Key messages
A phenotype of SAPHO syndrome exists in which lesions are limited to the skull.
Dear Editor, SAPHO syndrome is an inflammatory disease [1]. Osteoarticular lesions associated with SAPHO syndrome are most frequently found on the anterior chest wall (63%) [2], and skull involvement is rare. Although SAPHO syndrome is characterized by aseptic inflammation of the bone joint, Cutibacterium acnes (C.ances) may be involved in the pathology of SAPHO syndrome, and a few cases of C. acnes have reportedly been detected in SAPHO syndrome bone cultures [3]. In this letter, we report a case of SAPHO syndrome, in which the lesions were limited to the skull and C. acnes was detected after 10 days of skull bone culture.
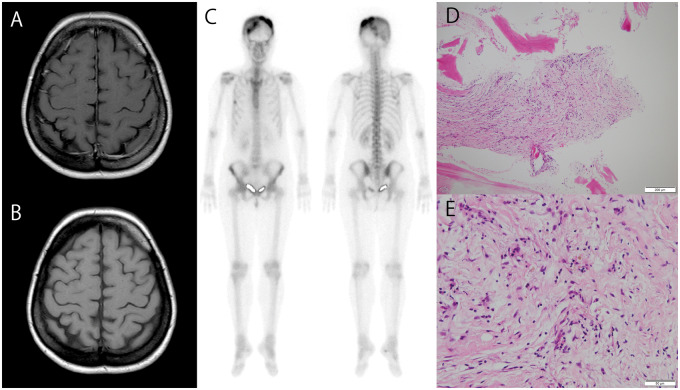
A 50-year-old woman with a background history of palmoplantar pustulosis presented with a 3-month history of intractable headache. She showed spontaneous pain throughout the head, with the strongest point on the left parietal region, and a pain visual analog scale value of 95 mm. She did not report any other joint pain. CRP levels were elevated to 6.57 mg/dl. Enhanced MRI showed a low-intensity area of bone marrow over a wide area of the skull on the T1-weighted image, and a contrast effect was observed on the bone marrow of the parietal and right frontal bones (Fig. 1A and B). Enhanced MRI did not show vessel wall thickening, luminal stenosis or arterial wall enhancement of the head, including the cranial artery and carotid artery. 99mTc-hydroxymethylene diphosphonate bone scintigraphy showed accumulation in the left parietal bone and the right frontal bone, but no accumulation was observed in other osteoarticular sites (Fig. 1C). An open biopsy of the left parietal bone was performed, in a clean operating room environment, using a strict disinfection protocol. Skull biopsy specimens showed the infiltration of fibroblasts, CD3+ T lymphocytes and CD20+ B lymphocytes, without any findings of malignancy (Fig. 1D and 1E). Additionally, C. acnes was detected in the long-term culture of a bone biopsy specimen. The patient met the modified diagnostic criteria for SAPHO syndrome in 2003 and was diagnosed with SAPHO syndrome. Given that loxoprofen was not sufficiently effective, minocycline was administered. After 6 weeks, the pain visual analog scale score improved to 15 mm, and CRP levels decreased to 1.03 mg/dl.
Fig. 1.
Enhanced MRI of the head and 99mTc-hydroxymethylene diphosphonate bone scintigraphy
(A) Enhanced MRI of the head, on a T1-weighted image, shows a low-signal area of the bone marrow over a wide area of the skull, and (B) a contrast effect was observed on the bone marrow of the parietal and right frontal bones. (C) 99mTc-hydroxymethylene diphosphonate bone scintigraphy shows accumulation in the left parietal and right frontal bones. The accumulation observed in the right rib was traumatic. (D, E) Skull biopsy specimens show the infiltration of fibroblasts, CD3+ T lymphocytes and CD20+ B lymphocytes, without any malignant findings.
Osteitis has been reported in 91% of patients with SAPHO syndrome [2]. Osteoarticular lesions associated with SAPHO syndrome are commonly observed in the anterior chest wall (63%), SI joints (40%) and vertebrae (33%). The mandible is the most common site for head lesions, which are observed in 10.8% of SAPHO syndrome patients, and skull involvement has been reported in only a few cases [4, 5]. However, one study reported osteitis lesions that were identified by bone scintigraphy in 157 patients who met the diagnostic criteria for SAPHO syndrome, and lesions of the neurocranium were observed in 7 (4.5%) patients, in the occipital bone (2.5%), temporal bone (1.3%) and parietal bone (0.6%) [6]. This report suggested that skull involvement might be overlooked in patients with SAPHO syndrome. Furthermore, previously reported cases were complicated by anterior chest wall involvement, and a case limited to the skull has never previously been reported.
Cutibacterium acnes is a Gram-positive, anaerobic bacterium that is a normal component of the flora found in the mucous membranes and skin and is involved in the development of acne [7]. The detection of C. acnes in culture can easily be influenced by the culturing environment and requires a long-term culture of ∼10 days [3]. Although the aetiology of SAPHO syndrome has not been clarified, infections, such as C. acnes, have previously been associated with the aetiology of SAPHO syndrome. Some cases have reported the detection of C. acnes in bone cultures derived from patients with SAPHO syndrome or related diseases [3, 7]. One study reported that SAPHO syndrome bone cultures were positive for C. acnes in 14 out of 21 patients, and antibiotic treatments reduced mean osteitis scores among these patients [8], suggesting the potential usefulness of antimicrobial treatments for patients who are positive for C. acnes. Previous reports of C. acnes-positive SAPHO syndrome bone biopsy cultures have most frequently been associated with cultures from anterior sternum lesions; however, no reports of positive skull bone cultures were identified in the literature.
This is the first case report of SAPHO syndrome with lesions limited to the skull and the detection of C. acnes in a skull bone culture. The detection of C. acnes in the bone biopsy, using appropriate techniques, contributed to the diagnosis of SAPHO syndrome. Moreover, our case suggested that a phenotype of SAPHO syndrome exists in which the lesion is limited to the skull. Therefore, even in the absence of other joint symptoms, skull involvement of SAPHO syndrome should be considered, especially among patients presenting with intractable headaches.
Funding: No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to perform the work described in this article.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1. Chamot AM, Benhamou CL, Kahn MF. et al. Acne-pustulosis-hyperostosis-osteitis syndrome. Results of a national survey. 85 cases. Rev Rhum Mal Osteoartic 1987;54:187–96. [PubMed] [Google Scholar]
- 2. Hayem G, Bouchaud-Chabot A, Benali K. et al. SAPHO syndrome: a long-term follow-up study of 120 cases. Semin Arthritis Rheum 1999;29:159–71. [DOI] [PubMed] [Google Scholar]
- 3. Zimmermann P, Curtis N. The role of Cutibacterium acnes in auto-inflammatory bone disorders. Eur J Pediatr 2019;178:89–95. [DOI] [PubMed] [Google Scholar]
- 4. DiMeco F, Clatterbuck RE, Li KW, McCarthy EF, Olivi A. Synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome presenting as a primary calvarial lesion. Case report and review of the literature. J Neurosurg 2000;93:693–7. [DOI] [PubMed] [Google Scholar]
- 5. Tsugawa J, Ouma S, Fukae J, Tsuboi Y. Recurrent unilateral headache associated with SAPHO syndrome. Intern Med 2014;53:1559–62. [DOI] [PubMed] [Google Scholar]
- 6. Cao Y, Li C, Yang Q. et al. Three patterns of osteoarticular involvement in SAPHO syndrome: a cluster analysis based on whole body bone scintigraphy of 157 patients. Rheumatology 2019;58:1047–55. [DOI] [PubMed] [Google Scholar]
- 7. Colina M, Lo Monaco A, Khodeir M, Trotta F. Propionibacterium acnes and SAPHO syndrome: a case report and literature review. Clin Exp Rheumatol 2007;25:457–60. [PubMed] [Google Scholar]
- 8. Assmann G, Kueck O, Kirchhoff T. et al. Efficacy of antibiotic therapy for SAPHO syndrome is lost after its discontinuation: an interventional study. Arthritis Res Ther 2009;11:R140. [DOI] [PMC free article] [PubMed] [Google Scholar]