0 | 0.0 | |||||
| Nervous? | Not at all | 58 | 53.2 | 85 | 78.0 | <.0001 | |||
| Mildly–it doesn’t bother me much | 39 | 35.8 | 21 | 19.3 | |||||
| Moderately–it’s unpleasant, but I can stand it | 11 | 10.1 | 1 | 0.9 | |||||
| Severely–I can barely stand it | 0 | 0.0 | 0 | 0.0 | |||||
| As though your hands are trembling? | Not at all | 95 | 87.2 | 95 | 87.2 | 0.8013 | |||
| Mildly–it doesn’t bother me much | 12 | 11.0 | 13 | 11.9 | |||||
| Moderately–it’s unpleasant, but I can stand it | 1 | 0.9 | 0 | 0.0 | |||||
| Severely–I can barely stand it | 0 | 0.0 | 0 | 0.0 | |||||
| Shaky/unsteady? | Not at all | 82 | 75.2 | 90 | 82.6 | 0.5895 | |||
| Mildly–it doesn’t bother me much | 21 | 19.3 | 17 | 15.6 | |||||
| Moderately–it’s unpleasant, but I can stand it | 4 | 3.7 | 1 | 0.9 | |||||
| Severely–I can barely stand it | 1 | 0.9 | 0 | 0.0 | |||||
| Fear of losing control? | Not at all | 98 | 89.9 | 104 | 95.4 | 0.4232 | |||
| Mildly–it doesn’t bother me much | 7 | 6.4 | 3 | 2.8 | |||||
| Moderately–it’s unpleasant, but I can stand it | 2 | 1.8 | 1 | 0.9 | |||||
| Severely–I can barely stand it | 1 | 0.9 | 0 | 0.0 | |||||
| Difficulty breathing? | Not at all | 104 | 95.4 | 103 | 94.5 | 0.3916 | |||
| Mildly–it doesn’t bother me much | 3 | 2.8 | 6 | 5.5 | |||||
| Moderately–it’s unpleasant, but I can stand it | 2 | 1.8 | 0 | 0.0 | |||||
| Severely–I can barely stand it | 0 | 0.0 | 0 | 0.0 | |||||
| Fear of dying? | Not at all | 92 | 84.4 | 96 | 88.1 | 0.4615 | |||
| Mildly–it doesn’t bother me much | 14 | 12.8 | 9 | 8.3 | |||||
| Moderately–it’s unpleasant, but I can stand it | 3 | 2.8 | 3 | 2.8 | |||||
| Severely–I can barely stand it | 0 | 0.0 | 1 | 0.9 | |||||
| Indigestion | Not at all | 93 | 85.3 | 99 | 90.8 | 0.1290 | |||
| Mildly–it doesn’t bother me much | 12 | 11.0 | 9 | 8.3 | |||||
| Moderately–it’s unpleasant, but I can stand it | 3 | 2.8 | 0 | 0.0 | |||||
| Severely–I can barely stand it | 0 | 0.0 | 0 | 0.0 | |||||
| Like your face is flushed? | Not at all | 97 | 89.0 | 99 | 90.8 | 0.3916 | |||
| Mildly–it doesn’t bother me much | 8 | 7.3 | 7 | 6.4 | |||||
| Moderately–it’s unpleasant, but I can stand it | 3 | 2.8 | 2 | 1.8 | |||||
| Severely–I can barely stand it | 0 | 0.0 | 0 | 0.0 | |||||
| Hot/cold sweats? | Not at all | 98 | 89.9 | 106 | 97.2 | 0.1736 | |||
| Mildly–it doesn’t bother me much | 7 | 6.4 | 2 | 1.8 | |||||
| Moderately–it’s unpleasant, but I can stand it | 2 | 1.8 | 0 | 0.0 | |||||
| Severely–I can barely stand it | 1 | 0.9 | 0 | 0.0 | |||||
| Pain-related questions (n=99†) | |||||||||
| Rate pain you are currently experiencing | 1–2 | 88 | 80.7 | 90 | 82.6 | 0.7254 | |||
| 3–4 | 2 | 1.8 | 4 | 3.7 | |||||
| 4–6 | 5 | 4.6 | 1 | 0.9 | |||||
| 7–8 | 2 | 1.8 | 2 | 1.8 | |||||
| 9–10 | 2 | 1.8 | 2 | 1.8 | |||||
| Satisfaction-related questions | |||||||||
| I think my doctors office has everything needed to provide complete medical care | Strongly agree | 92 | 84.4 | 94 | 86.2 | 0.5637 | |||
| Agree | 17 | 15.6 | 15 | 13.8 | |||||
| Uncertain | 0 | 0.0 | 0 | 0.0 | |||||
| Disagree | 0 | 0.0 | 0 | 0.0 | |||||
| Strongly disagree | 0 | 0.0 | 0 | 0.0 | |||||
| The medical care I have been receiving is just about perfect. | Strongly agree | 100 | 91.7 | 97 | 89.0 | 0.3173 | |||
| Agree | 9 | 8.3 | 12 | 11.0 | |||||
| Uncertain | 0 | 0.0 | 0 | 0.0 | |||||
| Disagree | 0 | 0.0 | 0 | 0.0 | |||||
| Strongly disagree | 0 | 0.0 | 0 | 0.0 | |||||
| I am dissatisfied with some things about the medical care I receive | Strongly agree | 3 | 2.8 | 0 | 0.0 | 0.747 | |||
| Agree | 0 | 0.0 | 1 | 0.9 | |||||
| Uncertain | 1 | 0.9 | 1 | 0.9 | |||||
| Disagree | 24 | 22.0 | 17 | 15.6 | |||||
| Strongly disagree | 81 | 74.3 | 90 | 82.6 | |||||
p-value for the Pearson chi-squared test for independence.
Total number of patients who completed all presurvey and postsurvey pain-related questions.
BAI, Beck Anxiety Inventory; VR, virtual reality.
Descriptive data were obtained for the subjective VR experience. The majority of patients reported that the VR experience “definitely improved” or “somewhat improved” (52.2% and 30.4%, respectively) any surgical day anxiety they may have been experiencing (Table 3). Similarly, most patients reported that they felt the VR experience “definitely” or “somewhat improved” their overall experience/satisfaction with the day (73.9% and 17.4%, respectively) (Table 3). Most patients reported that the VR experience did not subjectively improve surgical pain they may have been experiencing (Table 3).
TABLE 3.
Subjective Experience Responses From Mohs Patients Participating in a Virtual Reality Experience
| n = 92* | n | % |
|---|---|---|
| Do you feel that the virtual reality experience today helped improve any surgical day anxiety you may have been experiencing? | ||
| Yes | 48 | 52.2 |
| No | 16 | 17.4 |
| Somewhat | 28 | 30.4 |
| Do you feel the virtual reality experience today improved any surgical pain you may have experienced? | ||
| Yes | 37 | 40.2 |
| No | 42 | 45.7 |
| Somewhat | 13 | 14.1 |
| Do you feel the virtual reality experience today improved your overall experience/satisfaction with the day? | ||
| Yes | 68 | 73.9 |
| No | 6 | 6.5 |
| Somewhat | 16 | 17.4 |
| What type of general experiences did you participate in today? | ||
| Passive | 82 | 75.2 |
| Interactive | 27 | 24.8 |
| How comfortable was wearing the headset on your face? | ||
| Very comfortable | 42 | 38.5 |
| Comfortable | 48 | 44.0 |
| Slightly uncomfortable | 18 | 16.5 |
| Very uncomfortable | 1 | 0.9 |
| In the future, would you appreciate virtual reality experiences of solitude or social experiences? | ||
| Solitude | 78 | 75.7 |
| Social | 25 | 24.3 |
Total number of patients who completed all related presurvey- and postsurvey-related questions.
Discussion
Virtual reality technology has previously been used in the context of various medical conditions and procedures, in which its efficacy in anxiety and pain reduction has been evidenced. Here, the authors present a prospective interventional study of VR technology used specifically in the outpatient surgical setting to effectively combat anxiety and improve the overall patient experience in the context of skin cancer removal. In demonstrating results consistent with previous VR studies, this study provides valuable data that suggest the scalability of VR technology to the outpatient surgical setting and specifically, to improving the anxiety and overall patient satisfaction of patients undergoing Mohs surgery. Practically speaking, this scalability is further elucidated by the increasing affordability and user friendly nature of recent headsets, making them accessible to a wide array of practices and patients.
In the context of anxiety, VR has primarily been studied in the context of psychological disorders such as specific phobias, social anxiety disorder, panic disorder and agoraphobia, obsessive compulsive disorder, and schizophrenia.28 It has also been used for the treatment of addiction, eating pathologies, and autism.28 In these contexts, VR has been useful given the possibility of constructing, manipulating, and individualizing therapeutic exposures that may be difficult to implement in vivo.28 In the context of medical procedures, the efficacy of VR in managing and attenuating patient anxiety has been predominantly attributed to the power of distraction.29 This is likely responsible for most of the effect seen in this study in which the authors expand the applications into treatment of anxiety in the preoperative environment.
In the authors’ study, pain was not significantly improved by the VR experience, although this was likely secondary to study design and the authors’ patient population. Immediately after removal of the first Mohs layer, most of the patients experienced the residual effects of local anesthetic used during the procedure and remained anesthetized throughout the VR experience and subsequently, the post-VR survey. Similarly, in literature, most Mohs surgery patients report a low level of pain, although the highest levels of pain are reported on the day of surgery with a steady decline until postoperative Day 4.30 Intraoperative pain with the Mohs surgery procedure has been reported by 32% of patients in one Phase 1 study.31 In previous studies, pain was more commonly reported by patients who spent a longer time in the office, had 3 or more Mohs layers, and had a flap or graft repair.31 Patients were also more likely to report pain with surgical sites of the periorbital area and nose.31 These data in the current body of literature are supported by the low pain scores reported in both the pre-VR and post-VR surveys in the authors’ study. Most patients graded their pain as a “1 or 2” on a 10-point scale both before and after the VR experience (80.7% and 82.6%, respectively). In addition, as many of the patients were aged older than 60 years, many experienced chronic pain and misinterpreted the pain question as a means to assess their chronic rather than acute surgical pain.
An additional limitation of this study includes the use of individual questions from the BAI, rather than the BAI in its entirety. The authors chose to include only individual components of the BAI that are relevant to outpatient surgery rather than chronic medical conditions. Despite an effort to eliminate the effect of questions that may be measuring the effect of baseline comorbid medical conditions rather than that of the acute surgical experience, several questions included in the study have potential for confounding. For example, questions such as “do you feel as though your hands are trembling” or “do you have any difficulty breathing” may be measuring baseline medical conditions rather than measuring active anxiety symptoms due to the surgical procedure. In addition, the authors used 2 separate types of VR headsets that may alter individual patient experiences, although the patients were randomized and did not choose their experience. This was performed to determine the differential ability of various headsets and experiences to demonstrably improve the measured outcomes and both demonstrated statistically significant differences in pre-VR and post-VR BAI scores. In addition, it is possible that patients may have spontaneously become progressively less stressed as they spent more time in the waiting room, although this is unlikely given the significant and simultaneous improvement in multiple questions assessing levels of stress, fear, and/or anxiety. The authors’ study is further limited by the lack of a control group and should be replicated with the inclusion of such a group. Furthermore, there also exists the possibility of several biases. This includes one due to patients possibly selecting improvement in measured outcomes due to study inclusion. Another bias may result from the fact that 16 patients who declined to participate may not have been as receptive to the VR experience when compared with those who agreed to participate.
Of note, although the authors considered having patients complete the pre-VR survey before the first Mohs layer when patients may be more anxious, the authors ultimately opted to flank the VR experience with the pre-VR and post-VR survey to directly isolate the effect of the experience on measured outcomes. It was not feasible to complete both surveys and the VR experience before the first Mohs layer given the authors’ limited research staff and the risk of disrupting the clinical flow during the surgical day.
Despite its limitations, this study is the largest of its kind to demonstrate the ability of VR to increase relaxation, improve overall patient satisfaction, and decrease feelings of fear and nervousness in the outpatient skin cancer surgical setting. Given the levels of distress, anxiety, and QOL impairment experienced by patients with NMSC, particularly surrounding the surgical experience, the authors’ prospective intervention trial demonstrates the utility of a VR experience to help address these issues. Further study will focus on identifying features of the cohort that will most benefit from the VR experience in addition to identifying ideal device parameters and improving the pairing of device/experience with the patient for optimal patient experience outcomes.
Footnotes
The authors have indicated no significant interest with commercial supporters. Springbok Cares provided the personnel and virtual reality equipment required for completion of this study free of cost.
References
- 1.Stern RS. Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol 2010;146:279–82. [DOI] [PubMed] [Google Scholar]
- 2.Perera E, Gnaneswaran N, Staines C, Win AK, et al. Incidence and prevalence of non-melanoma skin cancer in Australia: a systematic review. Australas J Dermatol 2015;56:258–67. [DOI] [PubMed] [Google Scholar]
- 3.Leiter U, Eigentler T, Garbe C. Epidemiology of skin cancer. Adv Exp Med Biol 2014;810:120–40. [DOI] [PubMed] [Google Scholar]
- 4.Perera E, Sinclair R. An estimation of the prevalence of nonmelanoma skin cancer in the. U.S F1000Res 2013;2:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guy GP Jr, Machlin SR, Ekwueme DU, Yabroff KR. Prevalence and costs of skin cancer treatment in the U.S., 2002–2006 and 2007–2011. Am J Prev Med 2015;48:183–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the U.S. Population, 2012. JAMA Dermatol 2015;151:1081–6. [DOI] [PubMed] [Google Scholar]
- 7.Rogers HW, Weinstock MA, Harris AR, Hinckley MR, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol 2010;146:283–7. [DOI] [PubMed] [Google Scholar]
- 8.John Chen G, Yelverton CB, Polisetty SS, Housman TS, et al. Treatment patterns and cost of nonmelanoma skin cancer management. Dermatol Surg 2006;32:1266–71. [DOI] [PubMed] [Google Scholar]
- 9.Korner A, Garland R, Czajkowska Z, Coroiu A, et al. Supportive care needs and distress in patients with non-melanoma skin cancer: nothing to worry about? Eur J Oncol Nurs 2016;20:150–5. [DOI] [PubMed] [Google Scholar]
- 10.Bates AS, Davis CR, Takwale A, Knepil GJ. Patient-reported outcome measures in nonmelanoma skin cancer of the face: a systematic review. Br J Dermatol 2013;168:1187–94. [DOI] [PubMed] [Google Scholar]
- 11.Housman TS, Feldman SR, Williford PM, Fleischer AB Jr, et al. Skin cancer is among the most costly of all cancers to treat for the Medicare population. J Am Acad Dermatol 2003;48:425–9. [DOI] [PubMed] [Google Scholar]
- 12.Asgari MM, Warton EM, Neugebauer R, Chren MM. Predictors of patient satisfaction with Mohs surgery: analysis of preoperative, intraoperative, and postoperative factors in a prospective cohort. Arch Dermatol 2011;147:1387–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ganry L, Hersant B, Sidahmed-Mezi M, Dhonneur G, et al. Using virtual reality to control preoperative anxiety in ambulatory surgery patients: a pilot study in maxillofacial and plastic surgery. J Stomatol Oral Maxillofac Surg 2018;119:257–61. [DOI] [PubMed] [Google Scholar]
- 14.Gold JI, Belmont KA, Thomas DA. The neurobiology of virtual reality pain attenuation. Cyberpsychol Behav 2007;10:536–44. [DOI] [PubMed] [Google Scholar]
- 15.Gold JI, Kim SH, Kant AJ, Joseph MH, et al. Effectiveness of virtual reality for pediatric pain distraction during i.v. placement. Cyberpsychol Behav 2006;9:207–12. [DOI] [PubMed] [Google Scholar]
- 16.Li A, Montaño Z, Chen VJ, Gold JI. Virtual reality and pain management: current trends and future directions. Pain Manag 2011;1: 147–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trost Z, Zielke M, Guck A, Nowlin L, et al. The promise and challenge of virtual gaming technologies for chronic pain: the case of graded exposure for low back pain. Pain Manag 2015;5:197–206. [DOI] [PubMed] [Google Scholar]
- 18.Small C, Stone R, Pilsbury J, Bowden M, et al. Virtual restorative environment therapy as an adjunct to pain control during burn dressing changes: study protocol for a randomised controlled trial. Trials 2015; 16:329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Triberti S, Repetto C, Riva G. Psychological factors influencing the effectiveness of virtual reality-based analgesia: a systematic review. Cyberpsychol Behav Soc Netw 2014;17:335–45. [DOI] [PubMed] [Google Scholar]
- 20.Garrett B, Taverner T, Masinde W, Gromala D, et al. A rapid evidence assessment of immersive virtual reality as an adjunct therapy in acute pain management in clinical practice. Clin J Pain 2014;30:1089–98. [DOI] [PubMed] [Google Scholar]
- 21.Keefe FJ, Huling DA, Coggins MJ, Keefe DF, et al. Virtual reality for persistent pain: a new direction for behavioral pain management. Pain 2012;153:2163–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev 2010;30:1011–8. [DOI] [PubMed] [Google Scholar]
- 23.Shahrbanian S, Ma X, Korner-Bitensky N, Simmonds MJ. Scientific evidence for the effectiveness of virtual reality for pain reduction in adults with acute or chronic pain. Stud Health Technol Inform 2009;144:40–3. [PubMed] [Google Scholar]
- 24.Morris LD, Louw QA, Grimmer-Somers K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: a systematic review. Clin J Pain 2009;25:815–26. [DOI] [PubMed] [Google Scholar]
- 25.Maurice-Szamburski A Preoperative virtual reality experience may improve patient satisfaction and reduce anxiety. Evid Based Nurs 2018; 21:14. [DOI] [PubMed] [Google Scholar]
- 26.Gold JI, Mahrer NE. Is virtual reality ready for prime time in the medical space? A randomized control trial of pediatric virtual reality for acute procedural pain management. J Pediatr Psychol 2018;43:266–75. [DOI] [PubMed] [Google Scholar]
- 27.Gladstone HB, Raugi GJ, Berg D, Berkley J, et al. Virtual reality for dermatologic surgery: virtually a reality in the 21st century. J Am Acad Dermatol 2000;42(1 Pt 1):106–12. [DOI] [PubMed] [Google Scholar]
- 28.Maples-Keller JL, Bunnell BE, Kim SJ, Rothbaum BO. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv Rev Psychiatry 2017;25:103–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arane K, Behboudi A, Goldman RD. Virtual reality for pain and anxiety management in children. Can Fam Physician 2017;63:932–4. [PMC free article] [PubMed] [Google Scholar]
- 30.Firoz BF, Goldberg LH, Arnon O, Mamelak AJ. An analysis of pain and analgesia after Mohs micrographic surgery. J Am Acad Dermatol 2010;63:79–86. [DOI] [PubMed] [Google Scholar]
- 31.Connolly KL, Nehal KS, Dusza SW, Rossi AM, et al. Assessment of intraoperative pain during Mohs micrographic surgery (MMS): an opportunity for improved patient care. J Am Acad Dermatol 2016;75:590–4. [DOI] [PMC free article] [PubMed] [Google Scholar]


