Abstract
Objectives
Emergency department boarding is the practice of caring for admitted patients in the emergency department after hospital admission, and boarding has been a growing problem in the United States. Boarding of the critically ill has achieved specific attention because of its association with poor clinical outcomes. Accordingly, the Society of Critical Care Medicine and the American College of Emergency Physicians convened a Task Force to understand the implications of emergency department boarding of the critically ill. The objective of this article is to review the U.S. literature on (1) the frequency of emergency department boarding among the critically ill, (2) the outcomes associated with critical care patient boarding, and (3) local strategies developed to mitigate the impact of emergency department critical care boarding on patient outcomes.
Data sources and study selection
Review article.
Data extraction and data synthesis
Emergency department–based boarding of the critically ill patient is common, but no nationally representative frequency estimates has been reported. Boarding literature is limited by variation in the definitions used for boarding and variation in the facilities studied (boarding ranges from 2% to 88% of ICU admissions). Prolonged boarding in the emergency department has been associated with longer duration of mechanical ventilation, longer ICU and hospital length of stay, and higher mortality. Health systems have developed multiple mitigation strategies to address emergency department boarding of critically ill patients, including emergency department‐based interventions, hospital‐based interventions, and emergency department–based resuscitation care units.
Conclusions
Emergency department boarding of critically ill patients was common and was associated with worse clinical outcomes. Health systems have generated a number of strategies to mitigate these effects. A definition for emergency department boarding is proposed. Future work should establish formal criteria for analysis and benchmarking of emergency department–based boarding overall, with subsequent efforts focused on developing and reporting innovative strategies that improve clinical outcomes of critically ill patients boarded in the emergency department.
Keywords: boarding; critical care outcomes; critical care; emergency department‐intensive care unit; emergency service, hospital; resuscitation care units
The most sophisticated intensive care often becomes unnecessarily expensive terminal care when the pre‐ICU system fails. 1
—Peter Safar
In 2002, the Crowding Resources Task Force proposed a framework to understand how quality of care and outcomes relate to emergency department (ED) crowding. That framework was comprised of four key directives:
to develop measures of ED crowding that are valid, reliable, and sensitive to changes;
to identify the most important causes of ED crowding;
to measure the effect of crowding on quality of care; and
to evaluate interventions to decrease crowding. 2
Over the intervening period, ED crowding was compounded by widespread boarding: the prolonged treatment of patients in the ED after inpatient admission decisions because of the lack of inpatient bed availability. Although much has been written about ED boarding, the impact of boarding on the critically ill has not been completely explored. Many factors influence outcomes for patients awaiting ICU admission, including a safe and effective nursing staffing model, physician training and attention (prioritizing boarding inpatients during care of new patients), multidisciplinary team availability and staffing (e.g., pharmacists, physical therapists, respiratory therapists, etc.), and standardized care pathways that minimize harm and promote recovery from critical illness (e.g., delirium prevention, early mobility, nutrition).
Boarding critically ill patients stresses a burdened emergency care system. ED patient volumes have increased by 30% in the past decade, and hospital closures have led to an increase in inpatient boarding in many U.S. EDs. 2 , 3 , 4 Inpatient critical care occupancy has also been increasing. 5 This lack of inpatient capacity is the primary driver of ED boarding, and this is true even for the critically ill. 6 Most ED operations were built around diagnostic testing and medical stabilization, and the paradigm of inpatient care in the ED is underdeveloped. Emergency physicians are trained in the stabilization of the critically ill, but longitudinal management has not been a sustained focus of residency training.
Recognizing the increased burden of ED boarding of the critically ill and the impact of boarding on patient outcomes even after ICU arrival, the Society of Critical Care Medicine (SCCM) and the American College of Emergency Physicians (ACEP) jointly convened the ED‐Critical Care Medicine (ED‐CCM) Boarding Task Force in 2017. Members of the Task Force include emergency physicians, critical care physicians, an acute care nurse practitioner, and a clinical pharmacist, all involved with the care of critically ill patients boarding in the ED. The Task Force drafted this white paper, based on the directives described in the Crowding Task Force report in 2002, to explore the current state of ED boarding of the critically ill and offer direction for future efforts of optimizing care delivery for these patients.
1. METHODOLOGY
1.1. Task force structure
Members of the ED‐CCM Boarding Task Force were appointed by the presidents of SCCM and ACEP. Representatives were selected to have broad experience in emergency medicine, Critical Care Medicine, and to include individuals with experience caring for boarding critically ill patients. Cochairs of the task force represented the Chairs of the Emergency Medicine Section of SCCM (B.T.W.) and the Critical Care Section of ACEP (N.M.M.).
1.2. Focus areas
The Task Force determined that the scope of this report would be (1) to describe best available estimates on the frequency of ED boarding of critically ill adults within US EDs since 2000, (2) to summarize the association between ED‐CCM boarding and patient‐oriented outcomes, and (3) to explore local mitigation strategies developed to combat the deleterious effects of ED‐CCM boarding. With that goal, the Task Force divided into three work groups: prevalance, outcomes, and mitigation strategies. Each work group individualized their approach based on existing literature and resources. Due to heterogeneity in international delivery of emergency care and critical care (specifically with regard to financial, cultural, and clinical system‐based models of care) and concerns that international insights might not parallel the U.S. model of healthcare delivery, international literature was excluded. We also limited this discussion to management of patients identified for ICU admission; our focus did not include variation in the regional distribution of ICU patients between hospitals or the appropriate triage of patients for ICU‐level care within a hospital.
The Task Force additionally resolved to (1) avoid financial, satisfaction, or administrative metrics, (2) focus on data primarily from adult studies, and (3) recognize that health system variation could be substantial and that available literature may be biased in reporting the experience of academic medical centers, primarily. Ultimately, the Task Force aspired to develop recommendations for further study on mitigation strategy development and dissemination. All recommendations and conclusions were made using a modified Delphi method with unanimous approval by Task Force members. This article reports the results of the Task Force's work in the format of a review article.
1.3. Systematic review
As one subset of the entire scope of work, the Task Force conducted a systematic review to define the frequency of ED‐CCM boarding (Fig. 1). Inclusion criteria were broadly defined as an estimate of the frequency of ED‐CCM boarding regardless of unit of analysis (including national, regional, health system, or individual hospital data). This literature search was conducted on April 12, 2018 and resulted in 174 papers that met the broad definition of frequency of ED‐CCM boarding. Studies published before 2000 (selected because few relevant articles were published before this date), data collected exclusively outside the United States, or articles without a clear definition of boarding criteria were excluded. Each article was reviewed for inclusion and data abstracted by two independent reviewers (from among the following reviewers: N.M.M., M.‐C.E.‐T., K.M.J., S.R.), resulting in 18 papers relevant for inclusion.
FIGURE 1.
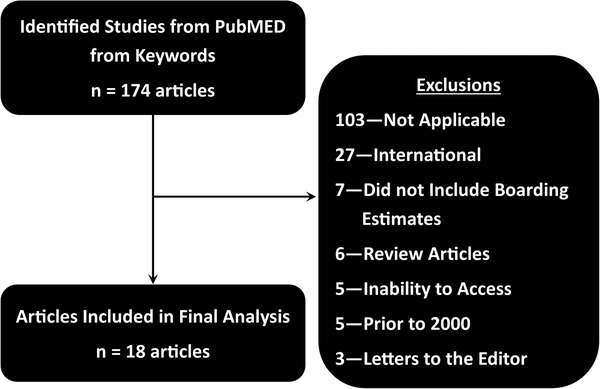
Literature search strategy for defining the frequency of emergency department critically ill patient boarding. A MEDLINE search was conducted with the assistance of a medical librarian (Heather Healy) using the following search terms: (((((“emergency service, hospital”[MeSH Terms] OR emergency[tw]))) AND ((“crowding”[MeSH Terms] OR boarding[tw] OR crowding[tw] OR overcrowding[tw] OR patient throughput[tw] OR patient flow[tw]))) AND ((“ICUs”[MeSH Terms] OR ICUs[tw] OR ICU[tw] OR ICU[tw] OR ICUs[tw] OR “critical illness”[MeSH Terms] OR critical illness[tw] OR critically ill[tw] OR critical patient[tw] OR critical patients[tw])))
2. RESULTS
2.1. To what extent is critical care medicine being provided in the ED?
EDs are providing more critical care procedures and management traditionally delivered within the confines of an ICU. ED visits for critically ill patients increased by 80% between 2006 and 2014, from 2.8 to 5.2 million visits 7 , 8 . Similarly, the number of patients intubated in the ED increased by 16% during this period (unpublished data estimated from National ED Sample, Healthcare Utilization Project, Agency for Healthcare Research and Quality [AHRQ]). 8 Over this corresponding period, there was minimal growth in available ED capacity and inpatient ICU beds. 9 This increased volume could be predicted, as the prevalence of chronic obstructive pulmonary disease and diabetes mellitus continue to increase, and sepsis incidence also has risen 10 , 11 , 12 . Estimates of critical care billing range between 15% and 20% of total ED volume at tertiary academic medical centers. 13
ED management of specific critical care–sensitive conditions also is increasing. Annually, 250,000 patients receive mechanical ventilation in U.S. EDs, with a reported median ED length of stay of greater than 3 hours. 14 Over 1.7 million cases of sepsis are treated in U.S. hospitals each year, and more than half of those are admitted from the ED. 15 Other common diseases may require critical care in the ED prior to admission, including diabetic ketoacidosis, metabolic derrangements, gastrointestinal hemorrhage, and neurovascular disorders. Unfortunately, the boarding of critically ill patients in the ED is associated with delays in care, which impact broad clinical outcomes in the critically ill. 16 , 17 , 18 , 19 , 20
2.2. How is the boarding of critically Ill patients in EDs currently defined?
No universally accepted consensus definition of ED boarding has been adopted, and as a result, researchers have developed their own varied definitions. This lack of standardization precludes meaningful aggregation of data or comparisons between published results. Some studies describe boarding as total time spent in the ED 18 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , with some defining that time only after the decision to admit. 18 , 20 , 26 One study required that ICU beds be unavailable for ED boarding to occur, 27 whereas another used the distribution of ED wait times to define outliers. 28 Several studies defined a time threshold a priori as greater than 2, 4, or 6 hours. 16 , 29 , 30 , 31 Two studies assessed boarding based only on the total number of hours an intubated patient spent in the ED. 19 , 32 The DELAY‐ED study group identified 6 hours in the ED (from time of arrival at triage) as the definition of ED boarding, based primarily on their observations that adverse outcomes among admitted critically ill patients are more common with an ED stay greater than 6 hours. 31 Nine distinct classifications for boarding definitions were identified and summarized (Supplemental Table 1, Supplemental Digital Content 1, http://links.lww.com/CCM/F477).
Healthcare quality organizations have also published definitions. The Joint Commission defines boarding as “the practice of holding patients in the ED or another temporary location after the decision to admit or transfer has been made. It is recommended that boarding time frames not exceed 4 hours in the interest of patient safety and quality of care”. 33 ACEP delineates boarding “as [remaining] in the ED after [being] admitted or placed into observation status”. 34 The Institute for Healthcare Improvement, Agency for Healthcare Research and Quality, and the American Medical Association each independently curate resources to assist with hospital flow, but they do not formally define boarding. 35 , 36 , 37
2.3. How common Is boarding of critically Ill patients in U.S. EDs?
Our review of published literature suggests that boarding is common for critically ill patients in the ED. The majority of studies were retrospective single‐center reports. Mean length of ED‐CCM boarding (using various definitions) ranged from 1.3 to 8.8 hours. The incidence of critically ill patients boarding in the ED ranged from 2.1% to 87.6%, suggesting that this estimate was sensitive to both setting and boarding definition. 16 , 31 As a result of the significant clinical heterogeneity of the included studies and lack of large regional or national boarding data estimates, data could not be pooled to estimate a standard frequency of ED boarding of critically ill patients. Thus, the generalizability of these published estimates is unclear because of the paucity of literature focused on nonacademic, community, or rural hospitals.
2.4. What clinically relevant outcomes are associated with ED boarding of critically Ill patients?
Both retrospective and prospective observational studies demonstrate worse outcomes for critically ill patients after ED boarding (Supplemental Table 2, Supplemental Digital Content 1, http://links.lww.com/CCM/F477), including increased duration of mechanical ventilation, longer ICU length of stay, and higher mortality. 16 , 18 , 19 , 31 , 32 , 38 , 39 Increased ED boarding times are associated with worsening organ dysfunction and a four‐fold increase in the probability of poor neurologic recovery in patients presenting with stroke. 38 For hospital survivors, extended ED boarding times are associated with a longer hospital length of stay. 40 Chalfin et al. 31 reported higher in‐hospital mortality (17.4% vs 12.9%) among a cohort of 120 hospitals for patients who were in the ED for more than 6 hours (number needed to harm = 22). Cardoso et al. 39 observed that ICU mortality increased with duration of ED boarding (37.6% [immediate admission] vs 43.4% [2–12 hr] vs 46.2% [12–18 hr] vs 52% [18–24 hr] vs 57.1% [> 24 hr]; p = 0.002).
ED boarding also contributes to low‐quality process‐related care of the critically ill waiting for ICU admission. Mechanically ventilated patients rarely have six postintubation care elements performed while boarding in the ED 19 and boarding for more than 7 hours increases duration of mechanical ventilation and hospital mortality. 32 Boarding patients have delays in home medication initiation, fluid, and antibiotic administration, disease‐specific protocolized care, and those boarding in the ED have more medication‐related adverse events than admitted inpatients. 41 , 42 , 43 In addition, inpatient boarding impacts the care of other ED patients. 3 , 40 , 44 , 45 , 46 , 47 , 48
Matthews et al. 18 compared the outcome of critically ill ED patients that are declined ICU admission versus those initially accepted. Boarding times were longer for those declined admission (11.7 vs 4.2 hr). This additional time may have been used to stabilize patients for non‐ICU admission, but the practice of triaging and managing patients who appear too well for ICU admission but too ill for floor admission was time consuming. Even when adjusted for ICU triage decision, critically ill patients with long boarding times had increased rates of persistent organ dysfunction and death.
ED boarding reflects symptoms of a systemic healthcare problem with multiple downstream effects; it is not simply a failure of ED operations. ED‐CCM boarding impacts nursing, respiratory therapy, pharmacy, radiology, and laboratory services, and it contributes to poor staff satisfaction. 49 , 50 Understanding the effect on the care process, staff, and clinical outcomes of critically ill patients may promote collaboration between key clinical and institutional stakeholders to mitigate risk, identify relevant barriers, and explore solutions.
2.5. What mitigation strategies have health systems used to ameliorate the impact of ED boarding on critically Ill patients?
Mitigation strategies were organized into three focus areas: 1) ED solutions, 2) hospital solutions, and 3) ED‐based resuscitative care units (RCUs) (see next section) (Fig. 2).
FIGURE 2.
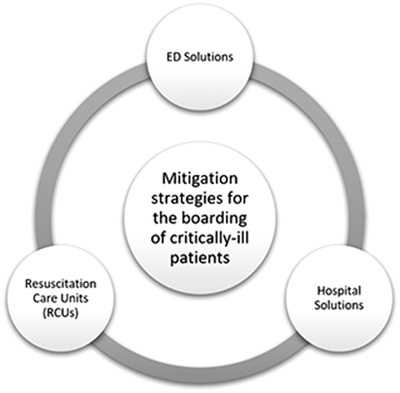
Subgroup delineation for potential mitigation strategies to combat resuscitation care unit (RCU) boarding. ED = emergency department
Many evidence‐based interventions are used in the ED to reduce morbidity and mortality among boarding critically ill patients. Targeted interventions to improve pain and agitation management, ventilator management, hemodynamic assessment, infection prevention, and targeted resource utilization can be applied to all critically ill patients regardless of patient disposition and physical location. Incorporating available recommendations and evidence‐based guidelines has been globally identified as a way to define essential care components and reduce patient harm. Although formal graded level of evidence evaluations were beyond the current scope of this Task Force, potential interventions for ED patients awaiting ICU admission were summarized (Supplemental Table 3, Supplemental Digital Content 1, http://links.lww.com/CCM/F477).
Hospital solutions encourage a system‐wide approach to boarding and managing critically ill patients in the ED. The majority of these solutions focus on attempting to control patient flow by matching demand with capacity. An early operational model of ED flow highlights the input, throughput, and disposition of a critically ill; however, the recognition of the causes of bottlenecks has evolved to recognize the interdependence of the operating room, ICU, hospital ward, and ED all competing for the same beds. 2 Most interventions work within a current system to increase the turnover of beds or to limit the dual‐claim from the operating room, floor, and ED for an ICU bed. Surge conditions occur when needed resources are outstripped by what is available, and harm can occur when staff are overwhelmed by competing demands on time and resources. 51
The ED, unlike other areas of the hospital, is an expandable space—patients are seen in hallways, waiting areas, and other non‐traditional patient care areas during periods of surge. Most solutions provide a “just‐in‐time” model responding to an excess volume situation only after it is recognized. The ability to predict inflow and trends in patient volume is currently drawn from historic population data and trends of daily ED patient census and arrival‐time data. Although historic trends help with global staffing, they do not allow for real‐time recognition of surge conditions, which prevents EDs from distinguishing between routine versus crisis conditions. Within the quality improvement literature, the method of statistical process control distinguishes between routine operational variation and crisis or special cause variation. 52 Succinctly, if a metric plotted over time falls outside of three standard deviations from the usual daily experience, it would identify that special cause variation, or a surge crisis condition, exists. Identifying meaningful metrics which predict ICU boarding requires additional research and testing across institutions; however, by identifying surge conditions accurately, real‐time metrics might trigger health system contingency plans. Some of the applicable disaster preparedness literature articulates the need for situational awareness to recognize that moving from “routine” to “crisis” conditions requires a contingent surge bundle of practices and policies. 53 The response is an adaptive strategy utilizing alternate sites and variations in daily practice and standards, such as reverse triage.
Active bed management can prevent surge conditions in multiple care locations simultaneously. Litvak et al. 54 reported on coordinating elective operating room scheduling for expected ICU admissions to fall on traditionally low ED census days as a mechanism to reduce ED boarding of ICU patients. Unfortunately, a higher ED “census day” is not predictive of more patients needing ICU care, limiting the effectiveness of this approach. In a similar approach, Howell et al. 55 studied the impact of an active bed management system controlled at the physician level (hospitalists) at a large academic medical center. These physicians were empowered to facilitate patient flow out of the ED to the medical ICU and coronary care unit. This change decreased ED length of stay by 98 minutes (458 vs 360 min, p < 0.001) for critically ill patients.
Some health systems have evaluated the utility of reserving ICU beds for emergencies, such as trauma, ST‐elevation myocardial infarction (STEMI), cardiac arrest, or acute stroke. Bhakta et al. 22 reported a 1‐hour decrease in ED length of stay for critically ill trauma patients at their level 1 trauma center with a reserved open trauma bed. An alternative approach is facilitating the timely movement of appropriate patients from the ICU to the hospital ward to create ICU bed availability. Mahmoudian‐Dehkordi et al. 56 evaluated a crisis surge process of prioritizing ICU patients awaiting ward transfer over ED ward admissions with the goal of opening ICU beds for critically ill ED admissions. Compared with other ICU bed management strategies tested in a crisis surge (“disaster”) model in a simulation, this strategy outperformed all others, resulting in 0.9 to 3.3 lives saved over the other scenarios (in a simulated U.S. hospital over a 3‐mo period).
Another proposed solution is to shift the location of the boarding. During surge conditions, critically ill patients are often admitted to another ICU within the same institution (e.g., surgical patients admitted to medical units), although this has not always improved outcomes 57 , 58 . Some have proposed boarding ED patients on hospital wards. 59 However, there is limited published data on this approach for critically ill patients.
Another strategy is to reassign ICU providers and nurses to provide care for boarding critically ill patients outside of the ICU. Elliott et al. 27 evaluated a medical ICU alert team (nurse and physician assistant) assigned to the ED to manage boarding critically ill medical admissions. Although the deployment of this team did not impact overall mortality, the authors report a 30% reduction in ED length of stay for these patients. The authors recognized the greatest benefit of this intervention was increased communication and interdepartmental collaboration between ED and ICU staff that helped them address potential admission barriers “in real time” and ultimately move patients to the ICU more quickly. Another model encourages intensivists to round in the ED and place orders on boarding patients, but in one study, no improvement in ED boarding time, organ dysfunction, or 28‐day in‐hospital mortality was observed. 18
Although most of these interventions work within the bed capacity of the hospital, methods of augmenting the bed capacity to meet the surge in demand also include expanding to alternate sites or changing care standards. Examples of surge‐space interventions include using routinely unused spaces to generate additional bed capacity (e.g. entryway, waiting room, parking lot for pop‐up medical facilities, office space) to create additional sites of care. “Discharge waiting rooms” for lower‐acuity patients awaiting imminent discharge (i.e. awaiting a final laboratory check or medication dose) can open up capacity quickly as well. 60 , 61 Other interventions can be system‐wide or regional. Some of the Task Force authors work within multihospital systems who have examined “reverse triage”: transferring lower acuity ICU patients to satellite ICUs in smaller facilities to avoid boarding in the ED.
2.6. How Do ED‐Based ICUs (RCUs) address ICU boarding?
Some centers have proposed adding resources to ED beds to address boarding or even building full critical care units within or adjacent to EDs to manage boarding patients (ED‐ICU). The term RCU was coined by Leibner et al to describe these ED‐ICU based models. 62 Although traditional ICUs are designed to focus on longitudinal critical care for a well‐defined cohort of patients, the RCU provides short‐term critical care that might replace more traditional ED boarding. Novel RCUs have sought to fill an unmet need for timely resuscitation, stabilization, and advanced triage of patients across many conditions requiring high intensity and time‐sensitive diagnostics and interventions. In general, these RCUs provide early respiratory, cardiovascular, neurologic, and hemodynamic support through the transition from the resuscitation in the ED to the early longitudinal phase of critical illness. This flexibility in delivering early care embodies the ultimate goal of providing critically ill patients appropriate care as soon as possible. 63
At the time of publication, several RCUs are in operation across the United States. Each is designed to meet the needs of the institutions in which they were developed. 62 These units differ in operations, patient flow, and staffing structure, but all focus on providing timely, high‐intensity, and specialized care to critically ill patients across a wide variety of diseases and introduce a degree of flexibility in early critical care that is uncommon in many tertiary ICUs (Table 1). Recent observational data from a single academic center associated opening of an RCU with a 15.4% reduction in risk‐adjusted 30‐day mortality among all ED patients, as well as significant reductions in hospital and 24‐hour mortality. ICU admissions from the ED fell by 12.9%, and short‐stay ICU admissions (ICU length of stay < 24 hr) were 37.1% lower. Time to ICU‐level care was reduced by 1.9 hours, and more patients received ICU‐level care within 6 hours (77.6% vs 58.3%). 64 Similar comparative data have not been published in other RCU models, but the role of the RCU will be clarified through more detailed studies in other practice settings.
TABLE 1.
Descriptive Characteristics of Some Existing Emergency Department–Based ICUs in the United States (Not Meant to Be All Inclusive)
| ED‐ICUs | Unit Size | Patient Care Model | Staffing Model |
|---|---|---|---|
| Massey EC3 (University of Michigan) | 5 resuscitation bays + 9 beds | Outpatients (ED), direct from ED, outside hospital (OSH) ED transfers | Physicians: All EM board‐certified, some dual EM‐CCM fellowship trained, CCM fellows nursing: CCRN and ED RNs undergo 8‐wk inpatient ICU orientation |
| CCRU (University of Maryland) | 6 beds | Outpatients (ED) and Inpatients (OSH ICU transfers, decompensating non‐ICU admitted patients, postoperative patients) | Physicians: All CCM fellowship trained (most EM) nursing: minimum 3 yr CCM experience |
| ResCCU (University of Pennsylvania) | 3 resuscitation bays + 2 beds | Outpatients (ED) and inpatients (ICU to ICU transfers as of 2018) | Physicians: All EM board‐certified, some dual EM‐CCM fellowship trained nursing: CCRN or ED RNs undergo extensive 8‐wk orientation |
| RACC (Stony Brook University) | 3 resuscitation bays + 3 beds (critical care acute area), additional 16 beds (high‐acuity area) | Outpatients (ED), direct from EMS, direct from ED, OSH ED transfers | All EM board‐certified, some dual EM‐CCM fellowship trained, resuscitation fellows |
CCM = critical care medicine, CCRN = specialty certification in critical care nursing, CCRU = Critical Care Resuscitation Unit, EC3 = Emergency Critical Care Center, ED = emergency department, EM = emergency medicine, EMS = emergency medical services, OSH = outside hospital, RACC = Resuscitation and Acute Critical Care Unit, ResCCU = Resuscitation and Critical Care Unit, RN = registered nurse.
Alternatively, some have proposed using surge pods for seasonal or system‐related variation in volume that could be applied to hospitals without a dedicated year‐round RCU, providing staffing and facilities in a “just‐in‐time” model. Ultimately, a multimodal approach will be required through a selection of ED‐based, hospital‐based, and hybrid critical care unit solutions that will optimize care delivery for boarding critically ill patients.
3. DISCUSSION AND RECOMMENDATIONS
The Task Force recognizes that ED‐CCM boarding is a pervasive local problem with national patient‐oriented implications. The specifics of the problem in each institution are embedded in institutional culture, with flow of information, prioritization of resources, and individual relationships significantly impacting feasible solutions. This local variability is what makes this problem difficult to address: estimates of frequency are difficult to pool because of asymmetric reporting from tertiary and academic centers, mitigation strategies are nuanced and incompletely evaluated, and the actual patient‐oriented effects for the system as a whole have been elusive. Nonetheless, understanding the common factors that lead to boarding and the principal ways to reduce its deleterious effects are worthy goals for all health system advocates, both within emergency medicine and within critical care.
The Task Force specifically concludes that the following:
No universally adopted definition for ED boarding of the critically ill patient exists to standardize research and mitigation strategy development.
Critical care services are provided, often for extended periods, in the ED setting by emergency physicians.
Boarding of the critically ill is prevalent in some large academic centers; it is often reported in isolation, and it is currently unclear how significant this issue is nationally in nonacademic EDs.
Boarding of the critically ill with prolonged ED stay is associated with worse patient outcomes.
Opportunities exist to improve, create, disseminate, and evaluate mitigation strategies to standardize care of the critically ill in the ED.
The Task Force specifically recommends the following next steps:
Adopt a formal definition for ED‐CCM boarding. The Task Force recommends that ED‐CCM boarding be defined as time spent in an ED (1) after the decision to admit to an ICU is made (existing ACEP boarding definition 34 ) or (2) after 6 hours in the ED (from ED arrival), whichever comes first. This recommendation is based on recognition that boarding applies to patients for whom inpatient resources have been requested but are unavailable, but also that patient outcomes are worse for critically ill patients after 6 hours of ED care even if no inpatient bed has been requested. This metric is not intended to penalize individual providers but rather to serve as a benchmark and tool for administrators and institutions to optimize resources and processes that limit the need for ED‐CCM boarding.
Report in future studies the time between the decision to admit a patient to an ICU and the time of transfer to an inpatient unit as one measure of boarding and health system strain.
Target research to address frequency of ED‐CCM boarding with a focus on unbiased estimates incorporating both academic and community settings. These research studies should also incorporate funding, reimbursement, staffing, and resource‐allocation factors in the reporting of outcomes for future comparative effectiveness research.
Continue ongoing multiprofessional collaboration to clarify the impact and mitigation strategies appropriate to address local critical care boarding in the ED (e.g., involving pharmacy, nursing, respiratory therapy, and other emergency medicine and critical care medicine professionals).
Supporting information
Supplementary information
ACKNOWLEDGMENTS
The authors would like to acknowledge Kathy Vermoch (Society of Critical Care Medicine) and Margaret Montgomery (American College of Emergency Physicians) for their administrative support of the Task Force, Heather Healy (Hardin Library for the Health Sciences, University of Iowa), and Barbara Shipman (Taubman Health Sciences Library, University of Michigan) for their assistance in literature review and Deb Roush (Department of Anesthesia, University of Iowa) for her technical assistance in preparation of this article.
Mohr NM, Wessman BT, Bassin B, et al. Boarding of critically Ill patients in the emergency department. JACEP Open. 2020;1:423–431. 10.1002/emp2.12107
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website (http://journals.lww.com/ccmjournal).
Emergency department–Critical Care Medicine Boarding Task Force was supported, in part, by the Society of Critical Care Medicine and the American College of Emergency Physicians.
Dr. Gunnerson disclosed that he is an Society of Critical Care Medicine council member. The remaining authors have disclosed that they do not have any potential conflicts of interest.
This article is being simultaneously co‐published in Critical Care Medicine (DOI: 10.1097/CCM.0000000000004385) and Journal of the American College of Emergency Physicians Open (DOI: 10.1002/emp2.12107).
Dr. Mohr and Dr. Wessman are co‐first authors for this work.
REFERENCES
- 1. Safar P. Critical care medicine—quo vadis? Crit Care Med. 1974;2:1–5. [DOI] [PubMed] [Google Scholar]
- 2. Asplin BR, Magid DJ, Rhodes KV, et al. A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42:173–180. [DOI] [PubMed] [Google Scholar]
- 3. Richardson DB. The access‐block effect: Relationship between delay to reaching an inpatient bed and inpatient length of stay. Med J Aust. 2002;177:492–495. [DOI] [PubMed] [Google Scholar]
- 4. Vicellio P, Schneider SM, Asplin B, et al. Emergency Department Crowding: High Impact Solutions. Dallas, TX: ACEP Task Force on Boarding, 2008. [Google Scholar]
- 5. Halpern NA, Pastores SM. Critical care medicine in the United States 2000‐2005: An analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38:65–71. [DOI] [PubMed] [Google Scholar]
- 6. McKenna P, Heslin SM, Viccellio P, et al. Emergency department and hospital crowding: Causes, consequences, and cures. Clin Exp Emerg Med. 2019;6:189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2015 Emergency Department Summary Tables, 2017. Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2015_ed_web_tables.pdf.
- 8. HCUP Nationwide Emergency Department Sample (NEDS) in Healthcare Cost and Utilization Project (HCUP). 2014.
- 9. American Hospital Association (AHA ): Annual Survey of Hospitals, Hospital Statistics: 1981, 1991, 1992, 2002, 2006, 2015, 2016, 2017 editions. Chicago, IL.
- 10. Doucet M, Rochette L, Hamel D. Incidence, prevalence, and mortality trends in chronic obstructive pulmonary disease over 2001 to 2011: A public health point of view of the burden. Can Respir J. 2016;2016:7518287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–1554. [DOI] [PubMed] [Google Scholar]
- 12. Rowley WR, Bezold C, Arikan Y, et al. Diabetes 2030: Insights from Yesterday, Today, and Future Trends. Popul Health Manag. 2017;20:6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wessman B, Griffey R. 1295: Cohort study of critical care medicine billing practices from The Ed At A Large Academic Center. Crit Care Med. 2015;43:325–326. [Google Scholar]
- 14. Easter BD, Fischer C, Fisher J. The use of mechanical ventilation in the ED. Am J Emerg Med. 2012;30:1183–1188. [DOI] [PubMed] [Google Scholar]
- 15. Rhee C, Dantes R, Epstein L, et al. CDC Prevention Epicenter Program: Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009‐2014. JAMA. 2017;318:1241–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Singer AJ, Thode HC, Jr , Viccellio P, et al. The association between length of emergency department boarding and mortality. Acad Emerg Med. 2011;18:1324–1329. [DOI] [PubMed] [Google Scholar]
- 17. Al‐Qahtani S, Alsultan A, Haddad S, et al. The association of duration of boarding in the emergency room and the outcome of patients admitted to the intensive care unit. BMC Emerg Med. 2017;17:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mathews KS, Durst MS, Vargas‐Torres C, et al. Effect of emergency department and ICU occupancy on admission decisions and outcomes for critically ill patients. Crit Care Med. 2018;46:720–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bhat R, Goyal M, Graf S, et al. Impact of post‐intubation interventions on mortality in patients boarding in the emergency department. West J Emerg Med. 2014;15:708–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reznek MA, Upatising B, Kennedy SJ, et al. Mortality associated with emergency department boarding exposure: Are there differences between patients admitted to ICU and Non‐ICU Settings? Med Care. 2018;56:436–440. [DOI] [PubMed] [Google Scholar]
- 21. Clark K, Normile LB. Patient flow in the emergency department: Is timeliness to events related to length of hospital stay? J Nurs Care Qual. 2007;22:85–91. [DOI] [PubMed] [Google Scholar]
- 22. Bhakta A, Bloom M, Warren H, et al. The impact of implementing a 24/7 open trauma bed protocol in the surgical intensive care unit on throughput and outcomes. J Trauma Acute Care Surg. 2013;75:97–101. [DOI] [PubMed] [Google Scholar]
- 23. McCoy JV, Gale AR, Sunderram J, et al. Reduced hospital duration of stay associated with revised emergency department‐intensive care unit admission policy: A before and after Study. J Emerg Med. 2015;49:893–900. [DOI] [PubMed] [Google Scholar]
- 24. Fuentes E, Shields JF, Chirumamilla N, et al. “One‐way‐street” streamlined admission of critically ill trauma patients reduces emergency department length of stay. Intern Emerg Med. 2017;12:1019–1024. [DOI] [PubMed] [Google Scholar]
- 25. Ko A, Harada MY, Dhillon NK, et al. Decreased transport time to the surgical intensive care unit. Int J Surg. 2017;42:54–57. [DOI] [PubMed] [Google Scholar]
- 26. Mathews KS, Long EF. A conceptual framework for improving critical care patient flow and bed use. Ann Am Thorac Soc. 2015;12:886–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Elliott DJ, Williams KD, Wu P, et al. An interdepartmental care model to expedite admission from the emergency department to the medical ICU. Jt Comm J Qual Patient Saf. 2015;41:542–549. [DOI] [PubMed] [Google Scholar]
- 28. McConnell KJ, Richards CF, Daya M, et al. Effect of increased ICU capacity on emergency department length of stay and ambulance diversion. Ann Emerg Med. 2005;45:471–478. [DOI] [PubMed] [Google Scholar]
- 29. Pitts SR, Vaughns FL, Gautreau MA, et al. A cross‐sectional study of emergency department boarding practices in the United States. Acad Emerg Med. 2014;21:497–503. [DOI] [PubMed] [Google Scholar]
- 30. Huynh TN, Kleerup EC, Raj PP, et al. The opportunity cost of futile treatment in the ICU*. Crit Care Med. 2014;42:1977–1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chalfin DB, Trzeciak S, Likourezos A, et al; DELAY‐ED study group: Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. [DOI] [PubMed] [Google Scholar]
- 32. Angotti LB, Richards JB, Fisher DF, et al. Duration of mechanical ventilation in the emergency department. West J Emerg Med. 2017;18:972–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Uhrenfeldt L, Aagaard H, Hall EO, et al. A qualitative meta‐synthesis of patients’ experiences of intra‐ and inter‐hospital transitions. J Adv Nurs. 2013;69:1678–1690. [DOI] [PubMed] [Google Scholar]
- 34. American College of Emergency Physicians (ACEP) . Definition of boarded patient. Policy statement. Ann Emerg Med. 2011;57:548. [DOI] [PubMed] [Google Scholar]
- 35. Rutherford PA, Provost LP, Kotagal UR, et al. Achieving Hospital‐wide Patient Flow. Cambridge, MA: Institute for Healthcare Improvement, 2017. [Google Scholar]
- 36. McHugh M, Dyke KV, McClelland M, et al. Improving Patient Flow and Reducing Emergency Department Crowding: A Guide for Hospitals. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ), 2018. [Google Scholar]
- 37. Barbe DO. Emergency Department Boarding and Crowding; 2009. Chicago, IL. Report No: CMS Report 3‐A‐09. [Google Scholar]
- 38. Rincon F, Mayer SA, Rivolta J, et al. Impact of delayed transfer of critically ill stroke patients from the emergency department to the neuro‐ICU. Neurocrit Care. 2010;13:75–81. [DOI] [PubMed] [Google Scholar]
- 39. Cardoso LT, Grion CM, Matsuo T, et al. Impact of delayed admission to intensive care units on mortality of critically ill patients: A cohort study. Crit Care. 2011;15:R28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sprivulis PC, Da Silva JA, Jacobs IG, et al. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184:208–212. [DOI] [PubMed] [Google Scholar]
- 41. Liu SW, Chang Y, Weissman JS, et al. An empirical assessment of boarding and quality of care: Delays in care among chest pain, pneumonia, and cellulitis patients. Acad Emerg Med. 2011;18:1339–1348. [DOI] [PubMed] [Google Scholar]
- 42. Sri‐On J, Chang Y, Curley DP, et al. Boarding is associated with higher rates of medication delays and adverse events but fewer laboratory‐related delays. Am J Emerg Med. 2014;32:1033–1036. [DOI] [PubMed] [Google Scholar]
- 43. Gaieski DF, Agarwal AK, Mikkelsen ME, et al. The impact of ED crowding on early interventions and mortality in patients with severe sepsis. Am J Emerg Med. 2017;35:953–960. [DOI] [PubMed] [Google Scholar]
- 44. Krochmal P, Riley TA. Increased health care costs associated with ED overcrowding. Am J Emerg Med. 1994;12:265–266. [DOI] [PubMed] [Google Scholar]
- 45. Liew D, Liew D, Kennedy MP. Emergency department length of stay independently predicts excess inpatient length of stay. Med J Aust. 2003;179:524–526. [DOI] [PubMed] [Google Scholar]
- 46. Pines JM, Pollack CV Jr, Diercks DB, et al. The association between emergency department crowding and adverse cardiovascular outcomes in patients with chest pain. Acad Emerg Med. 2009;16:617–625. [DOI] [PubMed] [Google Scholar]
- 47. Weissman JS, Rothschild JM, Bendavid E, et al. Hospital workload and adverse events. Med Care. 2007;45:448–455. [DOI] [PubMed] [Google Scholar]
- 48. Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006;184:213–216. [DOI] [PubMed] [Google Scholar]
- 49. Bornemann‐Shepherd M, Le‐Lazar J, Makic MB, et al. Caring for inpatient boarders in the emergency department: Improving safety and patient and staff satisfaction. J Emerg Nurs. 2015;41:23–29. [DOI] [PubMed] [Google Scholar]
- 50. Lu H, Barriball KL, Zhang X, et al. Job satisfaction among hospital nurses revisited: A systematic review. Int J Nurs Stud. 2012;49:1017–1038. [DOI] [PubMed] [Google Scholar]
- 51. Hick JL, Barbera JA, Kelen GD. Refining surge capacity: Conventional, contingency, and crisis capacity. Disaster Med Public Health Prep. 2009;3:S59–S67. [DOI] [PubMed] [Google Scholar]
- 52. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Howitt AM, Leonard HB. Managing Crises: Responses to Large‐Scale Emergencies. Washington, DC: CQ Press; 2009. [Google Scholar]
- 54. Managing Patient Flow . Smoothing OR schedule can ease capacity crunches, researchers say. OR Manager. 2003;19:9‐10. [PubMed] [Google Scholar]
- 55. Howell E, Bessman E, Marshall R, et al. Hospitalist bed management effecting throughput from the emergency department to the intensive care unit. J Crit Care. 2010;25:184–189. [DOI] [PubMed] [Google Scholar]
- 56. Mahmoudian‐Dehkordi A, Sadat S. Sustaining critical care: Using evidence‐based simulation to evaluate ICU management policies. Health Care Manag Sci. 2017;20:532–547. [DOI] [PubMed] [Google Scholar]
- 57. Pascual JL, Blank NW, Holena DN, et al. There's no place like home: Boarding surgical ICU patients in other ICUs and the effect of distances from the home unit. J Trauma Acute Care Surg. 2014;76:1096–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Stretch R, Della Penna N, Celi LA, et al. Effect of boarding on mortality in ICUs. Crit Care Med. 2018;46:525–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Boyle A, Viccellio P, Whale C. Is “boarding” appropriate to help reduce crowding in emergency departments? BMJ. 2015;350:h2249. [DOI] [PubMed] [Google Scholar]
- 60. Morton MJ, DeAugustinis ML, Velasquez CA, et al. Developments in surge research priorities: A systematic review of the literature following the Academic Emergency Medicine Consensus Conference, 2007‐2015. Acad Emerg Med. 2015;22:1235–1252. [DOI] [PubMed] [Google Scholar]
- 61. Kelen GD, McCarthy ML, Kraus CK, et al. Creation of surge capacity by early discharge of hospitalized patients at low risk for untoward events. Disaster Med Public Health Prep. 2009;3:S10–S16. [DOI] [PubMed] [Google Scholar]
- 62. Leibner E, Spiegel R, Hsu CH, et al. Anatomy of resuscitative care unit: Expanding the borders of traditional intensive care units. Emerg Med J. 2019;36:364–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Angood PB. Right Care, Right Now–you can make a difference. Crit Care Med. 2005;33:2729–2732. [DOI] [PubMed] [Google Scholar]
- 64. Gunnerson KJ, Bassin BS, Havey RA, et al. Association of an emergency department‐based intensive care unit with survival and inpatient intensive care unit admissions. JAMA Netw Open. 2019;2:e197584. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information


