Abstract
Objective
Even if performing rapid influenza diagnostic tests test will not change clinical decision making, we sometimes perform at triage to reduce length of stay in Japan. Whether performing rapid influenza diagnostic tests at triage may shorten emergency department (ED) length of stay (LOS) is remains unclear. We aimed to determine the utility of rapid influenza diagnostic tests at triage in shortening ED length of stay LOS.
Methods
We retrospectively reviewed medical records of patients discharged from our ED after receiving results from rapid influenza diagnostic tests during the influenza season from December, 2013 to March, 2019. Eligibility criteria were a walk‐in visit, age ≥15 years, triage performed, rapid influenza diagnostic test administered, and no admission. The triage group received rapid influenza diagnostic tests at triage. The after‐examination group received their tests only after examination by a doctor. The primary outcome was ED LOS after propensity score matching to adjust for several covariates.
Results
Of 2,768 eligible patients, 2,554 patients were enrolled in the triage group (n = 363) or after examination group (n = 2,191). There were 329 matched pairs after propensity score matching. Median ED LOS was significantly shorter in the triage group than in the after‐examination group after propensity score matching (81 min (interquartile range [IQR] 60 to 111) vs 106 min (IQR 80–142); median difference 24 min (95% confidence interval 17–30)).
Conclusions
Performing rapid influenza diagnostic tests at triage was associated with shorter ED LOS during the influenza season.
Keywords: crowding, emergency department, influenza, length of stay, point‐of‐care testing, propensity score, triage
1. INTRODUCTION
1.1. Background
Rapid influenza diagnostic tests are rarely necessary for seasonal influenza because diagnosis can usually be made based on symptoms. 1 This test is not often used in the diagnostic process, except in limited situations for patients at high risk for influenza complication. However, patients in Japan may seek rapid influenza diagnostic tests at the request of schools or companies despite the lack of medical necessity. Furthermore, the rapid influenza diagnostic tests have a low sensitivity at illness onset, and physicians sometimes recommend a repeat rapid influenza diagnostic test the following day according to the wishes of patients who need a more reliable diagnosis of influenza, even in patients who are not high risk. It is estimated from government statistics that at least 10 million individuals seek medical treatment for influenza every year in Japan. 2 Moreover, seasonal influenza appears to be 1 of the major causes of crowding in the emergency department. To use medical resources properly, physicians should explain and make consensus with patients about why the test is not necessary for diagnosis of influenza. However, patients sometimes refuse this information and visit other clinics or hospitals because of the request of schools or companies, which is a lost opportunity to educate patients. These patients will continue to seek medical service unless someone corrects the misunderstanding. Thus, in our hospital, we explain that we can diagnose as influenza without doing a rapid influenza diagnostic test first. We perform the test only when patients ask for it, even if it will not change clinical decision making. After the result is available, we try to educate patients again at discharge.
The Infectious Diseases Society of America published guidelines in 2018 recommending that clinicians consider rapid influenza diagnostic tests to shorten the ED length of stay and avoid further testing or unnecessary antibiotics in patients without strong risk factors for influenza‐related complications, who are likely to be discharged home. 1
1.2. Importance
Although some evidence suggests that performing rapid influenza diagnostic tests in the ED shortens length of stay, 3 , 4 , 5 , 6 , 7 1 report found that rapid influenza diagnostic tests did not significantly shorten ED length of stay. 8 Furthermore, it has been reported that radiography, electrocardiography, and laboratory investigations performed at triage do shorten ED length of stay. 9 , 10 , 11 , 12 , 13 , 14 , 15 To our knowledge, no reports have shown that performing rapid influenza diagnostic tests at triage shortens ED length of stay.
1.3. Goals of this investigation
We hypothesized that performing rapid influenza diagnostic tests at triage would be effective in shortening ED length of stay if performed during the ED stay and conducted this study to confirm this hypothesis.
The Bottom Line
Rapid influenza testing started early in triage could impact flow of patients through the emergency department during the winter season. Looking at historic controls, this study showed that an automatic testing protocol at triage was associated with reduced median length of stay for suspected influenza patients from 106 minutes down to 81 minutes.
2. METHODS
2.1. Study design and setting
We retrospectively reviewed the medical records of patients who presented to the ED at St. Luke's International Hospital, Tokyo, Japan, during the influenza season between December 1, 2013 and March 31, 2019 and received a rapid influenza diagnostic test. The ED volume is ∼45,000 visits per year. The study protocol was approved by the local ethics committee of St. Luke's International Hospital (approval number 19‐R017). The need for informed consent was waived.
2.2. Selection of study participants
Patients were enrolled in the study if they met the following eligibility criteria: a walk‐in visit, age 15 years or older, triage received, rapid influenza diagnostic test performed, and no admission. The exclusion criteria were: no record of arrival time, triage, no rapid influenza diagnostic test order or results, no discharge time, missing data for vital signs (temperature, pulse rate, and blood pressure), no information on the Japan Triage and Acuity Scale score (developed from the Canadian Triage and Acuity Scale with some modifications for the local context and widely used in Japan 16 ), and triage performed more than 1 hour after arrival, which showed errors in input of triage time. Patients who remained in the ED for more than 6 hours were also excluded. These extremely long ED length of stay times were mainly caused by early registration before arrival or an accounting delay. In such cases, the apparent ED length of stay was longer because we defined ED length of stay to include the interval between registration time and completion of payment.
2.3. Triage
We triaged patients only during busy periods; that is, 08:00–24:00 on weekends or holidays and 16:00–24:00 on weekdays. Patients were classified as 1 to 5 according to the Japan Triage and Acuity Scale, 16 where 1 means “needs resuscitation” and 5 indicates that the case is “not urgent.” Before November 30, 2016, triage nurses suggested to the doctor in charge that rapid influenza diagnostic tests be performed at triage for patients who had symptoms of influenza, but only performed the tests themselves when the ED was busy. Since December 1, 2016, we revised the triage protocol and have performed rapid influenza diagnostic tests at triage in patients with symptoms of influenza at the discretion of the triage nurses who have authorization to approve the rapid influenza diagnostic test order as necessary. The triage nurses are also authorized to distribute a fact sheet that explains why a rapid influenza diagnostic test is not needed for diagnosis of seasonal influenza for all applicable patients. A rapid influenza diagnostic test is only performed thereafter for patients who request it. Rapid influenza diagnostic tests ordered by nurses according to the triage protocol were all performed at triage, whereas tests ordered by doctors were performed after doctor examinations.
2.4. Rapid influenza diagnostic tests
In this study, the only rapid influenza diagnostic test that was used was the Prorast Flu One (LSI Medience Co., Tokyo, Japan), which can detect influenza A and B viral antigen from a nasopharyngeal swab within 5 minutes. 17 All nasopharyngeal swabs were taken by a doctor or nurse and sent to the laboratory. All Prorast Flu One tests were performed and checked by laboratory technicians. Rapid influenza diagnostic tests, including Prorast Flu One, are approved for diagnosis of influenza in Japan and at the time of this study cost 2,870 yen per test under the national health insurance system, which pays at least 70% of the medical cost.
2.5. Definitions used
We used the following definitions: ED length of stay, interval between arrival time (time of registration on the ED index) and time of finishing payment at discharge (Figure 1); order time, time of rapid influenza diagnostic test order recorded on the patient's medical record; result time, time when the results of the rapid influenza diagnostic test were recorded on the patient's medical record; and triage time, time recorded on the triage chart.
FIGURE 1.
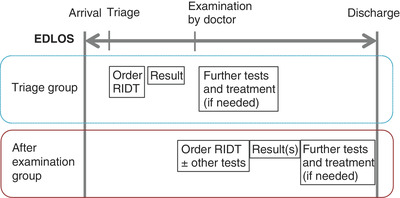
Patient flow through the emergency department. RIDT, rapid influenza diagnostic test
2.6. Measurements
For each patient, we recorded the following parameters: age and sex; whether the presentation was on a work day or on a day off; hour, month, and year of presentation; whether or not the patient was in residential care; past medical history of influenza‐related complications 18 ; use of steroids; clinical symptoms (fever, chills, fatigue, cough, nasal discharge, throat pain, joint pain, headache, sputum production, and muscle pain); vital signs (temperature, pulse rate, mean blood pressure); Japan Triage and Acuity Scale score; rapid influenza diagnostic test result; time of presentation; discharge time; rapid influenza diagnostic test order and result time; triage time; other examinations (chest radiography, blood investigations, blood culture, and urine test); medication (any parenteral medication, parenteral antibiotics, prescription for antibiotics, parenteral anti‐influenza medication, prescription for an anti‐influenza agent); and bounce‐back admission within 7 days. All necessary data was exported to spreadsheet from electronic charts. The author search keyword and coded about clinical symptoms, past medical history, regular medicine, and whether or not the patient was in residential care.
2.7. Outcomes
The primary outcome was ED length of stay. Secondary outcomes were the implementation of examinations other than rapid influenza diagnostic tests (radiographs, blood tests, blood culture, urine tests, urine culture, and cerebrospinal fluid analysis), medication (any parenteral medications, antibiotics, or anti‐influenza medications), bounce‐back admission within 7 days, and charges.
2.8. Data analysis
Patients who received a rapid influenza diagnostic test at triage were assigned to a triage group and those who only received the test after examination by a doctor were assigned to an after‐examination group as a control group. Baseline characteristics were compared between the 2 groups using the Wilcoxon test for continuous variables (presented as the mean and SD) and Fisher's exact test for binary and categorical variables (presented as a percentage). Primary and secondary outcomes were evaluated after propensity score (PS) matching for age, sex, risk factors for influenza‐related complications, whether or not the presentation was during a work day or on a day off, hour, month, and year of arrival, Japan Triage and Acuity Scale score, and time from arrival to triage. We performed 1:1 nearest‐neighbor matching on the propensity score with a caliper of ≤0.2. To compare the timing of ED discharge, we plotted Kaplan‐Meier curves and compared the ED length of stay rate between the triage and after examination groups using the log‐rank test.
All tests were 2‐tailed and P‐values <0.05 were considered statistically significant. The data were entered into a spreadsheet (Microsoft Excel for Mac 201, version 14.7.0). All statistical analyses were performed with EZR 19 (version 1.40; Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R 20 (version 3.6.0 R; Foundation for Statistical Computing, Vienna, Austria). More precisely, EZR is a modified version of R commander (version 2.5‐3) that is designed to add statistical functions frequently used in biostatistics.
3. RESULTS
We excluded 214 of the 2,768 eligible patients because of missing time records (n = 84), staying for more than 6 hours on the ED register and accounting system (n = 80, all in the after examination group), no temperature, blood pressure, or pulse rate recordings (n = 29), no record of Japan Triage and Acuity Scale score (n = 20), or arrival at 04:00, which was >1 hour away from the normal triage time (n = 1). The remaining 2,554 patients were enrolled in the study (triage group, n = 363; after examination group, n = 2,191; Figure 2).
FIGURE 2.
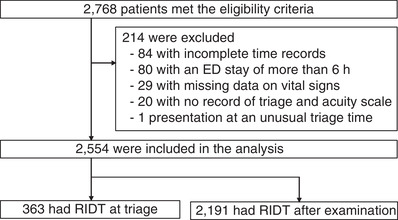
Patient selection process. ED, emergency department; RIDT, rapid influenza diagnostic test
3.1. Characteristics of study subjects
The triage group was smaller at the start of the influenza epidemic season because the protocol of performing rapid influenza diagnostic tests at triage was only implemented after confirmation of the start of the epidemic. However, patients in the triage group were more likely to arrive on a public holiday and therefore at a time of crowding in the ED (Supporting Information Appendix S1). There were statistically significant differences in age, sex, risk factors for influenza‐related complications, some symptoms (fever, nasal discharge, joint pain, and sputum production), temperature, and Japan Triage and Acuity Scale score. More rapid influenza diagnostic test results were positive and the time to arrival in triage was longer in the triage group. Overall, 35.9% of the 2,768 patients were at high risk of influenza‐related complications (Table 1). There were no differences in risk factors except that there were fewer patients younger than 65 years of age and fewer with diabetes in the triage group (Supporting Information Appendix S2).
TABLE 1.
Baseline characteristics
| Before PS matching | After PS matching | |||||
|---|---|---|---|---|---|---|
| Triage group (n = 363) | After examination group (n = 2191) | Standardized difference (%) | Triage group (n = 329) | After examination group (n = 329) | Standardized difference (%) | |
| Age (y), mean (SD) | 40.5 ± 15.0 | 43.3 ± 17.5 | 0.175 | 40.8 ± 15.1 | 41.3 ± 16.7 | 0.033 |
| Sex (male) | 200 (55.1%) | 1,016 (46.4%) | 0.175 | 173 (52.6%) | 172 (52.3%) | 0.006 |
| Risk factors for influenza‐related complications | 98 (27.0%) | 819 (37.4%) | 0.224 | 96 (29.2%) | 95 (28.9%) | 0.007 |
| Any of the following symptoms: | 363 (100%) | 2,169 (99.0%) | 0.142 | 329 (100%) | 329 (100%) | NA |
| Fever | 350 (96.4%) | 2,009 (91.7%) | 0.201 | 316 ( (96.0%) | 319 (97.0%) | 0.050 |
| Chill | 129 (35.5%) | 846 (38.6%) | 0.064 | 119 (36.2%) | 119 (36.2%) | 0 |
| Fatigue | 77 (21.2%) | 397 (18.1%) | 0.078 | 68 (20.7%) | 67 (20.4%) | 0.008 |
| Cough | 236 (65.0%) | 1,528 (69.7%) | 0.101 | 214 (65.0%) | 225 (68.4%) | 0.071 |
| Nasal discharge | 163 (44.9%) | 1,119 (51.1%) | 0.124 | 152 (46.2%) | 157 (47.7%) | 0.030 |
| Throat pain | 220 (60.6%) | 1,354 (61.8%) | 0.024 | 202 (61.4%) | 208 (63.2%) | 0.038 |
| Joint pain | 160 (44.1%) | 1,094 (49.9%) | 0.118 | 143 (43.5%) | 135 (41.0%) | 0.049 |
| Headache | 133 (36.6%) | 1,000 (45.6%) | 0.184 | 127 (38.6%) | 127 (38.6%) | 0 |
| Sputum production | 84 (23.1%) | 697 (31.8%) | 0.195 | 80 (24.3%) | 85 (25.8%) | 0.035 |
| Muscle pain | 48 (13.2%) | 282 (12.9%) | 0.010 | 44 (13.4%) | 34 (10.3%) | 0.094 |
| Vital signs | ||||||
| Temperature (°C), mean (SD) | 38.2 ± 0.8 | 38.1 ± 0.9 | 0.115 | 38.2 ± 0.8 | 38.1 ± 0.9 | 0.076 |
| Pulse rate (bpm), mean (SD) | 101.3 ± 15.3 | 100.1 ± 16.5 | 0.073 | 101.2 ± 15.5 | 100.2 ± 15.5 | 0.068 |
| MAP (mm Hg), mean (SD) | 91.3 ± 14.2 | 92.3 ± 15.1 | 0.068 | 90.9 ± 14.4 | 91.4 ± 14.7 | 0.032 |
| JTAS score | 0.255 | 0.040 | ||||
| 1 | 0 | 0 | 0 | 0 | ||
| 2 | 5 (1.4%) | 72 (3.3%) | 5 (1.5%) | 4 (1.2%) | ||
| 3 | 94 ( (25.9%) | 773 (35.3%) | 88 (26.7%) | 84 (25.5%) | ||
| 4 | 261 (71.9%) | 1,327 (60.6%) | 234 (71.1%) | 239 (72.6%) | ||
| 5 | 3 (0.8%) | 19 (0.9%) | 2 (0.6%) | 2 (0.6%) | ||
| Positive RIDT (A or B) | 187 (51.5%) | 756 (34.5%) | 0.349 | 162 (49.2%) | 160 (48.6%) | 0.012 |
| Arrival‐to‐triage time (min), median (IQR) | 19 (12–32) | 14 (9–22) | 0.394 | 18 (12–28) | 17 (10–29) | 0.003 |
MAP, systolic pressure + 2 × diastolic pressure)/3. Arrival‐to‐triage time, from the time the patient was registered to the ED index to the triage time recorded on the triage template. Risk factors for influenza‐related complications are described in detail in the Supporting Information Appendix S2.
ED, emergency department; IQR, interquartile range; JTAS, Japan Triage and Acuity Scale; MAP, mean arterial pressure; PS, propensity score; RIDT, rapid influenza diagnostic test.
3.2. After propensity score matching
There were 329 matched pairs after propensity score matching. The baseline characteristics were well balanced between the 2 groups (Table 1; Supporting Information Appendices S1 and S2).
3.3. Outcomes
Median ED length of stay was significantly shorter in the triage group than in the after‐examination group after propensity score matching (81 minutes [interquartile range (IQR) = 60–111) versus 106 minutes [IQR = 80–142); median difference 24 minutes [95% confidence interval (CI) = 17–30]). Median time from arrival to ordering the rapid influenza diagnostic test was significantly shorter in the triage group (23 minutes [IQR = 14–34] versus 52 minutes [IQR = 33–74]; median difference 26 minutes [95% CI = 22–30]). In contrast, median time from availability of the rapid influenza diagnostic test result to discharge was longer in the triage group (32 minutes [IQR = 20–56] versus 28 minutes [IQR = 17–46]); median difference −4 minutes [95% CI = −7 to −1]; Table 2).
TABLE 2.
Emergency department length of stay
| Before PS matching | After PS matching | |||||
|---|---|---|---|---|---|---|
| Triage group (n = 363) | After examination group (n = 2191) | Median difference (95% CI) | Triage (n = 329) | After examination group (n = 329) | Median difference (95% CI) | |
| ED length of stay (min), median (IQR) | 83 (61–114) | 100 (76–137) | 16 (12–21) | 81 (60–111) | 106 (80–142) | 24 (17–30) |
| Arrival‐to‐order time (min), median (IQR) | 25 (15–35) | 45 (31–64) | 20 (18–22) | 23 (14–34) | 52 (33–74) | 26 (22–30) |
| Order‐to‐result time (min), median (IQR) | 18 (15–24) | 18 (15–24) | 0 (−1–0) | 18 (15–23) | 18 (14–23) | 0 (−1–0) |
| Result‐to‐discharge time (min), median (IQR) | 32 (20–56) | 26 (17–47) | −5 (−7 to −2) | 32 (20–56) | 28 (17–46) | −4 (−7 to −1) |
Arrival‐to‐order time, from the time patients was registered to ED index to the time RIDT was ordered at medical chart. Order‐to‐result time, from the time RIDT was ordered on the medical chart to the time the RIDT result was recorded on the medical chart. Result‐to‐discharge time, from the time the RIDT result was recorded on the medical chart to the time patient had completed payment.
CI, confidence interval; IQR, interquartile range; PS, propensity score; RIDT, rapid influenza diagnostic test.
Kaplan‐Meier curves for the 2 groups are shown in Figure 3. The probability of ED length of stay was significantly higher in the triage group than in the after‐examination group (P < 0.001, log‐rank test).
FIGURE 3.
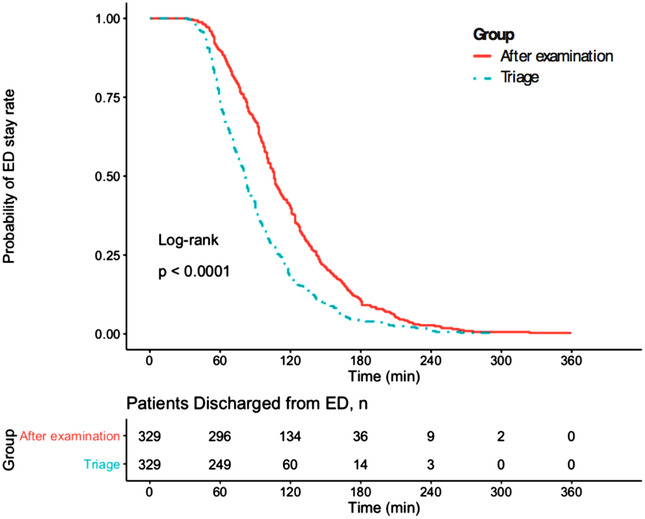
Kaplan‐Meier curves for time spent in the emergency department.*P < 0.05 was considered statistically significant. ED, emergency department
Fewer patients in the triage group received additional tests (7.6% versus 22.2%; odds ratio [OR] = 0.29 (95% CI = 0.17–0.48]) and the median associated charges were lower in this group (14,300 yen [IQR = 11,900–17,200] versus 15,000 yen [IQR = 12,400–18,500]; median difference 10,700 yen [95% CI = 2600–18,500]). There was no statistically significant difference in the number of patients who were prescribed antibiotic or anti‐influenza medication or in the bounce‐back admission rate between the 2 groups (Table 3).
TABLE 3.
Secondary outcomes
| Before PS matching | After PS matching | |||||
|---|---|---|---|---|---|---|
| Triage group (n = 363) | After examination group (n = 2191) | Odds ratio (95% CI) | Triage group (n = 329) | After examination group (n = 329) | Odds ratio (95% CI) | |
| Further test | 25 (6.9%) | 529 (24.1%) | 0.23 (0.15–0.35) | 25 (7.6%) | 73 (22.2%) | 0.29 (0.17–0.48) |
| Chest radiograph | 16 (4.4%) | 317 (14.5%) | 0.27 (0.15–0.46) | 16 (4.9%) | 40 (12.2%) | 0.37 (0.19–0.69) |
| Computed tomography of chest | 0 | 23 (1.0%) | 0 (0–1.04) | 0 | 3 (0.9%) | 0 (0–2.42) |
| Blood test | 16 (4.4%) | 336 (15.3%) | 0.25 (0.14–0.43) | 16 (4.9%) | 44 (13.4%) | 0.33 (0.17–0.62) |
| Blood culture | 12 (3.3%) | 155 (7.1%) | 0.45 (0.22–0.82) | 12 (3.6%) | 14 (4.3%) | 0.85 (0.35–2.02) |
| Urine test | 7 (1.9%) | 151 (6.9%) | 0.27 (0.10–0.57) | 7 (2.1%) | 14 (4.3%) | 0.49 (0.16–1.31) |
| Urine culture | 0 | 7 (0.3%) | 0 (0–4.19) | 0 | 0 | NA |
| Cerebrospinal fluid analysis | 0 | 0 | NA | 0 | 0 | NA |
| Any parenteral medications | 17 (4.7%) | 272 (12.4%) | 0.34 (0.20–0.57) | 16 (4.9%) | 38 (11.6%) | 0.39 (0.20–0.74) |
| Parenteral antibiotics | 2 (0.6%) | 50 (2.3%) | 0.23 (0.03–0.91) | 2 (0.6%) | 2 (0.6%) | 1 (0.07–13.90) |
| Any prescription | 136 (37.5%) | 951 (43.4%) | 0.78 (0.62–0.99) | 129 (39.2%) | 137 (41.6%) | 0.90 (0.65–1.25) |
| Antibiotic prescription | 17 (4.7%) | 203 (9.3%) | 0.48 (0.27–0.80) | 16 (4.9%) | 25 (7.6%) | 0.62 (0.30–1.24) |
| Any anti‐influenza medications | 44 (12.1%) | 216 (9.9%) | 1.26 (0.87–1.79) | 42 (12.8%) | 38 (11.6%) | 1.12 (0.68–1.84) |
| Bounce‐back admission within 3 days | 0 | 28 (1.3%) | 0 (0–0.84) | 0 | 2 (0.6%) | 0 (0–5.32) |
| Bounce‐back admission within 7 days | 0 (16.3%) | 42 (1.9%) | 0 (0–0.55) | 0 | 3 (0.9%) | 0 (0–2.42) |
|
Median Difference (95% CI) |
Median Difference (95% CI) |
|||||
| Cost (yen, thousand), median (IQR) | 14.3 (12.1–17.2) | 14.6 (11.5–18.7) | 6.4 (0.50–12.70) | 14.3 (11.9–17.2) | 15.0 (12.4–18.5) | 10.7 (2.60–18.50) |
CI, confidence interval; IQR, interquartile range; NA, not applicable; PS, propensity score.
4. LIMITATIONS
This study has some limitations, which stem mainly from its retrospective design and confounding by unobservables. In particular, the population was not the entirety of patients with influenza‐like symptoms, but only patients receiving a rapid flu test. In addition, the reason for performing rapid influenza diagnostic tests in the triage group was only due to wishes of patients, whereas in the after examination group was due to both wishes of patients and decision of physicians. This could affect the population difference because the need for payment for services at the time of discharge makes patients alter their choices. This could lead to false conclusions for other populations. Importantly, we could not ascertain the effect of rapid influenza diagnostic tests at triage in patients at high risk of influenza‐related complications. More research is needed to address these issues.
In addition, we should include variables related to crowding in the ED in the PS model, which was usually how many in the waiting room, how many arrivals in the previous 4 hours or how many patients boarding at the time of patient arrival. However, these variables were unlikely to be indicators of ED crowding in Japan because patients waited in waiting area after doctor examination, not in examination room until testing results were available. Crowding would be unlikely to affect work up or withholding of necessary testing. Instead of these variables, we used time from arrival to triage and date characteristics.
The single‐center design may have affected the generalizability of these findings.
5. DISCUSSION
Our findings suggest that performing the rapid influenza diagnostic tests at triage can shorten stayed length of stay during the influenza season with no effect on the bounce‐back admission rate. Such early strategic testing with decreased length of stay could also decrease the need for additional tests and the associated costs.
Previous studies have found that focused diagnostic tests, such as chest radiography, urine testing, and electrocardiography, at triage shorten ED length of stay. 9 , 10 , 11 , 12 , 13 , 14 , 15 Moreover, a drive‐through influenza examination model and a dedicated influenza clinic were also reported to shorten ED length of stay. 4 , 21 Performing rapid influenza diagnostic tests likely has a similar effect on ED length of stay.
After propensity score matching, the between‐group time difference was ∼25 minutes. This time is almost the same as the rapid influenza diagnostic test examination time, which also includes part of the waiting time before examination by a doctor, as shown by our results that the rapid influenza diagnostic test examination time mainly seemed to shorten ED length of stay.
Even though fewer additional tests were performed in the triage group, the time from availability of the rapid influenza diagnostic test results to discharge was longer in this group than in the after‐examination group. This finding indicates that the waiting time after obtaining the rapid influenza diagnostic test result is longer in the triage group. It seems that the medical interview and physical examination would be completed before the rapid influenza diagnostic test and that the doctor could explain the result immediately in the after‐examination group; however, this was not possible in the triage group. Conversely, if the patient did not to have wait for examination by a doctor for a long time, performing rapid influenza diagnostic test at triage would lengthen ED length of stay.
Whether performing a rapid influenza diagnostic test at triage is a useful way of addressing ED crowding is unclear, although it certainly may reduce ED length of stay. It may also reduce additional testing. If it is an effective approach to improve crowding and reduce additional tests, performing a rapid influenza diagnostic test at triage could streamline clinical practice. However, we performed rapid influenza diagnostic tests in more than half of our patients who were not at high risk of influenza‐related complications during the study period, and we were not sure whether the prescription of anti‐flu medications increased. Thus, we were not able to recommend performing rapid influenza diagnostic testing routinely for all patients, particularly in the influenza season, because testing results did not change clinical management in most cases. From an economic point of view, we should avoid rapid influenza diagnostic tests unless necessary. However, even when we explain that there was no need for rapid influenza diagnostic tests during the influenza season, many patients still request the test. This is possibly due to a need to confirm the illness with an employer or because educational institutions in Japan require a rapid influenza diagnostic test to exclude influenza before children can attend school. Before performing rapid influenza diagnostic tests routinely to shorten ED length of stay, we should educate patients and society at large that there is no need for rapid influenza diagnostic tests during the influenza season. Like several other hospitals in Japan, we are now attempting to address this problem by providing patients with written discharge instructions in addition to a fact sheet at triage. However, the effects of this strategy are thus far limited. For now, the best plan may be to tackle the problem at a national policy level to avoid unnecessary flu testing. After that, we can confirm the real effect of performing rapid influenza diagnostic tests at triage, particularly for patients at high risk of influenza‐related complications or to alleviate ED overcrowding. Although different at present, there is a possibility the rapid influenza diagnostic test would be useful within limited indication. In summary, performing rapid influenza diagnostic tests at triage is associated with shorter ED length of stay during the influenza season, but more research is needed to determine the impact of rapid influenza diagnostic tests at triage in high‐risk patients.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
TI conceived the study, designed the trial, collected the data, and drafted the manuscript. TH and KH provided statistical advice on the study design and analyzed the data. All authors contributed substantially to the revision of the manuscript. TI takes responsibility for the paper as a whole.
Supporting information
SUPPORTING INFORMATION
Biography
Tsutomu Iwasaki, MD, is a staff physician in the emergency medical care center at St. Luke's International Hospital, Tokyo, Japan.

Iwasaki T, Hifumi T, Hayashi K, Otani N, Ishimatsu S. Rapid influenza diagnostic test at triage can decrease emergency department length of stay. JACEP Open. 2020;1:494–501. 10.1002/emp2.12125
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
This study was presented at the 46th Annual Meeting of the Japanese Association for Acute Medicine, held at PACIFICO Yokohama, Yokohama, Japan, on November 19–21, 2018
Supervising Editor: Christian A. Tomaszewski, MD, MS.
REFERENCES
- 1. Uyeki TM, Bernstein HH, Bradley JS, et al. Clinical practice guidelines by the Infectious Diseases Society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenza. Clin Infect Dis. 2019;68(6):e1‐e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ministry of Health, Labour and Welfare.Influenza (general page) [in Japanese]. Tokyo, Japan: Ministry of Health, Labour and Welfare; https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/kenkou/kekkaku-kansenshou/infulenza/index.html. Accessed December 5, 2019. [Google Scholar]
- 3. Bonner AB, Monroe KW, Talley LI, et al. Impact of the rapid diagnosis of influenza on physician decision‐making and patient management in the pediatric emergency department: results of a randomized, prospective, controlled trial. Pediatrics. 2003;112(2):363‐367. [DOI] [PubMed] [Google Scholar]
- 4. Weiss EA, Ngo J, Gilbert GH, et al. Drive‐through medicine: a novel proposal for rapid evaluation of patients during an influenza pandemic. Ann Emerg Med. 2010;55(3):268‐273. [DOI] [PubMed] [Google Scholar]
- 5. Jeong HW, Heo JY, Park JS, et al. Effect of the influenza virus rapid antigen test on a physician's decision to prescribe antibiotics and on patient length of stay in the emergency department. PLoS One. 2014;9(11):e110978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Trabattoni E, Le V, Pilmis B, et al. Implementation of Alere i Influenza A & B point of care test for the diagnosis of influenza in an ED. Am J Emerg Med. 2018;36(6):916‐921. [DOI] [PubMed] [Google Scholar]
- 7. Diallo D, Hochart A, Lagree M, et al. Impact of the Sofia® Influenza A+B FIA rapid diagnostic test in a pediatric emergency department. Arch Pediatr. 2019;26(1):6‐11. [DOI] [PubMed] [Google Scholar]
- 8. Schechter‐Perkins EM, Mitchell PM, Nelson KP, et al. Point‐of‐care influenza testing does not significantly shorten time to disposition among patients with an influenza‐like illness. Am J Emerg Med. 2019;37(5):873‐878. [DOI] [PubMed] [Google Scholar]
- 9. Jang JY, Shin SD, Lee EJ, et al. Use of a comprehensive metabolic panel point‐of‐care test to reduce length of stay in the emergency department: a randomized controlled trial. Ann Emerg Med. 2013;61(2):145‐151. [DOI] [PubMed] [Google Scholar]
- 10. Cooper JJ, Datner EM, Pines JM. Effect of an automated chest radiograph at triage protocol on time to antibiotics in patients admitted with pneumonia. Am J Emerg Med. 2008;26(3):264‐269. [DOI] [PubMed] [Google Scholar]
- 11. Takakuwa KM, Burek GA, Estepa AT, et al. A method for improving arrival‐to‐electrocardiogram time in emergency department chest pain patients and the effect on door‐to‐balloon time for ST‐segment elevation myocardial infarction. Acad Emerg Med. 2009;16(10):921‐927. [DOI] [PubMed] [Google Scholar]
- 12. Ho JK, Chau JP, Chan JT, et al. Nurse‐initiated radiographic‐test protocol for ankle injuries: a randomized controlled trial. Int Emerg Nurs. 2018;41:1‐6. [DOI] [PubMed] [Google Scholar]
- 13. Lee WW, Filiatrault L, Abu‐Laban RB, et al. Effect of triage nurse initiated radiography using the Ottawa Ankle Rules on emergency department length of stay at a tertiary centre. CJEM. 2016;18(2):90‐97. [DOI] [PubMed] [Google Scholar]
- 14. Li Y, Lu Q, Du H, et al. The impact of triage nurse‐ordered diagnostic studies on pediatric emergency department length of stay. Indian J Pediatr. 2018;85(19):849‐854. [DOI] [PubMed] [Google Scholar]
- 15. Singer AJ, Taylor M, LeBlanc D, et al. Early point‐of‐care testing at triage reduces care time in stable adult emergency department patients. J Emerg Med. 2018;55(2):172‐178. [DOI] [PubMed] [Google Scholar]
- 16. Japanese Association for Acute Medicine, Japanese Association for Emergency Nursing, Japanese Society of Emergency Pediatrics, Japanese Society for Emergency Medicine Urgent Degree Judgment Support System, JTAS, Japan Triage and Acuity Scale, 2017 Guidebook [in Japanese]. Tokyo, Japan: Health Publishing Inc; 2017. [Google Scholar]
- 17. LSI Medience Corporation, Tokyo, J. Prorast Flu One. [in Japanese] https://www.medience.co.jp/h1_prorast/ Accessed December 5, 2019.
- 18. Centers for Disease Control and Prevention. Seasonal influenza (flu). People at high risk for flu complication. https://www.cdc.gov/flu/highrisk/index.htm. Accessed December 5, 2019.
- 19. Kanda Y. Investigation of the freely available easy‐to‐use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452‐458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. R Core Team .R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. https://www.R-project.org/. Accessed April 26, 2019. [Google Scholar]
- 21. Shih HI, Ho TS, Chang CM, et al. Impacts of rapid flu clinic services at an emergency department during the pandemic flu season. Am J Infect Control. 2012;40(2):165‐169. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SUPPORTING INFORMATION


