Abstract
Background
Shock from medical and traumatic conditions can result in organ injury and death. Limited data describe out‐of‐hospital treatment of shock. We sought to characterize adult out‐of‐hospital shock care in a national emergency medical services (EMS) cohort.
Methods
This cross‐sectional study used 2018 data from ESO, Inc. (Austin, TX), a national EMS electronic health record system, containing data from 1289 EMS agencies in the United States. We included adult (age ≥18 years) non‐cardiac arrest patients with shock, defined as initial systolic blood pressure ≤80 mm Hg. We compared patient demographics, clinical characteristics, and response (defined as systolic blood pressure increase) between medical and traumatic shock patients, looking at systolic blood pressure trends over the first 90 minutes of care.
Results
Among 6,156,895 adult 911 responses, shock was present in 62,867 (1.02%; 95% confidence interval [CI] = 1.01%–1.03%); 54,239 (86.3%) medical and 5978 (9.5%) traumatic, and 2650 unknown. Medical was more common than traumatic shock in women and older patients. The most common injuries associated with traumatic shock were falls (37.6%) and motor vehicle crashes (18.7%). Mean initial and final medical systolic blood pressure were 71 ± 10 mm Hg and 99 ± 24 mm Hg. Systolic blood pressure increased in 88.8% and decreased or did not change in 11.0%. Mean initial and final trauma systolic blood pressure were 71 ± 13 mm Hg and 105 ± 28 mm Hg; systolic blood pressure increased in 90.4% and decreased/did not change in 9.6%. On fractional polynomial modeling, systolic blood pressure changes were greater and faster for trauma than medical shock.
Conclusions
In this national series, 1 of every 100 EMS encounters involved shock. These findings highlight the current course and care of shock in the out‐of‐hospital setting.
Keywords: emergency medical services, hypotension, paramedics, resuscitation, sepsis, shock, trauma
1. INTRODUCTION
1.1. Background
Shock is a condition of poor tissue perfusion often resulting from hypotension. If prolonged, subsequent hypoxia of tissues can result in severe and permanent organ dysfunction and even tissue death. 1 Early recognition and treatment of shock are important in minimizing related adverse outcomes. Out‐of‐hospital emergency medical services (EMS) personnel are often the first to care for patients experiencing shock. Estimates regarding the prevalence of out‐of‐hospital hypotensive shock range from 9.5 to 19.0/1000 EMS patient contacts. 2 The hospital mortality of patients presenting with out‐of‐hospital shock is 33%–52%, exceeding the 12% mortality of patients who experience shock within the emergency department (ED).
1.2. Importance
An important step in improving out‐of‐hospital shock outcomes is to understand the magnitude of the problem. Prior efforts describing out‐of‐hospital shock have been restricted to a single state and presented limited information on the response of patients to initial EMS shock care. 3 There have been no large series describing the longitudinal course and outcomes of EMS shock care.
1.3. Goals of this investigation
We sought to characterize adult out‐of‐hospital shock care in a national cohort of EMS patients.
2. MATERIALS AND METHODS
2.1. Study design and setting
We conducted a cross‐sectional analysis using data from ESO, Inc. (Austin, TX). The Committee for the Protection of Human Subjects of the University of Texas Health Science Center at Houston approved the study. ESO, Inc. is one of the nation's largest providers of EMS electronic health record systems. The software system is internet‐based, with storage of clinical data at a central data warehouse. The software includes patient characteristics, vital signs, medications, agency information, incident details, narrative information, airway, defibrillation, and interventions. We used data from the 2018 ESO research data set, which included records from over 1200 EMS agencies in the United States that consented to release of de‐identified data for research purposes.
2.2. Selection of subjects
We included EMS patients initially presenting with shock, which we defined as initial systolic blood pressure ≤80 mm Hg. Although some sources define shock as systolic blood pressure ≤90 mm Hg, 2 we chose ≤80 mm Hg to focus attention on higher acuity patients. Whereas some patients may present with shock without hypotension, we opted to use systolic blood pressure as an inclusion criterion because normotensive shock is difficult to identify from data available in electronic medical records. We excluded those with a reported initial systolic blood pressure ≤0 mm Hg because we assumed that those values were due to a recording error or that the patient had expired. We excluded children (<18 years), interfacility transfers, patients found dead on EMS arrival, cardiac arrest patients, and non‐shock patients.
2.3. Outcomes
We examined key demographic and clinical characteristics of EMS shock patients. First, we separately identified medical and traumatic shock, using the medical/trauma classification variable in the data set. Although not formally defined in the national EMS data standard, in practice, EMS providers generally select the trauma designation for patients if an injury is present. Clinical characteristics included initial systolic blood pressure, EMS agency type, incident location, response time (dispatch to on scene), scene time (on scene to depart scene), transport time (depart scene to at destination), and receiving facility. For cases of medical shock, we described the distribution of underlying suspected illnesses associated with the case using EMS practitioners’ reported primary impression in the data set. For traumatic shock cases, we determined the injury mechanisms associated with the case using the primary injury listed in the data set. Treatment interventions included administration of fluids and vasopressor use. We determined the trends in systolic blood pressure during EMS care, limiting to the first 90 minutes of EMS care. We similarly determined shock index for the first 90 minutes of care.
2.4. Data analysis
We compared demographic, response, and clinical characteristics between medical and traumatic shock patients using univariate odds ratios (OR) with 95% confidence intervals (CI). We used the Wilcoxon rank‐sum test to compare median response, scene, and transport times between the 2 groups. We used box plots to characterize trends in systolic blood pressure and shock index over the first 90 minutes of treatment, partitioning the time in EMS care into 5‐minute segments. We used fractional polynomial regression models to characterize trends in systolic blood pressure over time.
We also sought to characterize physiological response to EMS care (all care given during EMS transport). We calculated the difference between the first and last systolic blood pressure measurements. We classified patients as EMS care responders (systolic blood pressure increased) or non‐responders (systolic blood pressure decreased or did not change). We then compared response between patients who did and did not receive shock treatment (administration of fluid ≥250 mL and/or vasopressor use) by medical and traumatic groups. All analyses were performed using Stata 15.1 (College Station, TX).
3. RESULTS
During the study period there were 7,574,879 EMS patient encounters from 1289 EMS agencies. After applying exclusions, there were 62,867 (1%) shock patients, including 54,239 (86%) medical shock patients, and 5978 (10%) traumatic shock patients; shock type was not reported in 2650 (4%) patients (Figure 1).
FIGURE 1.
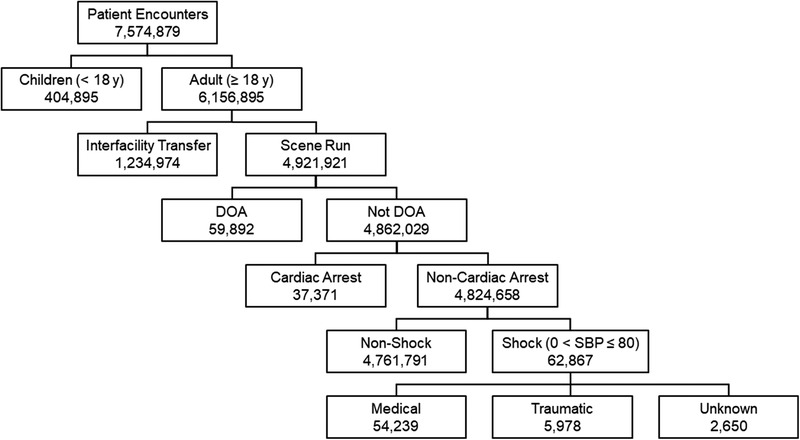
Study population. DOA; dead on arrival
The Bottom Line
In this national series, 1 of every 100 EMS encounters involved a patient in shock. Medical was more common than traumatic shock in women and older patients. The most common injuries associated with traumatic shock were falls (37.6%) and motor vehicle crashes (18.7%).
Medical shock was more common in older patients (Table 1). Males were less likely to experience medical shock. Non‐Hispanic patients were more likely to experience medical shock. Medical and traumatic shock patients were most often found in a place of residence. Traumatic shock patients were more likely be found in public settings compared to medical shock patients. For medical shock patients, the top underlying suspected illnesses were shock, cardiac symptoms, respiratory, and other (Table 2). For traumatic shock patients, the most common injury mechanisms were falls, vehicular collision, shooting, and unknown (Table 3). For patients with documented fluid administration, normal saline was the most common fluid given (Table 4). Pressor use occurred in <2% of patients. Median treatment time was 17 minutes (interquartile range [IQR]: 8–27); total treatment time was ≤30 minutes and ≤60 minutes for 80.3% and 98.6% of the cohort, respectively.
TABLE 1.
Characteristics of 62,867 out‐of‐hospital shock
| Characteristic | All shock, n (%) | Medical shock, n (%) | Traumatic shock, n (%) | OR medical versus traumatic shock (95% CI) |
|---|---|---|---|---|
| Age (y) | ||||
| 18–30 | 3625 (5.8) | 2502 (4.6) | 980 (16.4) | Reference |
| 31–40 | 3407 (5.4) | 2571 (4.7) | 672 (11.2) | 1.50 (1.34–1.68) |
| 41–50 | 5120 (8.1) | 4292 (7.9) | 613 (10.3) | 2.74 (2.45–3.07) |
| 51–60 | 10,495 (16.7) | 9067 (16.7) | 995 (16.6) | 3.57 (3.23–3.94) |
| 61–70 | 14,181 (22.6) | 12,542 (23.1) | 1036 (17.3) | 4.74 (4.30–5.23) |
| >70 | 26,039 (41.4) | 23,265 (42.9) | 1682 (28.1) | 5.42 (4.95–5.92) |
| Sex | ||||
| Female | 30,712 (48.9) | 26,910 (49.6) | 2653 (44.4) | Reference |
| Male | 31,257 (49.7) | 26,738 (49.3) | 3275 (54.8) | 0.80 (0.76–0.85) |
| Unknown | 898 (1.4) | 591 (1.1) | 50 (0.8) | N/A |
| Race | ||||
| American Indian or Alaska Native | 119 (0.2) | 106 (0.2) | 12 (0.2) | Reference |
| Asian | 543 (0.9) | 483 (0.9) | 47 (0.8) | 1.16 (0.60–2.27) |
| Black or African American | 10,565 (16.8) | 9398 (17.3) | 959 (16.0) | 1.11 (0.61–2.02) |
| Native Hawaiian or other Pacific Islander | 79 (0.1) | 72 (0.1) | 6 (0.1) | 1.36 (0.49–3.79) |
| Other race | 105 (0.2) | 86 (0.2) | 17 (0.3) | 0.57 (0.26–1.25) |
| White | 44,611 (71.0) | 39,128 (72.1) | 4341 (72.6) | 1.02 (0.56–1.86) |
| Unknown | 6844 (10.9) | 4967 (9.2) | 596 (10.0) | N/A |
| Ethnicity | ||||
| Hispanic or Latino | 2879 (4.6) | 2484 (4.6) | 378 (6.3) | Reference |
| Not Hispanic or Latino | 49,666 (79.0) | 44,538 (82.1) | 4829 (80.8) | 1.40 (1.25–1.57) |
| Unknown | 10,322 (16.4) | 7217 (13.3) | 771 (12.9) | N/A |
| Initial systolic blood pressure (mm Hg) | ||||
| 1–20 | 577 (0.9) | 416 (0.8) | 129 (2.2) | 0.36 (0.30–0.44) |
| 21–40 | 402 (0.6) | 338 (0.6) | 46 (0.8) | 0.82 (0.60–1.12) |
| 41–60 | 8570 (13.6) | 7528 (13.9) | 684 (11.4) | 1.23 (1.13–1.33) |
| 61–80 | 53,318 (84.8) | 45,957 (84.7) | 5119 (85.6) | Reference |
| EMS agency type | ||||
| Community, non‐profit | 39,355 (62.6) | 34,015 (62.7) | 3780 (63.2) | Reference |
| Fire department | 9086 (14.5) | 8052 (14.9) | 819 (13.7) | 1.09 (1.01–1.18) |
| Governmental, non‐fire | 9976 (15.9) | 8142 (15.0) | 977 (16.3) | 0.93 (0.86–1.00) |
| Private, non‐hospital | 4450 (7.1) | 4030 (7.4) | 402 (6.7) | 1.11 (1.00–1.24) |
| Incident location | ||||
| Healthcare facility | 10,055 (16.0) | 9496 (17.5) | 312 (5.2) | Reference |
| Public place | 6560 (10.4) | 5723 (10.6) | 662 (11.1) | 0.28 (0.25–0.33) |
| Residence | 40,245 (64.0) | 35,864 (66.1) | 3158 (52.8) | 0.37 (0.33–0.42) |
| Road/outdoor | 3520 (5.6) | 1612 (3.0) | 1675 (28.0) | 0.03 (0.03–0.04) |
| Other | 2398 (3.8) | 1535 (2.8) | 171 (2.9) | 0.30 (0.24–0.36) |
| Unknown | 89 (0.1) | 9 (0.0) | 0 (0.0) | N/A |
| Median minutes (interquartile range) | ||||
| Response time (dispatch to on scene) | 6 (5–10) | 6 (5–10) | 7 (5–10) | Rank‐sum P < 0.001 a |
| Scene time (on scene to depart scene) | 19 (14–24) | 19 (15–24) | 17 (12–24) | Rank‐sum P < 0.001 a |
| Transport time (depart scene to at destination) | 12 (7–18) | 12 (7–18) | 12 (8–19) | Rank‐sum P < 0.001 a |
| Receiving facility | ||||
| Non‐trauma center | 21,472 (34.2) | 19,942 (36.8) | 1448 (24.2) | Reference |
| Trauma center | 2665 (4.2) | 1859 (3.4) | 799 (13.4) | 0.17 (0.15–0.19) |
| Unknown | 38,730 (61.6) | 32,438 (59.8) | 3731 (62.4) | N/A |
CI, confidence interval; OR, odds ratio. Includes 54,239 medical and 5978 traumatic shock.
Wilcoxon rank‐sum test.
TABLE 2.
Suspected underlying illness for medical shock
| Suspected illness | n (%) |
|---|---|
| Airway obstruction | 25 (0.1) |
| Behavioral | 392 (0.7) |
| Cardiac arrest | 25 (0.1) |
| Cardiac symptoms | 4286 (7.9) |
| Diabetes/endocrine | 1221 (2.3) |
| Environmental | 267 (0.5) |
| Foreign body | 4 (0.007) |
| Gastrointestinal | 1168 (2.2) |
| Hemorrhage | 1790 (3.3) |
| Infectious | 2233 (4.1) |
| Injury/trauma | 216 (0.4) |
| Neurological | 1514 (2.8) |
| Obstetric/neonatal | 128 (0.2) |
| Pain | 2843 (5.2) |
| Poisoning/overdose | 1828 (3.4) |
| Renal | 1243 (2.3) |
| Respiratory | 3721 (6.9) |
| Shock | 10,525 (19.4) |
| Other | 20,804 (38.4) |
Includes n = 54,239 patients.
TABLE 3.
Injury mechanism for traumatic shock
| Injury mechanism | n (%) |
|---|---|
| Assault | 151 (2.5) |
| Bicycle | 4 (0.1) |
| Bite/poisoning | 9 (0.2) |
| Blunt | 8 (0.1) |
| Environmental | 2 (0.0) |
| Fall | 2247 (37.6) |
| Fire | 27 (0.5) |
| Shooting | 277 (4.6) |
| Sports | 21 (0.4) |
| Stabbing | 98 (1.6) |
| Vehicular | 1121 (18.7) |
| Unknown | 2013 (33.7) |
Includes n = 5978 patients.
TABLE 4.
Initial fluids, route, volume, and medications given for out‐of‐hospital shock
| Intervention | Medical shock, n (%) | Traumatic shock, n (%) |
|---|---|---|
| Intravenous fluid | ||
| Dextrose in water | 96 (0.2) | 3 (0.1) |
| Electrolytes | 293 (0.5) | 30 (0.5) |
| Normal saline | 19,898 (36.7) | 2145 (35.9) |
| Hypotonic saline | 4 (0.0) | 0 (0.0) |
| Lactated Ringer's | 1482 (2.7) | 185 (3.1) |
| Blood | 3 (0.0) | 0 (0.0) |
| Unknown | 17,035 (31.4) | 2157 (36.1) |
| Vascular route | ||
| Central line | 14 (0.0) | 1 (0.0) |
| Peripheral intravenous line | 47,034 (86.7) | 4668 (78.1) |
| Intraosseous access | 825 (1.5) | 181 (3.0) |
| Unknown | 14,053 (25.9) | 1910 (32.0) |
| Fluid volume | ||
| <250 mL | 15,989 (41.0) | 1457 (24.4) |
| ≥250 mL | 22,970 (59.0) | 2537 (42.4) |
| Unknown | 15,280 (28.2) | 1984 (33.2) |
| Vasopressors | ||
| Dopamine | 218 (0.4) | 3 (0.1) |
| Epinephrine | 591 (1.1) | 30 (0.5) |
| Norepinephrine | 132 (0.2) | 2 (0.0) |
| Phenylephrine | 17 (0.0) | 0 (0.0) |
| Vasopressin | 2 (0.0) | 0 (0.0) |
Includes 54,239 medical and 5978 traumatic shock.
Excluding 15% of patients with only 1 systolic blood pressure measurement, mean initial and final systolic blood pressures were 71 ± 10 and 99 ± 24 mm Hg for medical shock and 71 ± 13 and 105 ± 28 mm Hg for traumatic shock (Table 5). Among medical shock, systolic blood pressure increased in 88.8% and decreased/did not change in 11.0%. Among traumatic shock, systolic blood pressure increased in 90.4% and decreased/did not change in 9.6%. Systolic blood pressure increases were observed in both medical and traumatic cases that did and did not receive shock treatment (Figure 2; Table 5). Fractional polynomial fits suggested that patients receiving no shock treatment exhibited greater systolic blood pressure increases over time (Figure 3). Across all groups, initial median shock index was >1.0 but approached normal levels (0.5–0.7) by 25 minutes of treatment (Figure 4).
TABLE 5.
Response to shock treatment, defined as administration of ≥250 mL intravenous fluid and/or vasopressor use
| Category | Initial SBP (SD), mm Hg | Final SBP (SD), mm Hg | Change in SBP (95% CI), mm Hg |
|---|---|---|---|
| Medical shock | |||
| Treatment | 70 (9) | 99 (22) | +28 (28–29) |
| No treatment | 71 (10) | 100 (27) | +29 (28–29) |
| Traumatic shock | |||
| Treatment | 71 (9) | 102 (25) | +31 (30–32) |
| No treatment | 72 (10) | 107 (30) | +36 (34–37) |
CI, confidence interval; SBP, systolic blood pressure.
FIGURE 2.
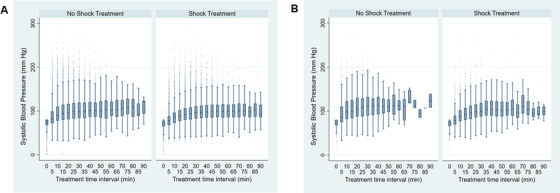
Systolic blood pressure over 5‐minute intervals for medical (A) and trauma (B) shock, stratified by shock treatment (administration of ≥250 mL intravenous fluid and/or vasopressor use)
FIGURE 3.
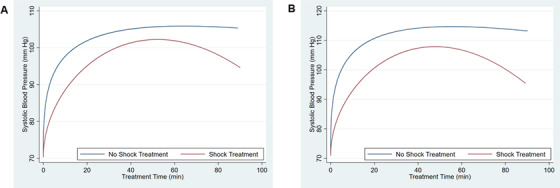
Fractional polynomial fits of systolic blood pressure over time for medical (A) and trauma (B) shock, stratified by shock treatment (administration of ≥250 mL intravenous fluid and/or vasopressor use)
FIGURE 4.
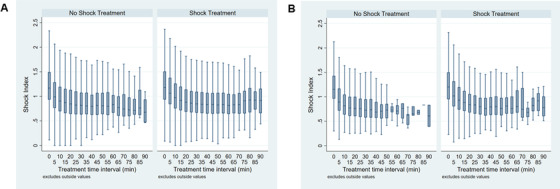
Shock index over 5‐minute intervals for medical (A) shock and trauma (B) shock, stratified by shock treatment (administration of ≥250 mL intravenous fluid and/or vasopressor use). Graphs exclude outliers
4. LIMITATIONS
Using systolic blood pressure as the sole indicator of shock and response is a significant limitation. However, systolic blood pressure is the measure most widely used to identify and gauge treatment of shock in the clinical setting. Alternate measures of shock such as serum lactate are potentially useful but are not widely available in the out‐of‐hospital setting. 4 , 5 We did include shock index as an alternative and additional indicator of shock in our analysis, but this measure is only limited in use in EMS. The timing of vital sign measurements was not protocolized. Treatment time varied across patients; certain patients may have developed or recovered from shock if they were observed for a longer period of time. We note that few patients had care extending beyond 60 minutes.
We excluded patients with an initial systolic blood pressure of 0 mm Hg assuming that the figures were erroneously reported. However, it is possible that a patient with a true initial systolic blood pressure of 0 could have been resuscitated upon EMS intervention. Only 15% of patients had only 1 systolic blood pressure measurement. Only a small number of cases included documentation on the use of vasopressors and fluid administration; it is unclear whether this reflects under‐documentation or a low incidence of pressor and/or fluid use. We could not determine the exact etiology of the shock. Although there were true increases and decreases in systolic blood pressure, it is difficult to ascertain whether this was due to inadequate treatment or the natural course of these patients.
Although our data are not nationally representative, they originate from over 1200 EMS agencies and are national in scope. We did not evaluate regional variations in geographic location or urbanicity. Our study was not intended to discern differences between urban and rural EMS care. Unequal observation periods is also another potential issue as advanced life support care is more likely in urban settings with shorter transport times. Hospital morbidity and mortality were not available in the data set.
5. DISCUSSION
Our findings provide important current perspectives of EMS shock care. One of every 100 adult EMS patients presented with shock. There were key differences between medical and traumatic shock cases both in suspected etiology and responsiveness over time. Traumatic shock patients experienced greater increases in systolic blood pressure than their medical counterparts. Although most patients demonstrated increases in systolic blood pressure during EMS care, a portion remained hypotensive. These results highlight opportunities for the early recognition and treatment of shock by EMS.
Few prior studies have described the characteristics or course of EMS shock patients. Our 1% shock prevalence is consistent with prior estimates of 0.95%–1.90% proposed by Holler et al. 2 Wang et al 3 examined EMS shock care using Pennsylvania statewide EMS data. Our current study using data from over 1200 EMS agencies across the United States exhibited similar patient demographics, shock prevalence, distribution between medical and trauma cases, suspected illnesses and injury mechanisms, and interventions. However, unlike the prior study, we were better able to characterize the course of clinical care including the interventions given as changes in blood pressure and shock index.
An interesting observation was that although the majority of EMS shock patients experienced increases in systolic blood pressure, a portion experienced no change or decreases in systolic blood pressure. Although this finding suggests the effectiveness of current EMS treatment practices, the exact reasons for the lack of response to care cannot be ascertained from these data. Potential reasons include the inadequacy of resuscitative care, the presence of multiple comorbidities, the severity of illness, or limitations in EMS treatment time. Additional information about shock subtypes could have enhanced these perspectives. For example, cardiogenic shock may be less amenable to treatments available in the out‐of‐hospital setting. We observed that medical shock cases were less responsive to shock treatment than traumatic cases but had only limited information regarding the patterns and severity of injury.
Another important observation was that 25% of patients with >1 systolic blood pressure measurement improved without any interventions. Seymour et al 6 found that half of EMS sepsis patients received no intravenous fluids. However, in some settings, practitioners use permissive hypotension in shock, restricting fluids to avoid fluid overload and related consequences. 7 , 8 While not indicated by our data, it is possible that strategies of fluid restriction may have a role in certain shock cases. EMS agencies in some settings use blood products as an alternative to fluids for trauma resuscitation. 9 , 10 Unfortunately, we could not fully ascertain blood product use in the current data set. Future study with prospective precise measurement of resuscitation measures and physiologic response are needed to better understand these diverse factors.
These results highlight the prominence of shock in EMS care and the opportunities for improving out‐of‐hospital shock care. In sepsis patients, Seymour et al 6 , 11 , 12 have found that EMS care can accelerate the hospital administration of intravenous fluid, but that less than half of EMS patients receive intravenous access. Although not defined by this study, there is potential guidance from in‐hospital practice guidelines. The Surviving Sepsis Campaign highlights the importance of early aggressive fluid resuscitation and early vasopressor administration in sepsis resuscitation. 13 Similarly, extensive guidelines on the management of heart failure have been published by the American Heart Association including the judicious use of vasopressors. 14 For traumatic hemorrhagic shock, blood products may play a key role in out‐of‐hospital resuscitation. In a randomized controlled trial, out‐of‐hospital thawed plasma administration was found to reduce 30‐day mortality when compared to standard‐care resuscitation for patients at risk for hemorrhagic shock. 15 Whole blood has been proposed as standard treatment, with many EMS agencies implementing its out‐of‐hospital use in the United States. 16 Although not supported by clinical data, some experts have suggested that triaging out‐of‐hospital shock cases to specialty shock centers could also potentially improve outcomes. 3 Finally, out‐of‐hospital extracorporeal membrane oxygen is a novel intervention that could benefit the most severe shock cases. 17
In conclusion, in this national series, 1 of every 100 EMS encounters involved shock. These findings highlight the current course and care of shock in the out‐of‐hospital setting. Additional studies are needed to evaluate innovative approaches to out‐of‐hospital shock care.
CONFLICTS OF INTEREST
Dr. Blaivas was the supervising editor of this article. Dr. Wang did not participate in the review process or editorial decision to accept the manuscript.
AUTHOR CONTRIBUTIONS
TPG and HEW conceived and designed the study. TPG, HKC, RPC and HEW were involved in acquisition of data, and analysis of data. All authors contributed to the interpretation of data. TPG and HEW drafted the manuscript. All authors revised the paper critically for important intellectual content. All authors gave final approval of the version to be published. Dr. Wang takes responsibility for the paper as a whole.
Biography
Timothy George is a medical student at McGovern Medical School in Houston, Texas. He holds a Bachelor of Music in Piano Performance from the University of Texas at Austin.

George TP, Chan HK, Crowe RP, et al. Clinical characteristics and course of out‐of‐hospital shock in a national emergency medical services cohort. JACEP Open. 2020;1:432–439. 10.1002/emp2.12090
Funding information: This work was funded by the Dean's Office of McGovern Medical School and its Department of Emergency Medicine.
Supervising Editor: Juan A. March, MD.
REFERENCES
- 1. Wacker DA, Winters ME. Shock. Emerg Med Clin North Am. 2014;32:747‐758. [DOI] [PubMed] [Google Scholar]
- 2. Holler JG, Bech CN, Henriksen DP, Mikkelsen S, Pedersen C, Lassen AT. Nontraumatic hypotension and shock in the emergency department and the prehospital setting, prevalence, etiology, and mortality: a systematic review. PLoS One. 2015;10:e0119331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang HE, Shapiro NI, Yealy DM. Characteristics of out‐of‐hospital shock care. Crit Care Med. 2011;39:2431‐2439. [DOI] [PubMed] [Google Scholar]
- 4. Pearse RM. Extending the role of lactate measurement into the prehospital environment. Crit Care. 2009;13:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. St John AE, McCoy AM, Moyes AG, Guyette FX, Bulger EM, Sayre MR. Prehospital lactate predicts need for resuscitative care in non‐hypotensive trauma patients. West J Emerg Med. 2018;19:224‐231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Seymour CW, Cooke CR, Mikkelsen ME, et al. Out‐of‐hospital fluid in severe sepsis: effect on early resuscitation in the emergency department. Prehosp Emerg Care. 2010;14:145‐152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brown RM, Semler MW. Fluid management in sepsis. J Intensive Care Med. 2019;34:364‐373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Self WH, Semler MW, Bellomo R, et al. Liberal versus restrictive intravenous fluid therapy for early septic shock: rationale for a randomized trial. Ann Emerg Med. 2018;72:457‐466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sperry JL, Guyette FX, Adams PW. Prehospital plasma during air medical transport in trauma patients. N Engl J Med. 2018;379:1783. [DOI] [PubMed] [Google Scholar]
- 10. Rehn M, Weaver A, Brohi K, et al. Effect of prehospital red blood cell transfusion on mortality and time of death in civilian trauma patients. Shock. 2019;51:284‐288. [DOI] [PubMed] [Google Scholar]
- 11. Seymour CW, Cooke CR, Heckbert SR, et al. Prehospital intravenous access and fluid resuscitation in severe sepsis: an observational cohort study. Crit Care. 2014;18:533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Seymour CW, Rea TD, Kahn JM, Walkey AJ, Yealy DM, Angus DC. Severe sepsis in pre‐hospital emergency care: analysis of incidence, care, and outcome. Am J Respir Crit Care Med. 2012;186:1264‐1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304‐377. [DOI] [PubMed] [Google Scholar]
- 14. van Diepen S, Katz JN, Albert NM, et al. Contemporary management of cardiogenic shock: a scientific statement From the American Heart Association. Circulation. 2017;136:e232‐e268. [DOI] [PubMed] [Google Scholar]
- 15. Sperry JL, Guyette FX, Brown JB, et al. Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock. N Engl J Med. 2018;379:315‐326. [DOI] [PubMed] [Google Scholar]
- 16. Murdock AD, Berseus O, Hervig T, Strandenes G, Lunde TH. Whole blood: the future of traumatic hemorrhagic shock resuscitation. Shock. 2014;41(suppl 1):62‐69. [DOI] [PubMed] [Google Scholar]
- 17. Singer B, Reynolds JC, Lockey DJ, O'Brien B. Pre‐hospital extra‐corporeal cardiopulmonary resuscitation. Scand J Trauma Resusc Emerg Med. 2018;26:21. [DOI] [PMC free article] [PubMed] [Google Scholar]


