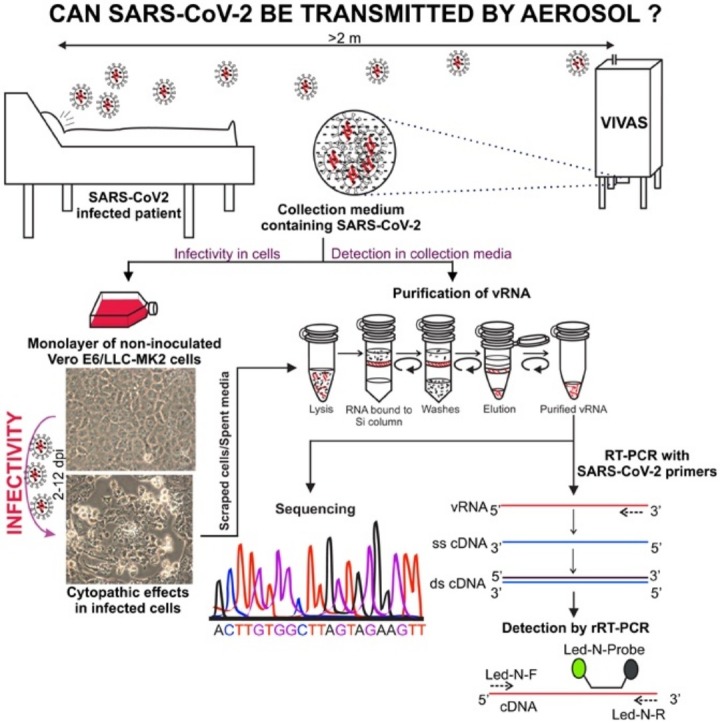
Graphical abstract
Abstract
Objectives
Because the detection of SARS-CoV-2 RNA in aerosols but failure to isolate viable (infectious) virus are commonly reported, there is substantial controversy whether severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can be transmitted through aerosols. This conundrum occurs because common air samplers can inactivate virions through their harsh collection processes. We sought to resolve the question whether viable SARS-CoV-2 can occur in aerosols using VIVAS air samplers that operate on a gentle water vapor condensation principle.
Methods
Air samples collected in the hospital room of two coronavirus disease-2019 (COVID-19) patients, one ready for discharge and the other newly admitted, were subjected to RT-qPCR and virus culture. The genomes of the SARS-CoV-2 collected from the air and isolated in cell culture were sequenced.
Results
Viable SARS-CoV-2 was isolated from air samples collected 2 to 4.8 m away from the patients. The genome sequence of the SARS-CoV-2 strain isolated from the material collected by the air samplers was identical to that isolated from the newly admitted patient. Estimates of viable viral concentrations ranged from 6 to 74 TCID50 units/L of air.
Conclusions
Patients with respiratory manifestations of COVID-19 produce aerosols in the absence of aerosol-generating procedures that contain viable SARS-CoV-2, and these aerosols may serve as a source of transmission of the virus.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), genus Betacoronavirus, subgenus Sarbecovirus, family Coronaviridae, is a positive-polarity single-stranded RNA virus that probably originated in bats (Andersen et al., 2020, Lu et al., 2020, Gorbalenya et al., 2020) and is the causative agent of coronavirus disease of 2019 (COVID-19) (Li et al., 2020). The dynamics of the COVID-19 pandemic have proven to be complex. Many challenges remain pertaining to a better understanding of the epidemiology, pathology, and transmission of COVID-19. For example, the clinical manifestations of COVID-19 range from an asymptomatic infection, mild respiratory illness to pneumonia, respiratory failure, multiorgan failure, and death (Guan et al., 2020, Jiang et al., 2020, Zhu et al., 2020). Diarrhea due to gastrointestinal infection can also occur, and in vitro modeling suggests that the virus infects human gut enterocytes (Lamers et al., 2020). Moreover, SARS-CoV-2 RNA can be found in rectal swabs and fecal aerosols, even after nasopharyngeal testing has turned negative (Liu et al., 2020, Wang et al., 2020, Holshue et al., 2020, Xiao et al., 2020), suggesting that a fecal–oral transmission route may be possible.
To date, there has been a strong emphasis on the role of respiratory droplets and fomites in the transmission of SARS-CoV-2 (WHO, 2020, CDC, 2020). Yet, SARS-CoV-2 does not appear to be exclusively inhaled as a droplet, and epidemiological data are consistent with aerosol transmission of SARS-CoV-2 (Hamner et al., 2020, Morawska and Cao, 2020, Jayaweera et al., 2020, Wang and Du, 2020, Fineberg, 2020). Furthermore, SARS-CoV-2 genomic RNA has been detected in airborne material collected by air samplers positioned distal to COVID-19 patients (Liu et al., 2020, Guo et al., 2020, Santarpia et al., 2020, Chia et al., 2020). Any respiratory virus that can survive aerosolization poses an inhalation biohazard risk, and van Doremalen et al. (2020) experimentally generated aerosol particles with SARS-CoV-2 and found that the virus remained viable during a three-hour testing period. More recently, Fears et al. (2020) reported that the virus retained infectivity and integrity for up to 16 h in laboratory-created respirable-sized aerosols. Nevertheless, finding virus RNA in material collected by an air sampler may not correlate with risk. Indeed, the air we breathe is full of viruses (animal, plant, bacterial, human, etc.); yet, a large proportion of the viruses in air are nonviable due to UV inactivation, drying, etc., and nonviable viruses cannot cause illnesses. Because efforts to isolate virus in cell cultures in the aforementioned air sampling studies in hospital wards were not made (Guo et al., 2020, Chia et al., 2020), or failed when they were attempted due to overgrowth by faster replicating respiratory viruses (Lednicky et al., 2020), and so far only one has provided evidence of virus isolation (Santarpia et al., 2020), uncertainties about the role of aerosols in COVID-19 transmission remain.
It is well known that virus particles collected by various air samplers become inactivated during the air sampling process (Pan et al., 2019), and if such is the case for SARS-CoV-2, this partly explains why it has been difficult to prove that SARS-CoV-2 collected from aerosols is viable. Because, we previously collected SARS-CoV-2 from the air of a respiratory illness ward within a clinic but were unable to isolate the virus in cell cultures due to out-competition by other respiratory viruses (Lednicky et al., 2020), we sought to perform air sampling tests in a hospital room reserved for COVID-19 patients, to lessen the probability of collecting other airborne human respiratory viruses. We thus collected aerosols containing SARS-CoV-2 in a room housing COVID-19 patients using our VIVAS air samplers that collect virus particles without damaging them, thus conserving their viability. These samplers operate using a water vapor condensation mechanism (Lednicky et al., 2016, Pan et al., 2017).
Air samplings were performed at the University of Florida Health (UF Health) Shands Hospital, which is a 1,050-bed teaching hospital situated in Gainesville, Florida. As of July 10, 2020, >200 patients have been treated at the hospital for COVID-19. The current study was conducted as part of ongoing environmental investigations by the UF Health infection control group, to assess possible healthcare worker exposure to SARS-CoV-2.
Methods
Additional details are provided in the Supplementary file that accompanies this article. An abbreviated description of the methods used for this work is provided below:
Patients
Patient 1 had coronary artery disease and other comorbidities, and after respiratory illness of two days duration, the patient was transferred from a long-term care facility for COVID-19 treatment in the evening before our air sampling tests were initiated. On admission, a nasopharyngeal (NP) swab from the patient was real-time reverse-transcription polymerase chain reaction (rRT-PCR) positive for SARS-CoV-2 RNA (Cq = 32). Patient 2 had been admitted four days before the air sampling tests with a mid-brain stroke; the patient had a positive NP swab test for SARS-CoV-2 on admission, but a repeat test was negative, and the patient was in the process of being discharged at the time the air sampling was being done. Both patients provided written consent for this study.
Hospital room
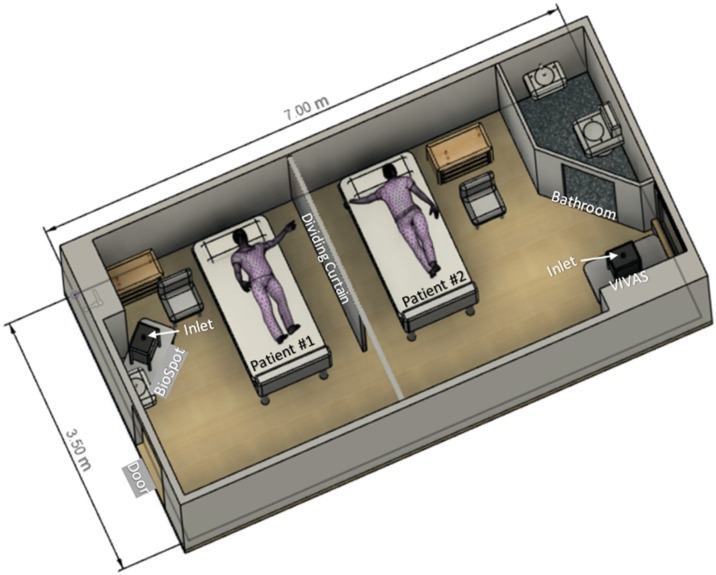
Air samples were collected in a room that was part of a designated COVID-19 ward (Figure 1 ). The room had six air changes per hour and the exhaust air underwent triple filter treatment (minimum efficiency reporting value 14, 75%-85% efficiency for 0.3 μm particles), coil condensation (to remove moisture), and UV-C irradiation before recycling 90% of the treated air back into the room.
Figure 1.
A schematic diagram of room with the depiction of patient bed and air sampler locations.
Air samplers and sampling parameters
Three serial 3-h air samplings were performed using our prototype VIVAS air sampler (Lednicky et al., 2020, Lednicky et al., 2016, Pan et al., 2017) and a BioSpot-VIVAS BSS300P, which is a commercial version of the VIVAS (available from Aerosol Devices Inc., Ft. Collins, CO). These samplers collect airborne particles by using a water vapor condensation method (Lednicky et al., 2020, Lednicky et al., 2016, Pan et al., 2017). Two samplers were used so that air could be collected/sampled at different sites of the same room during a given air sampling period. For each sampler, the second of the three samplings was performed with a high-efficiency particulate arrestance (HEPA) filter affixed to the inlet tube, a process we implement to reveal whether virus detected in consecutive samplings reflect true collection and not the detection of residual virus within the collector. The air samplers were stationed from 2 to 4.8 m away from the patients (Figure 1).
Detection of SARS-CoV-2 genomic RNA (vRNA) in collection media
vRNA was extracted from virions in collection media and purified by using a QIAamp Viral RNA Mini Kit (Qiagen, Valencia, CA, USA). Twenty-five μL (final volume) rRT-PCR tests were performed in a BioRad CFX96 Touch Real-Time PCR Detection System using 5 μL of purified vRNA and rRT-PCR primers and the probe listed in Table 1 , which detects a section of the SARS-CoV-2 N-gene (Lednicky et al., 2020). The N-gene rRT-PCR assay that was used was part of a dual (N- and RdRp-gene) rRT-PCR assay designed by J. Lednicky and does not detect common human alpha- or beta-coronaviruses. Using this particular N-gene rRT-PCR detection system, the limit of detection is about 1.5 SARS-CoV-2 genome equivalents per 25 μL rRT-PCR assay.
Table 1.
SARS-CoV-2 N-gene rRT-PCR primers and probe.
| Primer/probe name | Description | Oligonucleotide sequence (5’ to 3’) | Label |
|---|---|---|---|
| Led-N-F | SARS CoV-2 N Forward Primer | 5’-GGGAGCAGAGGCGGCAGTCAAG-3’ | None |
| Led-N-R | SARS CoV-2 N Reverse Primer | 5’-CATCACCGCCATTGCCAGCCATTC-3’ | None |
| Led-N-Probea | SARS CoV-2 N Probe | 5’ FAM-CCTCATCACGTAGTCGCAACAGTTC- BHQ1-3’ | FAM, BHQ1 |
This TaqMan® probe is 5'-end labeled with the reporter molecule 6-carboxyfluorescein (FAM) and with quencher Black Hole Quencher 1 (BHQ-1) at the 3'- end.
Cell lines for virus isolation
Cell lines used for the isolation of SARS-CoV-2 were obtained from the American Type Culture Collection (ATCC) and consisted of LLC-MK2 (Rhesus monkey kidney cells, catalog no. ATCC CCL-7) and Vero E6 cells (African green monkey kidney cells, catalog no. ATCC CRL-1586).
Isolation of virus in cultured cells
Cells grown as monolayers in a T-25 flask (growing surface 25 cm2) were inoculated when they were at 80% of confluency. First, aliquots (100 μL) of the concentrated air sampler collection media were filtered through a sterile 0.45-μm pore size PVDV syringe-tip filter to remove bacterial and fungal cells and spores. Next, the spent LLC-MK2 and Vero E6 cell culture media were removed and replaced with 1 mL of cell culture medium and the cells inoculated with 50 μL of cell filtrate. When virus-induced cytopathic effects (CPE) were evident, the presence of SARS-CoV-2 was determined by rRT-PCR.
Quantification of SARS-CoV-2 genomes in sampled air
The number of viral genome equivalents present in each sample was estimated from the measured quantification cycle (Cq) values. To do so, a 6-log standard curve was run using 10-fold dilutions of a calibrated plasmid containing an insert of the SARS-CoV-2 N-gene that had been obtained from IDT Technologies, Inc. (Coralville, Iowa). The data were fitted using equation (eq.) 1:
Eq. 1. y = (log10GE)(a) + b, where y = Cq value, a = slope of the regression line, log10GE is the base 10 log genome equivalents, and b is the intercept of the regression line.
Sanger sequencing of SARS-CoV-2 genomes in material collected by air samplers
To obtain the virus consensus sequence prior to possible changes that might occur during the isolation of the virus in cell cultures, a direct sequencing approach was used. Because the amount of virus present in the samples was low and thus unsuitable for common next-generation sequencing approaches, Sanger sequencing based on a gene-walking approach with nonoverlapping primers was used to obtain the virus sequence (Lednicky et al., 2020).
Next-generation sequencing the genome of SARS-CoV-2 isolated from NP swab
The vRNA extracted from virions in spent Vero E6 cell culture medium served as a template to generate a cDNA library using a NEBNext Ultra II RNA Library Prep kit (New England Biolabs, Inc.). Sequencing was performed on an Illumina MiSeq sequencer using a 600-cycle v3 MiSeq Reagent kit. Following the removal of host sequences (Chlorocebus sabaeus; GenBank assembly accession number GCA_000409795.2) using Kraken 2 (wood et al., 2019), de novo assembly of paired-end reads was performed in SPAdes v3.13.0 with default parameters (Bankevich et al., 2012).
Results
SARS-CoV-2 genomic RNA (vRNA) was detected by real-time reverse transcriptase quantitative polymerase chain reaction (rRT-qPCR) in material collected by air samplings 1-1, 1-3, 2-1, and 2-3, which had been performed without a HEPA filter covering the inlet tube. In contrast, in the presence of a HEPA filter, no SARS-CoV-2 genomes were detected in air samplings 1-2 and 2-2 (Table 2 ).
Table 2.
Results of rRT-qPCR tests of materials collected by air samplers.
| Sample ID | Approx. distance (m) from head of patient 1b | Approx. distance (m) from head of patient 2b | rRT-qPCR test | Cq value | SARS-CoV-2 genome equivalents/25 μL rRT-PCR test | SARS-CoV-2 genome equivalents/L of air |
|---|---|---|---|---|---|---|
| 1-1 BioSpot | 2 | 4.6 | + | 36.02 | 2.82E+03 | 94 |
| 1-2 BioSpot + HEPA | 2 | 4.6 | - | - | - | - |
| 1-3 BioSpot | 2 | 0 (PDb) | + | 37.69 | 9.12E+02 | 30 |
| 2-1 VIVAS | 4.8 | 3 | + | 37.42 | 1.15E+03 | 44 |
| 2-2 VIVAS+ HEPA | 4.8 | 3 | - | - | - | - |
| 2-3 VIVAS | 4.8 | 0 (PDd) | + | 38.69 | 4.68E+02 | 16 |
| SARS-CoV-2 vRNA | N/Ac | N/A | + | 29.53 | 2.20E+05 | N/A |
| N-genea DNA control - 1 | N/A | N/A | + | 26.56 | 1.00E+06 | N/A |
| N-gene DNA control - 2 | N/A | N/A | + | 31.21 | 1.00E+05 | N/A |
| N-gene DNA control - 3 | N/A | N/A | + | 34.71 | 1.00E+04 | N/A |
| N-gene DNA control -4 | N/A | N/A | + | 37.74 | 1.00E+03 | N/A |
| N-gene DNA control - 5 | N/A | N/A | + | 40.41 | 1.00E+02 | N/A |
| N-gene DNA control - 6 | N/A | N/A | + | - | 1.00E+01 | N/A |
| Known positive (NP swabe) | N/A | N/A | + | 24.12 | 8.36E+06 | N/A |
| Negative (no RNA) control | N/A | N/A | N/A | - | 0 | N/A |
N-gene, N-gene plasmid (positive control template).
Distance from sampler inlet nozzle to patient’s head.
N/A, Not applicable.
PD, patient discharged.
NP, Nasopharyngeal swab from a person screened for SARS-CoV-2 at the UF EPI high-throughput COVID-19 research testing facility.
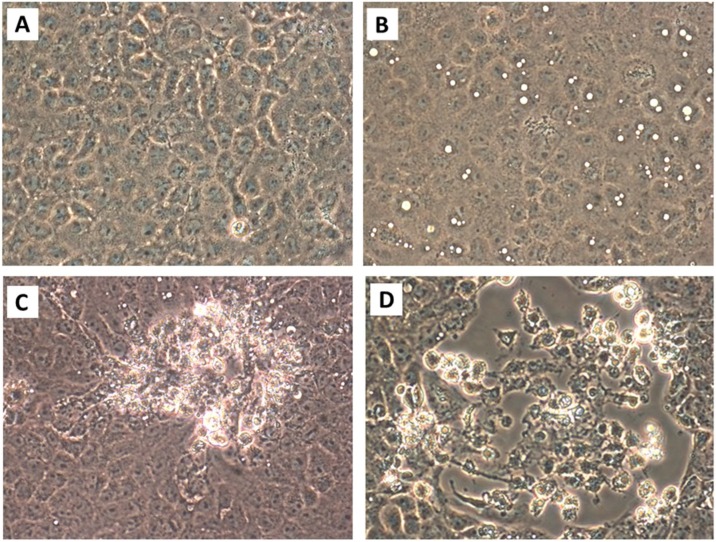
Virus-induced CPE were observed in LLC-MK2 and Vero E6 cells inoculated with material extruded from the NP specimen of patient 1 and from liquid collection media from air samples 1-1, 1-3, 2-1, and 2-3. Early CPE in both LLC-MK2 and Vero E6 cells consisted of the formation of cytoplasmic vacuoles that were apparent within 2 days postinoculation (dpi) of the cells with material extruded from the NP swab and 4 to 6 dpi with aliquots of the liquid collection media from the air samplers. At later times (4 days onwards after the inoculation of cell cultures with material from the NP swab, and 6 – 11 dpi of the cells with material collected by air samplers), rounding of the cells occurred in foci, followed by the detachment of the cells from the growing surface. Some of the rounded cells detached in clumps, and occasional small syncytia with 3-5 nuclei were observed. Apoptotic and necrotic cells were also observed. A representative collage showing the progressive development of CPE in Vero E6 cells inoculated with material collected during air sampling 1-1 is shown in Figure 2. CPE were not observed and the virus was not detected or isolated from the culture medium of samples 1-2 and 2-2, wherein HEPA filters had been affixed to the inlet nozzles of the air samplers, and were not observed in mock-inoculated cells, which were maintained in parallel with the inoculated cell cultures.
Figure 2.
Cytopathic effects in Vero E6 cells inoculated with material collected from the air during air sampling 1-1. [A] Mock-infected Vero E6 cells, 10 days post-inoculation with sterile collection medium. [B]. Large cytoplasmic vacuoles in Vero E6 cells inoculated with collection medium from BioSpot sample 1-1 at 4 dpi. [C] Early focus of infection 7 dpi. [D] Focus of infection 10 dpi. Rounded cells that are detaching, some in clumps, are present. Attached cells remaining in this focus of infection have dark cytoplasm, some have large cytoplasmic inclusion bodies, and some cells are elongated. Original magnifications at 400 × .
SARS-CoV-2-specific rRT-PCR tests were performed and the results indicated that the LLC-MK2 and Vero E6 cultures inoculated with collection media from air samplings 1-1, 1-3, 2-1, and 2-3 contained SARS-CoV-2 (Table 3 ). No other respiratory virus was identified in the samples using a BioFire FilmArray Respiratory 2 Panel (BioMérieux Inc., Durham, North Carolina), following the manufacturer’s instructions.
Table 3.
rRT-PCR detection of SARS-CoV-2 N-gene sequences in air sample cultures.
| Air sampling interval |
||||||
|---|---|---|---|---|---|---|
| 1-1 | 1-2 | 1-3 | 2-1 | 2-2 | 2-3 | |
| LLCb Veroc | LLC Vero | LLC Vero | LLC Vero | LLC Vero | LLC Vero | |
| 4 dpia | 38.1 38.4 | NDd ND | ND ND | ND ND | ND ND | ND ND |
| 7 dpi | 35.3 35.9 | ND ND | 39.1 40.2 | 37.3 38.8 | ND ND | ND ND |
| 10 dpi | 31.5 32.2 | ND ND | 33.7 34.8 | 32.8 33.2 | ND ND | 36.4 37.2 |
dpi, days post-inoculation with material collected by air sampler.
LLC, LLC-MK2 cell culture.
Vero, Vero E6 cell culture.
ND, Not detected.
Whereas the concentration of SARS-CoV-2 genome equivalents per liter of air were estimated (Table 2), the determination of the specific infectivity (ratio of SARS-CoV-2 genome equivalents present for every one able to infect a cell in culture) required the performance of a plaque assay or a standard 50% endpoint dilution assay (TCID50 assay). Plaque assays could not be performed due to a nationwide nonavailability of some critical media components (due to COVID-19 pandemic-related temporary lockdown of production facilities), so TCID50 assays were performed in Vero E6 cells to estimate the percentage of the collected virus particles that were viable. Estimates ranged from 2 to 74 TCID50 units/L of air (Table 4 ).
Table 4.
Estimate of viable virus counts based on TCID50 tests.
| Sample ID | Virus genome equivalents/L of aira | TCID50/100 μl | Viable virus count/L air |
|---|---|---|---|
| 1-1 BioSpot | 94 | 2.68E+04 | 74 |
| 1-2 BioSpot + HEPA | - | 0 | 0 |
| 1-3 BioSpot | 30 | 6.31E+03 | 18 |
| 2-1 VIVAS | 44 | 1.00E+04 | 27 |
| 2-2 VIVA S+ HEPA | - | 0 | 0 |
| 2-3 VIVAS | 16 | 2.15E+03 | 6 |
From Table 2.
A nearly complete SARS-CoV-2 genome sequence was obtained by next generation sequencing (NGS) of RNA purified from cell culture medium of Vero E6 cells 7 dpi with NP swab material from patient 1. The RNA that was used for NGS had an rRT-PCR Cq value of 14 when tested using the SARS-CoV-2 N-gene primers described in Table 1. The nearly complete genome sequence (and the virus isolate) was designated SARS-CoV-2/human/UF-19/2020, and this genome sequence has been deposited in GenBank (accession no. MT668716) and in GISAID (accession no. EPI_ISL_480349). Because the amount of virus RNA was below the threshold that could be easily sequenced by our NGS methods, Sanger sequencing was used to sequence SARS-CoV-2 RNA directly purified from the collection media of air samplers 1-1, 1-3, 2-1, and 2-3. One complete SARS-CoV-2 sequence was attained for RNA purified in the material collected by air sampling 1-1, and three nearly complete sequences for 1-3, 2-1, and 2-3, respectively. After alignment, the comparisons of the three partial sequences with the complete sequence of SARS-CoV-2 in air sampling, 1-1 indicated that the same consensus genome sequence was present in the virions that had been collected in all the air samplings. Moreover, they were an exact match with the corresponding sequences of the virus isolated from patient 1. This complete genome sequence of the virus collected by the air samplers (and the virus therein) was considered the same isolate and designated SARS-CoV-2/Environment/UF-20/2020, and this genome sequence has been deposited in GenBank (accession no. MT670008) and in GISAID (accession no. EPI_ISL_477163). The virus’ genomic sequence currently falls within GISAID clade B.1(GH), which is characterized by mutations C241T, C3037T, A23403G, G25563T, S-D614G, and NS3-Q57H relative to reference genome WIV04 (GenBank accession no. MN996528.1). As of July 10, 2020, SARS-CoV-2 clade B.1(GH) was the predominant virus lineage in circulation in the USA.
Discussion
There are substantial epidemiological data supporting the concept that SARS-CoV, which is highly related to SARS-CoV-2 (Gorbalenya et al., 2020), was transmitted through an aerosol route (Yu et al., 2004, Li et al., 2005, McKinney et al., 2006). For SARS-CoV-2, there have also been two epidemiological reports consistent with aerosol transmission (Hamner et al., 2020, Park et al., 2020). However, despite these reports, uncertainties remain about the relative importance of aerosol transmission of SARS-CoV-2, given that so far, only one study has provided weak evidence of virus isolation from material collected by air samplers (Santarpia et al., 2020). In other reports, attempts to isolate the virus were not successful. The current study takes advantage of a newer air sampling technology that operates using a water vapor condensation mechanism, facilitating the likelihood of isolating the virus in tissue culture.
As reported in air sampling tests performed by others (Liu et al., 2020, Wang et al., 2020, Holshue et al., 2020, Santarpia et al., 2020) and in our previous report (Lednicky et al., 2020), airborne SARS-CoV-2 was present in a location with COVID-19 patients. The distance from the air samplers to the patients (≥ 2 m) suggests that the virus was present in aerosols. Unlike previous studies, we have demonstrated that the virus in aerosols can be viable, and this suggests that there is an inhalation risk for acquiring COVID-19 within the vicinity of people who emit the virus through expirations including coughs, sneezes, and speaking.
The amount of airborne virus detected per liter of air was small, and future studies should address (a) whether this is typical for COVID-19, (b) if this represented virus production relative to the phase of infection in the patient, (c) if this was a consequence of active air flow related to air exchanges within the room, (d) or if the low number of virus was due to technical difficulties in removing small airborne particles from the air (Pan et al., 2019).
Our findings reveal that viable SARS-CoV-2 can be present in aerosols generated by a COVID-19 patient in a hospital room in the absence of an aerosol-generating procedure, and can thus serve as a source for transmission of the virus in this setting. Moreover, the public health implications are broad, particularly as current best practices for limiting the spread of COVID-19 center on social distancing, wearing of face coverings while in proximity to others and hand washing. For aerosol-based transmission, measures such as physical distancing by 6 feet would not be helpful in an indoor setting, provide a false-sense of security, and lead to exposures and outbreaks. With the current surge of cases, to help stem the COVID-19 pandemic, clear guidance on control measures against SARS-CoV-2 aerosols are needed, as recently voiced by other scientists (Morawska and Milton, 2020).
Contributors
JAL, ML, ZHF, AJ, AEF, KC, JGM Jr, and C-YW conceived and designed the study. JAL, ML, KC, JG M Jr, and C-YW curated the data. JAL, ML, JGM Jr, and C-YW performed formal analyses of the data. JAL, ML, ZHF, AJ, JGM Jr. obtained funding for the work; JAL, TBT, MG, MU, SNS, KM, CJS, MMA, MAE, JCL, KS, and TBW performed experiments; JAL, M L, TBT, SNS, CJS, JCL, KS, TBW, JGM Jr, and C-YW established methods; JAL, ML, JCL, JGM Jr, and C-YW administered the project; JAL, ML, ZHF, AJ, JGM Jr, and C-YW provided resources; JAL, ML, JCL, JGM Jr, and C-YW supervised the project; JAL, JGM Jr., and C-Y Wu wrote the original manuscript draft; all authors revised the manuscript critically. All authors read and approved the final version of the manuscript.
Funding
Partly funded by Grant No. 2030844 from the National Science Foundationand by award 1R43ES030649 from the National Institute of Environmental Health Sciences of the National Institutes of Health, and by funds made available by the University of Florida Emerging Pathogens Institute and the Office of the Dean, University of Florida College of Medicine.
Declaration of interests
The authors proclaim they have no conflicts of interest to report.
Institutional review board (IRB) approval
The study protocol was approved by the UF IRB (study IRB202002102).
Acknowledgments
The authors thank Dr. Katherine Deliz (UF Environmental Engineering Sciences) for access to her laboratory for some essential engineering tasks, Drs. Christine Angelin and David Kaplan (UF Environmental Engineering Sciences) for providing critical supplies not readily available from vendors due to the COVID-19 pandemic, and Mark Dykes and Brad Pollitt of UF Health/Shands Hospital Facilities for providing room configuration and ventilation system info. Funding of work reported in this publication was partly supported by the National Science Foundation under Grant No. 2030844, partially by the National Institute of Environmental Health Sciences of the National Institutes of Health award number 1R43ES030649, and funds made available by the UF Emerging Pathogens Institute and the Office of the Dean, UF College of Medicine. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Science Foundation and the National Institutes of Health.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2020.09.025.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Andersen K.G., Rambaut A., Lipkin W.I. The proximal origin of SARS-CoV-2. Nat Med. 2020;26(4):450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bankevich A., Nurk S., Antipov D. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol. 2012;19:455–477. doi: 10.1089/cmb.2012.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . 2020. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Frequently asked questions. 2020.https://www.cdc.gov/coronavirus/2019-ncov/faq.html [Google Scholar]
- Chia P.Y., Coleman K.K., Tan Y.K., Ong S.W.X., Gum M., Lau S.K. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat Commun. 2020;11:2800. doi: 10.1038/s41467-020-16670-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fears A.C., Klimstra W.B., Duprex P., Hartman A., Weaver S.C., Plante K.S. Persistence of severe acute respiratory syndrome coronavirus 2 in aerosol suspensions. Emerg Infect Dis. 2020;26(9) doi: 10.3201/eid2609.201806). [DOI] [PMC free article] [PubMed] [Google Scholar]
- HV Fineberg. Rapid expert consultation on the possibility of bioaerosol spread of SARS-CoV-2 for the COVID-19 pandemic (April 1, 2020). In: The National Academies Press N.R.C., ed. Washington, DC: The National Academies Press, National Research Council. 2020.
- Gorbalenya A.E., Baker S.C., Baric R.S., de Groot R.J., Drosten C., Gulyaeva A.A. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Z.D., Wang Z.Y., Zhang S.F., Li X., Li L., Li C. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis. 2020;26:1583–1591. doi: 10.3201/eid2607.200885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamner L., Dubbel P., Capron I., Ross A., Jordan A., Lee J. High SARS-CoV-2 attack rate following exposure at a choir practice - Skagit County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:606–610. doi: 10.15585/mmwr.mm6919e6. [DOI] [PubMed] [Google Scholar]
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayaweera M., Perera H., Gunawardana B., Manatunge J. Transmission of COVID-19 virus by droplets and aerosols: a critical review on the unresolved dichotomy. Environ Res. 2020;188 doi: 10.1016/j.envres.2020.109819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang S., Du I., Shi Z. An emerging coronavirus causing pneumonia outbreak in Wuhan, China: Calling for developing therapeutic and prophylactic strategies. Emerg Microbes Infect. 2020;9:275–277. doi: 10.1080/22221751.2020.1723441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamers M.M., Beumer J., van der Vaart J., Knoops K., Puschhof J., Breugem T.I. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020;369:50–54. doi: 10.1126/science.abc1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lednicky J., Pan M., Loeb J., Hsieh H., Eiguren-Fernandez A., Hering S. Highly efficient collection of infectious pandemic influenza H1N1 virus (2009) through laminar-flow water based condensation. Aerosol Sci Technol. 2016;50(7):i–iv. [Google Scholar]
- Lednicky J.A., Shankar S.N., Elbadry M.A., Gibson J.C., Alam M.M., Stephenson C.J. Collection of SARS-CoV-2 virus from the air of a clinic within a university student health care center and analyses of the viral genome. Aerosol Air Qual Res. 2020;20:1167–1171. doi: 10.4209/aaqr.2020.02.0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Duan S., Yu I.T., Wong T.W. Multi-zone modeling of probable SARS virus transmission by airflow between flats in block E. Amoy Gardens Indoor Air. 2005;15:96–111. doi: 10.1111/j.1600-0668.2004.00318.x. [DOI] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Ning Z., Chen Y., Guo M., Liu Y., Gali N.K. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557–560. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. The Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney K.R., Gong Y.Y., Lewis T.G. Environmental transmission of SARS at Amoy Gardens. J Environ Health. 2006;68:26–30. [PubMed] [Google Scholar]
- Morawska I., Cao J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environ Int. 2020;139 doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Milton D.K. It is Time to Address Airborne Transmission of COVID-19. Clin Infect Dis. 2020:ciaa939. doi: 10.1093/cid/ciaa939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan M., Bonny T.S., Loeb J., Jiang X., Lednicky J.A., Eiguren-Fernandez A. Collection of viable aerosolized influenza virus and other respiratory viruses in a student health care center through water-based condensation growth. mSphere. 2017;2(5):e00251–17. doi: 10.1128/mSphere.00251-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan M., Lednicky J.A., Wu C.-Y. Collection, particle sizing and detection of airborne viruses. J Appl Microbiol. 2019;127:1595–1611. doi: 10.1111/jam.14278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S.Y., Kim Y.M., Yi S., Lee S., Na B.J., Kim C.B. Coronavirus disease outbreak in call center. South Korea Emerg Infect Dis. 2020;26(8):1666–1670. doi: 10.3201/eid2608.201274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santarpia J.L., Rivera D.N., Herrera V., Morwitzer M.J., Creager H.M., Santarpia G.W. Aerosol and surface transmission potential of SARS-CoV-2 observed in quarantine and isolation care. Sci Rep. 2020;10(1):12732. doi: 10.1038/s41598-020-69286-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Du G. COVID-19 may transmit through aerosol. Ir J Med Sci. 2020;24:1–2. doi: 10.1007/s11845-020-02218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Xu Y., Gao R., Lu R., Han K., Wu G. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323(18):1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. World Health Organization. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations: scientific brief, 27 March 2020. (WHO/2019-nCoV/Sci_Brief/Transmission_modes/2020.2). (Accessed 9 July 2020) [Google Scholar]
- Wood D.E., Lu J., Langmead B. Improved metagenomic analysis with Kraken 2. Genome Biol. 2019;20(1):257. doi: 10.1186/s13059-019-1891-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao F., Tang M., Zheng X., Liu Y., Li X., Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158:1831–1833.e3. doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu I.T., Li Y., Wong T.W., Tam W., Chan A.T., Lee J.H.W. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N Engl J Med. 2004;350:1731–1739. doi: 10.1056/NEJMoa032867. [DOI] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Song J., Zhao X. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.