Abstract
E‐cigarette or vaping product‐use‐associated lung injury is a disease process obtained from smoke inhalation with electronic delivery systems and typically presents with shortness of breath, cough, and fever, not unlike pneumonia. Our patient presented with similar symptoms, and his case went unrecognized through several emergency department visits. The pathophysiology is similar to chemical pneumonitis and can cause significant morbidity and mortality, particularly when it goes unrecognized. It often presents with a pneumonia‐like picture and may be treated as such. The distinguishing and controversial treatment for this disease is systemic glucocorticoids, which are not often given in pneumonia. This case is unique for the significant leukocytosis found on laboratory testing and profound weight loss associated with his course of illness. Emergency medicine providers should be vigilant in recognizing this illness to prevent progression of this disease.
Keywords: E‐cigarette, EVALI, leukocytosis, vaping
1. INTRODUCTION
A 20‐year‐old male with no significant past medical history presented to the emergency department (ED) for chest pain, fever, and shortness of breath. For 2 weeks prior to presentation, he had a coarse‐sounding cough productive of yellow sputum, intermittent fever with a maximum temperature of 103°F, diarrhea, nausea, and a >20 lb weight loss. He was initially evaluated at a local ED and was diagnosed with a viral illness. He failed to improve, and while visiting family in Illinois, he presented to an ED and was hospitalized with the diagnosis of bilateral pneumonia that was confirmed by computed tomography (CT) scan of the chest. He was admitted for 4 days on intravenous antibiotics (ceftriaxone, levofloxacin, and azithromycin), but after he failed to improve, he left against medical advice and returned home, where he presented same day from outside hospital discharge to our ED.
On arrival to our ED, he denied any history of intravenous drug use and stated he had recently been tested for hepatitis and HIV with negative results. He denied sick contacts and tick exposures. He endorsed smoking marijuana and tobacco.
On physical exam, he was alert but ill appearing. He had an initial blood pressure of 99/64, a heart rate of 108, had an oxygen saturation of 95% on room air, and a temperature of 98.3°F. He was tachycardic, but had a normal S1, S2 without additional heart sounds, and had crackles in the lower lobes bilaterally without rhonchi or wheezing. The remainder of his exam was unremarkable.
Throughout his first few hours in the emergency department, he desaturated to the low 90s while talking or moving and required 2 L of oxygen via nasal cannula. His blood work was remarkable for a WBC of 44.8 × 10(3)/µL, platelet count of 713 × 10(3)/µL, aspartate aminotransferase (AST) of 161 units/L, and alanine aminotransferase (ALT) of 254 units/L. His lactate was 1.6 mmol/L. Blood and sputum cultures were drawn.
A chest x‐ray was obtained (Figure 1) and was read as “radiographic appearance.” He was started on broad spectrum antibiotics and admitted to the medicine service.
Figure 1.
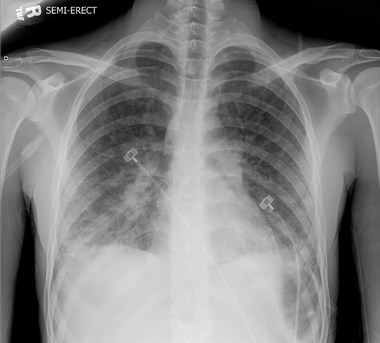
CXR showing bilateral patchy airspace opacities in the mid and lower lung zones concerning for multifocal pneumonia
The admitting service obtained a computed tomography angiography (CTA) of the chest (Figure 2) to exclude pulmonary embolism and was read as "bilateral basilar dependent consolidations with diffuse patchy ground‐glass opacities and mild smooth septal thickening. There is subpleural sparing most apparent in the non‐dependent portions of the lungs," which is consistent with the bilateral infiltrates and ground‐glass opacities typically seen in e‐cigarette or vaping product‐use‐associated lung injury (EVALI).1
Figure 2.
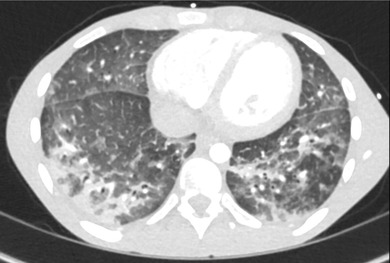
CTA chest showing bilateral basilar‐dependent consolidations with diffuse patchy ground‐glass opacities and mild smooth septal thickening
A pulmonary consult was obtained, and further history revealed that the patient began vaping cannabis oil (one cartridge per day on average) several months prior via a commercial device purchased in Tennessee approximately 1 month prior. The cartridges containing THC were reportedly given to him by a friend, and the purchased location was unknown. Three weeks prior to presentation to our hospital, he discontinued vaping due to the development of symptoms that prompted him to seek medical care.
With this additional history, the radiologist was able to confirm that the CTA chest was consistent with EVALI. This particular pattern on CT imaging of the chest is often seen in EVALI, but is not specific to this alone.
Inpatient bronchoscopy revealed “acute lung injury with collections of neutrophils. Vacuolated smoker's macrophages are also noted. There are no granulomas, vasculitis, viral inclusion, or foreign bodies. The differential includes infection versus vaping lung injury or both.”
Additional negative workup included strep/legionella antigens, HIV, antineutrophil cytoplasmic antibodies (ANCA), hepatitis panels, transthoracic echocardiogram, respiratory virus panel, and thyroid function studies. The bronchoalveolar lavage cultures obtained during his bronchoscopy also failed to yield an infectious cause of his symptoms.
After the bronchoscopy and biopsies were performed, the patient was started on 1 mg/kg of prednisone and trimethoprim‐sulfamethoxazole PO. The efficacy of systemic glucocorticoids in EVALI is unknown and has yet to be studied, but published case series cite they are frequently given (>90%).2 In 1 study of 5 patients, high dose intravenous methylprednisolone was given in critically ill patients with notable improvement 24–72 hours from initiation.3 Our patient improved significantly after the initiation of prednisone, coming off oxygen within 48 hours. He remains in the hospital system but has failed to appear for his scheduled follow‐up appointments.
EVALI has recently been identified as a disease process that has received significant media attention in the last few months. Its pathophysiology is similar to chemical pneumonitis, which has traditionally been seen in industrial workers and includes airway inflammation, edema, and hypoxemia. As of October 15, 2019, there have been 1479 cases of EVALI, and 33 deaths have been confirmed in 24 states.2 The degree of leukocytosis seen in this case (44,800) is markedly higher from the median WBC count of 15,900 seen in prior case reports (interquartile range [IQR] 12,300–18,100).1 It is unclear if this was due to the prolonged time from symptom onset to diagnosis, or a severe systemic inflammatory response syndrome due to pulmonary inflammation related to smoke/marijuana inhalation via electronic delivery systems. Smoke inhalation has been proven to cause activation of inflammatory interleukins and inflammatory polymorphonuclear neutrophils,4 and an already injured alveolar membrane may be more susceptible to damage from electronic delivery of nicotine and other substances. The patient did not receive steroids at the outside facility, eliminating that as a possible contributor to his leukocytosis so far outside the standard deviation. The combination of significant leukocytosis (>40,000/µL in the setting of bilateral pneumonia) should prompt the clinician to evaluate for other sources of inflammation.
The incidence of EVALI is rapidly expanding, because vaping is the most widely used form of tobacco among high school students,5 and the disease becomes more recognized by healthcare providers. Typical symptoms include cough, shortness of breath, fever, fatigue, nausea, and diarrhea. It is not clear whether there is a particular chemical that is causing the injury, whether it is the use of cannabinoids within the vaping device, or a byproduct of the vaping product itself. The lung injury that vaping causes has many different radiographic appearances, including acute eosinophilic pneumonia, organizing pneumonia, lipoid pneumonia, diffuse alveolar damage, diffuse alveolar hemorrhage, hypersensitivity pneumonitis, and acute respiratory distress syndrome.6 The only known treatment for the disease at this time is cessation of vaping, and there are promising case reports regarding systemic glucocorticoids without a formal recommendation.2, 3 It is currently a diagnosis of exclusion and should be applied only to those patients with the appropriate clinical context. No biomarker exists to confirm the diagnosis. Infection, autoimmune, and other inflammatory processes must be ruled out.
As EVALI becomes more widespread, it will be important for emergency physicians to take a thorough social history and to recognize the historical and radiologic features consistent with this disease process. Prompt recognition is important, because the disease often progresses in severity quite rapidly. Thirty‐two percent of patients in a recent report required intubation and mechanical ventilation.1 The current treatment for EVALI includes supplemental oxygen and systemic glucocorticoids for worsening hypoxemia. Inpatient treatment should be considered in patients with a known history of electronic nicotine‐marijuana delivery systems.
Works K, Stack L. E‐cigarette or vaping product‐use‐associated lung injury (EVALI): A case report of a pneumonia mimic with severe leukocytosis and weight loss. JACEP Open. 2020;1:46–48. 10.1002/emp2.12002
[Correction added on 20 January 2020, after first online publication: the author degrees are added to author byline.]
REFERENCES
- 1. Layden JE, Ghinai I, Pray I, et al. Pulmonary illness related to e‐cigarette use in Illinois and Wisconsin—preliminary report. N Engl J Med. 2019. 10.1056/NEJMoa1911614 [DOI] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention . Outbreak of Lung Injury Associated with the Use of E‐Cigarette, or Vaping, Products . 2019. Available at: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html
- 3. Davidson K, Brancato A, Heetderks P, et al. Outbreak of electronic‐cigarette‐associated acute lipoid pneumonia–North Carolina, July‐August 2019. MMWR Morb Mortal Wkly Rep. 2019;68(36):784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhou M, He JS, Li Q, et al. Pulmonary immune responses to acute lung injury following smoke inhalation and it's mechanisms. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2007;19(4):209‐213. [PubMed] [Google Scholar]
- 5. Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the field: use of electronic cigarettes and any tobacco product among middle and high school students–United States, 2011‐2018. MMWR Morb Mortal Wkly Rep. 2018;67(45):1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Christiani DC. Vaping‐induced lung injury. N Engl J Med. 2019. 10.1056/NEJMe1912032 [DOI] [PubMed] [Google Scholar]


