Abstract
Background
Sedentary behavior (SB) and physical activity (PA) are important determinants of health in older adults. This study aimed to describe the composition of accelerometer-measured SB and PA in older adults, to explore self-reported context-specific SB, and to assess sociodemographic and functional correlates of engaging in higher levels of SB in participants of a multicenter study including four European countries.
Method
One thousand three hundred and sixty community-dwelling older adults from the SITLESS study (61.8% women; 75.3 ± 6.3 years) completed a self-reported SB questionnaire and wore an ActiGraph accelerometer for 7 days. Accelerometer-determined compositional descriptive statistics were calculated. A fixed-effects regression analysis was conducted to assess the sociodemographic (country, age, sex, civil status, education, and medications) and functional (body mass index and gait speed) correlates.
Results
Older adults spent 78.8% of waking time in SB, 18.6% in light-intensity PA, and 2.6% in moderate-to-vigorous PA. Accelerometry showed that women engaged in more light-intensity PA and walking and men engaged in higher amounts of moderate-to-vigorous PA. Watching television and reading accounted for 47.2% of waking time. Older age, being a man, single, taking more medications, being obese and overweight, and having a slower gait speed were statistically significant correlates of more sedentary time.
Conclusions
The high amount of SB of our participants justifies the need to develop and evaluate interventions to reduce sitting time. A clinically relevant change in gait speed can decrease almost 0.45 percentage points of sedentary time. The distribution of context-specific sedentary activities by country and sex showed minor differences, albeit worth noting.
Keywords: Compositional analysis, Sedentary behavior, Physical activity, Sociodemographic correlates
Physical activity (PA) and sedentary behavior (SB) (any waking activity in a sitting, reclining, or lying posture where energy expenditure is <1.5 metabolic equivalents) (1) are important determinants of health and quality of life in older adults (2,3). Diseases associated with prolonged SB cost the UK public health system £0.8 billion in the 2016–2017 financial year (4). Prolonged SB throughout the day increases the risk of poor health, even in people who are moderately physically active (5,6). However, some evidence suggests the observed risks of SB may not be completely independent of total PA levels (7), as it is assumed that the reduction in PA on the one hand is accompanied by concomitant increases in SB on the other hand (8). Older adults spend most of their waking day sitting (9), placing them at increased risk for various detrimental health outcomes, among them all-cause mortality, metabolic syndrome, obesity, and cognitive health (10–12).
Most of the past research has relied on self-reported assessments of the time spent in sedentary activities. Both objective and self-reported measures have strengths and limitations. Self-reported tools can be subject to response bias (eg, recall bias) (13). For example, Harvey and colleagues (9) found that the self-reported SB of older adults averaged 5.3 h/d, well below values recorded using accelerometry, which averaged 9.4 h/d. Objective measures such as accelerometers are unable to capture how the sedentary time is spent.
Self-report instruments to assess PA have mainly focused on moderate-to-vigorous PA (MVPA) as these activities are more regimented and therefore easier to remember (14), and in line with international and national PA guidelines (15). However, evidence is accumulating that older adults spend much more of their time in lower-intensity PA. In a recent study, objectively measured MVPA accounted for just 2% of the day in a large sample of older adults from the Netherlands. In contrast, the time spent in light-intensity PA (LPA) was 33% and time spent sedentary was 65% of their day (16). To date, efforts to increase PA in the population have also mainly focused on increasing MVPA (17). As accumulating evidence is suggesting that a higher level of LPA is associated with health benefits (18–20), it would appear logical that inactive adults should initially be encouraged to reduce SB and engage in any intensity of PA.
For a more detailed understanding of the relationship between PA and SB, it is necessary to know how the time spent in both behaviors is distributed across the day, and whether sex-related differences are worth exploring. The pattern of waking activity is made up of periods of SB, LPA, and MVPA interspersed throughout the day (21). SB is tightly linked in a zero-sum time-use relationship with overall PA (22); standing up from a chair results in increased PA, albeit typically of a low intensity. The evidence linking SB to poor health therefore suggests that health-related benefits may be acquired displacing prolonged sitting time with LPA throughout the day. It is widely thought that a greater understanding of the role of each PA and SB component in this age group is necessary to inform appropriate strategies to modify both behaviors, and should be assessed in a holistic way (23). Compositional analysis provides a new method to deal directly with the compositional nature of movement behavior. The amount of time spent on a behavior is meaningful only in light of the time spent on other behaviors and not on its own (21). In comparison to more traditional methods, compositional analysis eliminates collinearity problems and deals with the codependence between time spent in different movement behaviors (21). Even if the information contained in the movement behavior composition is relative and thus scale invariant, it can be normalized to any sum (such as 100 for percentages) without loss of information.
Different types of SB occur in a variety of situations for different purposes, including leisure, household, occupation, and transportation (24). Most health-based studies in older adults have focused on total sedentary time (9,25,26). However, knowing in which context SB is accumulated (eg, watching television, reading a book, sitting in any transport mode) as well as sex-related differences might be of use in targeting the best-suited strategies to decrease overall SB time. Also, being able to identify how SB and PA (LPA and MVPA) are interrelated and distributed across countries, age categories and other demographic and health factors is needed to identify the characteristics of older adults that could be targeted by preventive intervention efforts and aging research and by cross-European policies and guidelines (27–29).
Accordingly, the goals of this study were to (a) describe the composition of accelerometer-measured SB and PA time in a cohort of community-dwelling older adults from four European countries from the SITLESS study; (b) explore the context in which self-reported SB occurs in both men and women and across countries; and (c) assess the correlates of SB according to country or residence, age, sex, civil status, education level, number of current medications, body mass index (BMI), and gait speed.
Method
The SITLESS study is a multicenter pragmatic three-armed parallel randomized controlled trial. Community-dwelling older adults aged 65 years or older, with a score on the Short Physical Performance Battery (SPPB) of four or above (30), who were insufficiently active and/or reported high levels of SB (31), were recruited in study centers in Denmark, Spain, United Kingdom, and Germany according to their existing primary prevention pathways. Spain and the United Kingdom had 85.5% and 58.6% recruitment through primary health care professionals, respectively. In Denmark, the largest recruitment pathway was through existing preventive home visits (83.2%). In Germany, participants were mostly reached through invitation letters (76.8%). The study protocol can be found elsewhere (32). The present article uses data from the preintervention baseline assessments.
A total of 1,360 community-dwelling older adults (61.8% women; 75.3 ± 6.3 years old) were analyzed at baseline. The study design was approved by the Ethics and Research Committee of each intervention site: The Regional Committees on Health Research Ethics for Southern Denmark (Denmark), the Ethics and Research Committee of Ramon Llull University (Spain), the Office for Research Ethics Committees in Northern Ireland (ORECNI; United Kingdom), and the Ethical Review Board of Ulm University (Germany). Participation was voluntary, and all participants signed informed consent before the start of the study.
Outcome Measures
Personal information regarding age, sex, civil status, educational background, medical conditions, and number of current medications was collected by means of a structured interview in the study centers. Weight and height were objectively measured by a trained researcher using a TANITA BC 420 and a SECA 213 portable stadiometer, respectively, to derive the participants’ BMI. Gait speed was obtained from a 4-m walk test. Participants were asked to walk at their normal pace, and speed was calculated as distance in meters divided by time in seconds. Participants self-reported the number of hours spent sitting on a weekday and on a weekend day in different contexts using the Sedentary Behavior Questionnaire (SBQ). Reliability and validity of the SBQ had been validated among overweight adults in a previous study (33); intraclass correlation coefficients were acceptable for all items and the total scale, and significant associations were found with the sitting time question of the International Physical Activity Questionnaire and BMI (33). Context-specific SBs included in the SBQ were as follows: watching television, playing computer or video games, sitting listening to music or radio, sitting and talking on the phone, doing paperwork or computer work, sitting reading a book or magazine, playing a musical instrument, doing artwork or crafts, and sitting and driving in a car, bus, or train.
Participants wore an ActiGraph wGT3X-BT triaxial accelerometer (ActiGraph, LLC, Pensacola, FL) on their dominant hip during waking hours for seven consecutive days, removing it only for water-based activities such as bathing or swimming and to sleep during the night. Participants recorded wear time in an activity diary. The devices were initialized to collect data at 30 Hz. To be included in the analysis, an accelerometer record needed to contain at least four valid days (including at least one weekend day), with a valid day defined as containing at least 600 minutes (10 h/d) of wear time as in previous studies (34). Nonwear time was defined using a two-window system: a 90-minute window for checking for consecutive zero counts and another 30-minute upstream and downstream window for checking for more than 2 minutes of nonzero counts (35). Due to some participants wearing the ActiGraph during nighttime sleeping, a maximum daily wear time threshold was set at 19 hours using a pragmatic choice based on participants’ diaries and sleep time duration recommendations for older adults (36). For participants meeting the selected threshold for maximum wear time the activity diary was used to determine whether the wear time by the software was similar to the activity diaries. For relevant participants, a log diary was used to determine daily wear time when awake.
SB was defined as <100 counts per minute (CPM), LPA as 100–2019 CPM, and MVPA as ≥2,020 CPM (37) on the vertical axis. Daily step counts were also extracted. Values were normalized to the total wear time. Raw accelerometry data were analyzed using ActiLife v6.13.3 software with the normal filter and summarized into 10-second epochs, as have been recommended for estimation of SB in clinical older adult populations (38). Values were normalized against total wear time and the proportions of daily time spent in SB, LPA, and MVPA are presented.
Data Analysis
Baseline cross-sectional characteristics were presented descriptively as mean and SD for continuous variables or number and percentage for categorical variables.
Analyses followed the guide to compositional data analysis for SB, PA, and sleep research published by Chastin and colleagues (21). Accelerometer-determined compositional descriptive statistics including compositional geometric means for central tendency and variation matrices for dispersion were calculated among the overall study sample and also for each country’s sample separately. Log-ratio plots with the three behaviors (SB, LPA, and MVPA) were generated to show the distribution of the sample compositions using the CoDaPack software 2.02.21 (39).
The composition of daily sedentary time according to sedentary activity was obtained crossing the context-specific distribution of self-reported sedentary time using the SBQ, with the percentage of daily sedentary time assessed with accelerometry. Descriptive results were presented for the overall sample, by country, and by sex.
To assess the covariates related to accelerometer-derived sedentary time, a linear regression analysis was conducted with covariables: country of residence, age, sex, civil status (single vs. other—in a relationship, widowed or, separated), education (primary vs. secondary vs. post-secondary), number of medications currently taken, category of BMI (obese when BMI is ≥30 kg/m2 vs. overweight when BMI is 25–29.9 kg/m2 vs. normal weight when BMI is 18.5–24.9 kg/m2), and gait speed. The fixed-effects regression model included country as a cluster factor to take into account any potential correlation between participants in the same country, by setting up a diagonal covariance matrix structure for the residuals. The results were reported as unstandardized regression coefficients with 95% confidence intervals.
Statistical test significance was assessed at the usual 5% significance level. For the statistical analyses, STATA V13 software was used.
Results
Of the overall SITLESS participants (n = 1,360), mean age was 75.3 (SD 6.3) years (range from 72.8 years in United Kingdom to 77.4 years in Denmark) and 840 (61.8%) were women (Table 1). Half of the sample were married (52.6%), whereas 27.0% were widowed. Participants (53.2%) reported having completed secondary education, with German participants having the highest proportion at 71.6%, whereas Spanish participants had the lowest one (30.8%). Participants from Germany and Spain reported the highest number of medical conditions (3.5 [SD 2.1] and 3.4 [SD 2.2], respectively), and current medications ranged from 0 to 19 across all participants (mean 4.5). Gait speed was the slowest in German and Danish participants (1.0 [SD 0.2] m/s in both sites). Mean BMI was 28.9 (SD 5.2) kg/m2. Self-reported SB did not differ between weekdays versus weekend days among the overall sample. The self-reported average mean hours per day in SB was 7.75 (SD 2.9).
Table 1.
Sociodemographic and Movement Behavior Characteristics of the Study Sample
| Overall (n = 1,360) | Denmark (n = 338) | Spain (n = 356) | United Kingdom (n = 321) | Germany (n = 345) | |
|---|---|---|---|---|---|
| Age, y, mean (SD) | 75.3 (6.3) | 77.4 (5.7) | 76.0 (6.5) | 72.8 (5.7) | 74.8 (6.2) |
| Sex, n (%) women | 840 (61.8) | 197 (58.3) | 273 (76.7) | 172 (53.6) | 198 (57.4) |
| Civil status, n (%) | |||||
| Single | 117 (8.9) | 43 (13.0) | 28 (8.2) | 19 (6.0) | 27 (8.3) |
| Married/stable relationship | 690 (52.6) | 149 (45.2) | 173 (50.9) | 186 (58.5) | 182 (56.0) |
| Widow/widower | 354 (27.0) | 104 (31.5) | 111 (32.6) | 71 (22.3) | 68 (20.9) |
| Divorced | 147 (11.2) | 34 (10.3) | 28 (8.2) | 42 (13.2) | 43 (13.2) |
| Unknown | 5 (0.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (1.5) |
| Education, n (%) | |||||
| I do not know how to read or write | 5 (0.4) | 0 (0.0) | 5 (1.5) | 0 (0.0) | 0 (0.0) |
| I know how to read and write | 36 (2.7) | 1 (0.3) | 34 (10.0) | 0 (0.0) | 1 (0.3) |
| Primary education | 279 (20.8) | 97 (28.9) | 151 (44.3) | 20 (6.3) | 11 (3.2) |
| Secondary education | 712 (53.2) | 195 (58.0) | 105 (30.8) | 167 (52.2) | 245 (71.6) |
| University | 303 (22.6) | 42 (12.5) | 45 (13.2) | 132 (41.3) | 84 (24.6) |
| Unknown | 3 (0.2) | 1 (0.3) | 1 (0.3) | 1 (0.3) | 0 (0.0) |
| Number of self-reported medical conditions: mean (SD) | 2.9 (2.1) | 2.9 (1.8) | 3.4 (2.2) | 1.9 (1.7) | 3.5 (2.1) |
| Number of current medications, mean (range) | 4.5 (0–19) | 4.0 (0–14) | 4.0 (0–17) | 4.9 (0–19) | 4.4 (0–16) |
| BMI, mean (SD) | 28.9 (5.2) | 27.4 (5.0) | 29.8 (4.9) | 29.0 (5.1) | 29.3 (5.6) |
| BMI categories, n (%) | |||||
| Underweight and normal | 301 (22.3) | 111 (33.0) | 54 (15.3) | 68 (21.3) | 68 (19.7) |
| Overweight | 555 (41.1) | 136 (40.5) | 140 (39.8) | 131 (41.1) | 148 (42.9) |
| Obese | 496 (36.7) | 89 (26.5) | 158 (44.9) | 120 (37.6) | 129 (37.4) |
| Gait speed, mean (SD) | 1.1 (0.3) | 1.0 (0.2) | 1.1 (0.3) | 1.2 (0.2) | 1.0 (0.2) |
| Self-report SB, h/d, mean (SD) | |||||
| 7 d | 7.75 (2.9) | 7.93 (2.7) | 7.46 (3.3) | 7.86 (2.8) | 7.72 (2.5) |
| Weekday | 7.82 (3.0) | 7.85 (2.8) | 7.59 (3.6) | 8.08 (3.1) | 7.78 (2.6) |
| Weekend day | 7.54 (3.0) | 8.13 (2.9) | 7.05 (3.2) | 7.30 (2.8) | 7.62 (2.7) |
| Accelerometrya | n = 1,266 | n = 326 | n = 313 | n = 310 | n = 317 |
| % daily sedentary time | 78.8 (7.0) | 81.0 (6.6) | 79.2 (6.6) | 76.5 (6.5) | 78.4 (7.4) |
| % daily LPA time | 18.6 (5.8) | 17.2 (5.6) | 18.5 (5.9) | 19.8 (5.2) | 18.9 (6.1) |
| % daily MVPA time | 2.6 (2.3) | 1.8 (1.8) | 2.3 (1.9) | 3.7 (2.6) | 2.7 (2.2) |
| Number daily steps, mean (SD) | 5,056.0 (2,596.9) | 4,420.1 (2,409.7) | 5,225.7 (2,302.8) | 5,838.5 (2,985,3) | 4,777.1 (2,439.5) |
| MVPA daily counts, mean (SD) | 2,945.3 (386.8) | 2,915.3 (352.4) | 2,844.7 (335.8) | 3,062.3 (388.0) | 2,961.1 (433.6) |
| Daily wear time, h, mean (SD) | 14.4 (1.1) | 14.5 (1.1) | 14.3 (1.2) | 14.3 (1.1) | 14.3 (1.2) |
Notes: BMI = body mass index; LPA = light-intensity physical activity; MVPA = moderate-to-vigorous physical activity. an of participants with valid accelerometry data.
Composition of Accelerometer-Measured SB and PA
Overall, participants spent 78.8% of daily awake time in SB, 18.6% in LPA, and 2.6% in MVPA (375 participants with less than 1%). Participants in Denmark showed the highest percentage of daily awake time in SB (81%), followed by participants from Spain (79.2%), Germany (78.4%), and the United Kingdom (76.5%). LPA ranged from 17.2% of waking time among participants from Denmark to 19.8% among participants in the United Kingdom. MVPA accounted for less than 4% of waking time across all four sites (Denmark 1.8%; Spain 2.3%; Germany 2.7%; and United Kingdom 3.7%). Accelerometry showed minimal differences by sex (data not in table), with women engaging in more LPA (19.7% [SD 5.6] vs. 16.6% [SD 5.5]) and walking (5,099 steps/day [SD 2,436.1] vs. 4,987 steps/day [SD 2,839.7]) and men engaging in higher amounts of MVPA (2.8% [SD 2.6] vs. 2.5% [SD 2.1]).
Participants in the United Kingdom took the highest mean number of daily steps with 5,839 (SD 2,985), with participants from Denmark taking the lowest (mean 4,420 [SD 2,410]).
Figure 1 shows the sample composition of time spent in SB, LPA, and MVPA for the whole sample, by means of a matrix of ternary plots with the three behaviors represented at a time. Ternary plots can be understood as the scatterplots of compositions. The overlap of points toward the SB corner indicates the highest data concentration in this behavior. The dispersion structure is represented by 99% and 95% normal-based probability regions around the compositional center. These reflect that the highest variability is found in the direction of MVPA, with some variability toward the LPA.
Figure 1.
Ternary plots of the sample composition of time spent in sedentary behavior (X), light physical activity (Y), and moderate-to-vigorous physical activity (Z) for the whole sample (A) and for the whole sample centered (B).
The variability of the data is summarized in the variation matrix (Supplementary File 1) containing all pair-wise log-ratio variances. A value close to zero implies that the time spent in the two behaviors involved in the ratio (arranged by rows and columns) is highly proportional. For example, the variance of log(SB/LPA) ranges from 0.138 to 0.206, which reflects the highest (proportional) relationship or codependence (not correlation in the usual sense) between two behaviors. On the other end, it can be observed that the highest log-ratio variances all involve MVPA, which shows that time spent in MVPA is the least codependent on the other behaviors (is independent of LPA and SB).
Self-report Context-Specific Sedentary Behavior
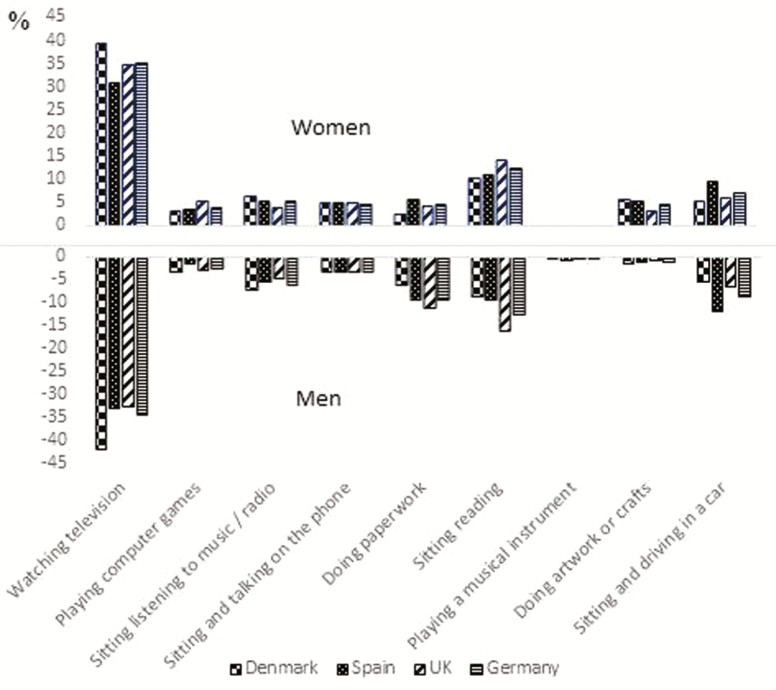
Table 2 shows the descriptive statistics of the proportion of time spent in context-specific SBs by participants of the four European countries and by sex. Watching television and reading were the context-specific SBs that accounted for most of the daily time in the four countries (34.8% and 12.4% respectively; ie, 47.2% of daily waking hours). Distribution of context-specific SBs was broadly similar across countries. The highest proportion of daily sedentary time was spent watching television, and Spain showed the highest percentage with 40.1% (SD 17.8), followed by Denmark (34.2% [SD 14.0]), Germany (33.8% [SD 15.1]), and the United Kingdom showing the lowest (31.7% [SD 12.9]). Distribution of activities by sex was similar, with some differences in activities such as doing paperwork (9.9% [SD 11.5] in men and 4.6% [SD 6.9] in women) and doing artwork or crafts (1.3% [SD 4.5] in men and 4.6% [SD 8.5] in women; Figure 2).
Table 2.
Compositional Descriptive Statistics of the Percentage of Daily Time Spent in Context-Specific Sedentary Behaviors by Country
| Overalla (n = 1,230) | Denmark (n = 325) | Spain (n = 284) | United Kingdom (n = 309) | Germany (n = 312) | Overall Men (n = 474) | Overall Women (n = 756) | |
|---|---|---|---|---|---|---|---|
| Daily % | |||||||
| Watching television | 34.8 (15.3) | 34.2 (14.0) | 40.1 (17.8) | 31.7 (12.9) | 33.8 (15.1) | 34.6 (15.4) | 35.0 (15.2) |
| Playing computer games | 3.6 (7.2) | 3.6 (7.4) | 3.6 (7.3) | 2.7 (5.8) | 4.4 (7.8) | 2.9 (6.6) | 4.1 (7.5) |
| Sitting listening to music/radio | 5.7 (7.9) | 6.2 (8.5) | 6.8 (9.3) | 5.3 (6.8) | 4.6 (6.6) | 6.3 (8.0) | 5.4 (7.8) |
| Sitting and talking on the phone | 4.2 (4.1) | 3.7 (3.2) | 4.6 (5.3) | 4.2 (3.6) | 4.3 (4.0) | 3.4 (3.3) | 4.7 (4.4) |
| Doing paperwork | 6.6 (9.3) | 7.5 (8.8) | 3.7 (7.4) | 7.4 (9.4) | 7.4 (10.7) | 9.9 (11.5) | 4.6 (6.9) |
| Sitting reading | 12.4 (9.2) | 14.0 (9.8) | 9.9 (8.8) | 10.3 (7.6) | 15.1 (9.3) | 12.6 (9.6) | 12.3 (9.0) |
| Playing a musical instrument | 0.4 (2.0) | 0.5 (2.6) | 0.2 (1.7) | 0.5 (2.0) | 0.4 (1.6) | 0.6 (2.4) | 0.3 (1.8) |
| Doing artwork or crafts | 3.4 (7.4) | 2.8 (7.1) | 5.0 (8.5) | 3.5 (8.0) | 2.2 (5.5) | 1.3 (4.5) | 4.6 (8.5) |
| Sitting and driving in a car | 7.7 (6.5) | 8.3 (6.4) | 5.5 (5.2) | 10.6 (7.4) | 6.2 (5.3) | 8.9 (7.3) | 6.9 (5.7) |
Note: an of participants with valid accelerometry and Sedentary Behavior Questionnaire data.
Figure 2.
Distribution of daily time spent in context-specific sedentary behaviors by sex and country.
Correlates of Sedentary Time
Table 3 displays correlates of sedentary time according to the country of residence, age, sex, civil status, education, medication, gait speed, and BMI. Most of the variables had a weak association with daily sedentary time. Participants who were male (women = reference; β = 2.78), those who declared themselves to be single (eg, had never been married or living with a stable relationship; not single = reference; β = 1.89), and those with upper-secondary education (education level, primary = reference; β = 1.54) were more likely to be sedentary.
Table 3.
Mixed Linear Regression Analysis of Correlates of Sedentary Timea per Country
| SITLESS Overall Sample (n = 1,360) | |||
|---|---|---|---|
| Β | 95% CI | p Value | |
| Constant | 89.85 | (86.39, 93.32) | <.001 |
| Site (Denmark = reference) | |||
| Spain | −0.22 | (−1.25, −0.81) | .671 |
| United Kingdom | −3.14 | (−4.18, −2.10) | <.001 |
| Germany | −2.95 | (−3.97, −1.93) | <.001 |
| Age (y) | 0.23 | (0.17, 0.29) | <.001 |
| Sex | |||
| Men (women = reference) | 2.78 | (2.05, 3.52) | <.001 |
| Civil status | |||
| Single (not single = reference) | 1.89 | (0.67, 3.12) | .002 |
| Education level (primary = reference) | |||
| Secondary | 0.83 | (−0.11, 1.77) | .084 |
| Higher | 1.54 | (0.39, 2.69) | .009 |
| Number of current medications | 0.36 | (0.24, 0.47) | <.001 |
| BMI (kg/m2) (obese = reference) | |||
| Under or normal weight | −2.77 | (−3.74, −1.80) | <.001 |
| Overweight | −1.98 | (−2.79, −1.17) | <.001 |
| Gait speed (m/s) | −4.29 | (−5.83, −2.75) | <.001 |
Notes: BMI = body mass index; CI = confidence interval; SE = unstandardized regression coefficients and standard errors. Likelihood test for the cluster component, p = .0098.
aExpressed as percentage of total wear time.
Sedentary time increased with age and number of medications taken, and it was also higher in participants with slower gait speed. For each 10-year increase in age over 65 years (the minimum to be included in the study), sedentary time increased two percentage points (2.3%). A clinically relevant change in gait speed of 0.1 m/s (40) translated into a change of 0.43 percentage points of sedentary time. Compared with obese participants (obese = reference; β = 1), those with who were overweight (β = −1.98) and normal weight (β = −2.77) were less sedentary.
The model accounted for within-country correlation of participants in the same site, which is not negligible as shown by the significant likelihood test comparing this model against a standard regression model with no clustering (p = .0098).
Discussion
In 1,360 participants of a multicenter study including four European countries (the SITLESS study), we show that participants spent 78.8% of daily awake time in SB, 18.6% in LPA, and 2.6% in MVPA. Accelerometry showed minimal differences by sex with women engaging in more LPA and walking and men engaging in higher amounts of MVPA. Notably, we found that correlates of SB were broadly similar in the four included countries except for a few minor differences, an observation that enables a relative general preventative strategy applicable to older adults in similar socioeconomic living conditions, irrespective of the country.
A recent study in a cohort of Dutch older adults showed that participants spent on average 65% of total wear time sedentary, 33% performing LPA, and 2% MVPA using the same tri-axial accelerometer worn at the hip (16). The mean age in van Ballegooijen and colleagues’ (16) study was younger compared with our study (70.7 [SD 8] years vs. 75.3 [SD 6.3] years), and this might partly explain the differences. Several studies have reported higher proportions of time spent being sedentary in older age groups using hip-worn accelerometers (41–43). However, the difference noted in daily time in SB and LPA in both studies might also be related to a lower health status reported by the SITLESS participants. In our study, women engaged in more LPA and walking and men engaged in higher amounts of MVPA, whereas daily SB was similar. Similarly, in a recent study, combined categories of SB and PA indicated that men were more often high sedentary and high physically active, whereas women were more often low sedentary and low physically active (16). These differences could be partly explained by traditional gender roles, where women may be in charge of household chores and thus engaging in LPA, and men being more sedentary at home and engaging in more organized and regimented PA.
In our study, as in previous literature (21), the highest log-ratio variances all involved MVPA, which shows that time spent in MVPA is the least codependent with the other behaviors and might be unreliable. As shown in previous studies (44), environmental-, social-, and individual-level determinants for sedentary time are distinct from those linked to the adoption and maintenance of MVPA. As a result, novel intervention strategies that focus on reducing SB and increasing any intensity of PA by leveraging the surrounding environment (eg, home) as well as individual-level cues and habits of SB should be designed and tested (45).
The percentage of daily time spent in SB in older adults is concerning. A better understanding of the distribution of movement behavior across the awake-time span will benefit and inform the development of cost-effective public health interventions. Reducing sitting could potentially improve older adults’ subjectively and objectively measured health status (46,47) and well-being (48). Thus, focusing on ways to reduce sitting with nonsitting activities (eg, doing some activities that are usually completed in a seated position by standing up) may be a promising first step to address sedentary time among older adults.
Because LPA appears to makeup a larger proportion of the day compared with MVPA in older adults, replacing SB with LPA seems to be the second step to designing successful strategies to enhance movement without immediately increasing MVPA, which might not be feasible for some older adults. This may eventually lead to a progression to higher-intensity activities, if this is safe and appropriate for the individual. Thus, efforts that target SB as a means to increase LPA is a new behavioral leverage-point that could help us increase overall PA and induce health benefits within the population (45). A recent study using isotemporal substitution regression modeling to assess the relationship of replacing the amount of time spent in one activity for another showed that replacing 60 min/d of SB with 10 min/d of MVPA and 50 min/d of LPA was associated with significant improvements in physical function (49). However, there is little evidence to guide SB limiting strategies or LPA promotion activities for older adults (50).
Our study showed that the highest proportion of daily sedentary time was spent watching television (34.8%) and reading (12.4%), with a similar percentage among men and women. Time spent watching television has been related to increased odds for multimorbidity (51), and the risk for multiple chronic conditions has been previously investigated to be higher for those spending more time watching television (52). Being physically active (ie, spending ≥ 30 min/d of MVPA for at least 5 d/wk) has not only been beneficial for having reduced risk of multiple morbidities, but also helped to attenuate or eliminate the negative role of watching television (51). However, mean MVPA in our older adults accounted for less than 2% of waking hours, highlighting the difficulty of acquiring such benefits in an older adult population and stressing the importance of reducing SB with LPA. Detrimental associations of SB while watching television with various health outcomes (53) may be due to the continuous nature of television viewing and its linked unhealthy behaviors such as eating snacks or smoking. Following our first step approach, breaking television time by simple means (eg, standing up during advertisement breaks and leaving remote control on TV which would require standing up to switch program) should be a key strategy to reduce the health impact of SB among older adults, and when done with a partner one could act as a reminder to the other.
Distribution of activities by sex, in general, showed some differences such as doing paperwork being more common in men and doing artwork or crafts being more common in women. Previous research has provided some insight into the type and context of SB and has shown that sitting activities, which older adults typically engage in, include watching television, reading, eating meals, using the computer and transport (54). A recent study showed that many sedentary activities are embedded in older adults’ lives as part of their daily routines, meaning that they might be difficult to change (55). A small number of qualitative studies have begun to explore factors that influence older adults’ SB. These studies suggest that older adults enjoy and recognize the physical, social, and mental benefits of some sitting community-based activities (eg, doing arts, crafts, and puzzles) (56,57), but view excessive sitting as unhealthy. However, older adults tend to report that many community activities are not only sedentary (56), but also lack the availability of information about community-based resources that lead them to sit more (57). A third step in the approach to engaging older adults in healthier lifestyles could be offering information about community-based activities using each country’s existing primary prevention pathways (eg, primary health care professionals in Spain and the United Kingdom or preventive home visits in Denmark), ideally thought to engage both men and women according to their preferences, and searching for alternatives to perform such activities in a nonsitting position.
It would also be interesting to know when these context-specific SB activities take place during the day. One study using time-lapse cameras suggested that older adults often sit most in the afternoon and evening (compared with the morning), and when they are alone at home (58). Following our second and third-step approach, promising strategies may be to reduce television time mainly in the afternoon by first, supporting older adults to go out more and engage in community-based activities in local facilities and other resources (eg, community groups). Supporting older adults to remain socially active will not only support them to reduce SB, but might help enhance new social connections and reduce social isolation, which is associated with poor health (59).
In our study, being older, a man, single, taking more medications per day, and being obese and overweight were important correlates of higher levels of SB time. Recent studies showed that men, those who were older, and those with higher BMI were also found to be more sedentary (16,28,41,42,60). A previous study among Japanese older adults revealed living alone was significantly associated with prolonged television viewing time (61). Living with a partner was associated with more activity in participants younger than 80 years and in those with BMI ≥ 27 kg/m2 in another study (28). The results from this and previous studies suggest the need for opportunities of focused intervention, highlighting the need to engage older adults in group-based community activities with those sharing a similar profile to themselves (eg, single or overweight).
SB was also higher in participants with slower gait speed in our study, similar to that reported in another study (16). SB shows a tendency to increase with frailty-related outcomes in the current literature such as age, loneliness, and mobility restrictions (62). Slowing gait may reflect both damaged systems and a high-energy cost of walking (63–65). Gait speed, age, and sex may offer the clinician tools for assessing expected survival to contribute to tailoring goals of care in older adults (66). German and Danish participants showed the slowest gait speed and German participants reported the highest number of medical conditions, probably due to the most common recruitment pathway in Germany that used invitation letters sent from health professionals targeting participants with major health needs. Once again, our fourth step is that these outcomes should be borne in mind when designing and prioritizing health-related interventions for older adults.
This study has not only several strengths but also limitations. It is the first study providing a comprehensive description of the composition of accelerometer-measured SB and PA time in a cohort of community-dwelling older adults from four European countries, combining self-reported information not available from accelerometry. However, as the accelerometer was not worn during the 24-hour period, we did not include sleep time in the compositional analysis, so that the movement composition was assessed as a proportion of wearing time, which may vary among participants. For the present study, we could only use a cross-sectional approach and therefore the temporal relationship between the investigated correlates and SB is unclear. The accelerometer presents some well-known limitations to assess posture that could be overcome using an inclinometer (eg, time spent standing is likely to be classified as sedentary using an accelerometer). In addition, the representativeness for the different populations is difficult to estimate.
Conclusions
This sample of older adults from four European countries on average spent 78.8% of daily awake time in SB, 18.6% in LPA, and 2.6% in MVPA. Accelerometry showed minimal differences by sex with women engaging in more LPA and walking and men engaging in higher amounts of MVPA. The highest proportion of self-reported daily sedentary time was spent watching television and reading. Notably, the distribution of context-specific sedentary activities by country and sex showed only minor differences. Being older, a man, single, taking more medications per day, being obese and overweight, and having a slower gait speed were important correlates of more sedentary time. A clinically relevant change in gait speed can decrease almost 0.45 percentage points of sedentary time. With an ever aging European population, the high amount of SB of our participants emphasizes the need to encourage older adults to reduce sitting time with nonsitting activities.
Funding
This work was supported by the European Union program Horizon 2020 (H2020-Grant 634270).
Conflict of Interest
None reported.
Supplementary Material
Acknowledgments
The named authors present the study on behalf of the SITLESS Group: Laura Coll-Planas (PI), Maria Giné-Garriga, Àlex Domingo, Marta Roqué, Antoni Salvà, Míriam Guerra, Carme Martín-Borràs, Javier Jerez-Roig, Oriol Sansano-Nadal, Marta Santiago, Kelly Ferry, Manel Font, Ana Claudia Farche, Paolo Caserotti, Mathias Skjødt, Mark A. Tully, Frank Kee, Jason J. Wilson, Nicole E. Blackburn, Ilona McMullan, Michael Denkinger, Dietrich Rothenbacher, Katharina Wirth, Dhayana Dallmeier, Emma McIntosh, Manuela Deidda, Guillaume Lefebvre, and Denise González.
References
- 1. Tremblay MS, Aubert S, Barnes JD, et al. ; SBRN Terminology Consensus Project Participants Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kim Y, Lee E. The association between elderly people’s sedentary behaviors and their health-related quality of life: focusing on comparing the young-old and the old-old. Health Qual Life Outcomes. 2019;17:131. doi: 10.1186/s12955-019-1191-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim J, Im J-S, Choi Y-H. Objectively measured sedentary behavior and moderate-to-vigorous physical activity on the health-related quality of life in US adults: the National Health and Nutrition Examination Survey 2003–2006. Qual Life Res. 2017;26:1315–1326. doi: 10.1007/s11136-016-1451-y [DOI] [PubMed] [Google Scholar]
- 4. Heron L, O’Neill C, McAneney H, Kee F, Tully MA. Direct healthcare costs of sedentary behaviour in the UK. J Epidemiol Community Health. 2019;73:625–629. doi: 10.1136/jech-2018-211758 [DOI] [PubMed] [Google Scholar]
- 5. Gennuso KP, Gangnon RE, Matthews CE, Thraen-Borowski KM, Colbert LH. Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc. 2013;45:1493–1500. doi: 10.1249/MSS.0b013e318288a1e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95:437–445. doi: 10.3945/ajcn.111.019620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maher C, Olds T, Mire E, Katzmarzyk PT. Reconsidering the sedentary behaviour paradigm. PLoS One. 2014;9:e86403. doi: 10.1371/journal.pone.0086403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996-2011. Am J Prev Med. 2011;41:207–215. doi: 10.1016/j.amepre.2011.05.004 [DOI] [PubMed] [Google Scholar]
- 9. Harvey JA, Chastin SF, Skelton DA. How sedentary are older people? A systematic review of the amount of sedentary behavior. J Aging Phys Act. 2015;23:471–487. doi: 10.1123/japa.2014-0164 [DOI] [PubMed] [Google Scholar]
- 10. Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults a systematic review and meta-analysis. Ann Intern Med. 2015;162:123–132. doi: 10.7326/M14-1651 [DOI] [PubMed] [Google Scholar]
- 11. de Rezende LFM, Rey-López JP, Matsudo VKR, Luiz O do C. Sedentary behavior and health outcomes among older adults: a systematic review. BMC Public Health. 2014;14:333. doi: 10.1186/1471-2458-14-333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wullems JA, Verschueren SM, Degens H, Morse CI, Onambélé GL. A review of the assessment and prevalence of sedentarism in older adults, its physiology/health impact and non-exercise mobility counter-measures. Biogerontology. 2016;17:547–565. doi: 10.1007/s10522-016-9640-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Celis-Morales CA, Perez-Bravo F, Ibañez L, Salas C, Bailey ME, Gill JM. Objective vs. self-reported physical activity and sedentary time: effects of measurement method on relationships with risk biomarkers. PLoS One. 2012;7:e36345. doi: 10.1371/journal.pone.0036345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ensrud KE, Blackwell TL, Cauley JA, et al. ; Osteoporotic Fractures in Men Study Group Objective measures of activity level and mortality in older men. J Am Geriatr Soc. 2014;62:2079–2087. doi: 10.1111/jgs.13101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. World Health Organization. Global Recommendations on Physical Activity for Health. Geneva, Switzerland: World Health Organization; 2010. [PubMed] [Google Scholar]
- 16. van Ballegooijen AJ, van der Ploeg HP, Visser M. Daily sedentary time and physical activity as assessed by accelerometry and their correlates in older adults. Eur Rev Aging Phys Act. 2019;16:3. doi: 10.1186/s11556-019-0210-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Physical Activity Guidelines Committee. Physical Activity Guidelines Committee Report. Washington, DC: U.S. Department of Health and Human Services; 2008. www.health.gov/paguidelines/report. [Google Scholar]
- 18. U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd ed.Washington, DC: U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 19. Füzéki E, Engeroff T, Banzer W. Health benefits of light-intensity physical activity: a systematic review of accelerometer data of the National Health and Nutrition Examination Survey (NHANES). Sports Med. 2017;47:1769–1793. doi: 10.1007/s40279-017-0724-0 [DOI] [PubMed] [Google Scholar]
- 20. LaCroix AZ, Bellettiere J, Rillamas-Sun E, et al. ; Women’s Health Initiative (WHI) Association of light physical activity measured by accelerometry and incidence of coronary heart disease and cardiovascular disease in older women. JAMA Netw Open. 2019;2:e190419. doi: 10.1001/jamanetworkopen.2019.0419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chastin SF, Palarea-Albaladejo J, Dontje ML, Skelton DA. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: a novel compositional data analysis approach. PLoS One. 2015;10:e0139984. doi: 10.1371/journal.pone.0139984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131. PMID: 3920711. [PMC free article] [PubMed] [Google Scholar]
- 23. McPhee JS, French DP, Jackson D, Nazroo J, Pendleton N, Degens H. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. 2016;17:567–580. doi: 10.1007/s10522-016-9641-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tam-Seto L, Weir P, Dogra S. Factors influencing sedentary behaviour in older adults: an ecological approach. AIMS Public Health. 2016;3:555–572. doi: 10.3934/publichealth.2016.3.555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Copeland JL, Ashe MC, Biddle SJ, et al. Sedentary time in older adults: a critical review of measurement, associations with health, and interventions. Br J Sports Med. 2017;51:1539. doi: 10.1136/bjsports-2016-097210 [DOI] [PubMed] [Google Scholar]
- 26. Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, Sallis JF. Adults’ sedentary behavior determinants and interventions. Am J Prev Med. 2011;41:189–196. doi: 10.1016/j.amepre.2011.05.013 [DOI] [PubMed] [Google Scholar]
- 27. Chastin SF, Buck C, Freiberger E, et al. ; DEDIPAC Consortium Systematic literature review of determinants of sedentary behaviour in older adults: a DEDIPAC study. Int J Behav Nutr Phys Act. 2015;12:127. doi: 10.1186/s12966-015-0292-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Koolhaas CM, van Rooij FJA, Schoufour JD, et al. Objective measures of activity in the elderly: distribution and associations with demographic and health factors. J Am Med Dir Assoc. 2017;18:838–847. doi: 10.1016/j.jamda.2017.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Viken H, Aspvik NP, Ingebrigtsen JE, Zisko N, Wisløff U, Stensvold D. Correlates of objectively measured physical activity among Norwegian older adults: the Generation 100 Study. J Aging Phys Act. 2016;24:369–375. doi: 10.1123/japa.2015-0148 [DOI] [PubMed] [Google Scholar]
- 30. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ku P-W, Steptoe A, Liao Y, Hsueh M-C, Chen L-J. A threshold of objectively-assessed daily sedentary time for all-cause mortality in older adults: a meta-regression of prospective cohort studies. J Clin Med. 2019;8:564. doi: 10.3390/jcm8040564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Giné-Garriga M, Coll-Planas L, Guerra M, et al. The SITLESS project: exercise referral schemes enhanced by self-management strategies to battle sedentary behaviour in older adults: study protocol for a randomised controlled trial. Trials. 2017;18:221. doi: 10.1186/s13063-017-1956-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rosenberg DE, Norman GJ, Wagner N, Patrick K, Calfas KJ, Sallis JF. Reliability and validity of the Sedentary Behavior Questionnaire (SBQ) for adults. J Phys Act Health. 2010;7:697–705. doi: 10.1123/jpah.7.6.697 [DOI] [PubMed] [Google Scholar]
- 34. Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47:1821–1845. doi: 10.1007/s40279-017-0716-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43:357–364. doi: 10.1249/MSS.0b013e3181ed61a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1:40–43. doi: 10.1016/j.sleh.2014.12.010 [DOI] [PubMed] [Google Scholar]
- 37. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- 38. Byrom B, Rowe DA. Measuring free-living physical activity in COPD patients: deriving methodology standards for clinical trials through a review of research studies. Contemp Clin Trials. 2016;47:172–184. doi: 10.1016/j.cct.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 39. Comas M, Thió-Henestrosa S.. CoDaPack 2.0: A Stand-Alone, Multi-platform Compositional Software. Spain: Universitat de Girona. [Google Scholar]
- 40. Miller ME, Magaziner J, Marsh AP, et al. ; LIFE Investigators Gait speed and mobility disability: revisiting meaningful levels in diverse clinical populations. J Am Geriatr Soc. 2018;66:954–961. doi: 10.1111/jgs.15331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Arnardottir NY, Koster A, Van Domelen DR, et al. Objective measurements of daily physical activity patterns and sedentary behaviour in older adults: Age, Gene/Environment Susceptibility-Reykjavik Study. Age Ageing. 2013;42:222–229. doi: 10.1093/ageing/afs160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Berkemeyer K, Wijndaele K, White T, et al. The descriptive epidemiology of accelerometer-measured physical activity in older adults. Int J Behav Nutr Phys Act. 2016;13:2. doi: 10.1186/s12966-015-0316-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Davis MG, Fox KR, Hillsdon M, Sharp DJ, Coulson JC, Thompson JL. Objectively measured physical activity in a diverse sample of older urban UK adults. Med Sci Sports Exerc. 2011;43:647–654. doi: 10.1249/MSS.0b013e3181f36196 [DOI] [PubMed] [Google Scholar]
- 44. Koohsari MJ, Sugiyama T, Sahlqvist S, Mavoa S, Hadgraft N, Owen N. Neighborhood environmental attributes and adults’ sedentary behaviors: review and research agenda. Prev Med. 2015;77:141–149. doi: 10.1016/j.ypmed.2015.05.027 [DOI] [PubMed] [Google Scholar]
- 45. Keadle SK, Conroy DE, Buman MP, Dunstan DW, Matthews CE. Targeting reductions in sitting time to increase physical activity and improve health. Med Sci Sports Exerc. 2017;49:1572–1582. doi: 10.1249/MSS.0000000000001257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dogra S, Ashe MC, Biddle SJH, et al. Sedentary time in older men and women: an international consensus statement and research priorities. Br J Sports Med. 2017;51:1526–1532. doi: 10.1136/bjsports-2016-097209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wilson JJ, Blackburn NE, O’Reilly R, Kee F, Caserotti P, Tully MA. Association of objective sedentary behaviour and self-rated health in English older adults. BMC Res Notes. 2019;12:12. doi: 10.1186/s13104-019-4050-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ellingson LD, Meyer JD, Shook RP, et al. Changes in sedentary time are associated with changes in mental wellbeing over 1 year in young adults. Prev Med Rep. 2018;11:274–281. doi: 10.1016/j.pmedr.2018.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lerma NL, Cho CC, Swartz AM, Miller NE, Keenan KG, Strath SJ. Isotemporal substitution of sedentary behavior and physical activity on function. Med Sci Sports Exerc. 2018;50:792–800. doi: 10.1249/MSS.0000000000001491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Aunger JA, Doody P, Greig CA. Interventions targeting sedentary behavior in non-working older adults: a systematic review. Maturitas. 2018;116:89–99. doi: 10.1016/j.maturitas.2018.08.002 [DOI] [PubMed] [Google Scholar]
- 51. Marques A, Santos DA, Peralta M, Sardinha LB, González Valeiro M. Regular physical activity eliminates the harmful association of television watching with multimorbidity. A cross-sectional study from the European Social Survey. Prev Med. 2018;109:28–33. doi: 10.1016/j.ypmed.2018.01.015 [DOI] [PubMed] [Google Scholar]
- 52. Keadle SK, Moore SC, Sampson JN, Xiao Q, Albanes D, Matthews CE. Causes of death associated with prolonged TV viewing: NIH-AARP diet and health study. Am J Prev Med. 2015;49:811–821. doi: 10.1016/j.amepre.2015.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Grøntved A, Hu FB. Television Viewing and Risk of Type 2 Diabetes, Cardiovascular Disease, and All-Cause Mortality: A Meta-Analysis http://jama.jamanetwork.com/. [DOI] [PMC free article] [PubMed]
- 54. Lenz EK, Swartz AM, Strath SJ. Do sedentary behaviors modify the health status of older adults? Int J Kinesiol Sports Sci. 2014;2:13–22. doi: 10.7575/aiac.ijkss.v.2n.1p.13 [DOI] [Google Scholar]
- 55. Palmer VJ, Gray CM, Fitzsimons CF, et al. What do older people do when sitting and why? Implications for decreasing sedentary behavior. Gerontologist. 2019;59:686–697. doi: 10.1093/geront/gny020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Chastin SF, Fitzpatrick N, Andrews M, DiCroce N. Determinants of sedentary behavior, motivation, barriers and strategies to reduce sitting time in older women: a qualitative investigation. Int J Environ Res Public Health. 2014;11:773–791. doi: 10.3390/ijerph110100773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Mcewan T, Tam-Seto L, Dogra S. Perceptions of sedentary behavior among socially engaged older adults. Gerontologist. 2017;57:735–744. doi: 10.1093/geront/gnv689 [DOI] [PubMed] [Google Scholar]
- 58. Leask CF, Harvey JA, Skelton DA, Chastin SF. Exploring the context of sedentary behaviour in older adults (what, where, why, when and with whom). Eur Rev Aging Phys Act. 2015;12:4. doi: 10.1186/s11556-015-0146-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Shibata A, Oka K, Ishii K, et al. Objectively-assessed patterns and reported domains of sedentary behavior among Japanese older adults. J Epidemiol. 2019;29:334–339. doi: 10.2188/jea.JE20180041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kikuchi H, Inoue S, Sugiyama T, Owen N, Oka K, Shimomitsu T. Correlates of prolonged television viewing time in older Japanese men and women. BMC Public Health. 2013;13:213. doi: 10.1186/1471-2458-13-213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Del Pozo-Cruz B, Mañas A, Martín-García M, et al. Frailty is associated with objectively assessed sedentary behaviour patterns in older adults: Evidence from the Toledo Study for Healthy Aging (TSHA). PLoS One. 2017;12:e0183911. doi: 10.1371/journal.pone.0183911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13:881–889. doi: 10.1007/s12603-009-0246-z [DOI] [PubMed] [Google Scholar]
- 64. Baezner H, Blahak C, Poggesi A, et al. ; LADIS Study Group Association of gait and balance disorders with age-related white matter changes: the LADIS study. Neurology. 2008;70:935–942. doi: 10.1212/01.wnl.0000305959.46197.e6 [DOI] [PubMed] [Google Scholar]
- 65. Atkinson HH, Rosano C, Simonsick EM, et al. ; Health ABC study Cognitive function, gait speed decline, and comorbidities: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2007;62:844–850. doi: 10.1093/gerona/62.8.844 [DOI] [PubMed] [Google Scholar]
- 66. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.