Abstract
Rationale
Adolescents and young adults were identified internationally as a group with potentially low compliance rates with public health measures aimed at curbing the spread of coronavirus disease 2019 (COVID-19). Although non-compliance research during pandemics has typically focused on concurrent correlates, less is known about how prior social and psychological risk factors are associated with non-compliance during pandemics.
Objective
This paper leverages a prospective-longitudinal cohort study with data before and during the pandemic to describe patterns of non-compliance with COVID- 19 related public health measures in young adults and to identify which characteristics increase the risk of non-compliance.
Methods
Data came from an ongoing cohort study in Zurich, Switzerland (n=737). Non-compliance with public health measures and concurrent correlates were measured at age 22. Antecedent sociodemographic, social, and psychological factors were measured at ages 15-20. Young adults generally complied with COVID-19 public health measures, although non-compliance with some measures (e.g., cleaning/disinfecting mobile phones, standing 1.5-2 meters apart) was relatively higher.
Results
Non-compliance, especially with hygiene-related measures, was more prevalent in males, and in individuals with higher education, higher SES, and a nonmigrant background. Non-compliance was higher in young adults who had previously scored high on indicators of “antisocial potential,” including low acceptance of moral rules, pre-pandemic legal cynicism, low shame/guilt, low self-control, engagement in delinquent behaviors, and association with delinquent peers. Young adults with low trust, including in the government’s measures for fighting the virus, also complied less.
Conclusions
In order to increase voluntary compliance with COVID-19 measures, public health campaigns should implement strategies that foster moral obligation and trust in authorities, or leverage trustworthy individuals in the community to disseminate information. For young adults with low self-control, self-monitoring, environmental restructuring, or nudging may increase compliance. Long-term investments into integrating youth with antisocial potential into society may decrease rule-breaking behaviors, including during pandemics when compliance saves lives.
1. Introduction
Adolescents and young adults have been identified internationally as a group with potentially low compliance with public health measures aimed at curbing the spread of coronavirus disease 2019 [COVID-19], especially with social distancing measures (Barari et al., 2020; Cohen et al., 2020; Park et al., 2020; Roy-Chowdhury et al., 2020). In mid-March 2020, the World Health Organization [WHO] issued a special appeal to young people for increased compliance (Nebehay, 2020). This group often displays only mild or no symptoms of COVID-19, while still being infectious (Centers for Disease Control [CDC] COVID-19 Response Team, 2020; Pan et al., 2020). Thus, their potential for spreading the virus is high, considering that they also tend to have large social networks and active social lives (Andrews et al., 2020; Cohen et al., 2020; Wrzus et al., 2013).
Non-compliance research with this and previous pandemics has typically focused on proximal, concurrent correlates in explaining non-compliance with preventive measures (see Bults et al., 2015; Clark et al., 2020; Webster et al., 2020). For example, individuals who perceive a high risk of contracting or being harmed by the virus, who seek out more information, have trust in the government, and feel a moral obligation to comply are more likely to adopt preventive measures (Bults et al., 2015; Cho and Lee, 2015; Clark et al., 2020; Harper et al., 2020; Lammers et al., 2020; Prati et al., 2011a, 2011b; Rubin et al., 2009; Setbon et al., 2011; Shao and Hao, 2020; Van der Weerd et al., 2011; Webster et al., 2020). Certain sociodemographic characteristics, such as sex (i.e., female) and higher education, have also been associated with greater compliance (Bish and Michie, 2010; Brouard et al., 2020), whereas individuals from other demographic backgrounds may lack the practical capacity to comply due to their occupation or economic concerns (Bodas and Peleg, 2020; Kuiper et al., 2020; Webster et al., 2020).
Less is known about how prior social and psychological risk factors are associated with non-compliance during pandemics (Clark et al., 2020; Oosterhoff et al., 2020). In non-pandemic times, young people with characteristics of "antisocial potential" (Farrington, 2019)—that is low self-control, high engagement in delinquent behaviors, high association with delinquent peers, low acceptance of moral rules, legal cynicism, and low shame or guilt—are more likely to engage in rule-breaking behaviors. This makes the characteristics that constitute antisocial potential strong candidates as precursors of non-compliance with measures aimed at curbing the spread of the virus (see e.g., Andrews et al., 2020). Emerging evidence suggests that impulsivity and certain personality traits such as amorality, egoism, and psychopathy, are associated with non-compliance with COVID-19-related public health measures (Kuiper et al., 2020; Zajenowski et al., 2020; Zettler et al., 2020).
Whether earlier antisocial characteristics are associated with later non-compliance with COVID-19 public health measures is best examined using representative data featuring information on young people before and during the COVID-19 pandemic. The current analysis thus leverages a prospective-longitudinal study that began data collection years before the pandemic, and that most recently also collected data in April 2020. During the COVID-19 pandemic, young adults reported their non-compliance with public health measures, and attitudinal and situational characteristics, such as risk-status, information seeking, and trust in government. Before the pandemic, these same participants were extensively characterized in terms of their sociodemographic characteristics and the characteristics that contribute to antisocial potential during their adolescent and young adult years. We use the data to describe patterns of non-compliance with COVID-19 related public health measures in young adults and to identify which characteristics of adolescents and young adults increase risk for future and concurrent non-compliance.
Data were collected in Zurich, Switzerland's largest city. During the initial weeks of the COVID-19 outbreak in Europe, Switzerland was among the ten most affected countries worldwide, with one of the highest per-capita rates of infection (Salathé et al., 2020). Public health recommendations were first introduced on 28 February; from 16 March to April 26, 2020, Switzerland went into its first country-wide “lockdown”. Policies during that time included increased social distance and hygiene, prohibition of social gatherings of >5 people, and staying home whenever possible (Federal Office of Public Health [FOPH], 2020a; World Health Organization [WHO], 2020). Consistent information and messaging regarding these public health measures was widely broadcasted and disseminated by government representatives and the Federal Office for Public Health through multiple media channels (i.e., TV, radio, social media, poster campaigns, internet). Messaging was highly visible in public space (e.g., public transport). Information on the virus and restrictions was made available in 25 languages (FOPH, 2020b).
2. Method
2.1. Sample and procedures
Data came from the Zurich Project on Social Development from Childhood to Adulthood (z-proso), an ongoing prospective-longitudinal study on the development of child and adolescent prosocial and problem behavior. The cohort comprises children who entered 1st grade in one of the 56 primary schools in Zurich, in 2004. The initial target sample of schools was selected using random sampling procedures in which disadvantaged school districts were oversampled. The study consists of eight waves of child interviews at ages 7, 8, 9, 11, 13, 15, 17, and 20. Details on the original sample selection and attrition between waves 1 and 7 are available elsewhere (see Eisner et al., 2011; Eisner et al., 2019). Participants who had participated at the age-20 assessment were invited to participate in a COVID-19 online study at age 22 years old. The current analysis primarily uses data from the April 2020 COVID-19 assessment, and the age 15, 17, and 20 assessments. Subjects provided written informed consent for their study participation at ages 13–20. At age 22, informed consent was obtained online, as an extension to the age-20 written consent. Until age 15, parents could opt their child out of the study.
The sample for the COVID-19 data collection was based on participants of the z-proso age-20 assessment. Out of the 1180 participants at age 20, 21 were not contacted due to unclear status or invalid contact information. Out of the 1159 cases contacted, 786 participants responded (67.8% of the age-20 sample in 2018; 46.9% of original target sample in 2004). Given attrition over time, sampling weights were used in all analyses to allow generalizations back to the original recruitment population (see Supplementary Appendix A for more details). We excluded those no longer living in Switzerland during the time of the survey and those who had incomplete data on measures of interest here (final sample n = 737). Descriptive characteristics of the weighted sample are reported in Table 1 . Notably, 50% of the current sample had a migrant background (i.e., both parents born abroad), but have been living in Switzerland at least since the start of primary school. The largest proportion of migrant parents in the sample were born in the former Yugoslavia, Sri Lanka, Portugal, Germany, and Turkey. The study population is largely representative of the youth population in Zurich.
Table 1.
Descriptive statistics for weighted sample.
| Variables | N | Mean/% | Linearized SE | Min | Max |
|---|---|---|---|---|---|
| Outcome | |||||
| Overall COVID-19 non-compliance | 737 | 2.47 | 0.07 | 0 | 13 |
| Hygiene COVID-19 non-compliance | 737 | 1.77 | 0.05 | 0 | 6 |
| Social distancing COVID-19 non-compliance | 737 | 0.71 | 0.04 | 0 | 7 |
| Antecedent factors (ages 17 and 20) | |||||
| Social bonds and lifestyle | |||||
| Low parental involvement (age 17)a,f | 713 | 2.04 | 0.02 | 1 | 4 |
| Low parental monitoring (age 17)a,f | 712 | 1.99 | 0.02 | 1.3 | 4 |
| Low teacher-child bond (age 17)b,f | 673 | 1.85 | 0.02 | 1 | 4 |
| Low school commitment (age 17)b,f | 673 | 4.57 | 0.02 | 1.6 | 6.2 |
| Low social support (age 20)b,f | 736 | 1.75 | 0.03 | 1 | 4 |
| Social exclusion (age 20)b | 670 | 1.49 | 0.02 | 1 | 3.8 |
| Low generalized trust (age 20)b,f | 737 | 2.65 | 0.03 | 1 | 4 |
| Active lifestyle (age 20)c | 736 | 2.32 | 0.02 | 1 | 4 |
| Attitudes toward the law and police | |||||
| Legal cynicism (age 20)b | 737 | 2.07 | 0.02 | 1 | 4 |
| Low police legitimacy (age 20)b,f | 734 | 2.38 | 0.03 | 1 | 4 |
| Deviant peers and behavior | |||||
| Deviant peers (age 20) | 654 | 0.01 | 0.04 | −2.2 | 2.9 |
| Antisocial behavior (age 20) | 736 | 1.39 | 0.06 | 0 | 9 |
| Dispositional factors | |||||
| Low self-control (age 20)b,f | 737 | 2.03 | 0.02 | 1 | 3.8 |
| Low self-efficacy (age 20)b,f | 737 | 2.12 | 0.02 | 1 | 4 |
| Low guilt/shame (age 20)b,f | 737 | 2.08 | 0.02 | 1 | 4 |
| Concurrent factors (age 23) | |||||
| Family member has conditions increasing risk | 737 | 57% | 0.02 | 0 | 1 |
| Respondent has conditions increasing risk | 737 | 12% | 0.01 | 0 | 1 |
| Most do not follow instructionsb,f | 737 | 1.98 | 0.02 | 1 | 4 |
| Low moral normsd,f | 737 | 2.22 | 0.04 | 1 | 7 |
| COVID-19 moral disengagementb,f | 734 | 1.92 | 0.02 | 1 | 4 |
| Low trust in governmentb,f | 737 | 2.29 | 0.03 | 1 | 4 |
| Low information-seekinge,f | 737 | 3.34 | 0.05 | 1 | 5 |
| Sociodemographic background | 737 | 3.05 | 0.62 | 1 | 4 |
| Sex (1 = male) | 737 | 51% | 0.02 | 0 | 1 |
| SES quartiles | |||||
| Q4 (high SES) | 164 | 21% | 0.02 | – | – |
| Q3 | 195 | 25% | 0.02 | – | – |
| Q2 | 176 | 24% | 0.02 | – | – |
| Q1 (low SES) | 185 | 29% | 0.02 | – | – |
| Migrant background (1 = both parents born abroad) | 727 | 50% | 0.02 | 0 | 1 |
| Education level | |||||
| Gymnasium (high) | 213 | 27% | 0.02 | – | – |
| Secondary school A | 319 | 44% | 0.02 | – | – |
| Secondary school B/C | 183 | 28% | 0.02 | – | – |
| Special needs education | 9 | 1% | 0.00 | – | – |
Note. All estimates are computed accounting for sample weights. SE = standard error.
Answer categories range from 1 (never) to 4 (always).
Answer categories range from 1 (fully false) to 4 (fully true).
Answer categories range from 1 (never) to 6 (almost every day).
Answer categories range from 1 (not at all bad) to 7 (very bad).
Answer categories range from 1 (less than once per day) to 5 (pretty much constant).
Reverse coded so higher values indicate higher scores on a given risk factor (e.g. low parental involvement).
At ages 15 and 17, participants completed paper/pencil questionnaires in classrooms outside of regular lesson times. At age 20, participants completed surveys on a computer at a university research laboratory. Interviews typically lasted 90 min. Adolescents received a cash incentive for their participation in each wave: ~$50 at age 15, ~$60 at age 17, and ~$75 at age 20. Respondents in the age 22 COVID-19 survey were entered into a lottery with the opportunity to win one of 50 prizes of ~$100.
Those who had participated at age 20 were sent an invitation with a personalized link by SMS and e-mail. Data collection began during week 4 of the Swiss lockdown and ended during week 5. Invitations were sent on April 8, 2020, with reminders on 11 and 13 April. In total, participants were given 7 days to complete the survey.
Ethical approval was obtained by the Ethics Committee of the Faculty of Arts and Social Sciences of the University of Zurich.
2.2. Measures
2.2.1. Dependent variable
Non-compliance with COVID-19 public health measures. Respondents were asked whether or not they adopted 13 protective behaviors, reflecting national and international recommendations (CDC, 2020; FOPH, 2020; WHO, 2020). These can broadly be subdivided into hygiene measures (e.g., wash hands regularly, use hand disinfectant, cough into an elbow or cloth, do not touch face, wash hands after coughing or sneezing, disinfect mobile phone) and social distancing behaviors (e.g., stay at home, adhere to social distancing [1.5–2 m], stay at home with symptoms, avoid at-risk persons, do not shake hands). Wearing a face mask was included in the survey, but was excluded from analyses since this was explicitly not recommended by the Swiss government at the time. Accordingly, only 8% of participants reported wearing a face mask.
For each of the 13 behaviors, respondents indicated whether or not they followed the recommendation. A sum score was created to reflect how many of the 13 behaviors the respondent failed to comply with. Separate sum scores were created for non-compliance with hygiene and social distancing measures, respectively.
2.2.2. Sociodemographic variables
We included a range of sociodemographic variables that are relevant for understanding protective health behaviors and non-compliance: sex, socioeconomic status [SES] and educational level measured at age 15, and migrant background. Sex was coded 0 for females and 1 for males. SES was measured based on the primary caregiver's occupation when the respondent was 15 years old or younger. Codes were transformed into an International Socioeconomic Index of occupational status [ISEI] score (Ganzenboom et al., 1992). The respondent's SES score was based on the highest ISEI recorded for each household, and was divided into quartiles for analysis. The respondent's educational track level was measured at age 15. Respondents who were in Gymnasium (highest, college-track level) were the reference group (coded 0), compared to lower level education groups: secondary school A (higher non-college track, typically leading to “white collar” apprenticeships), secondary school B/C (lower non-college track, typically leading to “blue collar” apprenticeships), and special needs education, respectively. Migrant background was coded 0 for respondents with at least one parent born in Switzerland, and 1 for those with both parents born abroad.
2.2.3. Antecedent variables
In order to evaluate antecedent precursors associated with COVID-19 non-compliance, we used information from the two previous waves of the z-proso study (ages 17 and 20) that preceded the pandemic. All scales were constructed by taking the mean of the respective items, unless otherwise noted. Reliability statistics and example items for each antecedent and concurrent scale are reported in Supplementary Appendix B. Cronbach's α > 0.70 is considered acceptable.
Weak social bonds and active lifestyle. Weak bonds may reflect an individual's reduced embeddedness in social networks and less exposure to social pressures to comply (Sampson and Laub, 1990). In addition, an active social lifestyle may increase risk of non-compliance with social distancing measures. We used eight variables to measure elements of weak social bonds and social lifestyle: low parental involvement, low parental monitoring, low teacher-student bonds, low school commitment, low social support, perceived social exclusion, low generalized trust, and active social lifestyle (e.g., meeting with friends, practicing sports). Parent- and school-related variables were measured at age 17; exclusion, trust, and social lifestyle were measured at age 20. Low parental involvement is a proxy for family bonds consisting of six items measuring how often an adolescent's parents talked, comforted, and showed interest in them (α = 0.77). Low parental monitoring consisted of seven items capturing aspects of parental supervision and control (α = 0.66). The low teacher-student bond scale consisted of three items measuring the quality of the adolescent's relationship with their current teacher (α = 0.78). Low school commitment was a four-item scale that reflects a more general measure of an adolescent's bond to school (α = 0.64). A four-item low social support scale was included to capture the respondent's access to trustworthy social ties for problem-solving and support (α = 0.80). Social exclusion was a proxy for an individual's bonds to society (α = 0.88). The scale consisted of six items measuring feelings of segregation, alienation, isolation, and worthlessness. The low generalized trust scale consisted of three items capturing feelings that people can be trusted and try to help people (α = 0.84). An active social lifestyle may increase the risk of non-compliance, as individuals are motivated to maintain this lifestyle, for example, by leaving the home to engage in social gatherings. An individual's active social lifestyle was measured using 17 items that capture structured and unstructured routine activities outside the home, including meeting friends and practicing sports (α = 0.68).
Attitudes towards the law and police. We used two measures that capture attitudes towards the law and police (measured at age 20) which can be indicative of an individual's broader willingness to accept formal authorities and directives: low police legitimacy and legal cynicism. Low police legitimacy was measured using three items that reflect dimensions of police performance, fairness, and confidence in police effectiveness (α = 0.83). Legal cynicism reflects the belief that the law is not binding. The legal cynicism scale consisted of six items that capture justifications for acting outside the law (α = 0.77; Sampson and Bartusch, 1998).
Deviant peers and antisocial behavior. Two of the most important individual antecedents of rule-breaking are prior rule-breaking and affiliation with peers who exhibit social deviance (Nagin and Paternoster, 1991; Pratt et al., 2010). We therefore included measures of prior antisocial behavior and deviant peers measured at age 20. In order to capture the influence of deviant peers, respondents were asked about the deviant behavior of their two ‘best friends’ (e.g., kick/hit and injure somebody, steal something from a shop, take illegal drugs). For each respondent, the mean score of the six items was constructed based on one or both best friends. Respondents who reported that they did not have a best friend were treated as missing (n = 26, 3.5%). The range was 0–1, so the variable was z-transformed to ease interpretation. A one-unit increase therefore reflects a one-standard deviation increase in deviant peer behavior. Prior antisocial behavior was measured using a variety score of the respondent's involvement in 16 different antisocial behaviors in the year prior to the survey (i.e., between ages 19 and 20). Antisocial behaviors include bullying, truancy, substance use, theft, and violence.
Dispositional factors. We included three dispositional factors measured at age 20 as important predictors of health and risk behaviors: low self-control, low self-efficacy, and low feelings of guilt or shame (Cho and Lee, 2011; de Ridder et al., 2012; Moffitt et al., 2011). Low self-control was measured using 10 items including five sub-dimensions of self-control (i.e., impulsivity, self-centeredness, risk-seeking, preference for physical activities, and short temper, Cronbach's α = 0.73; Grasmick et al., 1993). The low self-efficacy scale consisted of five items that reflect an individual's feelings of control and confidence in achieving goals (α = 0.74). Low feelings of shame or guilt were captured using three items that ask respondents to what extent they feel bad or guilty when they have done wrong (α = 0.69).
2.2.4. Concurrent variables
Two items were used to measure risk of infection. Respondents were asked whether they or a family member had a pre-existing condition that increases their risk or seriousness of infection. Two measures captured the respondent's broader perceptions about low social compliance (i.e., social norms) and low moral norms regarding whether certain non-compliant behaviors are wrong (α = 0.75). The respondent's attitudes about broader social non-compliance (i.e., social norms) were measured using a single item that capture perceptions about others' behavior during the outbreak. Low moral norms were measured using four items that indicate whether the respondent believes certain non-compliant behaviors are wrong. The four-item COVID-19 moral disengagement scale reflected attitudes that underestimate or dismiss the risk of infection (α = 0.63). The low trust in government scale consisted of three items capturing the respondent's views on Swiss authorities in relation to the outbreak (α = 0.75). Finally, low information-seeking was measured by a single item that asks respondents how often he/she sought out news or information about COVID-19 in the two weeks prior to the survey.
2.2.5. Analytical strategy
Compared to the previous wave (age 20), an attrition analysis showed significantly higher response rates in the age 22 COVID-19 survey by women compared to men, and in (local) German speakers compared to participants whose parents were from other linguistic backgrounds (which serves as a proxy indicator for migrant background). Therefore, sampling weights were used in all analyses to allow the generalization of results to the original target sample.
Analyses were conducted in two stages. All analyses used binomial generalized linear model [GLM] regressions with a logit-link function. Binomial regression techniques tend to perform better when analyzing sum scores (i.e., bounded count data) compared to traditional or Poisson regression approaches (Britt et al., 2018). First, we examined differences in compliance behaviors by sociodemographic characteristics. Specifically, we estimated the likelihood of each non-compliance behavior by sex, and then examined the likelihood of overall, hygiene, and social distancing non-compliance by education level, sex, SES quartiles, and migrant background. Estimates were computed using sampling weights, and adjusting for other sociodemographic characteristics. The odds ratios [ORs] therefore reflect the adjusted odds of an additional non-compliance behavior in a given group compared to the reference group. Unadjusted and adjusted estimates are available in Supplementary Appendix C.
Second, we estimated bivariate associations between both antecedent and concurrent factors with non-compliance, adjusting for the sociodemographic characteristics described above. The resulting ORs reflect the odds of an additional non-compliance behavior given a one-unit increase in the independent variable. All analyses were conducted accounting for sample weights.
Missing data was low, with missingness for most variables ranging from 0% (e.g., compliance items) to 3% (e.g., parental monitoring). Four variables with the highest missingness were teacher-child bond (9%), school commitment (9%), social exclusion (9%), and peers exhibiting social deviance (11%). In order to assess whether results were influenced by missing data, we conducted multiple imputation using chained equations, which can handle different types of complex (bounded) data (Azur et al., 2011). Using the variables included in the analyses as predictors, we imputed 10 complete datasets and re-estimated all analyses with full information (n = 737). The substantive results remained the same, so we present the results for the listwise analyses (imputed results are available in the Supplementary Appendix D).
3. Results
3.1. Prevalence of non-compliance by sociodemographic characteristics
Table 1 shows descriptive statistics for the weighted sample. Overall, non-compliance was relatively low: On average, respondents reported failing to comply with 2–3 (out of 13) COVID-19-related measures (M = 2.47, SE = 0.07). Non-compliance with hygiene-related COVID-19 measures was reported more often (M = 1.77, SE = 0.05) than non-compliance with social distancing measures (M = 0.71, SE = 0.04).
Table 2 provides additional detailed information about average levels of non-compliance with each COVID-19 measure, stratified by sex. For the full sample, non-compliance varied across specific hygiene and social distancing measures. Non-compliance was more prevalent for certain hygiene measures, such as cleaning or disinfecting one's mobile phone (53%), washing one's hands after coughing or sneezing (53%), avoiding touching one's face (35%), and using hand disinfectant (27%). Conversely, non-compliance was low for coughing or sneezing into one's elbow (3%), and washing one's hands regularly (5%). Non-compliance for social distancing measures ranged from 3% (staying at home with symptoms) to 18% (adhering to 1.5–2 m social distancing guidelines). Table 2 also shows that non-compliance is generally greater among males compared to females, but this pattern varies by behavior. Specifically, there were no significant differences (p > 0.05) found for regular handwashing, adhering to social distancing guidelines, avoiding contact with people at risk, only using public transport when necessary, and staying at home with symptoms (see Table 2).
Table 2.
Binomial generalized linear model [GLM] regression results for odds of reporting non-compliance with each public health recommendation.
| Behavior type | Public health recommendation | Non-compliance |
OR (ref: female) | t | p | ||
|---|---|---|---|---|---|---|---|
| Full sample | Female | Male | |||||
| Hygiene | Avoid touching face | 35% | 31% | 39% | 1.42 | 2.19 | 0.028 |
| Clean/disinfect mobile phone | 53% | 47% | 59% | 1.59 | 2.97 | 0.003 | |
| Cough or sneeze into elbow/cloth | 3% | 1% | 5% | 4.07 | 2.66 | 0.008 | |
| Use hand disinfectant | 27% | 23% | 30% | 1.45 | 2.20 | 0.028 | |
| Wash hands after cough/sneeze | 53% | 47% | 58% | 1.59 | 2.97 | 0.003 | |
| Wash hands regularly | 5% | 4% | 7% | 1.82 | 1.78 | 0.075 | |
| Social distancing | Adhere to social distancing | 18% | 18% | 18% | 1.00 | 0.02 | 0.987 |
| Avoid contact with people at risk | 5% | 5% | 5% | 1.05 | 0.14 | 0.891 | |
| Avoid groups | 10% | 5% | 14% | 2.90 | 3.77 | <0.001 | |
| Don't shake hands | 12% | 7% | 16% | 2.63 | 3.85 | <0.001 | |
| Only necessary public transport | 10% | 8% | 12% | 1.53 | 1.65 | 0.098 | |
| Stay at home | 13% | 7% | 19% | 3.00 | 4.62 | <0.001 | |
| Stay at home with symptoms | 3% | 2% | 4% | 1.97 | 1.35 | 0.177 | |
Note. All estimates are computed accounting for sample weights. OR = odds ratios.
Adjusted odds ratios for hygiene, social distancing, and overall COVID-19 non-compliance levels by sociodemographic characteristics are presented in Table 3 . Males were 43% more likely to report an additional non-compliance behavior compared to females (overall non-compliance OR = 1.43, p < 0.001). Non-compliance with hygiene measures was lower in respondents from low and medium (i.e., ORsecondary A(medium) = 0.76; ORsecondary B/C(low) = 0.63) compared to higher educational backgrounds (i.e., Gymnasium). By contrast, respondents in the medium educational tracks (secondary A) were 42% (p = 0.060) and respondents in the low educational track (secondary B/C) were 93% more likely (p < 0.001) to report additional social distancing non-compliance behaviors compared to respondents with higher education (college-track). Respondents with low SES were less likely to report hygiene non-compliance (OR Quartile1(low) = 0.61, p < 0.001), but there were no differences for social distancing non-compliance. Respondents with a migration background were 25% less likely to report additional hygiene non-compliance compared to respondents with at least one parent born in Switzerland, but there were no differences in social distancing non-compliance.
Table 3.
Adjusted binomial generalized linear model [GLM] regression results for odds of an additional non-compliance behavior by sociodemographic characteristics.
| Hygiene non-compliance |
Social distancing non-compliance |
Overall non-compliance |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CIL | 95% CIU | P | OR | 95% CIL | 95% CIU | p | OR | 95% CIL | 95% CIU | p | ||||
| Education level (age 15) | |||||||||||||||
| Gymnasium (high) | ref. | ref. | ref. | ||||||||||||
| Secondary school A | 0.76 | 0.64 | – | 0.91 | <0.001 | 1.42 | 0.98 | – | 2.05 | 0.06 | 0.92 | 0.78 | – | 1.09 | 0.33 |
| Secondary school B/C | 0.63 | 0.49 | – | 0.82 | <0.001 | 1.93 | 1.26 | – | 2.98 | <0.001 | 0.92 | 0.74 | – | 1.16 | 0.49 |
| Special needs education | 0.86 | 0.35 | – | 2.14 | 0.75 | 1.45 | 0.34 | – | 6.21 | 0.62 | 1.00 | 0.39 | – | 2.57 | 1.00 |
| Sex | |||||||||||||||
| Female | ref. | ref. | ref. | ||||||||||||
| Male | 1.36 | 1.16 | – | 1.6 | <0.001 | 1.73 | 1.33 | – | 2.24 | <0.001 | 1.43 | 1.25 | – | 1.64 | <0.001 |
| SES quartiles | |||||||||||||||
| Q4 (high) | ref. | ref. | ref. | ||||||||||||
| Q3 | 0.71 | 0.57 | – | 0.87 | <0.001 | 0.86 | 0.58 | – | 1.29 | 0.47 | 0.78 | 0.65 | – | 0.93 | 0.01 |
| Q2 | 0.69 | 0.54 | – | 0.88 | <0.001 | 1.08 | 0.7 | – | 1.65 | 0.73 | 0.82 | 0.66 | – | 1.03 | 0.09 |
| Q1 (low) | 0.61 | 0.46 | – | 0.81 | <0.001 | 0.87 | 0.54 | – | 1.4 | 0.57 | 0.71 | 0.55 | – | 0.92 | 0.01 |
| Migrant background | |||||||||||||||
| At least one parent born in Switzerland | ref. | ref. | ref. | ||||||||||||
| Both parents born abroad | 0.75 | 0.62 | – | 0.91 | <0.001 | 0.94 | 0.68 | – | 1.3 | 0.71 | 0.83 | 0.69 | – | 0.98 | 0.03 |
Note. All estimates are computed accounting for sample weights. Estimates are adjusted for sociodemographic characteristics. OR = odds ratio. CIL = confidence interval (lower); CIU = confidence interval (upper).
3.2. Effects of antecedent and concurrent factors on non-compliance
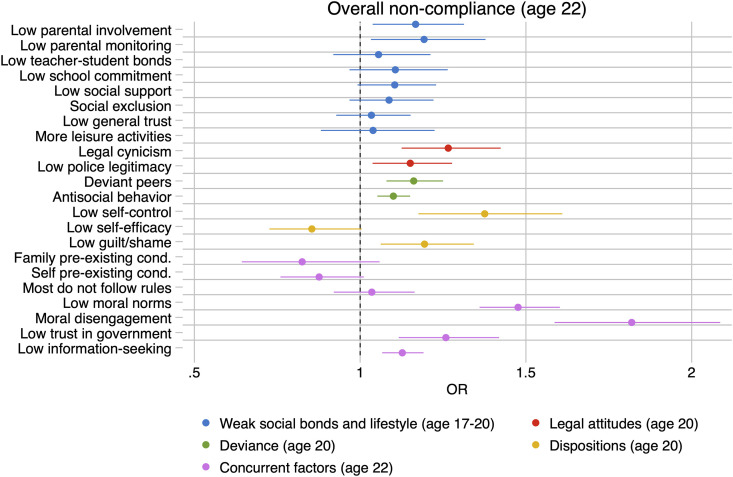
Adjusted ORs and 95% confidence intervals for antecedent and concurrent factors on overall non-compliance are visualized in Fig. 1 . All point estimates, 95% confidence intervals, and p-values for unadjusted and adjusted effects are available in Supplementary Appendix C. Overall, several antecedents are consistently associated with both types of non-compliance, even when adjusting for sociodemographic factors: legal cynicism (overall OR = 1.27, p < 0.001), deviant peers (overall OR = 1.16, p < 0.001), antisocial behavior (overall OR = 1.10, p < 0.001), and low guilt/shame (overall OR = 1.19, p = 0.003). For example, with each additional antisocial behavior reported (e.g., steal something from a shop, take illegal drugs) the odds of reporting an additional non-compliance behavior increased by 10%. Concurrent factors associated with non-compliance included low feelings of moral obligation (overall OR = 1.48, p < 0.001), COVID-19 moral disengagement (overall OR = 1.82, p < 0.001), and low information-seeking behavior (overall OR = 1.13, p < 0.001).
Fig. 1.
Adjusted odds ratios and 95% confidence intervals for antecedent and concurrent risk factors for overall non-compliance with COVID-19 public health measures at age 22. Note. All analyses are conducted on weighted sample; adjusted effects are estimated controlling for sex, SES, education level, and migrant background.
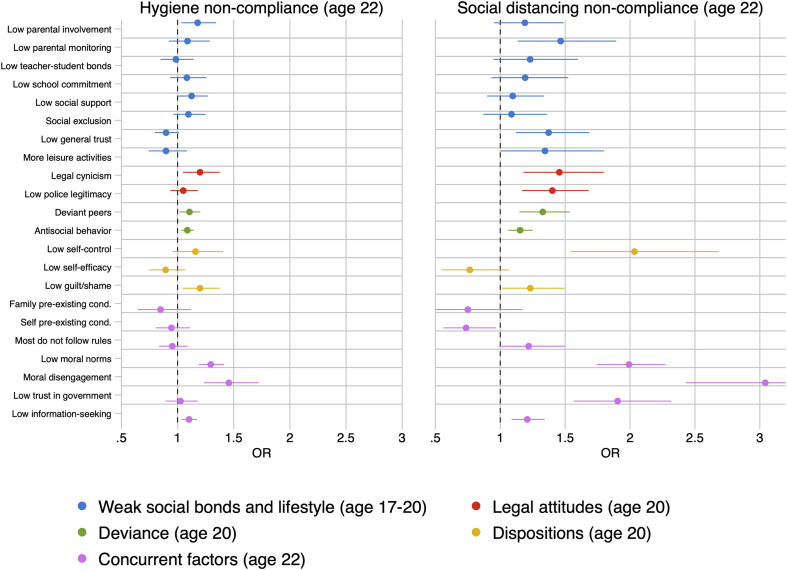
Adjusted ORs and 95% confidence intervals for hygiene and social distancing non-compliance respectively are presented in Fig. 2 . The results suggested that certain antecedent and concurrent factors are associated with hygiene and social distancing non-compliance to different degrees. We did not identify factors that were robustly associated with hygiene non-compliance only. By contrast, other antecedent and concurrent factors appeared to be uniquely associated with social distancing non-compliance: low parental monitoring (OR = 1.47, p = 0.003), low police legitimacy (OR = 1.40, p < 0.001), low self-control (OR = 2.03, p < 0.001), and low trust in government (OR = 1.90, p < 0.001). Association between low generalized trust and non-compliance varied by type of behavior. Low generalized trust was associated with a lower likelihood of hygiene non-compliance (OR = 0.90, p = 0.074), but an increased likelihood of social distancing non-compliance (OR = 1.37, p = 0.002).
Fig. 2.
Adjusted odds ratios and 95% confidence intervals for antecedent and concurrent risk factors for hygiene and social distancing non-compliance at age 22. Note. All analyses are conducted on weighted sample; adjusted effects are estimated controlling for sex, SES, education level, and migrant background.
4. Discussion
Understanding characteristics of young people who do not comply with COVID-19-related public health measures is essential for developing effective public health campaigns in the current and future pandemics. We leveraged data from a longitudinal cohort study with assessments before and during the COVID-19 pandemic to examine antecedent and concurrent factors associated with non-compliance. Results showed that rates of compliance with COVID-19-related measures in a representative sample of young adults were relatively high, and slightly better for social distancing than hygiene measures (see Table 2). Non-compliance was higher among males, those with a higher education level, higher SES, and non-migrant background (see Table 3). These associations were primarily driven by associations with non-compliance in hygiene-related measures.
Analyses of antecedent and concurrent risk factors suggested that non-compliance was associated with a cluster of characteristics sometimes termed “antisocial potential” (see Fig. 1): low acceptance of moral rules, legal cynicism, low shame or guilt, low self-control, high engagement in delinquent behaviors, and association with peers who exhibit social deviance (Farrington, 2019). Public health measures have in the past appealed to social pressure and moral obligations to motivate compliance (Webster et al., 2020). Our results support these approaches. The factors related to antisocial potential are considered by some to be less malleable in the short term making them less suitable for intervention (see Na and Paternoster, 2012). Although it is unlikely that public health campaigns can effectively change characteristics related to an individual's antisocial potential in emergency situations such as a pandemic, it is possible to manage the effects of certain antisocial risk factors in the short term. For example, evidence suggests that the effect of low self-control can be attenuated by intervention strategies that aim to manage deficits in self-control through self-monitoring, environmental restructuring, or nudging (Hagger et al., 2019).
In addition, our results suggest that hygiene and social distancing behaviors are in part driven by different mechanisms. For example, negative attitudes towards authorities (i.e., low police legitimacy, low trust in government) were associated with social distancing non-compliance but not with hygiene non-compliance (see Fig. 2). This has important implications for public health policies and campaigns that aim to motivate compliance with COVID-19-related measures. Compliance with social distancing measures involves greater or more restrictive behavioral change, with direct consequences for psychological, social, and economic well-being (Barari et al., 2020; Baum et al., 2009). Adopting these behavioral changes may be perceived as too burdensome without adequate trust and belief that authorities are fair and effective in implementing restrictive rules. In addition, trust may indirectly motivate compliance by increasing an individual's perception of risk (Shao and Hao, 2020; Van der Weerd et al., 2011).
Our results suggest that there are some areas of non-compliance that require additional attention from public health campaigns. Non-compliance with certain protective measures, such as avoiding groups, coughing or sneezing into one's elbow, and washing one's hands regularly, was generally low (see Table 2). This implies that the message was effectively disseminated and young people were generally receptive to these measures. However, non-compliance with certain hygiene and social distancing measures were relatively higher, including cleaning and disinfecting mobile phones or standing 1.5–2 m apart. Cleaning mobile phones was not an “official” recommendation by Swiss authorities, which may partly explain lower levels of compliance regarding these hygiene measures. Nevertheless cleaning environmental surfaces, including mobile phones, has been recommended by international public health authorities and media outlets as a protective measure against the spread of the virus (CDC, 2020; Ciric, 2020). Public health campaigns should address these aspects of non-compliance, for example by improving the awareness and understanding of the virus on smartphones and other methods of transmission (Kampf et al., 2020).
Finally, analyses of non-compliance by sociodemographic characteristics indicated that males are less likely to comply with both hygiene and social distancing measures (see Table 3). This is an important finding given that the available evidence suggests that COVID-19 mortality rates are higher for men compared to women (Global Health 50/50, 2020). Furthermore, our results showed that non-migrant background and high-SES young people were less likely to comply with hygiene measures, but not social distancing measures. This may in part reflect what is known as the “immigrant health paradox,” whereby first- and second-generation migrants tend to report fewer risky health behaviors and better health outcomes than natives (Markides and Rote, 2015). Hygiene practices may also depend on situational, household, or occupational characteristics that may influence the risk of infection. For example, migrant background or low SES/education individuals may be more likely to work in service sector positions that are considered “essential”, increasing exposure to environmental risks. Low SES or education groups also face higher barriers to compliance with social distancing rules, such as staying home or avoiding public transport, due to economic hardship and the fear of losing income (Webster et al., 2020). Social distancing non-compliance among these groups may be even higher in contexts that lack a strong social safety net or compensation for lost wages (Bodas and Peleg, 2020; Coatzee and Kagee, 2020; Templeton et al., 2020).
4.1. Limitations and conclusions
The current study has several strengths, most notably its broadly representative sample and measures of social and psychological antecedent risk factors. Limitations include that the sample is not necessarily representative of other areas of Switzerland or other countries. Furthermore, while the COVID-19-related measures in Switzerland are generally in line with global recommendations, there are important differences in policies and information which may influence non-compliance. For example, some countries and cities require face masks to be worn when going outside (Cheng et al., 2020), whereas this was not initially recommended in Switzerland. In addition, while the dissemination of information regarding the virus by Swiss authorities was relatively consistent, messaging and implementation in other countries such as the United States has been less centralized and uniform (Gordon et al., 2020). Non-compliance with certain measures may therefore vary by the specific public health campaigns and official recommendations in each region.
Overall, our findings suggest that young people were largely complying with COVID-19 public health measures during the initial wave of the pandemic in Zurich. This high level of overall compliance may speak to the centralized messaging regarding information and restrictions by Swiss authorities, however more research is needed to understand to what extent certain policy responses and public health campaigns influence compliance across countries. Non-compliance was strongly associated with weaker feelings of moral obligation and low trust in authorities, but also with characteristics related to antisocial potential. Public health campaigns can implement strategies that foster moral obligation and trust in authorities, or leverage trustworthy individuals in the community to disseminate information. Our results suggest that it is also important to implement strategies that address the factors related to antisocial potential such as self-control. This can be accomplished for example through self-monitoring or environmental restructuring (or “nudging”) to promote protective health habits and behaviors (Hagger, 2019; Harkin et al., 2016; Hollands et al., 2017).
Data sharing
Anonymized individual participant data and data dictionaries that underlie the results reported in this article are available to other researchers upon request. Our statistical code is available on request from AN. Requests including a brief proposal should be sent to DR.
As a research infrastructure supported by the SNSF the z-proso study is committed to an open data access policy. Anonymized data, protocols, and other metadata from earlier data collections of the study are generally available to the scientific community. Please contact DR to this purpose.
Contributors
ME, LS, DR, UH, and AM co-developed and co-led the study, AS, ME, LS, UH, DR, AM, and LB contributed to the design of the questionnaire, DR organized the data collection, AN conducted the analyses and wrote up the results, AN and LS drafted and wrote the manuscript, AS, LB, ME, LS, DR, UH, AM, and AN contributed to the interpretation of the data, and critically revised the manuscript for important intellectual content.
Declaration of competing interest
We declare no competing interests.
Acknowledgements
The research reported in this manuscript is currently financially supported by the Swiss National Science Foundation as a research infrastructure (SNF; Grants 10FI14_170409; 10FI14_170402/2; recipient: Prof. Michael Shanahan) and by the Jacobs Foundation (JF). The Zurich Project on Social Development from Childhood to Adulthood is a long-term study set up by ME and DR. Earlier phases of the study (2003–2016) were funded by the SNF, the JF, the Swiss Federal Office of Public Health, the Department of Education of the Canton of Zurich, the Swiss State Secretariat of Migration and its predecessors, the Julius Bär Foundation, and the Visana Plus Foundation.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2020.113370.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Andrews J.L., Foulkes L., Blakemore S.J. Peer influence in adolescence: public-health implications for COVID-19. Trends Cognit. Sci. 2020;24:585–587. doi: 10.1016/j.tics.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azur M.J., Stuart E.A., Frangakis C., Leaf P.J. Multiple imputations by chained equations: what is it and how does it work? Int J Meth Psych. 2011;20:40–49. doi: 10.1002/mpr.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barari S., Caria S., Davola A., Falco P., Fetzer T., Fiorin S., et al. MedRxiv; 2020. Evaluating COVID-19 Public Health Messaging in Italy: Self-Reported Compliance and Growing Mental Health Concerns.https://www.medrxiv.org/content/10.1101/2020.03.27.20042820v2 [Google Scholar]
- Baum N.M., Jacobson P.D., Goold S.D. “Listen to the people”: public deliberation about social distancing measures in a pandemic. Am. J. Bioeth. 2009;9:4–14. doi: 10.1080/15265160903197531. [DOI] [PubMed] [Google Scholar]
- Bish A., Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br. J. Health Psychol. 2010;15:797–824. doi: 10.1348/135910710X485826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodas M., Peleg K. Self-isolation compliance in the COVID-19 era influenced by compensation: findings from a recent survey in Israel. Health Aff. 2020;39:1–4. doi: 10.1377/hlthaff.2020.00382. [DOI] [PubMed] [Google Scholar]
- Britt C.L., Rocque M., Zimmerman G.M. The analysis of bounded count data in criminology. J. Quant. Criminol. 2018;34:591–607. [Google Scholar]
- Brouard S., Vasilopoulos P., Becher M. Sociodemographic and psychological correlates of compliance with COVID-19 public health measures in France. Can. J. Polit. Sci. 2020;53:253–258. [Google Scholar]
- Bults M., Beaujean J.M.A., Richardus J.H., Voeten H.A. Perceptions and behavioral responses of the general public during the 2009 Influenza A (H1N1) pandemic: a systematic review. Disaster Med Public. 2015;9:207–219. doi: 10.1017/dmp.2014.160. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Cleaning and Disinfecting Your Home: Everyday Steps and Extra Steps when Someone Is Sick.https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/disinfecting-your-home.html [Google Scholar]
- Centers for Disease Control COVID-19 Response Team Severe outcomes among patients with coronavirus disease 2019 (COVID-19) – United States, February 12-March 16, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69 doi: 10.15585/mmwr.mm6912e2. https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e2.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng K.K., Lam T.H., Leung C.C. Wearing face masks in the community during COVID-19 pandemic: altruism and solidarity. Lancet. 2020 doi: 10.1016/S0140-6736(20)30918-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho H., Lee J.S. The influence of self-efficacy, subjective norms, and risk perception on behavioral intentions related to the H1N1 flu pandemic: a comparison between Korea and the US. Asian J. Soc. Psychol. 2015;18:311–324. [Google Scholar]
- Ciric L. 22 March 2020. Keep it Coronavirus Free: How to Clean Your Mobile Phone. The Guardian [newspaper on the Internet]https://www.theguardian.com/lifeandstyle/2020/mar/22/coronavirus-free-how-to-clean-your-mobile-phone [cited 24 April 2020]. Available from: [Google Scholar]
- Clark C., Davila A., Regis M., Kraus S. Predictors of COVID-19 voluntary compliance behaviors: an international investigation. Global Transitions. 2020;2:76–82. doi: 10.1016/j.glt.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coetzee B.J., Kagee A. Structural barriers to adhering to health behaviors in the context of the COVID-19 crisis: considerations for low- and middle-income countries. Global Publ. Health. 2020;15:1093–1102. doi: 10.1080/17441692.2020.1779331. [DOI] [PubMed] [Google Scholar]
- Cohen A.K., Hoyt L.T., Dull B. A descriptive study of COVID-19-related experiences and perspectives of a national sample of college students in spring 2020. J. Adolesc. Health. 2020;67:369–375. doi: 10.1016/j.jadohealth.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisner M., Malti T., Ribeaud D. In: The SAGE Handbook of Criminological Research Methods. Gadd D., Karstedt D., Messner S., editors. Sage; London: 2011. Large-scale criminological field experiments: the Zurich project on the social development of children; pp. 410–424. [Google Scholar]
- Eisner M., Murray A.L., Eisner M., Ribeaud D. A practical guide to the analysis of non-response and attrition in longitudinal research using a real data example. Int. J. Behav. Dev. 2019;43:24–34. [Google Scholar]
- Farrington D.P. The integrated cognitive antisocial potential (ICAP) theory: past, present, and future. J Dev Life Course Criminol. 2019;6:172–187. doi: 10.1007/s40865-019-00112-9. [DOI] [Google Scholar]
- Federal Office of Public Health . The Federal Council; 2020. New Coronavirus: Protect Yourself and Others.https://www.bag.admin.ch/bag/en/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/so-schuetzen-wir-uns.html#-1762329805 [Google Scholar]
- Federal Office of Public Health. Current situation . 2020. Swiss Confederation.https://foph-coronavirus.ch/ [Google Scholar]
- Ganzeboom H., de Graaf P., Treiman D. A standard international socio-economic Index of occupational status. Soc. Sci. Res. 1992;21:1–56. [Google Scholar]
- Global Health 50/50 . 2020. COVID-19 Sex-Disaggregated Data Tracker: Sex, Gender, and COVID-19.http://globalhealth5050.org/covid19/ [Google Scholar]
- Gordon S.H., Huberfeld N., Jones D.K. JAMA Health Forum; 2020. What Federalism Means for the US Reponse to Coronavirus Disease 2019.https://jamanetwork.com/channels/health-forum/fullarticle/2766033 [DOI] [PubMed] [Google Scholar]
- Grasmick H.G., Tittle C.R., Bursik R.J., Jr., Arneklev B.J. Testing the core empirical implications of Gottfredson and Hirschi's general theory of crime. J. Res. Crime Delinquen. 1993;30:5–29. [Google Scholar]
- Hagger M.S. Habit and physical activity: theoretical advances, practical implications, and agenda for future research. Psychol. Sport Exerc. 2019;42:118–129. [Google Scholar]
- Hagger M.S., Gucciardi D.F., Turrell A.S., Hamilton K. Self-control and health-related behavior: the role of implicit self-control, trait self-control, and lay beliefs in self-control. Br. J. Health Psychol. 2019;24:764–786. doi: 10.1111/bjhp.12378. [DOI] [PubMed] [Google Scholar]
- Harkin B., Webb T.L., Chang B.P.I., Prestwich A., Conner M., Kellar I., et al. Does monitoring goal progress promote goal attainment? A meta-analysis of the experimental evidence. Psychol. Bull. 2016;142:198–229. doi: 10.1037/bul0000025. [DOI] [PubMed] [Google Scholar]
- Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addiction. 2020 doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollands G.J., Bignardi G., Johnston M., Kelly M.P., Ogilvie D., Petticrew M., et al. The TIPPME intervention typology for changing envrionments to change behavior. Nature Human Behavior. 2017;1 [Google Scholar]
- Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuiper M.E., de Bruijn A.L., Folmer C.R., Olthuis E., Brownlee M., Kooistra E.B., Fine A., van Rooij B. Amsterdam Law School Research Paper; 2020. The Intelligent Lockdown: Compliance with COVID-19 Mitigation Measures in the Netherlands.https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3598215 No. 2020-20. [Google Scholar]
- Lammers J., Crusius J., Gast A. Correcting misconceptions of exponential coronavirus growth increases support for social distancing. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117:16264–16266. doi: 10.1073/pnas.2006048117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides K.S., Rote S. In: Emerging Trends in the Social and Behavioral Sciences. Scott R., Kosslyn S., editors. John Wiley & Sons; 2015. Immigrant health paradox. [Google Scholar]
- Moffitt T.E., Arseneault L., Belsky D., Dickson N., Hancox R.J., Harrington H., et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proc. Natl. Acad. Sci. Unit. States Am. 2011;108:2693–2698. doi: 10.1073/pnas.1010076108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Na C., Paternoster R. Can self-control change substantially over time? Rethinking the relationship between self and social control. Criminology. 2012;50:427–462. [Google Scholar]
- Nagin D., Paternoster R. On the relationship of past to future participation in delinquency. Criminology. 1991;29:163–190. [Google Scholar]
- Nebehay S. Reuters; 2020. WHO Message to Youth on Coronavirus: ‘You Are Not Invincible’.https://www.reuters.com/article/us-health-coronavirus-who/who-message-to-youth-on-coronavirus-you-are-not-invincible-idUSKBN21733O [Google Scholar]
- Oosterhoff B., Palmer C.A., Wilson J., Shook N. Adolescents' motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J. Adolesc. Health. 2020;67:179–185. doi: 10.1016/j.jadohealth.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan A., Liu L., Wang C., Guo H., Hai X., Wang Q., et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. J. Am. Med. Assoc. 2020;2020 doi: 10.1001/jama.2020.6130. Published online April 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CL, Russell BS, Fendrich M, Finkelstein-Fox L, Hutchison M, Becker J. Americans' COVID-19 stress, coping, and adherence to CDC guidelines. J. Gen. Intern. Med. 35:2296-2303. [DOI] [PMC free article] [PubMed]
- Prati G., Pietrantoni L., Zani B. Compliance with recommendations for pandemic influenza H1N1 2009: the role of trust and personal beliefs. Health Educ. Res. 2011;26:761–769. doi: 10.1093/her/cyr035. [DOI] [PubMed] [Google Scholar]
- Prati G., Pietrantoni L., Zani B. A social-cognitive model of pandemic influenza H1N1 risk perception and recommended behaviors in Italy. Risk Anal. 2011;31:645–656. doi: 10.1111/j.1539-6924.2010.01529.x. [DOI] [PubMed] [Google Scholar]
- Pratt T.C., Cullen F.T., Sellers C.S., Winfree L.T., Jr., Madensen T.D., Daigle L.E., et al. The empirical status of social learning theory: a meta-analysis. Justice Q. JQ. 2010;27:765–802. [Google Scholar]
- Roy-Chowdhury V., Perera D., Tagliaferri G., Mottershaw A., Egan M. Behavioral Insights Team; 2020. Young Men Are Hardest to Engage on Coronavirus Guidance: Analysis of 11 Trials with 20,000 UK Adults.https://www.bi.team/blogs/young-men-are-hardest-to-engage-on-coronavirus-guidance/ [Google Scholar]
- Rubin G.J., Amlôt R., Page L., Wessely S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. BMJ. 2009;339:b2651. doi: 10.1136/bmj.b2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salathé M., Althaus C.L., Neher R., Stringhini S., Hodcroft E., Fallay J., et al. COVID-19 epidemic in Switzerland: on the importance of testing, contract tracing and isolation. Swiss Med. Wkly. 2020;150:w202205. doi: 10.4414/smw.2020.20225. [DOI] [PubMed] [Google Scholar]
- Sampson R.J., Bartusch D.J. Legal cynicism and (subcultural?) tolerance of deviance: the neighborhood context of racial differences. Law Soc. Rev. 1998;32:777–804. [Google Scholar]
- Sampson R.J., Laub L.H. Crime and deviance over the life course: the salience of adult social bonds. Am. Socio. Rev. 1990;55:609–627. [Google Scholar]
- Setbon M., Le Pape M.-C., Létroublon C., Caille-Brillet A.-L., Raude J. The public's preventive strategies in response to the pandemic influenza A/H1N1 in France: distribution and determinants. Prev. Med. 2011;52:178–181. doi: 10.1016/j.ypmed.2010.11.010. [DOI] [PubMed] [Google Scholar]
- Shao W., Hao F. Confidence in political leaders can slant risk perceptions of COVID-19 in a highly polarized environment. Soc. Sci. Med. 2020;261:113235. doi: 10.1016/j.socscimed.2020.113235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Templeton A., Guven S.T., Hoerst C., Vestergren S., Davidson L., Ballentyne S., Madsen H., Choudhury S. Inequalities and identity processes in crises: recommendations for facilitating safe response to the COVID-19 pandemic. Br. J. Soc. Psychol. 2020;59:674–685. doi: 10.1111/bjso.12400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Coronavirus Disease (COVID-19) Advice for the Public.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public [Google Scholar]
- Van der Weerd W., Timmermans D.R.M., Beaujean D.J.M.A., Oudhoff J., van Steenbergen J.E. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in The Netherlands. BMC Publ. Health. 2011;11:575. doi: 10.1186/1471-2458-11-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster R.K., Brooks S.K., Smith L.E., Woodland L., Wessely S., Rubin J. How to improve adherence with quarantine: rapid review of the evidence. Publ. Health. 2020 doi: 10.1016/j.puhe.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrzus C., Hänel M., Wagner J., Neyer F. Social network changes and life events across the life span: a meta-analysis. Psychol. Bull. 2013;139:53–80. doi: 10.1037/a0028601. [DOI] [PubMed] [Google Scholar]
- Zajenowski M., Jonason P.K., Leniarska M., Kozakiewicz Z. Who complies with the restrictions to reduce the spread of COVID-19?: personality and perceptions of the COVID-19 situation. Pers. Indiv. Differ. 2020;166:110199. doi: 10.1016/j.paid.2020.110199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zettler I., Schild C., Lillehold L., Böhm R. PsyArXiv; 2020. Individual Differences in Accepting Personal Restrictions to Fight the COVID-19 Pandemic: Results from a Danish Sample.https://psyarxiv.com/pkm2a/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.