Abstract
During the current pandemic of COVID-19, a myriad of manifestations and complications has emerged and are being reported on. We are discovering patients with COVID-19 are at increased risk of acute cardiac injury, arrythmias, thromboembolic complications (pulmonary embolism and acute stroke), and secondary infection to name a few. I describe a novel case of COVID-19 in a previously healthy 33-year-old female who presented for altered mental status and proptosis. She was ultimately diagnosed with mucormycosis and orbital compartment syndrome, in addition to COVID-19. Early identification of these high morbidity conditions is key to allow for optimal treatment and improved outcomes.
Keywords: COVID-19, Mucormycosis, Orbital compartment syndrome
1. Background
Coronavirus disease 2019 (COVID-19) is a new disease entity caused by a novel coronavirus (SARS-CoV-2) first documented in China in December 2019 and subsequently causing a worldwide pandemic. While the pathophysiology of the virus is still under investigation, new symptomatic manifestations and complications of the disease continue to be identified and described in medical literature. Mucormycosis and orbital compartment syndrome are rare, time sensitive conditions that must be recognized and treated promptly to avoid mortality and morbidity. Herein I present a case of rhino-orbital-cerebral mucormycosis in a patient who presented to the Emergency Department with altered mental status, proptosis, and COVID-19 infection.
2. Case presentation
A 33-year-old Somali female with past medical history of hypertension and asthma, presented to the emergency department with altered mental status. Her husband stated the patient began with symptoms of vomiting, cough, and shortness of breath 2 days prior to presentation. Vital signs on arrival were notable for mild tachycardia, hypertension, and tachypnea. She was afebrile and maintained normal oxygen saturation. Upon examination, she appeared in moderate distress with acutely altered mental status. Most notable was left eye ptosis with 1 cm proptosis. The eye had a fixed dilated pupil with complete ophthalmoplegia. No surrounding erythema, warmth or discharge was noted. Her nasal exam was unremarkable. The mucous membranes were dry, and palate had brown, dry appearing secretions.
3. Investigations
3.1. Emergency management
Blood chemistry, complete blood count, lactate, blood gas, and blood cultures were obtained. The patient was found to have a White Blood Cell count of 27 with 82.9% neutrophils and 5.1% lymphocytes. Serum chemistry was significant for glucose 649, carbon dioxide 5, creatinine 2.28, and lactate 2.8. Venous blood gas found a pH < 6.9, and pCO2 29. The chest radiograph showed left lower lobe consolidation consistent with pneumonia (Fig. 1 ). A stat CT of the head, face, and orbits were obtained. CT head was negative for acute pathology. The face CT face showed significant for moderate bilateral maxillary sinus mucosal thickening as well as ethmoid sinus mucosal thickening, and mucosal opacification of the ostiomeatal units (Fig. 2 ). Emergent lateral canthotomy was performed by the ED physician due to intraocular pressures of 80 mmHg in the setting of proptosis and ophthalmoplegia. Otolaryngology was consulted and the nasal mucosa was swabbed for culture. Ophthalmology was also consulted, and the patient was admitted to the Medical Intensive Care Unit.
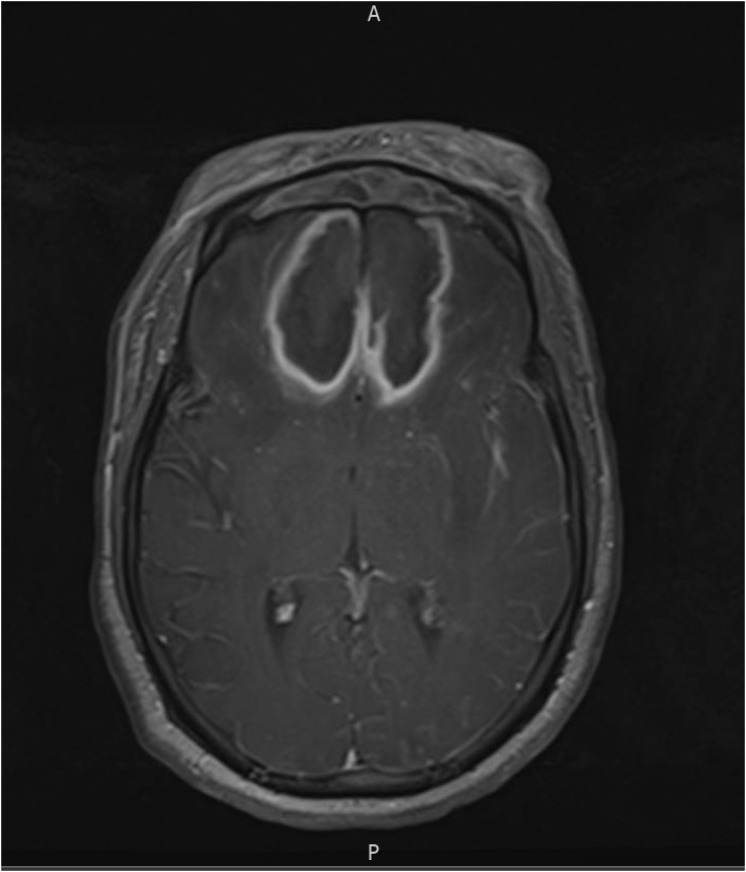
Fig. 1.
Chest x-ray: showing left lower pneumonia.
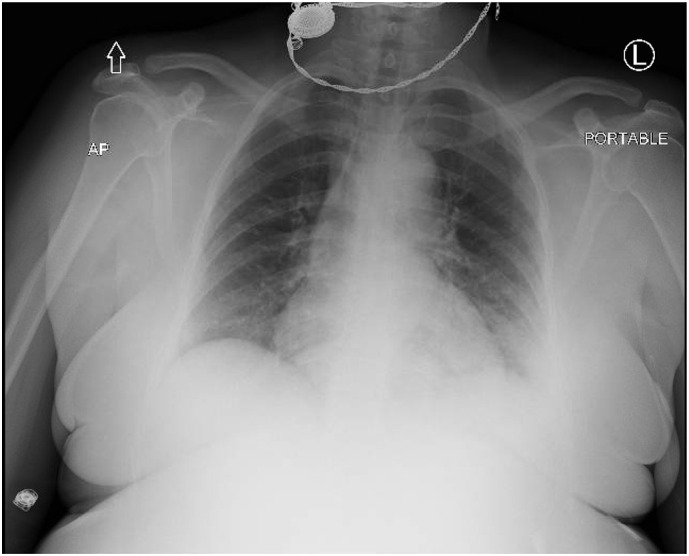
Fig. 2.
CT Head illustrating ethmoid sinus mucosal thickening.
4. Treatment
The patient's DKA was treated with intravenous fluids, sodium bicarbonate and, insulin infusions per local protocol. Vancomycin and piperacillin-tazobactam were administered for severe sepsis in treatment of pneumonia and possible orbital cellulitis. Amphotericin B was added for coverage of possible mucormycosis. Otolaryngology took the patient to the operating room for sinus debridement. Intraoperatively, the left middle turbinate was noted to be black. Sinus cultures were positive for moderate Staphylococcus aureus, as well as extensive fungal elements, including hyphae, yeast. The fungal culture was consistent with mucormycosis. An MRI brain was obtained during the ICU stay, demonstrating extensive multifocal signal abnormality with edema, and evidence of ischemia and infarction (Fig. 3, Fig. 4 ). These findings were highly suspicious for invasive rhino-orbital-cerebral mucormycosis. MRA head and neck was unremarkable. In addition, the patient received remdesivir and convalescent plasma. On day 24 of hospitalization, repeat MRI of the brain showed previously noted regions of cerebral edema had evolved into multiple encapsulated complex fluid collections predominantly in the bifrontal region suspicious for invasive mucormycosis (Fig. 5, Fig. 6 ). Neurosurgery was consulted for possible operative intervention. Ultimately, the family decided to make the patient comfort care because of her poor prognosis. The patient expired on day 26 of her hospitalization.
Fig. 3.

MRI brain showing paranasal sinus mucosal disease.
Fig. 4.
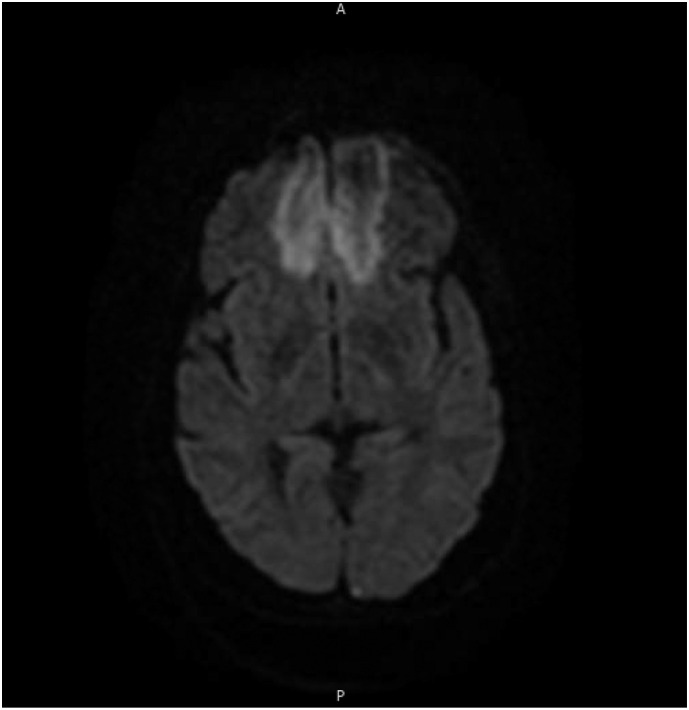
MRI brain showing multifocal infarction.
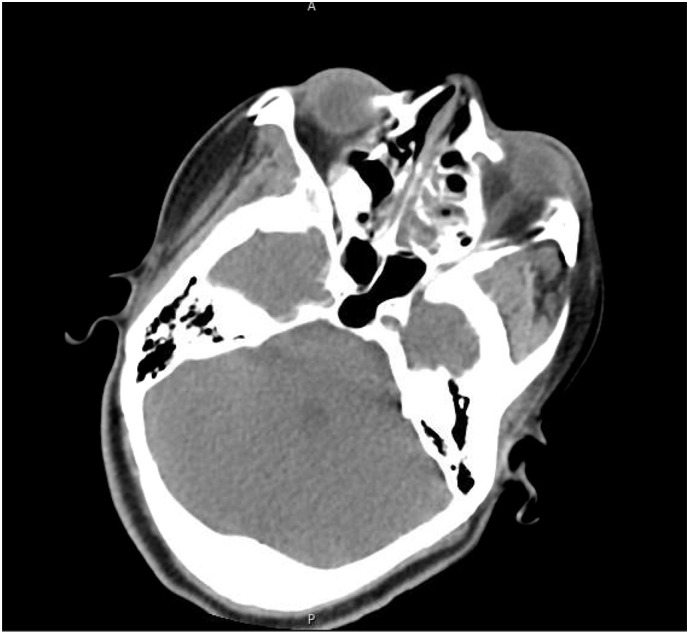
Fig. 5.
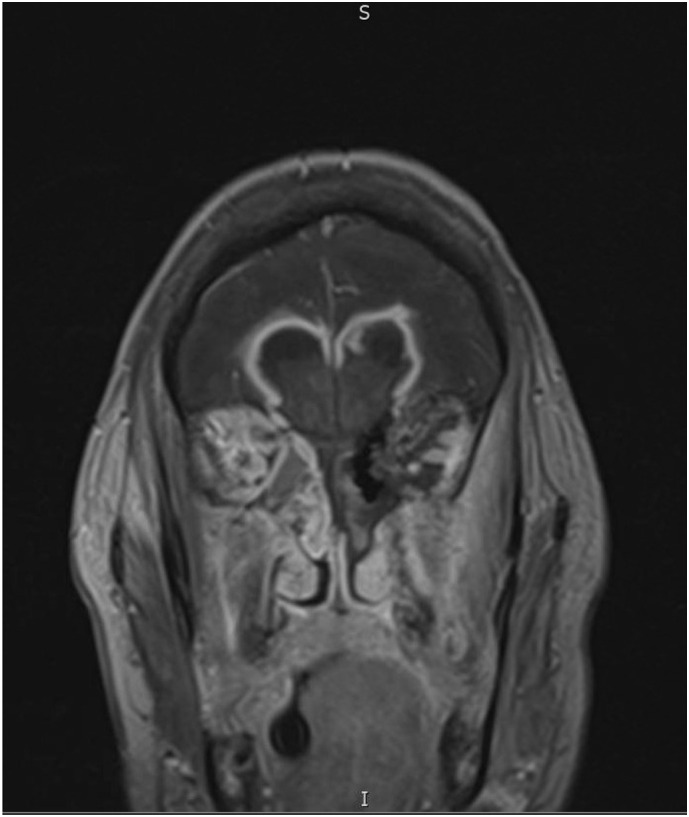
Inpatient MRI showing developing fungal brain abscess.
Fig. 6.
Additional MRI image of fungal brain abscess.
5. Discussion
Mucormycosis is rare opportunistic fungal infection characterized by infarction and necrosis of host tissues that results from invasion of the vasculature by hyphae. The most common clinical presentation of mucormycosis is rhino-orbital-cerebral infection, believed to be secondary to inhalation of spores into the paranasal sinuses of a susceptible host [1]. Predisposing situations for mucormycosis include diabetes, systemic corticosteroid use, neutropenia, hematologic malignancies, stem cell transplant, and immunocompromised individuals [2]. Seventy percent of rhino-orbital-cerebral mucormycosis cases have been found to be in patients with diabetes mellitus, most of whom had also developed ketoacidosis at the time of presentation. Infection usually presents with acute sinusitis, fever, nasal congestion, purulent nasal discharge and headache. All the sinuses become involved, and contiguous spread to adjacent structures such as the palate, orbit, and brain results in clinical symptoms. For example, spread of infection from the ethmoid sinus to the frontal lobe results in obtundation. Clinical suspicion and early treatment with surgical debridement are key to preventing morbidity in this often-fatal condition. Histopathology, direct microscopy, and culture from clinical specimens are the major diagnostic modalities for mucormycosis [3].
The incident rate of mucormycosis varies from 0.005 to 1.7 per million population [4]. The global mucormycosis case fatality rate is 46% [5]. Mucormycosis is difficult to diagnosis. Early diagnosis and treatment are essential, as a delay of even 6 days is associated with a doubling of 30-day mortality from 35% to 66%. Despite early diagnosis and aggressive combined surgical and medical therapy, the prognosis for recovery from mucormycosis is poor. A high suspicion for this disease must be considered in patients who are immunocompromised. In high-risk individuals, this diagnosis should be suspected if there is unilateral facial pain or swelling, orbital swelling, or proptosis. Tissue necrosis, often a late sign, is a hallmark of mucormycosis, resulting from angioinvasion and vascular thrombosis. Once the diagnosis is considered, empiric antifungal treatment should be started. Prompt surgical opinion should also be sought.
Orbital compartment syndrome (OCS) results from an expansile process within the closed compartment of the orbit leading to increased orbital pressure, and potentially resulting in ischemia and vision loss. It is a true ophthalmologic emergency that requires lateral canthotomy and inferior cantholysis to decompress the orbit. Delay in care can lead to permanent blindness. This diagnosis should be suspected in patients presenting with acute proptosis, elevated intraocular pressure, rapid vision loss, ophthalmoplegia, fixed dilated pupil or afferent pupillary defect. Causes of OCS can be retrobulbar hemorrhage (from trauma, vascular malformations, tumors), cellulitis or other infection, orbital malignancy, or previous orbital surgery [6].
My review of the literature indicates that this is likely the first documented case of mucormycosis in combination with COVID-19 infection. It is impossible to know for certain whether this patient's COVID-19 infection was contributory to her illness or merely coincidental. In my opinion, the patient's severe immunocompromised state from untreated diabetes, and ultimately diabetic ketoacidosis is what made her susceptible to contract both mucormycosis and COVID-19. As we learn more about COVID-19, and continue seeing more patients with this illness, we likely will continue seeing other unique presentations of other disease entities.
Declaration of Competing Interest
None.
References
- 1.Cox G. 2020. Mucormycosis. Uptodate- July 2020. [Google Scholar]
- 2.Serris A., Danion F., Lanternier F. Disease entities in mucormycosis. J Fungi. 2019;5(1):23. doi: 10.3390/jof5010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spellberg B., Edwards J., Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005;18(3):556–569. doi: 10.1128/CMR.18.3.556-569.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeong W., Keighley C., Wolfe R., et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25:26–34. doi: 10.1016/j.cmi.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 5.Chamilos G., Lewis R.E., Kontoyiannis D.P. Delaying amphotericin B-based frontline therapy significantly increases mortality among patients with hematologic malignancy who have zygomycosis. Clin Infect Dis. 2008;47:503–509. doi: 10.1086/590004. [DOI] [PubMed] [Google Scholar]
- 6.Stiff H., Chung A., et al. Orbital compartment syndrome curriculum. 2020. Eyerounds.org [DOI] [PubMed]