Abstract
The coronavirus disease 2019 (COVID‐19) pandemic has rapidly evolved and now dominates the attention and full efforts of the emergency medicine community, both domestic and abroad. Seattle is the site of the initial diagnosed COVID‐19 cases and fatalities in the United States. We provide an overview of the system‐level response of 6 Seattle emergency departments and the Washington state chapter of the American College of Emergency Physicians (ACEP) to the COVID‐19 pandemic. Local efforts involved the spectrum of emergency response including on‐ and off‐site triage strategies, an approach to personal protective equipment, testing and reporting protocols, early treatments, communication strategies, the impact on front‐line providers, and ongoing work.
Keywords: coronavirus, COVID‐19, disaster medicine, emergency preparedness, pandemic, Seattle
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic first impacted the United States in the Seattle region of Washington State. Illness caused by a novel severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) had been previously reported in Wuhan, China, in December 2019. 1 COVID‐19 spread throughout China, South Korea, and Italy and then was recognized for the first time in the United States in a skilled nursing facility outside of Seattle in February 2020.
Our community's response to the pandemic required coordination between all aspects of the healthcare system, including emergency medical services (EMS), hospitals and health systems, outpatient clinical networks, healthcare coalitions, public health officials, and government leaders. The Washington chapter of the American College of Emergency Physicians (ACEP) created a group to facilitate communication and coordinate response by the Seattle emergency medicine community. In this report, we provide an overview of our early experience with COVID‐19 response at 6 hospitals in the Seattle region.
2. SETTING
Seattle is a metropolitan region of >2 million individuals. Health care in the region is provided by a network of hospitals affiliated with the University of Washington (UW) academic medical center, as well as several private non‐profit hospital chains, district hospitals, and the Department of Veterans Affairs. The Washington State Hospital Association (WSHA) lists 20 acute care hospitals in King County and 3 in Snohomish County.
Our report reflects the experiences at a cohort of 6 of these hospitals: EvergreenHealth Medical Center in Kirkland, Highline Medical Center—CHI Franciscan in Burien, Providence Regional Medical Center in Everett, Swedish Medical Center in Edmonds, Valley Medical Center—UW Medicine in Renton, and Virginia Mason Hospital and Medical Center in Seattle.
These hospitals represent 6 health systems, encompass 360,000 annual ED patients, and comprise >33% of the 4,900 inpatient beds in the region (Table 1 and Figure 1).
TABLE 1.
List of cohort hospitals
| Hospital | Health system | Location | Annual ED visits | Inpt beds | ICU beds |
|---|---|---|---|---|---|
| EvergreenHealth Medical Center | Evergreen | Kirkland | 57,000 | 318 | 20 |
| Highline Medical Center | CHI Franciscan | Burien | 55,000 | 124 | 10 |
| Providence Regional Medical Ctr | Providence | Everett | 90,000 | 591 | 48 |
| Swedish Medical Center | Swedish | Edmonds | 50,000 | 130 | 12 |
| Valley Medical Center—UW Med | Univ of WA | Renton | 84,000 | 310 | 30 |
| Virginia Mason Hospital | Virginia Mason | Seattle | 27,000 | 275 | 20 |
| 363,000 | 1748 | 140 |
ED, emergency department; ICU, intensive care unit; UW, University of Washington.
FIGURE 1.
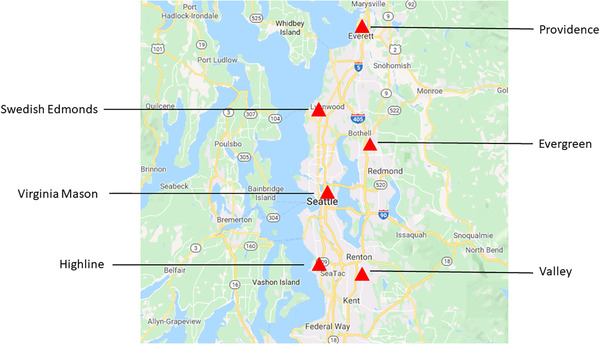
Geographic locations of cohort hospitals
3. CURRENT SITUATION
On January 20, 2020, the first patient in the United States was diagnosed with the novel coronavirus at 1 of the cohort hospitals. 2 , 3 On February 29, 2020, the first COVID‐19 death was reported at another cohort hospital; this case involved a resident from a skilled nursing facility. It was later recognized that 2 individuals previously died of COVID‐19 on February 26, 2020. At the time this report was written, March 23, 2020, our 2 counties have had 98 deaths and 1689 confirmed cases, and these numbers climb daily. 4
During this time, emergency departments (EDs) in our 2 counties have experienced an increase in respiratory cases with multiple ED patients testing positive for COVID‐19 daily. Crowding of EDs in our region has generally not occurred. Rather, our EDs have observed a 10%–20% decline in overall volume, and 1 ED reports a nearly 40% decline. We suspect this is due to coordinated messaging from local health jurisdictions, organizations such as WSHA, and public media directing patients to avoid EDs for less serious respiratory symptoms.5 Also, multiple health systems are expanding their telehealth capabilities, offering patients virtual care options and alternatives. Finally, perception exists among physicians that many patients are staying away from the EDs due to fears of being exposed to the virus during a visit.
Though our ED volumes have declined, our inpatient capacity is stretched. Hospitals in the Pacific Northwest were already experiencing a high inpatient census, usually running close to or over capacity. One hospital reports all ventilators are currently being used with no additional units available. Our hospital systems have cancelled non‐critical surgical cases to optimize current capacity as part of surge planning. We are also noting contraction of the available blood supply. While at this point most of our institutions maintain some intensive care unit (ICU) and inpatient bed capacity, due in part to rapid efforts to expand critical care beds, we expect conditions to change in the next few days to weeks.
4. TRIAGE
Triage processes vary across institutions, but all have set up separate waiting areas for potential respiratory patients. When presenting to the hospital, patients are typically greeted by a clinical staff member in personal protective equipment (PPE). The exact PPE varies by institution; some are in mask and gloves; others also add full gown and goggles or facemask. Initial screening focuses on the presence of respiratory complaints. Patients with respiratory symptoms are masked immediately upon arrival and asked to clean their hands with alcohol‐based hand sanitizer. Some facilities report that unattended masks and alcohol‐based hand sanitizers stationed at the public entrance are being stolen, so these supplies have been removed from patient‐facing areas and are distributed individually to patients by staff.
Several EDs have set up or are in the process of setting up tents for surge capacity of patients with respiratory complaints. Many EDs are developing sub‐waiting rooms for respiratory isolation, walling off areas, and installing fans to create a negative pressure environment. There is discussion about evaluating stable patients in their vehicles, but none of our institutions have yet developed robust protocols for vehicle‐based evaluations. Some hospitals are advancing screening for EMS patients outside the building in their ambulance bays. As the number of infected, critically ill, and at‐risk residents increased during the initial outbreak at a local long‐term care facility, the 2‐county designated disaster medical coordination centers (DMCC) collaborated to triage, track, and distribute patients via EMS and private ambulance services to multiple EDs across both counties.
In some cases, only a limited in‐person exam is performed and much of the history is via telephone between the patient in their ED room and the physician present outside the room. Some EDs are setting up video devices to augment a focused in‐person evaluation. None of our EDs have implemented a sole telemedicine process for patients who present on hospital grounds, and everyone receives an in‐person assessment as part of their Emergency Medical Treatment and Labor Act (EMTALA)‐associated medical screening exam (Figures 2 and 3).
FIGURE 2.
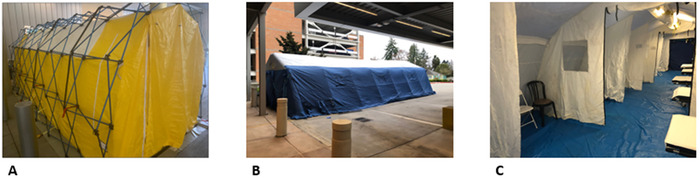
Tents for patients with respiratory symptoms. (A) Exterior view of tent in Virginia Mason Hospital and Medical Center parking garage. (B) Exterior view of tent at Providence Regional Medical Center Everett. (C) Interior view of tent at Providence Regional Medical Center Everett
FIGURE 3.
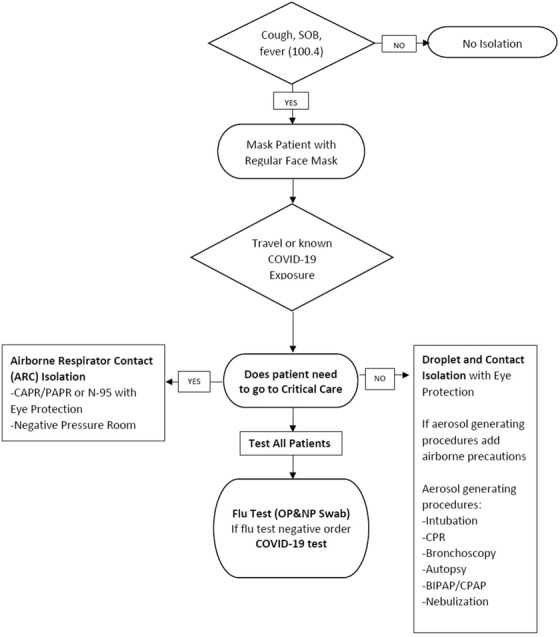
Sample triage algorithm. CAPR, controlled air purifying respirators; OP, oropharyngeal; NP, nasopharyngeal; PAPR, powered air purifying respirators; SOB, shortness of breath
5. PERSONAL PROTECTIVE EQUIPMENT AND ISOLATION MEASURES
Personal protection equipment guidelines have changed rapidly based on local institutional supply and are continuing to change. In general, due to dwindling PPE supplies, our usage transitioned to the World Health Organization (WHO) guidelines of contact/droplet precautions, reserving airborne precautions for high risk/aerosolizing procedures such as intubation, high‐flow nasal cannula, bilevel ventilation, and nebulized treatments. 6 In general, however, high‐risk procedures are avoided in all respiratory patients when possible. Our current PPE practice is in contrast to much of the rest of the country, and to the CDC guidelines, which had been recommending broad airborne precautions. 7
We wear surgical masks rather than respirators for typical patient encounters, in addition to face shields, gowns, and gloves. If aerosolizing procedures are being performed (eg, endotracheal intubation), our staff wear respirators such as N95 masks, controlled air purifying respirators (CAPRs), or powered air purifying respirators (PAPRs). During nasal swab collection, most hospitals require donning a respirator, though at least 1 hospital currently only requires surgical masks and eye protection. One hospital has directed all intubations to be performed with PAPRs and not N95s in order to minimize particulate spread to hair and neck associated with intubation. Two hospitals have developed a “Code COVID” for patients requiring intubation that prompts the involvement of an anesthesiologist with CAPR/PAPR and fiberoptic scope.
Consistent with the WHO guidelines, most patients are treated in closed rooms but not necessarily airborne infection isolation rooms (AIIR)/negative pressure rooms.
Maintaining and communicating PPE standards remains a major issue. We are experiencing shortages of PPE, forcing us to ration N95 masks, and reuse disposable face shields after cleaning. Some staff use CAPRs and PAPRs in order to conserve disposable PPE.
Incertitude exists as when to discontinue droplet and contact precautions for patients with respiratory symptoms who are deemed at low risk for coronavirus infection. In addition, conflicting PPE guidelines between the WHO and CDC have created confusion. Complicating the situation is that some medical staff have increased vulnerability to COVID due to age or other chronic health conditions. The varying quarantining practices and reports of hospitalization of healthcare workers have added to existing consternation. Alignment among all the hospitals in the region to uniformly adopt WHO guidelines over CDC guidelines has helped standardize the approach.
6. TESTING
Initially, testing was only performed on hospitalized patients or symptomatic patients with known exposures due to the lack of approved laboratory sites and capacity. Now that commercial testing is increasingly available, we are beginning community‐based testing. Protocols are determined at each hospital, but no longer require notifying the Department of Health (DOH) prior to ordering a COVID‐19 test or a confirmatory test by the Washington State Public Health Laboratory before reporting. As a result, and with the availability of a combination of UW and commercial laboratories, turnaround times have reduced from >48 to ≈12 hours. Discharged patients awaiting test results received preprinted instructions based on CDC and local DOH guidelines with self‐quarantine instructions and the contact phone numbers for the DOH or local follow‐up clinics.
The workflows for notifying discharged patients of initial COVID‐19 results parallel existing processes for reporting sexually transmitted disease or culture results. Each ED has a designated person (eg, an emergency physician, physician assistant, or infection control nurse) in charge of receiving the results, contacting patients with positive cases, and DOH notification. Because of patients’ concerns and potential lost work time associated with the infection, some EDs are also contacting patients with negative COVID‐19 test results. The workflow differs across hospitals with some utilizing the ED for callbacks and others using designated staff (eg, infection control or nursing supervisors). As the crisis has evolved, systems have set up more consistent processes to notify all discharged patients of COVID‐19 test results, though the specifics differ from hospital to hospital.
At least 3 hospitals have set up drive‐by COVID‐19 testing sites, with one site being available to healthcare workers as well as patients referred from ambulatory clinics. These sites are operating with certain capacity restrictions and several require an appointment or scheduled visits process. We anticipate the number of these alternate screening sites to grow significantly in the coming weeks.
The UW Reference Laboratory Services reports that about 5%–10% of tested specimens are positive for COVID‐19, and one of our EDs reports numbers closer to 15%. As of March 23, 2020, of 31,712 COVID‐19 tests performed in Washington State, 2221 (7.0%) have been positive (Table 2).
TABLE 2.
2019 Novel coronavirus (COVID‐19) cases and deaths in Washington State as of March 23, 2020
| Area | Positive/confirmed cases | Deaths |
|---|---|---|
| King County | 1170 | 87 |
| Snohomish County | 519 | 11 |
| Washington State | 2221 | 110 |
Source: Washington Department of Health 2019 Novel Coronavirus Outbreak (COVID‐19).
However, we have observed anecdotal cases in which a patient's initial test was negative but a subsequent test was positive. More accurate understanding of the epidemiology and actual community prevalence is evolving. Our anecdotal experience from discharged follow‐ups of COVID‐19‐positive patients is that most report symptomatic improvement. Unfortunately, this has not been the case for many admitted patients, some of whom have experienced prolonged mechanical ventilation. 8
7. TREATMENT
The treatment of COVID‐19 is constantly evolving. Within the first 2 weeks, there was limited information regarding the optimal care for admitted patients. While the vast majority of COVID‐19 patients are managed in the outpatient setting, many have been hospitalized. We have been limiting non‐invasive positive pressure ventilation (NIPPV) given the risk of aerosolization, although some institutions experiencing ventilator shortages are now encouraging use of NIPPV. Intubations are done typically using CAPR or PAPR and ideally in an AIIR/negative pressure room. Dozens of individuals have been intubated, typically older patients with comorbidities. However, there have been individuals in their 30s–40s without significant underlying disease who have also been intubated. Our experience so far with mechanical ventilation is that it appears to be prolonged, with only a small number of patients having been extubated at the time of this writing.
In some cases, we are using remdesivir on a compassionate‐use protocol, though we understand this protocol will be modified in favor of clinical trials. Some facilities are also participating in a clinical trial, enrolling all qualified, consenting admissions into a 5‐day and 10‐day arm trial of remdesivir (no placebo). We are not starting ED patients on chloroquine or antivirals.
8. WORK RESTRICTIONS
At least 2 Seattle emergency physicians have been infected by COVID‐19; it has not yet been ascertained if the infections were work‐ or community‐related exposure. One has recovered without major complication. Several additional physicians were placed on work restrictions after confirmed COVID‐19 exposure. Once these physicians tested negative for COVID‐19, they were allowed to return to work while wearing a mask and being monitored for symptoms. These individuals were not required to refrain from work for 14 days as had been recommended by the CDC at the time.
As this event continues, further physician and healthcare staff attrition is expected because of infection, quarantine protocols, fatigue, and absenteeism. Our workforce has also been impacted by childcare challenges as school are closed. Some hospitals are implementing or expanding their own childcare service programs for staff. The Washington State Governor has authorized the state DOH to activate and further enroll emergency volunteer practitioners through the Uniform Emergency Volunteer Health Practitioner Act.
9. COMMUNICATION
ED staff were faced with a daily deluge of information from a myriad of sources, such as friends, colleagues, social media, press, employers, healthcare systems, and government agencies. Separate communications about new protocols from the ED medical director, the hospital, and the healthcare systems sometimes conflicted, and their frequent updates were difficult for individual physicians to track. Password‐protected postings on health systems’ internal websites were difficult to access by physicians not employed by the hospital, as many were unfamiliar with those online environments and unaware of their login credentials. It took time and commitment to eliminate the panic chatter and create clear, once‐daily “sources of truth” that staff could rely on for up‐to‐date information and guidelines. For Seattle, the Northwest Healthcare Response Network (NWHRN), a regional healthcare coalition, has hosted a daily conference call that facilitates discussion of new developments, greater uniformity of messaging, and responses by ED directors, hospitals, hospitals, and emergency managers.
10. FUTURE PLANNING AND QUESTIONS
Based on the experiences in Italy, we are concerned about what might transpire over the next several weeks. Our inpatient capacity is tight, elective surgical cases have been canceled, and some chemotherapy treatments requiring hospitalization are postponed. One hospital has completed an improvised installation of fans in windows to convert an inpatient unit to negative pressure. Another hospital is building out more ICU beds in its labor and delivery unit. Further critical care bed construction is anticipated.
While only 1 hospital has run out of ventilators, other institutions anticipate similar shortages. The NWHRN has been facilitating scarce resource utilization discussions and revising its crisis standards of care algorithms that have been in development over the past several years. 9 Many sites are actively engaging their palliative care teams, as well as reaching out to skilled nursing, long‐term care, behavioral health, and correctional facilities to determine transport guidelines.
Now that testing is becoming more available, EDs are receiving symptomatic, highly suspected patients from referring facilities, who have in turn declined to accept patients back from the hospital until negative COVID‐19 results are available. As the testing process can still take up to several days, our ED and inpatient units are boarding mildly symptomatic patients who do not require an inpatient level of care while they await confirmatory results. The requirement for negative COVID‐19 screening has become a bottleneck for inpatient disposition and, in response, hospital systems are engaging with long‐term care facilities proactively with on‐site testing, triage strategies, cohort processes, and training to mitigate spread to and within this vulnerable population and improve patient flows.
11. LESSONS LEARNED
The transmissibility and mortality related to COVID‐19 requires a significant re‐tooling of ED processes to deal with endemic disease. Our hospitals have adapted to shifting guidelines and confronted common limitations. Our early experience has identified several important lessons:
Triage: For EDs, appropriate separation of low‐ and high‐risk patients in a space that will not jeopardize other patients and staff is challenging. An example is a pre‐ED triage tent with staff in PPE, able to do swabs and risk stratify patients. To expand patient access and reduce unnecessary ED congestion, protocols can be distributed to clinics regarding patient dispositions, such as who is eligible for home monitoring versus should be referred to EDs.
Testing: Consistent local testing pathways, from sample acquisition to receipt of confirmed results, are critical to efficient patient disposition and reporting. Influential factors include sampling protocols, availability of testing media, access to certified laboratories, processing capacity and time, and reporting of results.
PPE: Maintaining adequate supplies that support adopted clear and consistent guidelines is an obvious necessity. Monitoring burn rates and adjusting orders as guidelines evolve will reassure and better protect staff and promote compliance.
Treatment: Our hospitals have converted and designated units dedicated for COVID‐19 patients. The creation of designated care areas should be an early consideration along with the development of contingency expansion plans. Several hospitals have also created “Code COVID” teams who can rapidly respond with appropriate PPE and specialized equipment for patients requiring intubation.
Disposition: Clear guidance by public health regarding whom to test, self‐isolate, and admit will reduce confusion, promote judicious use of limited resources, and facilitate ED flow. Public health also served as a needed resource when long‐term care, psychiatric, dialysis, and shelter facilities declined to accept ED and hospitalized patients who were ready to be discharged until they tested negative.
Communication: Establishing focused communication from a clear chain of command is vital to share important updates. Hospitals should avoid multiple sources of information streams and funnel information through a curated mechanism, such as a single daily email update, that is accessible to personnel who are not directly employed by the hospital.
Collaboration: The COVID‐19 event accelerated and erupted when an outbreak occurred in a skilled nursing facility, creating a hot spot of severe disease. The coordination between the King and Snohomish County DMCCs provided a central command and control to distribute critically ill patients and greatly reduced the burden on individual hospitals.
Staff safety: Guidelines on quarantine of healthcare personnel have changed over the course of the crisis and vary by institution. A clear and uniform policy for what to do when a staff member has been exposed, tests positive, and exhibits symptoms will mitigate stress, and conserve scheduling and sustained sufficient staffing. We found it necessary to have backup staffing readily available when personnel are notified, quarantined, or become symptomatic on short notice.
12. CONCLUSION
We know that we will get through this. While we have certainly seen concern and anxiety in our patients and staff, we have also seen tremendous resolve and courage. We are grateful to our international colleagues who have shared their knowledge and insight, proud of our partners on the front lines of this event, and appreciate the opportunity to share our experiences and lessons learned with those who will also potentially face this challenge and future events.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
Miller GA, Buck CR, Kang CS, et al. COVID‐19 in Seattle—Early lessons learned. JACEP Open 2020;1:85–91. 10.1002/emp2.12064
Supervising Editor: Henry E. Wang, MD, MS.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
REFERENCES
- 1. Wu Z, McGoogan J. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID‐1) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. Published online February 24, 2020. 10.1001/jama/2020.2648. [DOI] [PubMed] [Google Scholar]
- 2. Holshue ML, DeBolt C, Lindquist S et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929‐936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McMichael TM, Clark S, Pogosjans S etal. COVID‐19 in a long‐term care facility—King County, Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly Rep. ePub: 18 March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Washington State Department of Health COVID‐19. https://www.doh.wa.gov/Emergencies/Coronavirus. Accessed March 13, 2020.
- 5. Washington State Hospital Association Coronavirus information for the public and media. https://www.wsha.org/for-patients/coronavirus/coronavirus-information-for-the-public-and-media/ Accessed March 14, 2020.
- 6. Rational Use of Personal Protective Equipment for Coronavirus Disease 2019 (COVID‐19)— Interim Guidance February 27, 2020. World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf. Accessed March 20, 2020.
- 7. Interim infection prevention and control recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID‐19) in Healthcare Settings https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Finfection-control.html. Accessed March 20, 2020.
- 8. Lai C, Shih TP, Ko WC et al. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS‐CoV‐2) and Coronavirus Disease‐2019 (COVID‐19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Scarce resource management and crisis standards of care overview and Materials. Northwest Healthcare Response Network. https://nwhrn.org/scarce-resource-management-and-crisis-standards-of-care-overview-and-materials/ Accessed March 18, 2020


