Supplemental Digital Content is available in the text.
Keywords: criteria, critical care, health policy, intensive care unit admission, transfer, triage
Objectives:
To identify and appraise articles describing criteria used to prioritize or withhold a critical care admission.
Data Sources:
PubMed, Embase, Medline, EBM Reviews, and CINAHL Complete databases. Gray literature searches and a manual review of references were also performed. Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines were followed.
Study Selection:
We sought all articles and abstracts of original research as well as local, provincial, or national policies on the topic of ICU resource allocation. We excluded studies whose population of interest was neonatal, pediatric, trauma, or noncritically ill. Screening of 6,633 citations was conducted.
Data Extraction:
Triage and/or transport criteria were extracted, based on type of article, methodology, publication year, and country. An appraisal scale was developed to assess the quality of identified articles. We also developed a robustness score to further appraise the robustness of the evidence supporting each criterion. Finally, all criteria were extracted, evaluated, and grouped by theme.
Data Synthesis:
One-hundred twenty-nine articles were included. These were mainly original research (34%), guidelines (26%), and reviews (21%). Among them, we identified 200 unique triage and transport criteria. Most articles highlighted an exclusion (71%) rather than a prioritization mechanism (17%). Very few articles pertained to transport of critically ill patients (4%). Criteria were classified in one of four emerging themes: patient, condition, physician, and context. The majority of criteria used were nonspecific. No study prospectively evaluated the implementation of its cited criteria.
Conclusions:
This systematic review identified 200 criteria classified within four themes that may be included when devising triage programs including the coronavirus disease 2019 pandemic. We identified significant knowledge gaps where research would assist in improving existing triage criteria and guidelines, aiming to decrease arbitrary decisions and variability.
The decision to admit a patient to the ICU is the result of a complex process in which several human and logistic factors intertwine. Resource availability, patient characteristics, and physician assessment’s variability all contribute to patients’ outcome uncertainty (1). A lack of a standardized process to evaluate patient referrals and optimize resource allocation accentuates those differences leading to several critically ill patients being prevented access to ICU resources, which directly impacts their prognosis. The current coronavirus disease 2019 (COVID-19) pandemic shines a light on the ethical and practical issues clinicians face when triaging patients.
Triage centers, or the process of regionalization, can potentially help solve these issues. It involves access to a larger pool of resources provided by members of a network and allocation, as appropriate, according to the needs of each individual patient triaged (2). Drawing from the trauma literature, where implementation of organized and coordinated triage systems was shown to decrease mortality (3) and reduce time-consuming inter-hospital transfers (4), several groups have proposed that similar structures could be beneficial to critical care patients (5, 6). However, despite two decades of advocacy (7), only few initiatives were developed.
In the Province of Quebec (Canada), such a proposition has garnered the interest of policymakers and clinicians alike (8). More recently, the COVID-19 pandemic has shined a light on strained critical medical resources and the need for a triage process (9–11). However, there is currently a lack of universally agreed specific recommendations as to the triage criteria that should be used outside of the trauma population for ICU transport and admission. Namely, recommendations are especially vague when it comes to describing circumstances where the triage should result in the withholding of critical care resources including mass casualties such as COVID-19. Therefore, the purpose of this review was to systematically identify and appraise the published literature that defined criteria under which ICU admissions (triage and transport) should be withheld or not prioritized. We then propose a general framework to help clinicians use the results of this review to develop local triage guidelines adapted to the COVID-19 pandemic context.
MATERIALS AND METHODS
Search Strategy
In order to capture the broadest scope of articles, we aimed to include articles pertaining to critical care triage for admission to the unit or for interventions that mandatorily require critical care admission (e.g., extracorporeal membrane oxygenation [ECMO], heart-lung transplant) We searched PubMed, Medline (Ovid), Embase (Ovid), EBM Reviews (Ovid), and CINAHL Complete (EBSCO) using relevant keywords from inception to November 8, 2016. For each database, we used terms from controlled vocabulary (MESH, EMTREE, and CINAHL headings) and also performed a free text searching in title, abstract, and author keywords fields. A gray literature search was also executed in the following sources: Health Development Agency; National Guideline Clearing House; National Institute for Health and Clinical Excellence; National Institutes of Health; Research Service Delivery and Organisation Programme; Research Register for Social Care; and Google Scholar and OpenGrey. We limited our search to English and French languages. We also manually searched the reference lists of all articles remaining at the full-text review step for any potentially relevant article missed by our electronic searches. Our complete search strategy can be found in Supplemental Digital Content 1 (http://links.lww.com/CCM/F760).
Inclusion and Exclusion Criteria
We sought all articles and abstracts of original research, such as trials and observational studies, guidelines, reviews, editorials, and commentaries published in peer-reviewed journals, which listed criteria for ICU admission. Furthermore, we sought to include local, provincial, and/or national policies on the topic of ICU resource allocation. We excluded studies whose population of interest was neonatal, pediatric, trauma, or noncritically ill. Furthermore, we excluded studies if the ICU selection criteria did not permit to discriminate between ICU candidates or if they did not reflect systematic practice.
Study Identification and Selection
After removal of duplicates, one reviewer (J.D.) systematically reviewed the results and performed a title screen. All potentially relevant records, as well as those that did not contain enough information to determine eligibility, were retained for abstract screening. We went on to perform an abstract screen and retained all records that met inclusion criteria for full-text review. If no abstract was available, the citation was automatically selected for full-text review.
Data Extraction and Analysis
Data extraction was completed by one team member (J.D.). Data were collected on an electronically prepared Excel-based data collection tool (Microsoft Corp, Seattle, WA). Information extracted were the type of article and study design when applicable, year and country of publication, mechanism and setting of the triage and/or transport process, including whether it was condition-specific, and whether the criteria were proposed or currently in use. Given the heterogeneity of the studies, we developed a three-level appraisal scale to allow quality grading: level 1: randomized controlled trials, society guidelines, and national policies; level 2: rigorous reviews and multicenter observational studies; and level 3: single-center studies, editorials/commentaries where criteria are not backed up by evidence, and other articles with methodological flaws. Of note, certain exceptions, where papers that became highly cited references with time, were assigned a higher level (Supplemental Digital Content 2, http://links.lww.com/CCM/F761). To appraise the strength of the triage and transport criteria, we developed a robustness score (RS) which factors the number of studies listing each criteria as well as their quality (RS = [nL1 × FL1] + [nL2 × FL2] + [nL3 × FL3], where n = number of studies; F = factor; L1 = level 1 quality [highest]; L2 = level 2 quality; and L3 = level 3 quality [lowest]). Level 1, 2, and 3 quality studies were given a factor of 2 points, 1 point, and 0.25 point, respectively. From this score, we classified the robustness of the evidence supporting all criteria within one of three categories: strongly robust evidence (defined as > two sds from the average RS), averagely robust evidence (above average RS but < 2 sds), and weakly robust evidence (below average RS). Additionally, we assessed whether extracted criteria met the following criteria: specific, scientifically sound, measurable, feasible to implement, and usable (12, 13). (Supplemental Digital Content 3, http://links.lww.com/CCM/F762; Supplemental Digital Content 4, http://links.lww.com/CCM/F763; Supplemental Digital Content 5, http://links.lww.com/CCM/F764; and Supplemental Digital Content 6, http://links.lww.com/CCM/F765). Finally, all articles were evaluated by identifying key themes. Criteria were grouped by theme and classified as patient-, condition-, physician-, or context-related. Context-related criteria are those criteria that are to be triggered only under specific circumstances. For example, they may pertain to time, location, or resource shortages, such as during pandemics or mass disasters.
Reporting Guidelines
We published our review protocol on International prospective register of systematic reviews (CRD42016047239). We also followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses guideline as applicable to this study’s design (14) (Supplemental Digital Content 7, http://links.lww.com/CCM/F766).
RESULTS
Eligible Studies
The literature search identified 5,818 unique articles. Review of titles and abstracts resulted in the retrieval of 416 potentially full-text articles. Manual search of the reference lists of these articles led to 29 further full-text reviews. Of these, we identified 129 articles that met inclusion criteria and were included in this review (Fig. 1)
Figure 1.
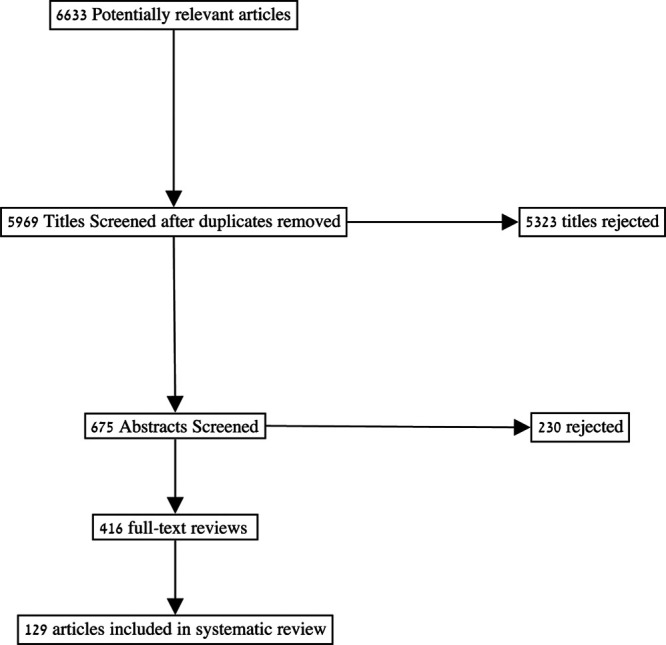
Flow diagram of studies identified and included in the systematic review.
Characteristics of Studies
Table 1 summarizes the characteristics of the articles. All articles were in English except for five written in French (3.8%). Most articles were original research studies (n = 44, 34%) of which the vast majority were cohort studies (n = 31, 70%). Of note, no randomized controlled trials were identified. Pertaining to triage criteria, 62 articles (48%) were specific to certain patient populations or situations. Most articles described a triage process which relied on complete exclusion from ICU admission (n = 91, 70.5%) rather than a prioritization process (n = 22, 17%), whereas a few more articles described a combination of both. About a third of identified articles listed criteria that addressed more than one theme (n = 48, 37%). The most common theme for triage criteria was condition-related (n = 63, 48.8%) followed by patient-related criteria (n = 48, 37%).
Table 1.
Characteristics of Studies Included in Review (n = 129 Articles)
| Characteristics | Articles, n (%) |
|---|---|
| Type of article | |
| Original research | 44 (34) |
| Cohort study | 31 (24) |
| Systematic review | 1 (1) |
| Nonrandomized control trial with contemporaneous controls | 1 (1) |
| Series of consecutive cases | 2 (2) |
| Policy analysis | 1 (1) |
| Qualitative study | 1 (1) |
| Other original research | 7 (5) |
| Policy/guideline | 33 (26) |
| Editorial/commentary | 19 (15) |
| Review | 27 (21) |
| Other | 6 (5) |
| Country of origin | |
| United States | 63 (48) |
| France | 21 (16) |
| United Kingdom | 13 (10) |
| Canada | 7 (5) |
| Language of publication | |
| English | 124 (96) |
| Year of publication | |
| 1970–1989 | 6 (5) |
| 1990–1999 | 23 (18) |
| 2000–2009 | 36 (28) |
| 2010–2016 | 64 (50) |
| Type of process | |
| Triage | 124 (96) |
| Transport | 3 (2) |
| Both | 2 (2) |
| Process type | |
| Complete exclusion | 91 (71) |
| Prioritization/waiting lists | 22 (17) |
| Both | 12 (9) |
| Other | 4 (3) |
| Themes | |
| Patient-related | 48 (37) |
| Condition-related | 63 (49) |
| Physician-related | 45 (35) |
| Context-related | 37 (29) |
Triage and Transport Criteria
A total of 200 unique triage and transport criteria were extracted from the 129 articles (1, 6, 15–141). Only five articles (4%) discussed transport criteria. A complete list of all triage and transport criteria are listed in Supplemental Digital Content 7 (http://links.lww.com/CCM/F766). As previously mentioned, we grouped identified criteria under four themes. Where possible, synonymous criteria were grouped unless it was felt that the differences in terminology evocated significant clinically relevant nuances. Condition-related criteria consisted in the most diverse and populous theme.
Analysis for patient-related criteria yielded eight categories and 18 unique criteria stemming from 48 citations. Patient preference was the most common reason cited to exclude patients from ICU admission (n = 29, 60.4%). Articles citing functional status (n = 13, 27%) and age to exclude patients were also common (n = 7, 14.6%), but only two citations used a specific age cutoff (i.e., 65 and 70 yr old) (33, 97). Social support and technical considerations were found but related to specific interventions (transplant or ECMO).
We found 63 articles that contained at least one condition-related criteria. Analysis yielded 11 categories and 87 unique criteria of which most related to comorbidities or diagnosis (n = 69). The most common criteria cited for ICU refusal was when no further oncological treatment options were available (n = 12) followed by persistent vegetative state and terminal diagnosis (n = 8). The majority of criteria had only one citation supporting it (n = 67). Thirteen articles pertained to a prioritization process, but only one article described a prioritization that was exclusively condition-related (42).
A total of 45 articles addressed physician-related criteria. Only two categories were extracted from this theme: prognosis and physician evaluation. All articles contained a criterion attributable to prognosis, although one article also listed incomplete physician evaluation as a reason to deny ICU admission. Within the prognosis category, 14 unique criteria were found. Most citations were encompassed by two criteria: patients who were judged by the physician to either be too well (n = 20) or too sick (n = 15). Fifteen citations used a prioritization scheme rather than exclusion.
Finally, analysis for context-related criteria yielded six categories and 81 unique criteria stemming from 37 articles. Citations citing metastatic malignant disease (n = 14), advanced and irreversible neurologic disease (n = 13), and Sequential Organ Failure Assessment (SOFA) score greater than 11 (n = 11) led to these three criteria being the most common within this theme. The most populous category is that of epidemics and pandemics (including influenza) or other mass disasters (24 citations, 65.9%). Within this category, we further divided the data into 19 themes and 70 criteria. Several subthemes pertained to clinical conditions (n = 13 criteria, 68.4%), while the balance pertained to age (n = 1, 5.3%) or other forms of prognostication (n = 4, 21.1%). Within the context-related criteria, only seven studies were published prior to 2006, and none of these addressed pandemics or other large-scale disasters. Other relevant categories pertained to bed availability (n = 7 citations, 18.9%) or other lack of resources (n = 5, 13.5%). Furthermore, only one study specifically pertained to transport criteria and related to unsuitable flying conditions.
Developing and ranking criteria per our robustness scale provided further insight. We extracted the top 10% most robust criteria for a total of 20 criteria (Table 2). While the most robust criteria related to patient preference (i.e., avoiding admission of patients or families who decline intensive care), 75% of those triage criteria pertained to epidemics, which falls under the context theme.
Table 2.
Criteria Achieving the Highest Robustness Score (Top 10%)
| Rank | Theme/Category | Specific Criteria | Robustness Score |
|---|---|---|---|
| 1 | Patient/patient preference | Patients or families who decline intensive care or some of its components (e.g., mechanical ventilation, do not resuscitate) | 26.25 |
| 2 | Context/epidemics | Metastatic malignant disease | 22.25 |
| 3 | Context/epidemics | Advanced and irreversible neurologic event or condition | 21.25 |
| 4 | Context/epidemics | If cardiac arrest: Any of: unwitnessed cardiac arrest, witnessed cardiac arrest not responsive to electrical therapy, recurrent cardiac arrest | 18.25 |
| 5 | Context/epidemics | End-stage lung failure: Primary pulmonary hypertension with NYHA class III or IV heart failure, right atrial pressure > 10 mm Hg, or mean pulmonary artery pressure > 50 mm Hg | 18.25 |
| 6 | Context/epidemics | If burn injury: Any two of: > 60 yr old, > 40% total body area, inhalational injury | 17.25 |
| 7 | Context/epidemics | End-stage lung failure: Chronic obstructive pulmonary disease < 25% or Pao2 < 55 mm Hg or secondary pulmonary hypertension or on home o2 (10) | 17.25 |
| 8 | Context/epidemics | Advanced untreatable neuromuscular disease | 16.25 |
| 9 | Context/epidemics | End-stage heart failure: NYHA III or IV | 16.25 |
| 10 | Context/epidemics | End-stage lung failure: Cystic fibrosis with post-bronchodilator forced expiratory volume in 1 s < 30% or baseline Pao2 < 55 mm Hg | 16.25 |
| 11 | Context/epidemics | End-stage lung failure: Pulmonary fibrosis with vital capacity or total lung capacity < 60% predicted or Pao2 < 55 mm Hg or secondary pulmonary hypertension | 16.25 |
| 12 | Context/epidemics | End-stage liver failure: Child-Pugh score ≥ 7 | 16.25 |
| 13 | Context/epidemics | Elective palliative surgery | 15.25 |
| 14 | Context/epidemics | Sequential Organ Failure Assessment score > 11 | 14.5 |
| 15 | Physician/prognosis | Too well | 12.5 |
| 16 | Physician/prognosis | Too sick | 12 |
| 17 | Condition/diagnosis | No further oncological treatment options | 11.25 |
| 18 | Context/epidemics | Severe baseline cognitive impairment | 11.25 |
| 19 | Context/epidemics | Age > 85 yr old | 11.25 |
| 20 | Condition/diagnosis | Persistent vegetative state | 9.5 |
NYHA = New-York Heart Association.
The overlap between context and the three other themes was further analyzed. All but five of the 81 context criteria (Supplemental Digital Content 8, http://links.lww.com/CCM/F767, in red) were not akin to being classified under patient-, condition-, or physician-related criteria. Furthermore, the terminology used for context-related criteria tended to be more specific as 66% of criteria were measurable as opposed to patient (51.6%) or condition (44.8%) related. None of the physician-related criteria were measurable (Supplemental Digital Content 5, http://links.lww.com/CCM/F764). Furthermore, we analyzed the data across geographic regions using the three most commonly cited criteria for each theme (Table 3). This analysis generally showed international consistency.
Table 3.
Thematic Top Three Most Commonly Cited Criteria by Geographic Region
| Specific Criteria | Citations | All Articles, n | North America, n (%) | Europe, n (%) | Asia, n (%) | Other, n (%) |
|---|---|---|---|---|---|---|
| Patient | ||||||
| Patients or families who decline intensive care or some of its components | (36, 37, 44, 50, 55, 59, 73, 94, 105, 127, 133) (1, 19, 30, 47, 53, 56, 66–68, 93, 102, 103, 117–119, 125, 136, 140) | 29 | 10 (16) | 14 (30) | 4 (33) | 1 (14) |
| Bedridden | (47, 53, 79, 109, 129) | 5 | 0 (0) | 5 (11) | 0 (0) | 0 (0) |
| Advanced age | (23, 62, 69, 111) | 4 | 1 (2) | 3 (9) | 0 (0) | 0 (0) |
| Condition | ||||||
| No further oncological treatment options | (20, 47, 48, 53, 56, 66, 77, 79, 113, 118, 129, 133) | 12 | 2 (3) | 8 (17) | 2 (17) | 0 (0) |
| Persistent vegetative state | (39, 66, 82, 103, 115, 117, 118, 133) | 8 | 6 (9) | 1 (2) | 1 (8) | 0 (0) |
| Terminal diagnosis | (20, 35, 87, 100, 109, 118, 119, 133) | 8 | 4 (6) | 2 (4) | 2 (17) | 0 (0) |
| Physician | ||||||
| Too well | (15, 16, 26, 32, 45, 50, 62, 63, 66–69, 87, 95, 98, 110, 112, 125, 136, 138, 141) | 21 | 8 (13) | 9 (20) | 1 (8) | 3 (43) |
| Too sick | (15, 16, 26, 32, 50, 62, 63, 67–69, 95, 98, 101, 112, 138, 141) | 16 | 6 (10) | 7 (15) | 1 (8) | 2 (29) |
| Likelihood of benefit | (25, 31, 66, 103, 133, 135, 139, 141) | 8 | 3 (5) | 3 (7) | 2 (17) | 0 (0) |
| Context | ||||||
| Metastatic | (17, 27, 40, 41, 65, 70, 74, 75, 89–91, 95, 104, 131, 137) | 15 | 9 (14) | 4 (9) | 1 (8) | 1 (14) |
| Advanced and irreversible neurologic event or condition | (17, 27, 40, 41, 65, 70, 74, 75, 90, 91, 95, 124, 131, 137) | 14 | 8 (13) | 4 (9) | 1 (8) | 1 (14) |
| Sequential Organ Failure Assessment score > 11 | (17, 27, 40, 46, 70, 75, 90, 91, 95, 104, 124, 131) | 12 | 6 (9) | 5 (9) | 1 (8) | 0 (0) |
DISCUSSION
The objective of this systematic review was to identify published criteria about recommended or used criteria for the triage or transport of patients to a critical care facility. We identified 200 unique criteria, stemming from 129 articles and 23 countries depicting a wide variety of ICU organizational models. Yet, despite an ICU exclusion mechanism identified in 71% of the articles, several cited exclusion criteria do not meet minimal standards of a good criterion as was previously defined (Supplemental Digital Content 3, http://links.lww.com/CCM/F762; Supplemental Digital Content 4, http://links.lww.com/CCM/F763; Supplemental Digital Content 5, http://links.lww.com/CCM/F764; and Supplemental Digital Content 6, http://links.lww.com/CCM/F765). For example, none of the physician-related criteria are quantitative, while only 45% to 66% of the patient-, condition-, and context-related criteria are measurable. Furthermore, while we assessed 16% of the articles to be of high quality (i.e., national policies, society guidelines), none of the criteria stemmed from randomized controlled trials. More importantly, not a single study evaluated the impact of the implementation of its triage criteria.
Vague wording of ICU triage guidelines such as “likelihood of benefit,” “futility,” or “advanced age” provides practical issues, notably not allowing for measurement of compliance rates (142, 143). It also results in unintended externalities such as lack of transparency (144) or, at least, that of significant physician decision-making variation (145–153). Hence, despite the Society of Critical Care Medicine recommending each unit develops its own admission policy as early as in 1999 (112) and again in 2016 (36), there is no universally accepted set of specific and measurable admission criteria. This probably relates to the importance that physician autonomy holds in modern medical practice and its consequent freedom of treatment options based on best clinical judgment (154).
Nonetheless, our results show that there may be an emerging trend in the past decade, where exclusion criteria are becoming more specific. The temporal trend seems to correlate with the publication in 2006 of the article by Christian et al describing a triage protocol for an Influenza pandemic which described 12 exclusion criteria (91). The interest generated by this highly cited study largely accounts for the findings of our study, where criteria were ranked by robustness. Indeed, out of the 20 most robust criteria according to the score we developed, 15 pertain to epidemics situations and, when not identical, draw inspiration from the propositions by Christian et al (91). This is a testimony to the acceptability within the triage community of such specific criteria.
Our study adds to existing reviews documenting the process of ICU triage and transport (15, 95, 136, 155). Namely, our study is the first systematic review documenting criteria, either currently in use or proposed, adopted homogeneously within a team or organization. Indeed, previous studies aimed to document individual practices and usually used survey methodology. Such studies identified different themes than ours, mainly religion (156), country of practice (157), socioeconomic status (158), or even nursing morale (18).
Moving Forward
Several frameworks have been proposed to help triage patients and allocate scarce resources during the current COVID-19 (severe acute respiratory syndrome coronavirus 2) pandemic (9–11, 159). Guidance to help front-line clinicians make critical rationing decisions have been recently proposed (160). Our review provides guidance on the type of criteria to include in triage programs and systems. An earlier version of this work was submitted to the provincial critical care pandemic preparedness working group in Quebec (Canada). The work informed the design of a provincial triage protocol. Robust criteria were validated against what was then known about COVID-19. Hence, patients’ preferences to decline intensive care as well as comorbidities which decreased short- and long-term prognosis were chosen as exclusion criteria (Table 2). Such exclusion criteria become more stringent as surge increases (159). We recommend using criteria that are specific, scientifically sound, measurable, feasible, and usable in order to favor reproducibility of the decisions and accountability (Supplemental Digital Content 3, http://links.lww.com/CCM/F762; Supplemental Digital Content 4, http://links.lww.com/CCM/F763; Supplemental Digital Content 5, http://links.lww.com/CCM/F764; and Supplemental Digital Content 6, http://links.lww.com/CCM/F765). Criteria which do not discriminate in the context of COVID-19, such as the SOFA score (161), should be avoided despite their robustness. Finally, as many COVID-19 infected patients present with few comorbidities, clinicians should familiarize themselves with nonclinical triage principles such as the multiplier effect (i.e., can saving this patient’s life help save many others?), the life-cycle principle (i.e., how many further life stages is the patient expected to live through?), and randomization. Such principles may help discriminate between seemingly similar patients during mass triage. Others have integrated such concepts into a point system (123). Our approach is summarized in Figure 2.
Figure 2.
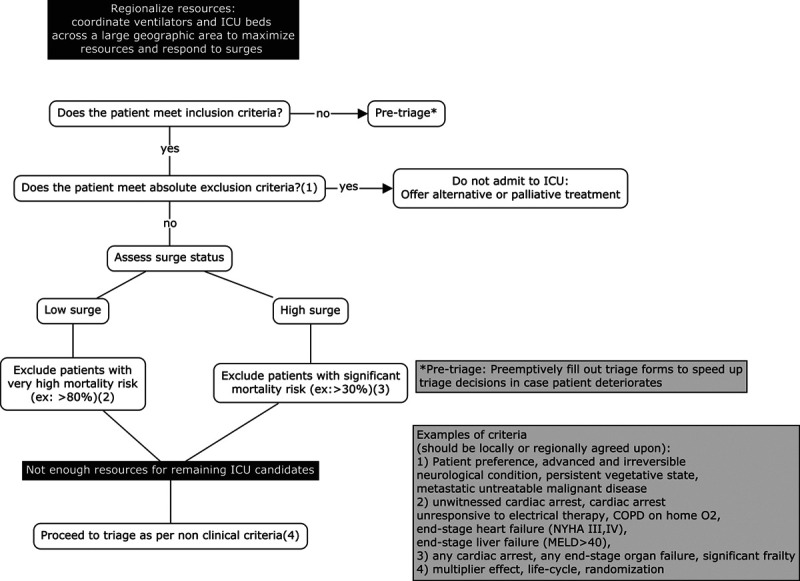
Proposed ICU triage algorithm for access to critical care resources during the coronavirus disease 2019 pandemic. COPD = chronic obstructive pulmonary disease, MELD = model for end-stage liver disease, NYHA = New-York Heart Association.
Limitations
Despite the strengths of our study, its conclusions are bound by a few limitations. First, we did not include articles published in languages other than English or French. We also may have missed local or national policies that are not cross-referenced in any of our search engines or that are only available offline. However, such an endeavor would have been beyond the scope of this work. Finally, only a single author (J.D.) performed the screens and full-text reviews which may have impacted the sensitivity of the review.
Future Research
Optimization of triage and transport practices for critically ill patients will require further research to help address the process deficiencies identified by our study. Namely, environmental scans should be undertaken to identify organizations where triage criteria were objectively evaluated after successful implementation to help benchmark expected process and outcome changes. These environmental scans should not be limited to the realm of intensive care as other patient populations with similar challenges may offer valuable insight (e.g., trauma, PICU, organ transplant) Then, acceptability of identified triage and transport criteria should be determined using Delphi methodology with knowledge users. Finally, formal triage and transport criteria performance should be rigorously tested. A stepped wedge cluster randomized trial may provide the ideal design if the new triage and transfer criteria are implemented within the context of a change in regional health policies (162).
CONCLUSIONS
A systematic review aimed at identifying triage and transport criteria used to prioritize or exclude certain patient populations under different settings helped to generate a list of 200 criteria classified within four themes (patient-, condition-, physician-, and context-related). These criteria may help clinicians and decision-makers devise local, regional, or national ICU triage criteria. A practical example is proposed using the COVID-19 pandemic. However, further high-quality studies or policies yielding specific and measurable criteria tailored to clearly defined patient populations are needed to promote wider clinical adoption in an effort to decrease practice variability and improve transparency.
ACKNOWLEDGMENTS
We acknowledge the work of Nicole Leduc who reviewed an early version of this work.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http:/journals.lww.com/ccmjournal).
Supported, in part, $1,000 grant from the Centre de recherche de l’Université de Montréal was received for this study.
Dr. Dahine received funding from Centre de recherche du Centre Hospitalier de l’Université de Montréal. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Précis: We undertook a systematic review to identify critical care triage criteria. We identified 200 triage criteria among 129 articles. We appraised their robustness and classified them within four themes: patient-, condition-, physician-, and context-related.
REFERENCES
- 1.Joynt GM, Gomersall CD. Making moral decisions when resources are limited – an approach to triage in ICU patients with respiratory failure. South Afr J Crit Care. 2005; 21:34–44 [Google Scholar]
- 2.Bouzat P, Ageron FX, Brun J, et al. ; TRENAU group. A regional trauma system to optimize the pre-hospital triage of trauma patients. Crit Care. 2015; 19:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006; 354:366–378 [DOI] [PubMed] [Google Scholar]
- 4.van Laarhoven JJ, Lansink KW, van Heijl M, et al. Accuracy of the field triage protocol in selecting severely injured patients after high energy trauma. Injury. 2014; 45:869–873 [DOI] [PubMed] [Google Scholar]
- 5.Barnato AE, Kahn JM, Rubenfeld GD, et al. Prioritizing the organization and management of intensive care services in the United States: The PrOMIS Conference. Crit Care Med. 2007; 35:1003–1011 [DOI] [PubMed] [Google Scholar]
- 6.Ramos JG, Perondi B, Dias RD, et al. Development of an algorithm to aid triage decisions for intensive care unit admission: A clinical vignette and retrospective cohort study. Crit Care. 2016; 20:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson DR, Clemmer TP, Applefeld JJ, et al. Regionalization of critical care medicine: Task force report of the American College of Critical Care Medicine. Crit Care Med. 1994; 22:1306–1313 [DOI] [PubMed] [Google Scholar]
- 8.Groupe d’experts en soins intensifs du Québec. Aspects organisationnels des soins intensifs au Québec: Rapport du Groupe d’experts en soins intensifs du Québec. 201323
- 9.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020; 382:2049–2055 [DOI] [PubMed] [Google Scholar]
- 10.Truog RD, Mitchell C, Daley GQ. The toughest triage - allocating ventilators in a pandemic. N Engl J Med. 2020; 382:1973–1975 [DOI] [PubMed] [Google Scholar]
- 11.White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020; 323:1773–1774 [DOI] [PubMed] [Google Scholar]
- 12.Doran GT. There’s a S.M.A.R.T. way to write management’s goals and objectives. Manag Rev. 1981; 70:35–36 [Google Scholar]
- 13.Stelfox HT, Straus SE. Measuring quality of care: Considering measurement frameworks and needs assessment to guide quality indicator development. J Clin Epidemiol. 2013; 66:1320–1327 [DOI] [PubMed] [Google Scholar]
- 14.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009; 339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strosberg MA. Intensive care units in the triage mode. An organizational perspective. Crit Care Clin. 1993; 9:415–424 [PubMed] [Google Scholar]
- 16.Strosberg MA. Intensive care units in the triage mode: An organizational perspective. Hosp Health Serv Adm. 1991; 36:95–109 [PubMed] [Google Scholar]
- 17.Sprung CL, Zimmerman JL, Christian MD, et al. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: Summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med. 2010; 36:428–443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sprung CL, Geber D, Eidelman LA, et al. Evaluation of triage decisions for intensive care admission. Crit Care Med. 1999; 27:1073–1079 [DOI] [PubMed] [Google Scholar]
- 19.Simchen E, Sprung CL, Galai N, et al. Survival of critically ill patients hospitalized in and out of intensive care. Crit Care Med. 2007; 35:449–457 [DOI] [PubMed] [Google Scholar]
- 20.Shanker J, Ghorpode A, Upasani CB. Triage for surgical ICU: Anesthesiologist and intensivist as gatekeepers to ICU. Indian J Crit Care Med. 2006; 10:167–170 [Google Scholar]
- 21.Shamim F, Asghar A, Karam K. Frequency of intensive care unit admission after elective interventional neuroradiological procedures under general anesthesia in a tertiary care hospital. Saudi J Anaesth. 2015; 9:23–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sen A, Callisen HE, Alwardt CM, et al. Adult venovenous extracorporeal membrane oxygenation for severe respiratory failure: Current status and future perspectives. Ann Card Anaesth. 2016; 19:97–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schulman CS, Bibro C, Downey DB, et al. Transferring patients with refractory hypoxemia to a regional extracorporeal membrane oxygenation center: Key considerations for clinicians. AACN Adv Crit Care. 2014; 25:351–364 [DOI] [PubMed] [Google Scholar]
- 24.Scheinkestel CD. The evolution of the intensivist: From health care provider to economic rationalist and ethicist. Med J Aust. 1996; 164:310–312 [DOI] [PubMed] [Google Scholar]
- 25.Roupie E. Admission or refusal decisions for intensive care. [French]. Reanimation Urgences. 2001; 10:679–684 [Google Scholar]
- 26.Reignier J, Dumont R, Katsahian S, et al. Patient-related factors and circumstances surrounding decisions to forego life-sustaining treatment, including intensive care unit admission refusal. Crit Care Med. 2008; 36:2076–2083 [DOI] [PubMed] [Google Scholar]
- 27.Powell T, Christ KC, Birkhead GS. Allocation of ventilators in a public health disaster. Disaster Med Public Health Prep. 2008; 2:20–26 [DOI] [PubMed] [Google Scholar]
- 28.Patroniti N, Zangrillo A, Pappalardo F, et al. The Italian ECMO network experience during the 2009 influenza A(H1N1) pandemic: Preparation for severe respiratory emergency outbreaks. Intensive Care Med. 2011; 37:1447–1457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pateron D, Boumendil A, Garrouste-Orgeas M, et al. Criteria of intensive care unit admission for oldest old patients from emergency department: Determination of a list by Delphi method. [French]. Jeur. 2008; 21:56–63 [Google Scholar]
- 30.Osborne ML. Physician decisions regarding life support in the intensive care unit. Chest. 1992; 101:217–224 [DOI] [PubMed] [Google Scholar]
- 31.Osborne M, Evans TW. Allocation of resources in intensive care: A transatlantic perspective. Lancet. 1994; 343:778–780 [DOI] [PubMed] [Google Scholar]
- 32.Orsini J, Butala A, Ahmad N, et al. Factors influencing triage decisions in patients referred for ICU admission. J Clin Med Res. 2013; 5:343–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Orens JB, Estenne M, Arcasoy S, et al. International guidelines for the selection of lung transplant candidates: 2006 update—a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2006; 25:745–755 [DOI] [PubMed] [Google Scholar]
- 34.Oerlemans AJM, Wollersheim H, van Sluisveld N, et al. Rationing in the intensive care unit in case of full bed occupancy: A survey among intensive care unit physicians. BMC Anesthesiol. 2016; 16:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oddi LF, Huerta SR. Which patient gets the critical care bed?. Dimens Crit Care Nurs. 1990; 9:288–295 [DOI] [PubMed] [Google Scholar]
- 36.Nates JL, Nunnally M, Kleinpell R, et al. ICU admission, discharge, and triage guidelines: A framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016; 44:1553–1602 [DOI] [PubMed] [Google Scholar]
- 37.Ñamendys-Silva SA, Plata-Menchaca EP, Rivero-Sigarroa E, et al. Opening the doors of the intensive care unit to cancer patients: A current perspective. World J Crit Care Med. 2015; 4:159–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Murphy DJ, Matchar DB. Life-sustaining therapy. A model for appropriate use. JAMA. 1990; 264:2103–2108 [PubMed] [Google Scholar]
- 39.Murphy DJ, Barbour E. GUIDe (guidelines for the use of intensive care in Denver): A community effort to define futile and inappropriate care. New Horiz. 1994; 2:326–331 [PubMed] [Google Scholar]
- 40.Morton B, Tang L, Gale R, et al. Performance of influenza-specific triage tools in an H1N1-positive cohort: P/F ratio better predicts the need for mechanical ventilation and critical care admission. Br J Anaesth. 2015; 114:927–933 [DOI] [PubMed] [Google Scholar]
- 41.Ministry of Health, New South Wales Influenza Pandemic - Providing Critical Care. 2010, Sydney, NSW, Australia [Google Scholar]
- 42.Mielke J, Martin DK, Singer PA. Priority setting in a hospital critical care unit: Qualitative case study. Crit Care Med. 2003; 31:2764–2768 [DOI] [PubMed] [Google Scholar]
- 43.Meyfroidt G, Bollaert PE, Marik PE. Acute ischemic stroke in the ICU: To admit or not to admit?. Intensive Care Med. 2014; 40:749–751 [DOI] [PubMed] [Google Scholar]
- 44.Mery E, Kahn JM. Does space make waste? The influence of ICU bed capacity on admission decisions. Crit Care. 2013; 17:315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McKeown A, Booth MG, Strachan L, et al. Unsuitable for the intensive care unit: What happens next?. J Palliat Med. 2011; 14:899–903 [DOI] [PubMed] [Google Scholar]
- 46.Marriott D, Turner Z, Robin N, et al. To admit or not to admit? The suitability of critical care admission criteria. Crit Care. 2012; 16:S181–S182 [Google Scholar]
- 47.Markou N, Demopoulou E, Myrianthefs P. The critically ill patient with cancer - indications for intensive care unit admission and outcomes. J Buon. 2008; 13:469–478 [PubMed] [Google Scholar]
- 48.Malak S, Sotto JJ, Ceccaldi J, et al. Ethical and clinical aspects of intensive care unit admission in patients with hematological malignancies: Guidelines of the ethics commission of the French society of hematology. Adv Hematol. 2014; 2014:704318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Luchetti M. Intensive care resource allocation: When difficult choices have to be made. Br J Med Pract. 2013; 6:a633 [Google Scholar]
- 50.Louriz M, Abidi K, Akkaoui M, et al. Determinants and outcomes associated with decisions to deny or to delay intensive care unit admission in Morocco. Intensive Care Med. 2012; 38:830–837 [DOI] [PubMed] [Google Scholar]
- 51.Lindvig KP, Teisner AS, Kjeldsen J, et al. Allocation of patients with liver cirrhosis and organ failure to intensive care: Systematic review and a proposal for clinical practice. World J Gastroenterol. 2015; 21:8964–8973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lim SC, Fok AC, Ong YY. Patient outcome and intensive care resource allocation using APACHE II. Singapore Med J. 1996; 37:488–491 [PubMed] [Google Scholar]
- 53.Lecuyer L, Chevret S, Thiery G, et al. The ICU trial: A new admission policy for cancer patients requiring mechanical ventilation. Crit Care Med. 2007; 35:808–814 [DOI] [PubMed] [Google Scholar]
- 54.Leclercq F, Iemmi A, Macia JC, et al. Transcatheter aortic valve implantation without intensive care unit admission is possible in selected “low risk” patients. Circulation. 2015; 132:A10111 [Google Scholar]
- 55.Lazzeri C, Bernardo P, Sori A, et al. Venous-arterial extracorporeal membrane oxygenation for refractory cardiac arrest: A clinical challenge. Eur Heart J Acute Cardiovasc Care. 2013; 2:118–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.La commission d’éthique de la société française d’hématologie, la société de réanimation en langue française, le groupe francophone de réanimation et urgences pédiatriques. Clinical and ethical aspects of admission in intensive care unit of patients with malignant hemopathies. Réanimation. 2010; 19:699–705 [Google Scholar]
- 57.Kose I, Zİncircioglu C, Cakmak M, et al. Postoperative patients in the intensive care unit: Identifying those who do not really need it. J Crit Care. 2015; 30:1295–1298 [DOI] [PubMed] [Google Scholar]
- 58.Kaposy C, Bandrauk N, Pullman D, et al. Adapting the Hamilton Health Sciences critical care pandemic triage protocol. Healthc Q. 2010; 13:60–63 [DOI] [PubMed] [Google Scholar]
- 59.Joynt GM, Gomersall CD. What do “triage” and “informed consent” really mean in practice?. Anaesth Intensive Care. 2011; 39:541–544 [DOI] [PubMed] [Google Scholar]
- 60.Jemison T. ICU guidelines. Care levels defined. US Med. 1983; 19:2, 16. [PubMed] [Google Scholar]
- 61.Javidfar J, Bacchetta M. Bridge to lung transplantation with extracorporeal membrane oxygenation support. Curr Opin Organ Transplant. 2012; 17:496–502 [DOI] [PubMed] [Google Scholar]
- 62.Iapichino G, Corbella D, Minelli C, et al. Reasons for refusal of admission to intensive care and impact on mortality. Intensive Care Med. 2010; 36:1772–1779 [DOI] [PubMed] [Google Scholar]
- 63.Howe DC. Observational study of admission and triage decisions for patients referred to a regional intensive care unit. Anaesth Intensive Care. 2011; 39:650–658 [DOI] [PubMed] [Google Scholar]
- 64.Hick JL, Rubinson L, O’Laughlin DT, et al. Clinical review: Allocating ventilators during large-scale disasters - problems, planning, and process. Crit Care. 2007; 11:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hick JL, O’Laughlin DT. Concept of operations for triage of mechanical ventilation in an epidemic. Acad Emerg Med. 2006; 13:223–229 [DOI] [PubMed] [Google Scholar]
- 66.Gruppo di Studio ad Hoc della Commissione di Bioetica della SIAARTI. SIAARTI guidelines for admission to and discharge from intensive care units and for limitation of treatment in intensive care. Minerva Anestesiol. 2003; 69:101–111, 111–118 [PubMed] [Google Scholar]
- 67.Garrouste-Orgeas M, Timsit JF, Montuclard L, et al. Decision-making process, outcome, and 1-year quality of life of octogenarians referred for intensive care unit admission. Intensive Care Med. 2006; 32:1045–1051 [DOI] [PubMed] [Google Scholar]
- 68.Garrouste-Orgeas M, Montuclard L, Timsit JF, et al. ; French ADMISSIONREA Study Group. Predictors of intensive care unit refusal in French intensive care units: A multiple-center study. Crit Care Med. 2005; 33:750–755 [DOI] [PubMed] [Google Scholar]
- 69.Garrouste-Orgeas M, Montuclard L, Timsit JF, et al. Triaging patients to the ICU: A pilot study of factors influencing admission decisions and patient outcomes. Intensive Care Med. 2003; 29:774–781 [DOI] [PubMed] [Google Scholar]
- 70.Frolic A, Kata A, Kraus P. Development of a critical care triage protocol for pandemic influenza: Integrating ethics, evidence and effectiveness. Healthc Q. 2009; 12:54–62 [DOI] [PubMed] [Google Scholar]
- 71.Franco M, Smith C. Admission location triage by grace score 2.0 in ST elevation myocardial infarction (STEMI) results in improved resource utilization in low risk patients. J Am College Cardiol. 2015; 65:A126 [Google Scholar]
- 72.Extracorporeal Life Support Organization ELSO Guidelines for Cardiopulmonary Extracorporeal Life Support, Version 1.4. 2017, Ann Arbor, MI [Google Scholar]
- 73.Elnour S, Shankar-Hari M. The critically ill patient: Making the referral to intensive care. Brit J Hosp Med (London, England: 2005). 2011; 72:M154–M156 [DOI] [PubMed] [Google Scholar]
- 74.Devereaux AV, Dichter JR, Christian MD, et al. ; Task Force for Mass Critical Care. Definitive care for the critically ill during a disaster: A framework for allocation of scarce resources in mass critical care: From a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest. 2008; 133:51S–66S [DOI] [PubMed] [Google Scholar]
- 75.Department of Health Pandemic. Flu: Management of Demand and Capacity in Healthcare Organisations. 2009, London, United Kingdom Government [Google Scholar]
- 76.Dawson S, Runk JA. Right patient? Right bed? A question of appropriateness. AACN Clin Issues. 2000; 11:375–385 [DOI] [PubMed] [Google Scholar]
- 77.Dawson JA. Admission, discharge, and triage in critical care. Principles and practice. Crit Care Clin. 1993; 9:555–574 [PubMed] [Google Scholar]
- 78.Das AM, Sood N, Hodgin K, et al. Development of a triage protocol for patients presenting with gastrointestinal hemorrhage: A prospective cohort study. Crit Care. 2008; 12:R57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Darmon M, Azoulay E. Critical care management of cancer patients: Cause for optimism and need for objectivity. Curr Opin Oncol. 2009; 21:318–326 [DOI] [PubMed] [Google Scholar]
- 80.Daniel M. Bedside resource stewardship in disasters: A provider’s dilemma practicing in an ethical gap. J Clin Ethics. 2012; 23:331–335 [PubMed] [Google Scholar]
- 81.Dahm P, Tuttle-Newhall JE, Nimjee SM, et al. Indications for admission to the surgical intensive care unit after radical cystectomy and urinary diversion. J Urol. 2001; 166:189–193 [PubMed] [Google Scholar]
- 82.Crippen D, Whetstine L. ICU resource allocation: Life in the fast lane. Crit Care. 1999; 3:R47–R51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Courtney PM, Melnic CM, Gutsche J, et al. Which patients need critical care intervention after total joint arthroplasty?: A prospective study of factors associated with the need for intensive care following surgery. Bone Joint J. 2015; 97-B:1512–1518 [DOI] [PubMed] [Google Scholar]
- 84.Conrad SA. Extracorporeal cardiopulmonary resuscitation. Egypt J Crit Care Med. 2016; 4:11–15 [Google Scholar]
- 85.Conlon KM, Ruhren C, Johansen S, et al. Developing and implementing a plan for large-scale burn disaster response in New Jersey. J Burn Care Res. 2014; 35:e14–e20 [DOI] [PubMed] [Google Scholar]
- 86.Conlon KM, Martin S. ‘Just send them all to a burn centre’: Managing burn resources in a mass casualty incident. J Bus Contin Emer Plan. 2011; 5:150–160 [PubMed] [Google Scholar]
- 87.Cohen RI, Eichorn A, Silver A. Admission decisions to a medical intensive care unit are based on functional status rather than severity of illness. A single center experience. Minerva Anestesiol. 2012; 78:1226–1233 [PubMed] [Google Scholar]
- 88.Cohen CB. Ethical problems of intensive care. Anesthesiology. 1977; 47:217–227 [DOI] [PubMed] [Google Scholar]
- 89.Christian MD, Sprung CL, King MA, et al. ; Task Force for Mass Critical Care; Task Force for Mass Critical Care. Triage: Care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014; 146:e61S–e74S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Christian MD, Joynt GM, Hick JL, et al. Chapter 7. Critical care triage. Intensive Care Med. 2010; 36Suppl 1S55–S64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Christian MD, Hawryluck L, Wax RS, et al. Development of a triage protocol for critical care during an influenza pandemic. CMAJ. 2006; 175:1377–1381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chipp E, Warner RM, McGill DJ, et al. Air ambulance transfer of adult patients to a UK regional burns centre: Who needs to fly?. Burns. 2010; 36:1201–1207 [DOI] [PubMed] [Google Scholar]
- 93.Chalmers JD, Taylor JK, Mandal P, et al. Validation of the Infectious Diseases Society of America/American Thoratic Society minor criteria for intensive care unit admission in community-acquired pneumonia patients without major criteria or contraindications to intensive care unit care. Clin Infect Dis. 2011; 53:503–511 [DOI] [PubMed] [Google Scholar]
- 94.Carr BG, Meisel ZF. Patient-centered regionalization: Including the patient voice in hospital selection for time-critical illness. Acad Emerg Med. 2014; 21:214–216 [DOI] [PubMed] [Google Scholar]
- 95.Capuzzo M, Moreno RP, Alvisi R. Admission and discharge of critically ill patients. Curr Opin Crit Care. 2010; 16:499–504 [DOI] [PubMed] [Google Scholar]
- 96.Callahan D. Old age and new policy. JAMA. 1989; 261:905–906 [PubMed] [Google Scholar]
- 97.Bohman JK, Hyder JA, Iyer V, et al. Early prediction of extracorporeal membrane oxygenation eligibility for severe acute respiratory distress syndrome in adults. J Crit Care. 2016; 33:125–131 [DOI] [PubMed] [Google Scholar]
- 98.Blanch L, Abillama FF, Amin P, et al. ; Council of the World Federation of Societies of Intensive and Critical Care Medicine. Triage decisions for ICU admission: Report from the Task Force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2016; 36:301–305 [DOI] [PubMed] [Google Scholar]
- 99.Biscotti M, Agerstrand C, Abrams D, et al. One hundred transports on extracorporeal support to an Extracorporeal Membrane Oxygenation Center. Ann Thorac Surg. 2015; 100:34–39; discussion 39–40 [DOI] [PubMed] [Google Scholar]
- 100.Birnbaum M, Walleck CA. Rationing health care. Impact on critical care. Crit Care Clin. 1993; 9:585–602 [PubMed] [Google Scholar]
- 101.Birch K. Who benefits from intensive care in the field?. J R Army Med Corps. 2009; 155:122–124 [DOI] [PubMed] [Google Scholar]
- 102.Benes R, Brobst K. Ethics in critical care: Practitioners discuss collaborative approaches to decision making. QRB Qual Rev Bull. 1992; 18:33–39 [DOI] [PubMed] [Google Scholar]
- 103.Bekes CE, Bayly RW, Carlon GC, et al. Recommendations for intensive care unit admission and discharge criteria. Crit Care Med. 1988; 16:807–808 [DOI] [PubMed] [Google Scholar]
- 104.Beigi RH, Hodges J, Baldisseri M, et al. Clinical review: Considerations for the triage of maternity care during an influenza pandemic - one institution’s approach. Crit Care. 2010; 14:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Baruch M, Messer B. Criteria for intensive care unit admission and severity of illness. Surgery (United Kingdom). 2015; 33:158–164 [Google Scholar]
- 106.Bargues L, Fall MM. Afflux massif de brûlés: La doctrine française de triage en temps de paix [French]. Ann Burns Fire Disasters. 2015; 28:50–56 [PMC free article] [PubMed] [Google Scholar]
- 107.Azoulay E, Soares M, Darmon M, et al. Intensive care of the cancer patient: Recent achievements and remaining challenges. Ann Intensive Care. 2011; 1:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Azoulay E, Pochard F, Chevret S, et al. ; PROTOCETIC Group. Compliance with triage to intensive care recommendations. Crit Care Med. 2001; 29:2132–2136 [DOI] [PubMed] [Google Scholar]
- 109.Azoulay E, Afessa B. The intensive care support of patients with malignancy: Do everything that can be done. Intensive Care Med. 2006; 32:3–5 [DOI] [PubMed] [Google Scholar]
- 110.Augier R, Hambleton IR, Harding H. Triage decisions and outcome among the critically ill at the University Hospital of the West Indies. West Indian Med J. 2005; 54:181–186 [DOI] [PubMed] [Google Scholar]
- 111.Artru F, Louvet A. Admission of cirrhotic patients in intensive care unit: Is the Child-Pugh score a useful tool?. Reanimation. 2015; 24:389–397 [Google Scholar]
- 112.American College of Critical Care Medicine of the Society of Critical Care Medicine Guidelines for ICU Admission, Discharge, and Triage 1999; 27:633–638 [PubMed] [Google Scholar]
- 113.Alentorn A, Weiss N, Delattre JY, et al. Adult patients with primary malignant brain tumor and admission to the intensive care unit. Reanimation. 2015; 24:424–432 [Google Scholar]
- 114.Albertine P, Borofsky S, Brown D, et al. Small subdural hemorrhages: Is routine intensive care unit admission necessary?. Am J Emerg Med. 2016; 34:521–524 [DOI] [PubMed] [Google Scholar]
- 115.Teno JM, Lynn J. Using SUPPORT (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment) to GUIDe (Guidelines for Use of Intensive Care in Denver) our fix on futility. Hosp Ethics. 1995; 11:1–5 [PubMed] [Google Scholar]
- 116.Vincent JL, Artigas A, Bihari D, et al. Guidelines for the utilisation of intensive care units. European Society of Intensive Care Medicine. Intensive Care Med 1994. 20:163–164 [DOI] [PubMed] [Google Scholar]
- 117.Sprung CL, Danis M, Armstrong C, et al. ; U.S. Department of Veterans Affairs, VACO [VA Central Office] Bioethics Committee, Subcommittee on Futility (Chairperson: Dorothy Rasinski Gregory). Futility guidelines: A resource for decisions about withholding and withdrawing treatment. NCCE News. 1994; 23 Insert1–5 [PubMed] [Google Scholar]
- 118.Consensus statement on the triage of critically ill patients. Society of Critical Care Medicine Ethics Committee. JAMA. 1994; 271:1200–1203 [PubMed] [Google Scholar]
- 119.Wise MP, Barnes RA, Baudouin SV, et al. ; British Committee for Standards in Haematology. Guidelines on the management and admission to intensive care of critically ill adult patients with haematological malignancy in the UK. Br J Haematol. 2015; 171:179–188 [DOI] [PubMed] [Google Scholar]
- 120.Winsor S, Bensimon CM, Sibbald R, et al. Identifying prioritization criteria to supplement critical care triage protocols for the allocation of ventilators during a pandemic influenza. Healthc Q. 2014; 17:44–51 [DOI] [PubMed] [Google Scholar]
- 121.Williams KE. Extracorporeal membrane oxygenation for acute respiratory distress syndrome in adults. AACN Adv Crit Care. 2013; 24:149–160 [DOI] [PubMed] [Google Scholar]
- 122.Wilkens EP, Klein GM. Mechanical ventilation in disaster situations: A new paradigm using the AGILITIES score system. Am J Disaster Med. 2010; 5:369–384 [PubMed] [Google Scholar]
- 123.White DB, Katz MH, Luce JM, et al. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Ann Intern Med. 2009; 150:132–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Veterans Health Administration Meeting the Challenge of Pandemic Influenza: Ethical Guidance for Leaders and Health Care Professionals in the Veterans Health Administration. 2010. 2018. Available at: https://www.ethics.va.gov/docs/pandemicflu/Meeting_the_Challenge_of_Pan_Flu-Ethical_Guidance_VHA_20100701.pdf. Accessed July 19. [Google Scholar]
- 125.Vanhecke TE, Gandhi M, McCullough PA, et al. Outcomes of patients considered for, but not admitted to, the intensive care unit. Crit Care Med. 2008; 36:812–817 [DOI] [PubMed] [Google Scholar]
- 126.van Diepen S, Lin M, Bakal JA, et al. Do stable non-ST-segment elevation acute coronary syndromes require admission to coronary care units?. Am Heart J. 2016; 175:184–192 [DOI] [PubMed] [Google Scholar]
- 127.Toffart AC, Sakhri L, Potton L, et al. Intensive care unit admission for lung cancer: Which patients and for which benefits?. [French]. Reanimation. 2013; 22:54–61 [Google Scholar]
- 128.Toffart AC, Duruisseaux M, Sakhri L, et al. ICU admissions in thoracic oncology. [French]. Revue des Maladies Respiratoires Actualites. 2015; 7:545, 553 [Google Scholar]
- 129.Thiery G, Darmon M, Azoulay E. Deciding intensive care unit-admission for critically ill cancer patients. Indian J Crit Care Med. 2007; 11:12–18 [Google Scholar]
- 130.Teres D. Civilian triage in the intensive care unit: The ritual of the last bed. Crit Care Med. 1993; 21:598–606 [DOI] [PubMed] [Google Scholar]
- 131.Taylor B, Kemp V, Goldhill D, et al. Critical care contingency planning: Phased responses and triaging framework. J Intensive Care Soc. 2008; 9:16–19 [Google Scholar]
- 132.Swenson MD. Scarcity in the intensive care unit: Principles of justice for rationing ICU beds. Am J Med. 1992; 92:551–555 [DOI] [PubMed] [Google Scholar]
- 133.Sprung CL, Danis M, Iapichino G, et al. Triage of intensive care patients: Identifying agreement and controversy. Intensive Care Med. 2013; 39:1916–1924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sprung CL, Artigas A, Kesecioglu J, et al. The Eldicus prospective, observational study of triage decision making in European intensive care units. Part II: Intensive care benefit for the elderly. Crit Care Med. 2012; 40:132–138 [DOI] [PubMed] [Google Scholar]
- 135.Sottiaux T, Mélot CH. [Refusal of admission in intensive care unit]. Rev Med Liege. 2005; 60:30–34 [PubMed] [Google Scholar]
- 136.Smith G, Nielsen M. ABC of intensive care. Criteria for admission. BMJ (Clin Res Ed). 1999; 318:1544–1547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Altevogt B, Stroud C, Hanson S, et al. Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations: A Letter Report. 2009, Washington, DC: Institute of Medicine of the National Academies; [PubMed] [Google Scholar]
- 138.Truog RD. Triage in the ICU. Hastings Cen Rep. 1992; 22:13. [PubMed] [Google Scholar]
- 139.ICU admission criteria need honing to block rationing. Med World News. 1989; 30:16. [PubMed] [Google Scholar]
- 140.Ledingham JGG, Ashworth P, Branthwaite M, et al. Intensive care in the United Kingdom: Report from the King’s Fund panel. Anaesthesia. 1989; 44:428–431 [DOI] [PubMed] [Google Scholar]
- 141.Joynt GM, Gomersall CD, Tan P, et al. Prospective evaluation of patients refused admission to an intensive care unit: Triage, futility and outcome. Intensive Care Med. 2001; 27:1459–1465 [DOI] [PubMed] [Google Scholar]
- 142.Hawryluck L. Ethics review: Position papers and policies–are they really helpful to front-line ICU teams?. Crit Care. 2006; 10:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Wilkinson DJ, Savulescu J. Knowing when to stop: Futility in the ICU. Curr Opin Anaesthesiol. 2011; 24:160–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ehlenbach WJ. The impact of patient preferences on physician decisions in the ICU: Still much to learn. Intensive Care Med. 2013; 39:1647–1649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Boumendil A, Angus DC, Guitonneau AL, et al. ; ICE-CUB study group. Variability of intensive care admission decisions for the very elderly. PLoS One. 2012; 7:e34387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Brannen AL, 2nd, Godfrey LJ, Goetter WE. Prediction of outcome from critical illness. A comparison of clinical judgment with a prediction rule. Arch Intern Med. 1989; 149:1083–1086 [PubMed] [Google Scholar]
- 147.Poses RM, Bekes C, Copare FJ, et al. The answer to “What are my chances, doctor?” Depends on whom is asked: Prognostic disagreement and inaccuracy for critically ill patients. Crit Care Med. 1989; 17:827–833 [DOI] [PubMed] [Google Scholar]
- 148.Poses RM, McClish DK, Bekes C, et al. Ego bias, reverse ego bias, and physicians’ prognostic. Crit Care Med. 1991; 19:1533–1539 [DOI] [PubMed] [Google Scholar]
- 149.Frick S, Uehlinger DE, Zuercher Zenklusen RM. Medical futility: Predicting outcome of intensive care unit patients by nurses and doctors–a prospective comparative study. Crit Care Med. 2003; 31:456–461 [DOI] [PubMed] [Google Scholar]
- 150.Meadow W, Pohlman A, Frain L, et al. Power and limitations of daily prognostications of death in the medical intensive care unit. Crit Care Med. 2011; 39:474–479 [DOI] [PubMed] [Google Scholar]
- 151.Dahine J, Mardini L, Jayaraman D. The perceived likelihood of outcome of critical care patients and its impact on triage decisions: A case-based survey of intensivists and internists in a Canadian, Quaternary Care Hospital Network. PLoS One. 2016; 11:e0149196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Cook DJ, Guyatt GH, Jaeschke R, et al. Determinants in Canadian health care workers of the decision to withdraw life support from the critically ill. Canadian Critical Care Trials Group. JAMA. 1995; 273:703–708 [PubMed] [Google Scholar]
- 153.Garrouste-Orgeas M, Tabah A, Vesin A, et al. The ETHICA study (part II): Simulation study of determinants and variability of ICU physician decisions in patients aged 80 or over. Intensive Care Med. 2013; 39:1574–1583 [DOI] [PubMed] [Google Scholar]
- 154.Emanuel EJ, Pearson SD. Physician autonomy and health care reform. JAMA. 2012; 307:367–368 [DOI] [PubMed] [Google Scholar]
- 155.White ST, Cardenas YR, Nates JL. What every intensivist should know about intensive care unit admission criteria. Rev Bras Ter Intensiva. 2017; 29:414–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zubek L, Szabo L, Horvath L, et al. The effect of religiosity on end-of-life decisions in Hungarian intensive care units. Intensive Care Med. 2011; 37:S71. [DOI] [PubMed] [Google Scholar]
- 157.Weng L, Joynt GM, Lee A, et al. ; Chinese Critical Care Ethics Group. Attitudes towards ethical problems in critical care medicine: The Chinese perspective. Intensive Care Med. 2011; 37:655–664 [DOI] [PubMed] [Google Scholar]
- 158.Escher M, Perneger TV, Chevrolet JC. National questionnaire survey on what influences doctors’ decisions about admission to intensive care. BMJ. 2004; 329:425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Maves RC, Downar J, Dichter JR, et al. ; ACCP Task Force for Mass Critical Care. Triage of scarce critical care resources in COVID-19 an implementation guide for regional allocation: An expert panel report of the Task Force for Mass Critical Care and the American College of Chest Physicians. Chest. 2020; 158:212–225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sprung CL, Joynt GM, Christian MD, et al. Adult ICU triage during the coronavirus disease 2019 pandemic: Who will live and who will die? Recommendations to improve survival. Crit Care Med. 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020; 395:1054–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hemming K, Haines TP, Chilton PJ, et al. The stepped wedge cluster randomised trial: Rationale, design, analysis, and reporting. BMJ. 2015; 350:h391. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


