Abstract
Background
The national incidence and characteristics of out‐of‐hospital cardiac arrest in the United States is unclear. We sought to describe the national characteristics of adult out‐of‐hospital cardiac arrest reported in the National Emergency Medical Services Information System (NEMSIS).
Methods
We used 2016 NEMSIS data, consisting of most emergency medical services (EMS) responses from 46 states and territories. We limited the analysis to adult (age ≥18 years) emergency “9‐1‐1” events. We defined out‐of‐hospital cardiac arrest as: (1) patient condition reported as cardiac arrest, (2) EMS reported attempted resuscitation of cardiac arrest, (3) EMS performance of cardiopulmonary resuscitation (CPR), or (4) EMS performance of defibrillation. We determined the incidence of adult out‐of‐hospital cardiac arrest among EMS responses. We also determined patient demographics (age, sex, race, ethnicity, location, US census region, and urbanicity), response characteristics (dispatch complaint and elapsed time) and clinical interventions (medications and procedures) of adult out‐of‐hospital cardiac arrest. We analyzed the data using descriptive techniques, calculating binomial proportions with exact 95% confidence intervals (CI).
Results
Among 18,679,873 adult 9‐1‐1 responses, there were 224,992 with patient condition cardiac arrest, 344,274 with EMS‐reported attempted cardiac arrest resuscitation, 149,775 with EMS performance of CPR, and 185,388 cases with EMS performance of defibrillation, resulting in a total of 574,824 out‐of‐hospital cardiac arrest (incidence 30.8 per 1000 EMS 9‐1‐1 responses, 95% CI = 30.69–30.85). Among identified out‐of‐hospital cardiac arrest responses, most involved patients who were older (mean = 62.4 ± 20.1 years). Most out‐of‐hospital cardiac arrest occurred at home (58.8%), in the South census region (65.4%), and in urban settings (79.8%). The most commonly reported medications used in out‐of‐hospital cardiac arrest were: epinephrine (22.5%), amiodarone (2.9%), sodium bicarbonate (6.2%), glucose (3.0%), and naloxone (5.1%). Commonly reported procedures included CPR (26.1%), orotracheal intubation (14.2%), bag‐valve‐mask ventilation (10.1%), manual defibrillation (29.3%) and automated external defibrillation (5.6%). Out‐of‐hospital cardiac arrest EMS treatment times were: elapsed response time (median = 7 minutes [interquartile range (IQR) = 5–10]), scene time (median = 17 minutes [IQR = 12–25]), and elapsed transport time (median = 11 minutes [IQR = 6–17]).
Conclusions
Using information available in the 2016 NEMSIS data, we estimate that there were over 570,000 reported adult out‐of‐hospital cardiac arrests in the United States. These results highlight the challenges of characterizing the epidemiology of adult out‐of‐hospital cardiac arrest in the United States.
Keywords: emergency medical services, out‐of‐hospital cardiac arrest
1. INTRODUCTION
1.1. Background
Out‐of‐hospital cardiac arrest is a major public health problem. An important step in reducing the public health burden of out‐of‐hospital cardiac arrest is understanding the number of persons suffering from the condition each year. Prior estimates of the annual number of adult out‐of‐hospital cardiac arrest in the United States range from 341,397–353,246, with survival ranging from 3.4%–22.0%. 1 , 2 , 3 , 4 However, these figures have important limitations. Some of these estimates were formulated from weighted national health surveys, such as Atherosclerosis Risk in Communities Study (ARIC) and Medical Expenditure Panel Survey (MEPS). 2 Other estimates were extrapolated from clinical data originated from single regions or communities. For example, the Resuscitation Outcomes Consortium (ROC) extrapolated out‐of‐hospital cardiac arrest data based on 7 United States and 3 Canadian communities. 5 The Cardiac Arrest Registry to Enhance Survival (CARES) extrapolated out‐of‐hospital cardiac arrest findings based on data from 73 emergency medical service (EMS) agencies from 23 states. 6
1.2. Importance
Most out‐of‐hospital cardiac arrest undergoing life‐saving efforts receive initial care from EMS. Thus, data collected through EMS responses might be helpful in defining the total number of out‐of‐hospital cardiac arrest cases and their characteristics.
1.3. Goals of this investigation
The National Emergency Medical Services Information System (NEMSIS) is a unique registry of EMS encounters in the United States. We sought to determine the national characteristics of adult out‐of‐hospital cardiac arrest reported in NEMSIS.
2. METHODS
2.1. Study design
We analyzed data from the 2016 NEMSIS public research dataset. The Committee for the Protection of Human Subjects at the University of Texas Health Science Center at Houston approved the study.
2.2. Data source
Formed in 2006, NEMSIS is a database system standardizing and aggregating EMS response data throughout the United States. 7 The overall goal of NEMSIS is to assist EMS stakeholders in assessing EMS needs and performance and planning strategies through uniform nationwide data. NEMSIS contains comprehensive information on the clinical course of EMS care, including dispatch and response characteristics, patient demographics, clinical presentation, interventions and medications, and episode outcomes. We used the 2016 NEMSIS Public Release Dataset (version 2.2.1) for this study, which included data on most EMS response data for 46 of 50 states (Figure 1). NEMSIS does not contain information on the hospital course or outcomes of EMS patients nor of the personnel providing EMS care.
FIGURE 1.
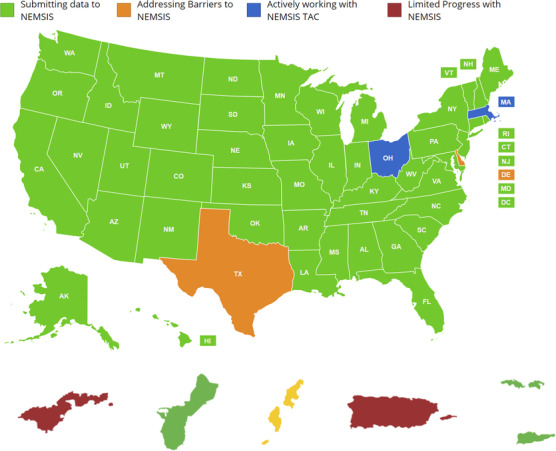
States contributing to NEMSIS Version 2
2.3. Selection of subjects—identification of out‐of‐hospital cardiac arrests
We included emergency “9‐1‐1” EMS responses reported in the data set (variable e02_04 [type of service requested] = 30 [911 response (scene)]). We excluded EMS intercepts, interfacility transfers, medical transports (scheduled transports for interfacility, critical care, and convalescent transports), mutual aid, and standby events. We limited the analysis to adults ≥18 years of age; we excluded all responses with unknown age (14.6%).
The Bottom Line
The authors used the NEMSIS data set to estimate the number of out‐of‐hospital cardiac arrest cases in the United States annually, and they estimate over 570,000 cases which is much higher than previous population‐based estimates.
The identification of out‐of‐hospital cardiac arrest from EMS records presents challenges. Although indicator variables for patient condition cardiac arrest and attempted cardiac arrest resuscitation exist, EMS personnel do not consistently report the entire spectrum of variables consistent with out‐of‐hospital cardiac arrest. Resuscitative interventions such as cardiopulmonary resuscitation (CPR) and defibrillation are often the only indications of the presence of out‐of‐hospital cardiac arrest. Therefore, we identified out‐of‐hospital cardiac arrest using 5 indicators from 4 variables: (1) EMS reported clinical condition of cardiac arrest (NEMSIS variable E11_01, prior to or after EMS arrival), (2) reported initiation of cardiac arrest resuscitation (variable E11_03), (3) performance of CPR chest compressions (variable E19_03), and (4) performance of defibrillation (variable E19_03). For the primary analysis, we defined out‐of‐hospital cardiac arrest as the combined presence of any of these indicators. In sensitivity analyses, we explored the use of different combinations of the component variables. Patients reported as “dead on scene” were retained in the analysis if they fulfilled 1 of the 5 out‐of‐hospital cardiac arrest indicators.
2.4. Clinical characteristics
Among the cases identified as out‐of‐hospital cardiac arrest, we sought to determine patient demographics, response characteristics, and clinical interventions. Demographics included age, sex, race, ethnicity, location, US census region, and urbanicity. Response characteristics included dispatch complaint and elapsed response times. Clinical medications for out‐of‐hospital cardiac arrest included epinephrine, amiodarone, sodium bicarbonate, glucose, and naloxone. Clinical procedures included CPR, orotracheal intubation, bag‐valve‐mask ventilation, and automated external defibrillation. We identified the census region and urbanicity of each out‐of‐hospital cardiac arrest event. We examined care times intervals including system response time (interval between unit notified by dispatch and unit arrival on scene), scene time (interval between unit arrival on scene and unit left scene), and elapsed transport time (interval between unit left scene and patient arrived at destination).
2.5. Data analysis
We analyzed the data using descriptive techniques, determining binomial proportions with exact 95% confidence intervals (CI). We determined the total number of out‐of‐hospital cardiac arrest cases based upon both the individual indicators as well as the composite of all indicators. We calculated the incidence of out‐of‐hospital cardiac arrest relative to the total number of EMS events. We explored the effect of applying varying out‐of‐hospital cardiac arrest definitions upon the total estimated number of out‐of‐hospital cardiac arrest. Because multiple EMS units may potentially respond to the same emergency event, we conducted a sensitivity analysis limiting to only events where the EMS vehicle was designated as a transport unit, excluding those designated as non‐transport, rescue, and supervisor. For out‐of‐hospital cardiac arrests identified using the composite definition, we determined the patient demographics, EMS response characteristics, and clinical interventions.
We conducted all analyses using Stata 15.1 (Stata, Inc., College Station, TX).
3. RESULTS
Among 29,919,652 reported EMS events, we excluded 2,328,480 canceled calls, interfacility transports, and stand‐bys. We further excluded 1,445,211 EMS events with children and 7,559,940 events with missing ages, leaving 18,586,021 adult “9‐1‐1” emergency responses in the analysis (Figure 2).
FIGURE 2.
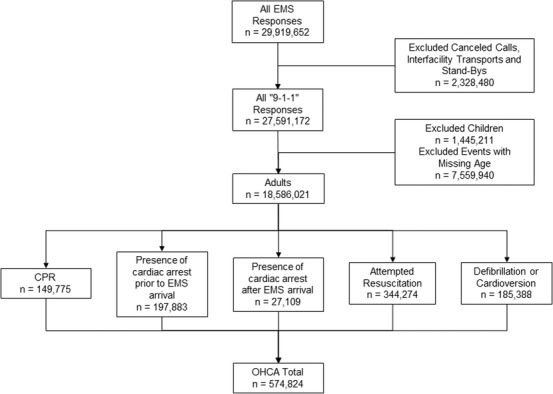
EMS events with indicators of out‐of‐hospital cardiac arrest in the NEMSIS
There were 224,992 events with a reported patient clinical condition of cardiac arrest (197,883 prior to EMS arrival and 27,109 after EMS arrival), 344,274 with attempts at cardiac arrest resuscitation, 149,775 receiving CPR, and 185,358 receiving at least 1 defibrillation attempt (Table 1). There were 574,824 (95% CI = 573,362–576,289) EMS responses with at least one of the defined cardiac arrest indicators (Table 1), reflecting an estimated incidence of 30.9 (95% CI = 30.8–31.0) out‐of‐hospital cardiac arrest per 1000 adult emergency events. The estimated number of out‐of‐hospital cardiac arrest events varied with differing combinations of cardiac arrest indicators. (Appendix 1) EMS attempted resuscitation and defibrillation exhibited the most overlap between out‐of‐hospital cardiac arrest indicators. When including only incidents where the responding vehicle was designated as the “transport” provider, the estimated number of out‐of‐hospital cardiac arrest was 500,415 (95% CI = 499,048–501,785) out‐of‐hospital cardiac arrest.
TABLE 1.
Indicators of adult out‐of‐hospital cardiac arrest in NEMSIS
| Indicator | n (%) |
|---|---|
| Reported patient condition = cardiac arrest prior to EMS arrival | 197,883 (1.1) |
| Reported patient condition = cardiac arrest after EMS arrival | 27,109 (0.2) |
| Reported attempted resuscitation of cardiac arrest | 344,274 (1.9) |
| Performance of cardiopulmonary resuscitation | 149,775 (0.8) |
| Defibrillation or cardioversion | 185,388 (1.0) |
| All categories (presence of any of the indicators) | 574,824 (3.1) |
Reflects total of n = 18,586,021 EMS events.
The EMS events with at least 1 out‐of‐hospital cardiac arrest indicator included mostly women (55.1%), older individuals (mean age 62.4 years), whites (53.0%), and non‐Hispanics (45.8%) (Table 2). Most out‐of‐hospital cardiac arrest events occurred at home (58.8%), in the South census region (65.4%), and in the urban setting (79.8%) (Table 2). Dispatch complaints for adult out‐of‐hospital cardiac arrest responses mainly included cardiac arrest (20.6%) and injury/poisoning/environmental complaints (14.5%). Median out‐of‐hospital cardiac arrest EMS elapsed response time was 7 minutes (interquartile range [IQR] = 5–10). Median out‐of‐hospital cardiac arrest scene treatment time was 17 minutes (IQR = 12–25). Median elapsed transport time was 11 minutes (IQR = 6–17).
TABLE 2.
Patient characteristics of out‐of‐hospital cardiac arrest events in the NEMSIS data set
| Characteristic | Adults (n = 574,824) |
|---|---|
| Age | |
| Mean ± SD | 62.4 ± 20.1 |
| Median (IQR) | 65 (49–79) |
| Sex, n (%) | |
| Male | 255,883 (44.5) |
| Female | 316,375 (55.1) |
| Unknown | 2566 (0.5) |
| Race, n (%) | |
| White | 304,494 (53.0) |
| African American | 79,883 (13.9) |
| Asian | 3423 (0.6) |
| American Indian/Alaska Native | 2252 (0.4) |
| Native Hawaiian/Pacific Islander | 1091 (0.2) |
| Other race | 33,722 (5.9) |
| Unknown | 149,959 (26.1) |
| Ethnicity, n (%) | |
| Hispanic | 59,761 (10.4) |
| Non‐Hispanic | 263,027 (45.8) |
| Unknown | 252,036 (43.9) |
| Incident location, n (%) | |
| Home | 338,036 (58.8) |
| Health care facility | 47,326 (8.2) |
| Residential institution | 40,207 (7.0) |
| Other locations | 126,278 (22.0) |
| Unknown | 22,977 (4.0) |
| US Census Region, n (%) | |
| Island areas | 460 (0.1) |
| Midwest | 70,990 (12.4) |
| Northeast | 56,769 (9.9) |
| South | 376,176 (65.4) |
| West | 70,429 (12.3) |
| Urbanicity, n (%) | |
| Rural | 26,527 (4.6) |
| Suburban | 38,340 (6.7) |
| Urban | 458,430 (79.8) |
| Wilderness | 6598 (1.2) |
| Unknown | 44,929 (7.8) |
| Dispatch complaint, n (%) | |
| Cardiac arrest | 118,546 (20.6) |
| Injury/poisoning/environmental | 83,358 (14.5) |
| Respiratory emergencies | 45,887 (8.0) |
| Other cardiac emergencies | 37,997 (6.6) |
| Neurologic problems | 21,907 (3.8) |
| Other | 155,929 (27.1) |
| Unknown | 111,200 (19.4) |
| Response time a (min) | n = 573,741 (99.8) |
| Median (IQR) | 7 (5–10) |
| Scene time b (min) | n = 457,190 (79.5) |
| Median (IQR) | 17 (12–25) |
| Transport time c (min) | n = 407,395 (70.9) |
| Median (IQR) | 11 (6–17) |
Includes EMS events with at least 1 of the 5 defined out‐of‐hospital cardiac arrest indicators.
Time difference between unit notified by dispatch and unit arrival on scene.
Time difference between unit arrival on scene and unit left scene.
Time difference between unit left scene and patient arrived at destination.
Among episodes with at least 1 out‐of‐hospital cardiac arrest indicator, epinephrine (22.5%), amiodarone (2.9%), sodium bicarbonate (6.1%), glucose (3.0%), and naloxone (5.1%) were the most commonly used medications (Table 3). The most commonly performed interventions were CPR (26.1%), orotracheal intubation (14.2%), bag‐valve‐mask ventilation (10.1%), manual defibrillation (29.3%), and automated external defibrillation (5.6%) (Table 4).
TABLE 3.
Medications administered among out‐of‐hospital cardiac arrest cases identified in the NEMSIS data set
| Medications n (%) | Out‐of‐hospital cardiac arrest events (n = 574,824) |
|---|---|
| Vasopressors | |
| Epinephrine | 129,389 (22.5) |
| Vasopressin | 1494 (0.3) |
| Antiarrhythmic, electrolytes, and other medications | |
| Atropine | 6533 (1.1) |
| Lidocaine | 4069 (0.7) |
| Amiodarone | 16,476 (2.9) |
| Adenosine | 1381 (0.2) |
| Calcium | 6187 (1.1) |
| Magnesium | 1282 (0.2) |
| Sodium bicarbonate | 35,052 (6.1) |
| Glucose (D50W) | 17,347 (3.0) |
| Insulin | 9 (0.0) |
| Continuous infusions | |
| Dopamine | 2352 (0.4) |
| Dobutamine | 29 (0.0) |
| Norepinephrine | 319 (0.1) |
| Phenylephrine | 37 (0.0) |
| Antidotes | |
| Flumazenil | 22 (0.0) |
| Naloxone | 29,036 (5.1) |
| Intravenous fluids | |
| Lactated Ringer's solution | 3024 (0.5) |
| Normal saline | 71,505 (12.4) |
| D5W, D10W | 813 (0.1) |
| Other medications | |
| Antihypertensive | 10,641 (1.9) |
| Sedatives | 6448 (1.1) |
| Paralytics | 2106 (0.4) |
| Anticoagulants | 122 (0.0) |
TABLE 4.
Procedures performed among out‐of‐hospital cardiac arrest cases identified in the NEMSIS data set
| Procedure | Out‐of‐hospital cardiac arrest events (n = 574,824) |
|---|---|
| Airway | |
| Bag‐valve mask ventilation | 57,971 (10.1) |
| Impedance threshold device | 17,625 (3.1) |
| Endotracheal intubation | |
| Orotracheal intubation | 81,568 (14.2) |
| Nasotracheal intubation | 16,674 (2.9) |
| Rapid sequence intubation | 17,038 (3.0) |
| Video laryngoscopy | 16,907 (2.9) |
| Supraglottic airway | |
| Combitube | 23,824 (4.1) |
| EOA/EGTA | 16,205 (2.8) |
| King laryngeal tube | 34,566 (6.0) |
| Laryngeal mask airway | 20,106 (3.5) |
| Cricothyrotomy | 16,196 (2.8) |
| a Other | 448,654 (78.1) |
| Cardiopulmonary resuscitation chest compressions | 149,775 (26.1) |
| Cardiac pacing | 19,300 (3.4) |
| Cardioversion | 20,624 (3.6) |
| Manual defibrillation | 168,154 (29.3) |
| Automated external defibrillation (AED) | 16,335 (2.9) |
| Patient cooling (cold pack, etc) | 1669 (0.3) |
EOA/EGTA, esophageal obturator airway/esophageal gastric tube airway.
Other airway procedures include bagged via tube, changing of tracheostomy tube, direct laryngoscopy, extubation, etc.
4. LIMITATIONS
Although NEMSIS encompasses most of the United States, select regions are still not represented in the data set. Reporting to NEMSIS is voluntary; although the majority of EMS events are reported to NEMSIS, the degree of missingness varies across states. In addition, there are inconsistencies in a few of the variables generated in the data collection process. Because NEMSIS captures data on only 46 of 50 states and because data capture in many states is incomplete, the estimated total number of out‐of‐hospital cardiac arrest in the United States may be even higher.
NEMSIS was not designed to identify or characterize out‐of‐hospital cardiac arrest. Our 5 selected indicators are relatively unique to out‐of‐hospital cardiac arrest. We included cardioversion as an indicator of out‐of‐hospital cardiac arrest, which may have slightly inflated the number of out‐of‐hospital cardiac arrest. As with most clinical registries, underreporting and missingness (age, race, medication info, etc) are potential concerns in NEMSIS. The extent of duplicate EMS response in NEMSIS is unknown.
We could not differentiate procedures performed and medications given before or after the onset of cardiac arrest. We also do not have granular information on the timing or dosage of medications of the performance of certain procedures. Due to NEMSIS policies, we could not examine variations among more granular geographic units smaller than census region. NEMSIS does not contain any information on the outcomes of patients, and thus, we cannot validate the mortality rate with previous studies.
5. DISCUSSION
An important step in mitigating the public health burden of out‐of‐hospital cardiac arrest in the United States is to estimate the number of cases. In this study, we illustrated the use of the large scale NEMSIS data set to estimate the total number of adult out‐of‐hospital cardiac arrest in the United States. We observed that over 570,000 EMS events in NEMSIS contained at least 1 of 5 indicators of out‐of‐hospital cardiac arrest. Based on the total US population from states contributing to NEMSIS in 2016, this estimate would translate to an adult out‐of‐hospital cardiac arrest incidence of 269.4 per 100,000 person‐years. 8
Prior estimates suggesting 300,000–450,000 annual adult out‐of‐hospital cardiac arrests in the United States are based on extrapolation from data sampled from individual communities. 2 Rea et al 9 estimated 55.0 EMS‐treated cardiac arrests per 100,000 person‐years, but the study was confined to 35 US communities identified from studies published between 1980 and 2003 and could not identify any characteristics of out‐of‐hospital cardiac arrest patients. Using 2006–2007 data from 10 North American communities in the ROC, Nichol et al 5 estimated the incidence of EMS‐treated out‐of‐hospital cardiac arrest at 52.1 per 100,000 person‐years (IQR = 48.0–70.1 per 100,000). McNally et al 6 reported 31,000 adult out‐of‐hospital cardiac arrest cases from October 2005 to December 2010 in the CARES study. In contrast, the NEMSIS data used in this analysis has enormous geographic reach, encompassing most of the EMS events in 46 of 50 US states.
Our estimates using the NEMSIS data must be tempered by important limitations of the data set. First, NEMSIS does not link to hospital data, and thus we cannot ascertain clinical outcomes such as survival and neurologic function. Linkage with hospital data is not currently possible given the scale of NEMSIS. Prior studies such as those using ROC and CARES data have found out‐of‐hospital cardiac arrest survival ranging from 4.5% to 9.6%. 3 , 5 , 6 We identified out‐of‐hospital cardiac arrest using 5 indicator variables; the total estimated number of out‐of‐hospital cardiac arrest varies from 149,775 to 574,824 depending upon the combination of these surveillance variables (Appendix 1). 5 , 6 Prior studies used narrower criteria for identifying out‐of‐hospital cardiac arrest. For example, CARES defined cases of out‐of‐hospital cardiac arrest by the delivery of resuscitation interventions (CPR or defibrillation). 6 ROC defined cases of out‐of‐hospital cardiac arrest as those receiving EMS attempted external defibrillation or chest compressions. 5 In many EMS systems, multiple units may respond to an out‐of‐hospital cardiac arrest event; for example, a basic life support and an advanced life support unit may be jointly dispatched to an out‐of‐hospital cardiac arrest event. Our sensitivity analysis including only EMS units designated as a transport vehicle reduced the estimated total number of out‐of‐hospital cardiac arrest by ≈12.9%.
Our analysis using NEMSIS also revealed unexpected findings. For example, there were inconsistencies such as the number of patients receiving defibrillation exceeded those receiving CPR; although likely due to the underreporting of CPR, we do not know the exact etiology for this discrepancy. The incidence of out‐of‐hospital cardiac arrest in the South census region was disproportionately higher than in other regions; while many life‐threatening conditions are more prevalent in the South, the differences we observed are likely influenced by case‐reporting practices. 10 We found a higher number of out‐of‐hospital cardiac arrest among women than men, contrasting with prior studies. 5 , 6 The proportion of cases receiving resuscitative medications or interventions was far lower than expected; for example, only one‐third received medications. In contrast, almost 3% of potential out‐of‐hospital cardiac arrest cases underwent cricothryoidotomy, a figure much higher than previously reported. These observations point to idiosyncrasies with the NEMSIS data set that must be accounted for in any analysis. We do not know if these inconsistencies result from variations in EMS reporting and documentation or the national data aggregation process. Investigators using NEMSIS to characterize out‐of‐hospital cardiac arrest must be aware of these important limitations.
If further validated, our observations using NEMSIS could have important implications for out‐of‐hospital cardiac arrest planning and care. Using information available in NEMSIS, we estimated a national incidence of out‐of‐hospital cardiac arrest over 50% higher than previous reports. Ample data indicate the effectiveness of coordinated community‐based approaches to out‐of‐hospital cardiac arrest, including early arrest recognition, early calling of 9‐1‐1, early CPR, early automated external defibrillation use, early EMS care, and quality post‐arrest critical care hospital care. 1 The evaluation of novel data sources must continue to precisely estimate the public burden of out‐of‐hospital cardiac arrest and to gauge the impact of community initiatives to improve out‐of‐hospital cardiac arrest care and outcomes.
In conclusion, using information available in the 2016 NEMSIS data set, we estimated that there were over 570,000 reported adult out‐of‐hospital cardiac arrest in the United States. These results highlight the challenges of characterizing the epidemiology of adult out‐of‐hospital cardiac arrest in the United States.
DISCLAIMER
Dr. Blaivas was the supervising editor of this manuscript. Dr. Wang did not participate in the editorial decision to review or accept this article.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
HW takes responsibility for the paper as a whole.
Biography
Hei Kit Chan, PhD, is a PhD candidate in Biostatistics at University of Texas Health Science Center at Houston.

APPENDIX 1. COMBINATIONS OF OUT‐OF‐HOSPITAL CARDIAC ARREST INDICATORS
1.1.
| Combinations of indicators | n |
|---|---|
| 1 | 149,775 |
| 2 | 197,883 |
| 3 | 27,109 |
| 4 | 344,274 |
| 5 | 185,388 |
| 1+2 | 252,611 |
| 1+3 | 159,667 |
| 1+4 | 390,975 |
| 1+5 | 277,906 |
| 2+3 | 224,992 |
| 2+4 | 415,930 |
| 2+5 | 342,592 |
| 3+4 | 350,313 |
| 3+5 | 206,642 |
| 4+5 | 486,897 |
| 1+2+3 | 262,503 |
| 1+2+4 | 453,380 |
| 1+2+5 | 371,676 |
| 1+3+4 | 394,919 |
| 1+3+5 | 286,405 |
| 1+4+5 | 510,245 |
| 2+3+4 | 421,969 |
| 2+3+5 | 363,846 |
| 2+4+5 | 554,746 |
| 3+4+5 | 492,215 |
| 1+2+3+4 | 457,324 |
| 1+2+3+5 | 380,175 |
| 1+2+4+5 | 571,094 |
| 1+3+4+5 | 513,975 |
| 2+3+4+5 | 560,064 |
| 1+2+3+4+5 | 574,824 |
1: Performance of cardiopulmonary resuscitation.
2: Indication of the presence of cardiac arrest prior to EMS arrival.
3: Indication of the presence of cardiac arrest after EMS arrival.
4: Attempted resuscitation.
5: Defibrillation.
Chan HK, Okubo M, Callaway CW, Mann NC, Wang HE. Characteristics of adult out‐of‐hospital cardiac arrest in the National Emergency Medical Services Information System. JACEP Open. 2020;1:445–452. 10.1002/emp2.12106
Reprints not available from the authors.
Funding and support: ByJACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Nicholas M. Mohr, MD, MS.
REFERENCES
- 1. Becker LB, Aufderheide TP, Graham R. Strategies to improve survival from cardiac arrest: a report from the Institute of Medicine. JAMA. 2015;314:223‐224. [DOI] [PubMed] [Google Scholar]
- 2. Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics‐2019 update: a report from the American Heart Association. Circulation. 2019;139:e56‐e528. [DOI] [PubMed] [Google Scholar]
- 3. Cardiac Arrest Registry to Enhance Survival . Available at https://mycares.net. Accessed May 20, 2020.
- 4. Kurz MC, Donnelly JP, Wang HE. Variations in survival after cardiac arrest among academic medical center‐affiliated hospitals. PLoS One. 2017;12:e0178793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nichol G, Thomas E, Callaway CW, et al. Regional variation in out‐of‐hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423‐1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McNally B, Robb R, Mehta M, et al. Out‐of‐hospital cardiac arrest surveillance—Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011;60:1‐19. [PubMed] [Google Scholar]
- 7. NEMSIS . Available at https://nemsis.org/. Accessed March 12, 2020.
- 8. United States Census. Explore Census Data . Available at https://data.census.gov/cedsci/. Accessed March 12, 2020.
- 9. Rea TD, Eisenberg MS, Sinibaldi G, White RD. Incidence of EMS‐treated out‐of‐hospital cardiac arrest in the United States. Resuscitation. 2004;63:17‐24. [DOI] [PubMed] [Google Scholar]
- 10. Wang HE, Devereaux RS, Yealy DM, Safford MM, Howard G. National variation in United States sepsis mortality: a descriptive study. Int J Health Geogr. 2010;9:9. [DOI] [PMC free article] [PubMed] [Google Scholar]


