Case presentation
A 65-year-old man was admitted to the intensive care unit (ICU) of Tenon hospital, a university teaching hospital in Paris, France, for severe confirmed COVID-19 pneumonia. He had a history of diabetes. In the preceding week, the patient developed fever (39 °C), cough, and shortness of breath. A chest computed tomography (CT) scan showed bilateral ground glass opacities with alveolar consolidation (Figure 1 A) predominant in the lung periphery as usually reported in COVID-19 pneumonia (Chung et al., 2020, Jajodia et al., 2020). Advanced life support was administered including lung-protective ventilation, prone-positioning, and vasoconstrictors. Empirical antimicrobial therapy was initiated, in association with hydrocortisone. The infusion of Tocilizumab was administered (Zhang et al. 2020). After initial improvement, the patient’s condition worsened. A second CT scan was performed on day 20, showing the extent of the right upper lobe lesions with a crazy paving pattern (Figure 1B). Multiple organ failure persisted. Two episodes of ventilator-associated pneumonia (VAP) were treated on day 16 (Citrobacter koseri) and day 40 (Achromobacter xylosoxidans). Pulmonary fibrosis with bronchiectasis and cavitation developed in the right upper lobe (Figure 1C). A bronchoalveolar lavage revealed macrophagic alveolitis. Fifty-four days after admission, the patient died of persisting multiple organ failure.
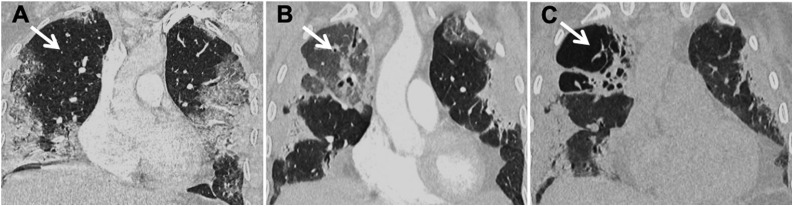
Figure 1.
Follow-up chest computed tomography scan of a 65-year-old man with confirmed COVID-19 pneumonia.
(A) Coronal chest computed tomography scan showing the evolution of the right upper lobe with initial normal pulmonary parenchyma on admission (day 1, arrow). (B) Ground-glass opacity at day 20 (arrow). (C) Fibrosis formation with traction bronchiectasis and cavitation at day 40 (arrow).
Acute cavitary lung lesions are usually related to mycobacterial, parasitic, fungal, or bacterial infection, particularly Staphylococcus aureus, Pseudomonas aeruginosa, and other gram-negative bacilli. In our case, despite VAP due to Citrobacter koseri and Achromobacter xylosoxidans, this hypothesis is unlikely because neither radiological changes nor signs of necrotizing pneumonia were present on successive chest x-rays. Other causes of lung cavitation, such as autoimmune disorder or genetic mutations, were not investigated but the speed of the development of cavitary lesion in a few days was considered atypical. In the last hypothesis, although interleukin 6 (IL-6) inhibitor-induced interstitial lung disease has already been described, cavitation related to tocilizumab has not been reported, thus it should be reported as a related side adverse event.
Severe COVID-19 pneumonia may progress to pulmonary fibrosis (George et al. 2020) related to diffuse alveolar damage, but the association with lung cavitation is uncommon and may significantly impair the outcome (Chen et al. 2020).
Authors’ contributions
All authors had access to the data and a role in writing the manuscript.
Funding
No specific funding was available for the generation of this manuscript.
Compliance with ethical standards
Consent was obtained from the relative.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgments
We would like to thank Prof. François Cornelis for the selection and formatting CT images.
References
- Chen Y., Chen W., Zhou J., Sun C., Lei Y. Large pulmonary cavity in COVID-19 cured patient case report. Ann Palliat Med. 2020 doi: 10.21037/apm-20-452. Jun 9. [DOI] [PubMed] [Google Scholar]
- Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV) Radiology. 2020;295(1):202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George P.M., Wells A.U., Jenkins R.G. Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Respir Med [Internet] 2020 doi: 10.1016/S2213-2600(20)30225-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7228727/ May 15 [cited 2020 Aug 3]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jajodia A., Ebner L., Heidinger B., Chaturvedi A., Prosch H. Imaging in corona virus disease 2019 (COVID-19)-A scoping review. Eur J Radiol Open. 2020:100237. doi: 10.1016/j.ejro.2020.100237. May 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Wu Z., Li J.-W., Zhao H., Wang G.-Q. The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality. Int J Antimicrob Agents. 2020:105954. doi: 10.1016/j.ijantimicag.2020.105954. Mar 29. [DOI] [PMC free article] [PubMed] [Google Scholar]