INTRODUCTION:
Despite the recent emergence of expensive biologic therapies, hospitalization and surgery remain important contributors for the overall costs of inflammatory bowel disease (IBD). In this study, we aimed to describe the burden of reoperations in patients with IBD by evaluating reoperation rates, charges, and risk factors over 16 years.
METHODS:
We performed a retrospective analysis of all hospital discharges, with focus on reoperations and with a primary diagnosis of IBD, in public hospitals between 2000 and 2015 in mainland Portugal from the Central Administration of the Health System's national registry. We collected data on patient, clinical, and healthcare charges. We used multivariate regressions to estimate the risk factors of IBD-related reoperations.
RESULTS:
We found that 5% of IBD-related hospitalizations were related to reoperations. The number of reoperations per year increased by approximately 200%. However, when corrected by the prevalence of the disease, IBD reoperation rates decreased. Mean IBD-related charges per hospitalization were 7,780 € in 2000 and 10,592 € in 2015, with total charges reaching 6.7 million euros by the end of the study. Risk factors for reoperation include urgent hospitalization, in patients with ulcerative colitis (odds ratio 1.94, 95% confidence interval 1.19–3.17, P = 0.008), and colic disease, in patients with Crohn's disease (odds ratio 1.57, 95% confidence interval 1.06–2.34, P = 0.025).
DISCUSSION:
To obtain an accurate scenario of reoperations among patients with IBD, it is mandatory to adjust the number of reoperations to the prevalence of the disease. Reoperation and its risk factors should be closely monitored to decrease the burden of IBD to the healthcare system.
INTRODUCTION
Inflammatory bowel diseases (IBDs) are a group of idiopathic autoimmune conditions, with unknown etiology, encompassing 2 major forms: Crohn's disease (CD) and ulcerative colitis (UC) (1,2).
The incidence and prevalence of IBD have been increasing since the middle of the twentieth century in all geographic regions. A recent essay on the global burden of IBD anticipates that more than 1 million residents in the United States and 2.5 million in Europe have IBD (3,4). In Portugal, it is estimated that 0.2%–0.3% of the population live with IBD and recent predictions indicate that in 2030, this number will reach 0.3%–0.5% (5).
In this context of increasing prevalence and given its chronic nature and unpredictable disease course, the impact of IBD in healthcare systems is increasing exponentially so that it became a considerable economic and social burden, with costs reaching $6.3 billion and €5 billion, in the United States and Europe, respectively (3,4). Direct healthcare costs, disability (physical and psychological), work absenteeism, and decreased productivity are among the main burdens of IBD in Western countries. This impact may be reduced by assessing and improving the quality of health care—for example, by identifying and analyzing potential sources of costly clinical outcomes.
Despite the recent emergence of expensive biologic therapies, hospitalization and surgery remain important contributors for the overall costs of IBD (6). The numbers and impact of recurrent surgery in patients with IBD are now being explored by several authors, and the reoperations rates vary between 17% and 38% (7–12). In these studies, laparoscopy, side-to-side anastomosis, wide anastomotic stoma, and anti-tumour necrosis factor therapy were associated with a decrease of reoperations, whereas latter introduction of pharmacological therapeutic, duration of the disease, age at diagnosis younger than 17 years, penetrating behavior (B3), no azathioprine use, preoperative smoking, and ileocolic disease were pointed out as risk factors for reoperation.
Despite its importance for the improvement of the quality of health care, there is only one report on the impact of IBD in Portugal (13) and a lack of data on the reoperation trends in Portuguese patients with IBD.
In this context, we have previously determined the national hospitalization rates of patients with IBD, between 2000 and 2015, resorting to an administrative database of all patients subjected to hospital discharge in that period (14). In this present study, we aim to describe the burden of recurrent surgeries to the healthcare system—by exploring the same database for the assessment of reoperation rates and healthcare charges—and to identify the risk factors for reoperation in patients with IBD in mainland Portugal.
METHODS
Data design and data source
Data were retrieved and collected from the national registry of the Central Administration of the Health System (ACSS), which contains administrative data concerning all patients subjected to hospital discharge from hospitals, governed by the National Health Service (NHS) in Portugal. We included all hospital discharges of patients, of all ages, and a primary diagnosis of IBD identified by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes of 555.x (for CD) and 556.x (for UC) between January 1, 2000, and December 27, 2015. The first hospital discharge with a primary diagnosis of IBD and coded for surgery during this study period was considered the index hospital discharge. The unit of observation was the hospital discharge.
Data collection
For each hospital discharge, the following data were collected: year (of the hospital discharge date), hospital name, hospital admission date, hospital discharge date, admission type, age (at the time of hospital discharge), sex, area of residence, primary and secondary diagnoses, and IBD-related medical procedures. Data on disease location/extension, IBD-related surgery, anemia, malnutrition, anxiety, weight loss, wound complications, depression, and previous steroid/immunomodulators use were identified by the ICD-9-CM codes listed in Supplementary Table 1 (see Supplementary Digital Content 2, http://links.lww.com/CTG/A393). The collected data also included the severity of illness and risk of mortality, based on the ACSS's terms of reference, for the contracting of health services in the Portuguese NHS (15) and ranked according to the 3M All Patient Refined-Diagnosis Related Group methodology (APR-DRG, version 21).
Each record within the ACSS national registry contains individual deidentified patient identifiers, such as age, sex, and residence, that enabled researchers to create a unique patient ID and to attribute multiple hospital discharges to the same individual.
Outcomes
Surgical recurrence or reoperation was defined as the necessity of subsequent operation(s) during the observational period.
Other outcome measures included IBD-related number of reoperations, reoperation rate per 100,000 inhabitants, reoperation rate per 100,000 hospitalizations, and reoperation rate per 100,000 patients with IBD. The reoperation rate was calculated by dividing the number of reoperations, during the study period (numerator), by the total number of inhabitants, the total number of hospitalizations, or the total number of patients with IBD (denominators) and multiplying by a factor of 100,000. The total number of inhabitants in mainland Portugal in the analyzed years considered for the computation of the rates was obtained from the National Institute of Statistics (16). The prevalence of IBD in Portugal was estimated based on our previous publication, where prevalence values were forecasted from 2009 to 2030 (5).
Statistical analysis
Continuous variables were summarized by mean and SD, mean and minimum and maximum (min-max), or median and interquartile range (IQR) as applicable. Categorical variables were summarized by absolute (n) and relative (%) frequencies and compared using the χ2 test.
Length of stay (LOS) was defined as the number of days between the hospital admission date and the discharge date for each hospitalization record. Hospital IBD discharge volume was defined as the number of IBD-related hospitalizations per year and categorized according to percentiles: low (≤7 discharges/year), below the 50th percentile; moderate (8–25 discharges/year), between the 50th and 75th percentiles; high (26–71 discharges/year), between the 75th and 95th percentiles; very high (72–139 discharges/year), between the 95th and 99th percentiles; and highest (>139 discharges/year), above the 99th percentile.
We analyzed trends in the total reoperation rates per 100,000 inhabitants or hospitalizations or patients with IBD over the study period. The total reoperation rates per 100,000 inhabitants or hospitalizations were analyzed by year and broken down by the patient's characteristics (sex and age) and disease (IBD, CD, and UC). We estimated the mean (min–max) of the reoperation rates per 100,000 inhabitants or hospitalizations between 2000 and 2015.
In addition, we used joinpoint regression to identify possible inflexion points (up to 2) at which there is a significant change in trends (P value of less than 0.05) using a Monte Carlo permutation method. We analyzed joinpoints using Joinpoint trend analysis software from the Surveillance Research Program of the National Cancer Institute Version 4.2.0.2 (Statistical Research and Applications Branch, National Cancer Institute).
Healthcare costs were estimated according to the Portuguese NHS reimbursements of hospital healthcare charges that are instituted by the national legislation. The cost analysis was derived from the 2009 expenditures tables because these were the latest to contemplate the 3M APR-DRG version 21, which spanned the entire study period. The mean reoperations charges in euros per patient were estimated (€/patient). Total reoperation charges were analyzed in million euros (M€) and broken down by disease (UC and CD).
Because of the particular study design, no control group was established to assess the risk factors for reoperation. Therefore, comparisons were performed between the groups “patients with only 1 surgery” and “patients with more than 1 surgery,” being the former defined as a one-time surgery, with the absence of any subsequent surgeries attributed to the same individual and the latter as multiple surgeries attributed to the same individual.
To identify the risk factors associated with reoperation, a logistic regression model was used for univariate and multivariate analyses of the outcome of interest and other covariates.
Variables in which a P ≤ 0.25 was identified, in the univariate analysis, were included in the final multivariate regression modeling (backward method). The odds ratio (OR) and 95% confidence intervals (CI) were estimated. The computed OR were adjusted for age, sex, LOS, risk of severity, risk of mortality, large intestine resection, anal/rectum surgery, ileostomy, partial/total colectomy, total proctocolectomy, colectomy/proctocolectomy, anemia, wound complications, extraintestinal manifestations, penetrating disease, bowel obstruction, gastrointestinal complications, hospital volume, and fragmented care for the outcomes related with rehospitalizations.
The cumulative probabilities of being reoperated in 5 and 10 years were calculated using the Kaplan–Meier method.
Statistical significance was considered for P < 0.05. Statistical analysis was performed using Statistical Package for the Social Sciences software (version 25.0).
RESULTS
Overall
During the study period, the database registered a total of 48,027 IBD-related hospitalizations in mainland Portugal public hospitals. In our study, we included only 5% of these total hospitalizations, corresponding to 2,214 IBD-related reoperations.
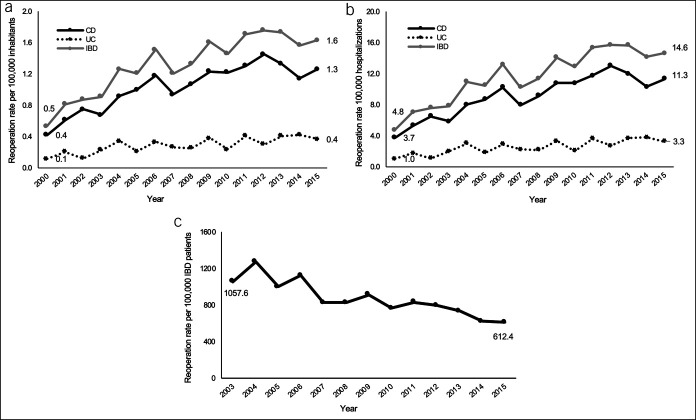
The overall number of reoperations per year increased by approximately 200% from 55 in the year 2000 to 169 in 2015 (Figure 1).
Figure 1.
IBD-related surgical recurrence rate (a) per 100,000 inhabitants, (b) per 100,000 hospitalizations , and (c) per 100,000 patients with IBD. CD, Crohn's disease; IBD, inflammatory bowel disease; UC, ulcerative colitis.
Reoperation per 100,000 inhabitants (Figure 1a) and per 100,000 hospitalizations (Figure 1b) increased from 0.5 to 1.6 and from 4.8 to 14.6, respectively. In addition, joinpoint regression analysis showed one joinpoint in 2005 for IBD reoperation trends per 100,000 inhabitants, indicating 2 significant periods of increasing rates at different paces (see Supplementary Figure 1a, Supplementary Digital Content 1, http://links.lww.com/CTG/A392).
Conversely, the reoperation rate per 100,000 patients with IBD decreased significantly from 1,057.6 to 612.4, between 2003 and 2015 (Figure 1c and Supplementary Figure 1b, Supplementary Digital Content 1, http://links.lww.com/CTG/A392).
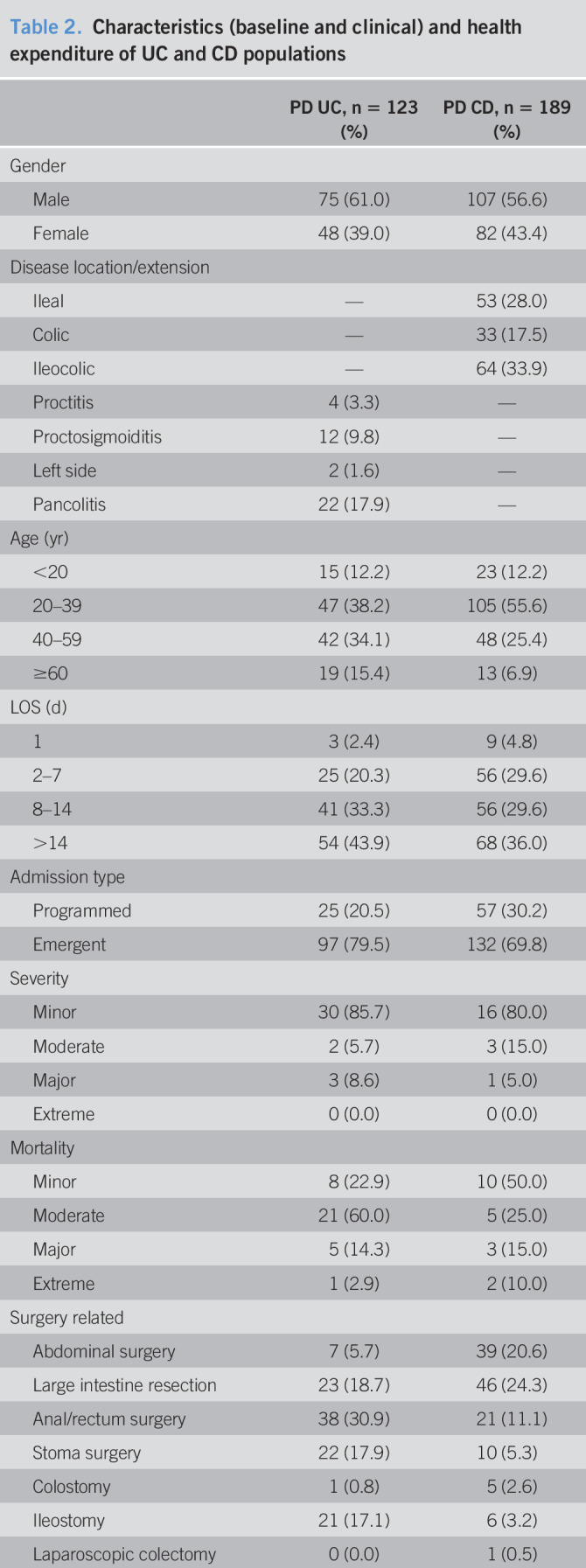
Ulcerative colitis
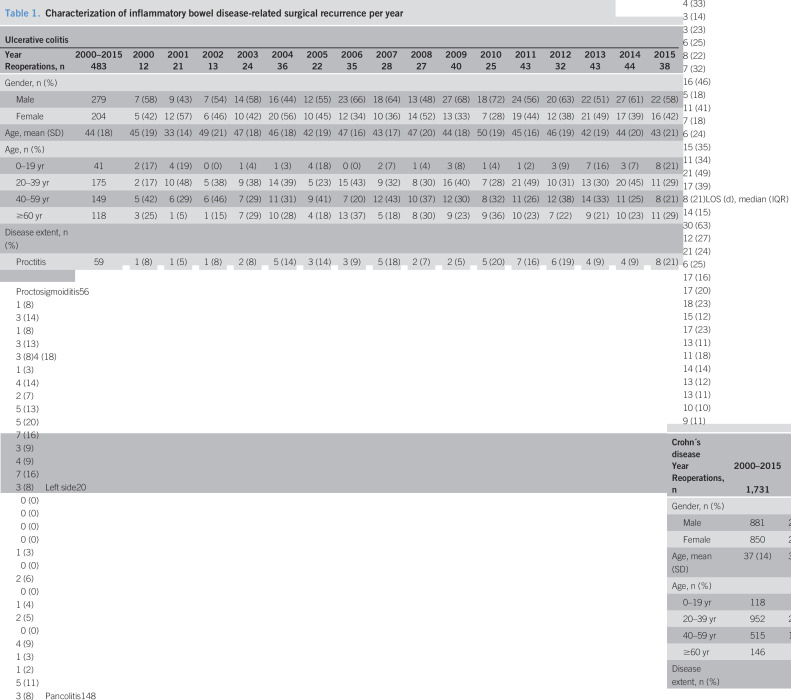
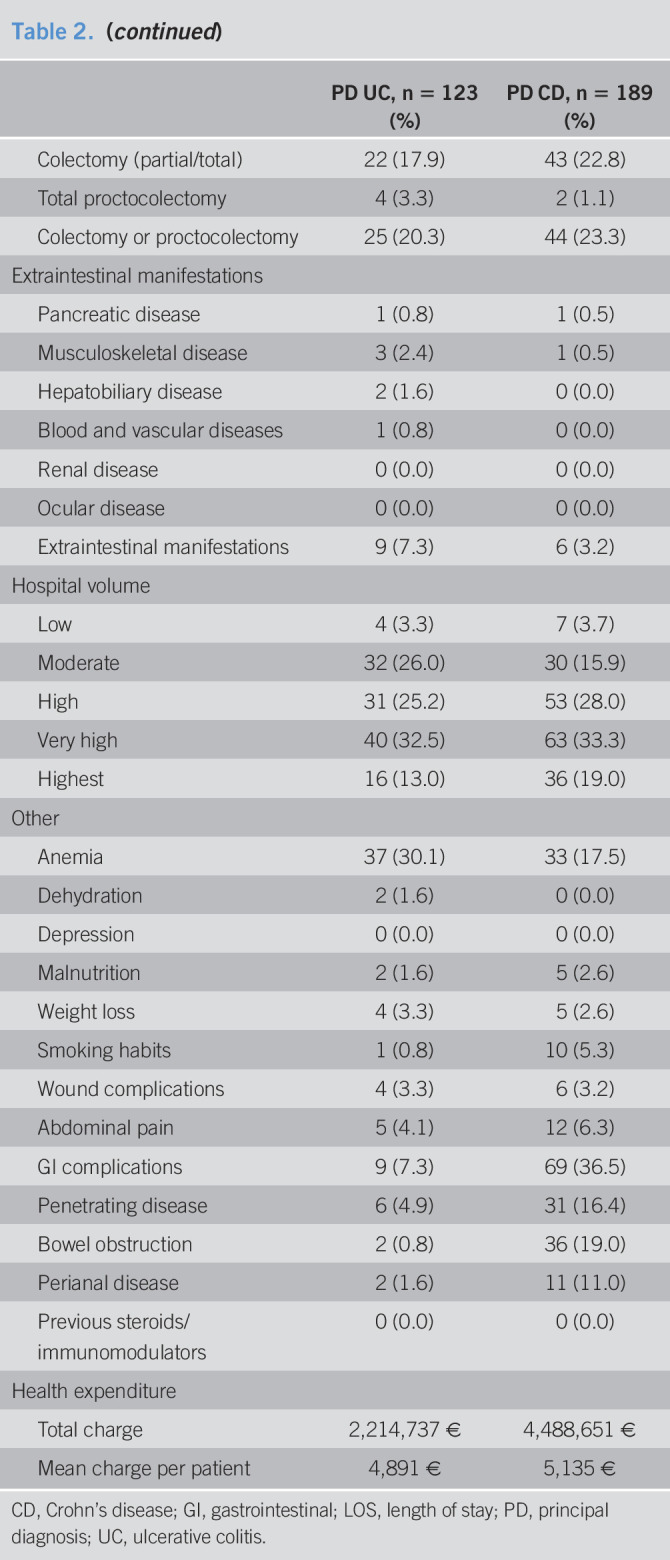
Over the 16-year study period, we found 483 reoperations related to a primary diagnosis of UC in 123 patients (Table 1). The UC extension was found as pancolitis in 22 reoperations (18%), proctosigmoiditis in 12 (10%), proctitis in 4 (3%), and left side in 2 (2%). Most of the UC-related reoperations older than or equal to 20 years old (88%) and male patients (61%), with a median LOS of 14 days (IQR: 15) (Table 2). Total healthcare charges corresponded to approximately 2 M€ and mean charge per patient was 4,891 € (Table 2). The mean charges per hospitalization increased from 4,000 € to 5,390 €, between 2000 and 2015. In the same period of time, the total charges per hospitalization increased from 96,010 € to 123,965 € (Table 3).
Table 1.
Characterization of inflammatory bowel disease-related surgical recurrence per year
| Ulcerative colitis | |||||||||||||||||
| Year | 2000–2015 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
| Reoperations, n | 483 | 12 | 21 | 13 | 24 | 36 | 22 | 35 | 28 | 27 | 40 | 25 | 43 | 32 | 43 | 44 | 38 |
| Gender, n (%) | |||||||||||||||||
| Male | 279 | 7 (58) | 9 (43) | 7 (54) | 14 (58) | 16 (44) | 12 (55) | 23 (66) | 18 (64) | 13 (48) | 27 (68) | 18 (72) | 24 (56) | 20 (63) | 22 (51) | 27 (61) | 22 (58) |
| Female | 204 | 5 (42) | 12 (57) | 6 (46) | 10 (42) | 20 (56) | 10 (45) | 12 (34) | 10 (36) | 14 (52) | 13 (33) | 7 (28) | 19 (44) | 12 (38) | 21 (49) | 17 (39) | 16 (42) |
| Age, mean (SD) | 44 (18) | 45 (19) | 33 (14) | 49 (21) | 47 (18) | 46 (18) | 42 (19) | 47 (16) | 43 (17) | 47 (20) | 44 (18) | 50 (19) | 45 (16) | 46 (19) | 42 (19) | 44 (20) | 43 (21) |
| Age, n (%) | |||||||||||||||||
| 0–19 yr | 41 | 2 (17) | 4 (19) | 0 (0) | 1 (4) | 1 (3) | 4 (18) | 0 (0) | 2 (7) | 1 (4) | 3 (8) | 1 (4) | 1 (2) | 3 (9) | 7 (16) | 3 (7) | 8 (21) |
| 20–39 yr | 175 | 2 (17) | 10 (48) | 5 (38) | 9 (38) | 14 (39) | 5 (23) | 15 (43) | 9 (32) | 8 (30) | 16 (40) | 7 (28) | 21 (49) | 10 (31) | 13 (30) | 20 (45) | 11 (29) |
| 40–59 yr | 149 | 5 (42) | 6 (29) | 6 (46) | 7 (29) | 11 (31) | 9 (41) | 7 (20) | 12 (43) | 10 (37) | 12 (30) | 8 (32) | 11 (26) | 12 (38) | 14 (33) | 11 (25) | 8 (21) |
| ≥60 yr | 118 | 3 (25) | 1 (5) | 1 (15) | 7 (29) | 10 (28) | 4 (18) | 13 (37) | 5 (18) | 8 (30) | 9 (23) | 9 (36) | 10 (23) | 7 (22) | 9 (21) | 10 (23) | 11 (29) |
| Disease extent, n (%) | |||||||||||||||||
| Proctitis | 59 | 1 (8) | 1 (5) | 1 (8) | 2 (8) | 5 (14) | 3 (14) | 3 (9) | 5 (18) | 2 (7) | 2 (5) | 5 (20) | 7 (16) | 6 (19) | 4 (9) | 4 (9) | 8 (21) |
| Proctosigmoiditis | 56 | 1 (8) | 3 (14) | 1 (8) | 3 (13) | 3 (8) | 4 (18) | 1 (3) | 4 (14) | 2 (7) | 5 (13) | 5 (20) | 7 (16) | 3 (9) | 4 (9) | 7 (16) | 3 (8) |
| Left side | 20 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (3) | 0 (0) | 2 (6) | 0 (0) | 1 (4) | 2 (5) | 0 (0) | 4 (9) | 1 (3) | 1 (2) | 5 (11) | 3 (8) |
| Pancolitis | 148 | 4 (33) | 3 (14) | 3 (23) | 6 (25) | 8 (22) | 7 (32) | 16 (46) | 5 (18) | 11 (41) | 7 (18) | 6 (24) | 15 (35) | 11 (34) | 21 (49) | 17 (39) | 8 (21) |
| LOS (d), median (IQR) | 14 (15) | 30 (63) | 12 (27) | 21 (24) | 6 (25) | 17 (16) | 17 (20) | 18 (23) | 15 (12) | 17 (23) | 13 (11) | 11 (18) | 14 (14) | 13 (12) | 13 (11) | 10 (10) | 9 (11) |
| Crohn´s disease | |||||||||||||||||
| Year | 2000–2015 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
| Reoperations, n | 1,731 | 43 | 63 | 78 | 71 | 96 | 105 | 124 | 99 | 113 | 130 | 129 | 138 | 153 | 139 | 119 | 131 |
| Gender, n (%) | |||||||||||||||||
| Male | 881 | 22 (51) | 41 (65) | 38 (49) | 41 (58) | 42 (44) | 54 (51) | 48 (39) | 53 (54) | 53 (47) | 77 (59) | 69 (53) | 74 (54) | 71 (46) | 72 (52) | 64 (54) | 62 (47) |
| Female | 850 | 21 (49) | 22 (35) | 40 (51) | 30 (42) | 54 (56) | 51 (49) | 76 (61) | 46 (46) | 60 (53) | 53 (41) | 60 (47) | 64 (46) | 82 (54) | 67 (48) | 55 (46) | 69 (53) |
| Age, mean (SD) | 37 (14) | 35 (12) | 36 (16) | 38 (15) | 34 (14) | 37 (15) | 35 (14) | 36 (12) | 37 (14) | 36 (14) | 38 (15) | 38 (15) | 38 (13) | 40 (14) | 38 (14) | 37 (15) | 39 (14) |
| Age, n (%) | |||||||||||||||||
| 0–19 yr | 118 | 4 (9) | 6 (10) | 7 (9) | 3 (4) | 6 (6) | 11 (10) | 7 (6) | 7 (7) | 5 (4) | 6 (5) | 9 (7) | 10 (7) | 9 (6) | 6 (4) | 9 (8) | 13 (10) |
| 20–39 yr | 952 | 24 (56) | 38 (60) | 38 (49) | 53 (75) | 53 (55) | 64 (61) | 73 (59) | 55 (56) | 68 (60) | 71 (55) | 69 (53) | 65 (47) | 73 (48) | 79 (57) | 67 (56) | 62 (47) |
| 40–59 yr | 515 | 13 (30) | 12 (19) | 24 (31) | 10 (14) | 29 (30) | 23 (22) | 37 (30) | 31 (31) | 31 (27) | 40 (31) | 37 (29) | 54 (39) | 54 (35) | 44 (32) | 33 (28) | 43 (33) |
| ≥60 yr | 146 | 2 (5) | 7 (11) | 9 (12) | 5 (7) | 8 (8) | 7 (7) | 7 (6) | 6 (6) | 9 (8) | 13 (10) | 14 (11) | 9 (7) | 17 (11) | 10 (7) | 10 (8) | 13 (10) |
| Disease extent, n (%) | |||||||||||||||||
| Ileal | 531 | 12 (28) | 10 (16) | 27 (35) | 19 (27) | 36 (38) | 29 (28) | 38 (31) | 31 (31) | 31 (27) | 43 (33) | 37 (29) | 48 (35) | 53 (35) | 44 (32) | 39 (33) | 34 (26) |
| Colonic | 207 | 4 (9) | 9 (14) | 10 (13) | 11 (15) | 15 (16) | 7 (7) | 18 (15) | 11 (11) | 11 (10) | 22 (17) | 16 (12) | 14 (10) | 11 (7) | 17 (12) | 12 (10) | 19 (15) |
| Ileocolonic | 804 | 20 (47) | 34 (54) | 29 (37) | 27 (38) | 38 (40) | 64 (61) | 64 (52) | 46 (46) | 57 (50) | 57 (44) | 65 (50) | 63 (46) | 69 (45) | 65 (47) | 47 (39) | 59 (45) |
| LOS (d), median (IQR) | 11 (14) | 15 (13) | 15 (14) | 14 (18) | 12 (16) | 12 (15) | 11 (12) | 11 (12) | 14 (19) | 13 (17) | 9 (15) | 11 (15) | 10 (10) | 9 (11) | 9 (13) | 10 (13) | 9 (12) |
IQR, interquartile range; LOS, length of stay.
Table 2.
Characteristics (baseline and clinical) and health expenditure of UC and CD populations
| PD UC, n = 123 (%) | PD CD, n = 189 (%) | |
| Gender | ||
| Male | 75 (61.0) | 107 (56.6) |
| Female | 48 (39.0) | 82 (43.4) |
| Disease location/extension | ||
| Ileal | — | 53 (28.0) |
| Colic | — | 33 (17.5) |
| Ileocolic | — | 64 (33.9) |
| Proctitis | 4 (3.3) | — |
| Proctosigmoiditis | 12 (9.8) | — |
| Left side | 2 (1.6) | — |
| Pancolitis | 22 (17.9) | — |
| Age (yr) | ||
| <20 | 15 (12.2) | 23 (12.2) |
| 20–39 | 47 (38.2) | 105 (55.6) |
| 40–59 | 42 (34.1) | 48 (25.4) |
| ≥60 | 19 (15.4) | 13 (6.9) |
| LOS (d) | ||
| 1 | 3 (2.4) | 9 (4.8) |
| 2–7 | 25 (20.3) | 56 (29.6) |
| 8–14 | 41 (33.3) | 56 (29.6) |
| >14 | 54 (43.9) | 68 (36.0) |
| Admission type | ||
| Programmed | 25 (20.5) | 57 (30.2) |
| Emergent | 97 (79.5) | 132 (69.8) |
| Severity | ||
| Minor | 30 (85.7) | 16 (80.0) |
| Moderate | 2 (5.7) | 3 (15.0) |
| Major | 3 (8.6) | 1 (5.0) |
| Extreme | 0 (0.0) | 0 (0.0) |
| Mortality | ||
| Minor | 8 (22.9) | 10 (50.0) |
| Moderate | 21 (60.0) | 5 (25.0) |
| Major | 5 (14.3) | 3 (15.0) |
| Extreme | 1 (2.9) | 2 (10.0) |
| Surgery related | ||
| Abdominal surgery | 7 (5.7) | 39 (20.6) |
| Large intestine resection | 23 (18.7) | 46 (24.3) |
| Anal/rectum surgery | 38 (30.9) | 21 (11.1) |
| Stoma surgery | 22 (17.9) | 10 (5.3) |
| Colostomy | 1 (0.8) | 5 (2.6) |
| Ileostomy | 21 (17.1) | 6 (3.2) |
| Laparoscopic colectomy | 0 (0.0) | 1 (0.5) |
| Colectomy (partial/total) | 22 (17.9) | 43 (22.8) |
| Total proctocolectomy | 4 (3.3) | 2 (1.1) |
| Colectomy or proctocolectomy | 25 (20.3) | 44 (23.3) |
| Extraintestinal manifestations | ||
| Pancreatic disease | 1 (0.8) | 1 (0.5) |
| Musculoskeletal disease | 3 (2.4) | 1 (0.5) |
| Hepatobiliary disease | 2 (1.6) | 0 (0.0) |
| Blood and vascular diseases | 1 (0.8) | 0 (0.0) |
| Renal disease | 0 (0.0) | 0 (0.0) |
| Ocular disease | 0 (0.0) | 0 (0.0) |
| Extraintestinal manifestations | 9 (7.3) | 6 (3.2) |
| Hospital volume | ||
| Low | 4 (3.3) | 7 (3.7) |
| Moderate | 32 (26.0) | 30 (15.9) |
| High | 31 (25.2) | 53 (28.0) |
| Very high | 40 (32.5) | 63 (33.3) |
| Highest | 16 (13.0) | 36 (19.0) |
| Other | ||
| Anemia | 37 (30.1) | 33 (17.5) |
| Dehydration | 2 (1.6) | 0 (0.0) |
| Depression | 0 (0.0) | 0 (0.0) |
| Malnutrition | 2 (1.6) | 5 (2.6) |
| Weight loss | 4 (3.3) | 5 (2.6) |
| Smoking habits | 1 (0.8) | 10 (5.3) |
| Wound complications | 4 (3.3) | 6 (3.2) |
| Abdominal pain | 5 (4.1) | 12 (6.3) |
| GI complications | 9 (7.3) | 69 (36.5) |
| Penetrating disease | 6 (4.9) | 31 (16.4) |
| Bowel obstruction | 2 (0.8) | 36 (19.0) |
| Perianal disease | 2 (1.6) | 11 (11.0) |
| Previous steroids/immunomodulators | 0 (0.0) | 0 (0.0) |
| Health expenditure | ||
| Total charge | 2,214,737 € | 4,488,651 € |
| Mean charge per patient | 4,891 € | 5,135 € |
CD, Crohn's disease; GI, gastrointestinal; LOS, length of stay; PD, principal diagnosis; UC, ulcerative colitis.
Table 3.
Mean charges per hospitalization and total charges per year
| Year | Mean charge per hospitalization | Total charge per year | ||
| UC | CD | UC | CD | |
| 2000 | 4,000 € | 3,780 € | 96,010 € | 154,994 € |
| 2001 | 4,454 € | 4,618 € | 155,898 € | 314,032 € |
| 2002 | 3,400 € | 4,594 € | 102,014 € | 284,823 € |
| 2003 | 4,300 € | 4,466 € | 141,900 € | 276,861 € |
| 2004 | 4,635 € | 5,185 € | 139,055 € | 316,300 € |
| 2005 | 4,287 € | 4,717 € | 128,623 € | 311,351 € |
| 2006 | 5,125 € | 4,238 € | 148,623 € | 271,258 € |
| 2007 | 4,759 € | 4,266 € | 166,554 € | 277,264 € |
| 2008 | 3,918 € | 4,151 € | 121,443 € | 348,664 € |
| 2009 | 5,172 € | 4,565 € | 181,012 € | 328,653 € |
| 2010 | 3,613 € | 4,459 € | 83,106 € | 298,727 € |
| 2011 | 5,175 € | 4,612 € | 181,141 € | 304,401 € |
| 2012 | 4,756 € | 4,473 € | 171,225 € | 304,162 € |
| 2013 | 4,663 € | 4,879 € | 177,175 € | 239,066 € |
| 2014 | 4,048 € | 6,207 € | 97,146 € | 180,010 € |
| 2015 | 5,390 € | 5,202 € | 123,965 € | 208,075 € |
CD, Crohn's disease; UC, ulcerative colitis.
We noticed an increase in the absolute number of UC-related reoperations from the year 2000–2015. Accordingly, as shown in Figure 1, the UC-related reoperations rates per 100,000 inhabitants increased significantly from 0.1 to 0.4 (Figure 1a and Supplementary Figure 1c, Supplementary Digital Content 1, http://links.lww.com/CTG/A392) and per 100,000 hospitalizations increased from 1.0 to 3.3 (Figure 1b). In the analysis by sex and age, the reoperation rates per 100,000 inhabitants evidenced a small increase (see Supplementary Table 2, Supplementary Digital Content 2, http://links.lww.com/CTG/A393).
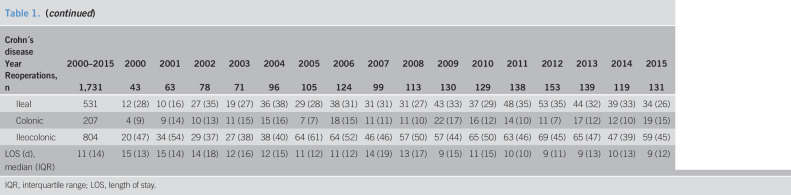
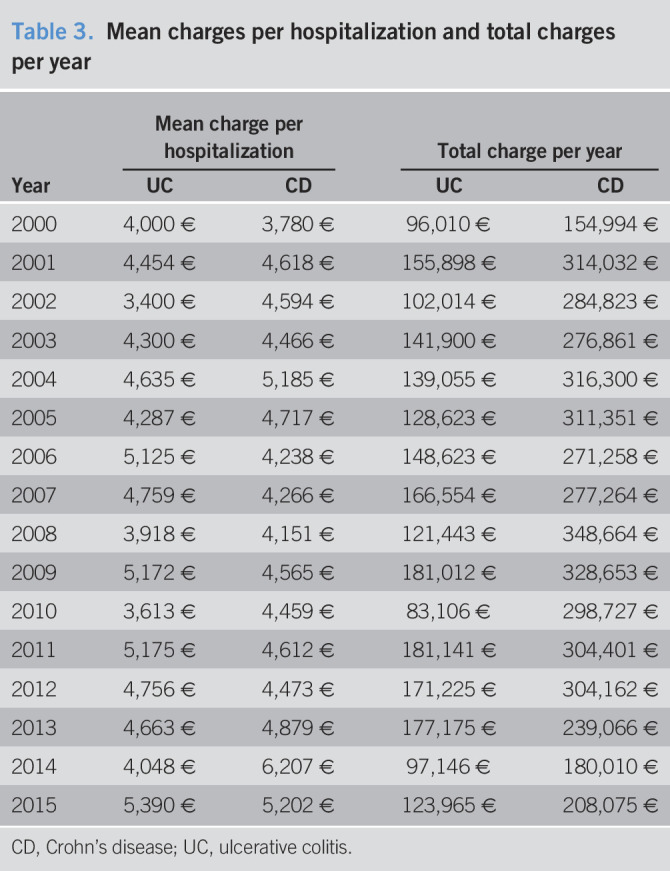
Regarding risk factors associated with reoperation in patients with UC, the results of the univariate analysis are summarized in Supplementary Table 3 (see Supplementary Digital Content 2, http://links.lww.com/CTG/A393). In the multivariate regression, urgent hospitalization was significantly associated with increased odds of reoperation (OR: 1.94; 95% CI: 1.19–3.17) (Table 4).
Table 4.
Multivariate analysis of risk factors associated with surgical recurrence in patients with ulcerative colitis
| Patients with 1 surgery (n = 775)a | Patients with more than 1 surgery (n = 123)b | ORc | 95% CI | P Value | ||
| Disease extension | ||||||
| Left side | 48 (6.2) | 2 (1.6) | 0.29 | 0.07 | 1.22 | 0.090 |
| Age (yr) | ||||||
| <20 | 75 (9.7) | 15 (12.2) | Ref | |||
| 20–39 | 254 (32.8) | 47 (38.2) | 0.82 | 0.43 | 1.58 | 0.555 |
| 40–59 | 225 (29.0) | 42 (34.1) | 0.91 | 0.46 | 1.77 | 0.777 |
| ≥60 | 221 (28.5) | 19 (15.4) | 0.38 | 0.18 | 0.80 | 0.011 |
| Admission type | ||||||
| Programmed | 241 (31.1) | 25 (20.5) | Ref | |||
| Emergent | 534 (68.9) | 97 (79.5) | 1.94 | 1.19 | 3.17 | 0.008 |
| Surgery related variables | ||||||
| Abdominal surgery | 88 (11.4) | 7 (5.7) | 0.49 | 0.21 | 1.12 | 0.093 |
| Anal/rectum surgery | 377 (48.6) | 38 (30.9) | 0.42 | 0.27 | 0.64 | <0.001 |
| Colostomy | 27 (3.5) | 1 (0.8) | 0.17 | 0.02 | 1.29 | 0.087 |
CI, confidence interval; OR, odds ratio.
Significant OR in boldface.
Refers to one-time surgery with the absence of any subsequent surgery attributed to the same individual.
Refers to patients with more than one surgery.
For each OR, analyzed as dichotomous variables with 2 categories: presence vs absence (absence as a reference category).
The factors significantly associated with decreased odds of reoperation included old age (OR: 0.38; 95% CI: 0.18–0.80) and anal/rectum surgery performed in the first surgery (OR: 0.42; 95% CI: 0.27–0.64) (Table 4).
Crohn's disease
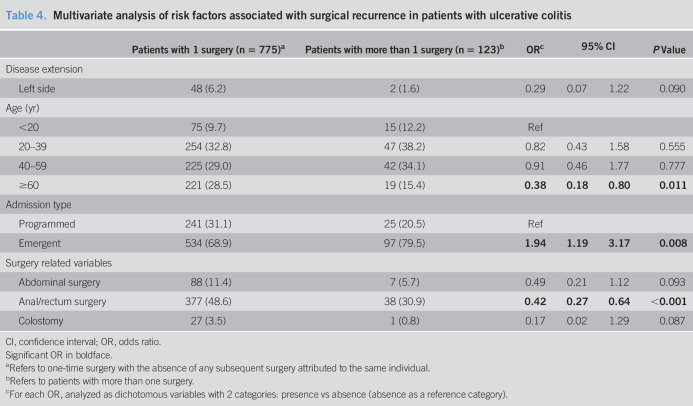
Over the 16-year study period, we registered 1,731 reoperations related to a primary diagnosis of CD from 189 unique patients (Table 1). The CD location was ileocolic in 64 reoperations (34%), ileal in 53 (28%), and colic in 33 (17.5%). Most of the CD-related reoperations comprised young adults (20–39 years, 56%) and male patients (57%), with a median LOS of 11 days (IQR: 14) (Table 2). Total healthcare charges corresponded to approximately 4.5 M€, and the mean charge per patient was 5,135 € (Table 2). The mean charges per hospitalization increased from 3,780 € to 5,202 €, between 2000 and 2015. In the same period of time, the total charges per hospitalization increased from 154,994 € to 208,075 € (Table 3).
The absolute number of CD-related reoperations increased from 43 in 2000 to 131 in 2015 (Table 2). Accordingly, as shown in Figure 1, between 2000 and 2015, the CD-related reoperation rate per 100,000 inhabitants increased from 0.4 to 1.3 (Figure 1a) and per 100,000 hospitalizations increased from 3.7 to 11.3 (Figure 1b).
Similar increases were also observed when the reoperation rates per 100,000 inhabitants were analyzed by sex and age (see Supplementary Table 2, Supplementary Digital Content 2, http://links.lww.com/CTG/A393).
In addition, joinpoint regression analysis showed one joinpoint in 2012 for CD reoperation trends per 100,000 inhabitants, with a significant increase in the first period (see Supplementary Figure 1d, Supplementary Digital Content 1, http://links.lww.com/CTG/A392).
The overall cumulative 5- and 10-year reoperation rates were 29.4% and 43.9%, respectively (see Supplementary Figure 2, Supplementary Digital Content 1, http://links.lww.com/CTG/A392).
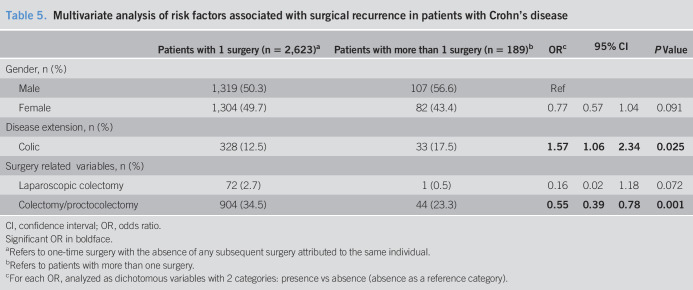
Regarding the risk factors associated with reoperation in patients with CD, the univariate analysis revealed crude OR for reoperation (data not shown, see Supplementary Table 4, Supplementary Digital Content 2, http://links.lww.com/CTG/A393). In multivariate regression, the only factor significantly associated with increased odds of reoperation was colic disease (OR: 1.57; 95% CI: 1.06–2.34) (Table 5). The factors significantly associated with decreased odds of reoperation were colectomy or proctocolectomy performed in the first surgery (OR: 0.55; 95% CI: 0.39–0.78) (Table 5).
Table 5.
Multivariate analysis of risk factors associated with surgical recurrence in patients with Crohn's disease
| Patients with 1 surgery (n = 2,623)a | Patients with more than 1 surgery (n = 189)b | ORc | 95% CI | P Value | ||
| Gender, n (%) | ||||||
| Male | 1,319 (50.3) | 107 (56.6) | Ref | |||
| Female | 1,304 (49.7) | 82 (43.4) | 0.77 | 0.57 | 1.04 | 0.091 |
| Disease extension, n (%) | ||||||
| Colic | 328 (12.5) | 33 (17.5) | 1.57 | 1.06 | 2.34 | 0.025 |
| Surgery related variables, n (%) | ||||||
| Laparoscopic colectomy | 72 (2.7) | 1 (0.5) | 0.16 | 0.02 | 1.18 | 0.072 |
| Colectomy/proctocolectomy | 904 (34.5) | 44 (23.3) | 0.55 | 0.39 | 0.78 | 0.001 |
CI, confidence interval; OR, odds ratio.
Significant OR in boldface.
Refers to one-time surgery with the absence of any subsequent surgery attributed to the same individual.
Refers to patients with more than one surgery.
For each OR, analyzed as dichotomous variables with 2 categories: presence vs absence (absence as a reference category).
DISCUSSION
This study aims to evaluate the reoperation rates—and respective costs and risk factors—in patients with IBD, based on a retrospective analysis of a nationwide database of all hospitalizations, from public hospitals in mainland Portugal. Although, several authors have already explored the trends in reoperation rates in patients with IBD worldwide (7,9,17–20), this is, to our best knowledge, the first project exploring the reoperation rates and the associated risk factors and costs in patients with IBD in Portugal.
We found that 5% of the IBD-related hospitalizations corresponded to IBD-related reoperations (CD: 78%; UC: 22%) that increased by 200% from 2000 to 2015 (Table 1), resulting in an increase of the rates per 100,000 inhabitants and per 100,000 hospitalizations in both patients with UC and CD (see Supplementary Table 2, Supplementary Digital Content 2, http://links.lww.com/CTG/A393). This is probably related with the increasing prevalence of IBD in Portugal that, ultimately, conducts to an increase in the absolute numbers of surgeries and recurrent surgeries (5). In addition, we found inflexion points in the years 2005 and 2012 in IBD and CD reoperation rates per 100,000 inhabitants, respectively (see Supplementary Figures 1a and 1d, Supplementary Digital Content 1, http://links.lww.com/CTG/A392). These results may be explained by the approval of novel biologic therapeutic approaches since the year 2000 in Portugal that allegedly reduced the risk of hospitalization, surgery, and recurrent surgery among patients with IBD (22).
However, we observed a 1.7-fold decrease in the reoperation rate by adjusting the reoperation numbers for the forecasted population of patients with IBD (Figure 1c and Supplementary Figure 1b, Supplementary Digital Content 1, http://links.lww.com/CTG/A392). This decrease of adjusted reoperation rates among patients with IBD that has also been evidenced recently by other authors in distinct geographic zones (4,5,7,17,18,21) might be explained by a combination of 2 factors: (i) the increasing prevalence of IBD in Portugal (and globally) (3,5) and (ii) the approval of novel biologic treatments (22). These results evidence that the analysis of reoperation rates can only be conclusive and realistic when performed in a broad perspective considering total population, hospitalizations, and disease prevalence.
Furthermore, we found that the cumulative 5- and 10-year reoperation rates were 29.4% and 43.9%, respectively. These results are in line with those found in the literature for CD (7–9,18,21). We did not analyze the cumulative reoperation rate for patients with UC because we were not able to consider multistage procedures and thus overestimating the cumulative reoperation rate.
Regarding health expenditure of reoperated patients, our study evidenced that the mean charges per hospitalization and the total charges per year increased about 35% and 31%, respectively, between 2000 and 2015. The total charges per year reached 332,040 € in 2015, with CD being responsible for 63% of the expenses (Table 3). However, this increasing tendency was not constant and showed several fluctuations, between 2000 and 2015, hindering the establishment of a direct causal association between the number of reoperations (registered each year) and costs. This can be related to the wide range of costs of the reoperations—registered in the database—that, depending on the technical complexity, can vary significantly resulting in total charges that are not proportional to the total number of reoperations in each year.
Although it is undeniable that the cost profile of patients with IBD is changing because of the recent advances in biologic therapies, several studies evidence that hospitalization and surgery remain important contributors to direct costs in IBD (3,4,6).
Our study also aimed to identify the risk factors for reoperation, for both patients with CD and UC. Regarding UC, our data revealed that, among the evaluated factors, urgent hospitalization is the only risk factor for reoperation (Table 4). This is possibly because of emergency surgeries, such as colectomies, performed as consequence of emergency hospitalizations (17). In fact, there is a described tendency for the decrease of colectomy at first instance, among patients with IBD, probably because of the use of biologics but that possibility cannot be excluded in cases of severe complications. Distinctly, old age (≥60 years) and anal/rectum surgery (performed in the first surgery) were identified as factors decreasing the odds of reoperation in good agreement with clinical and literature data (Table 4). Age is generally considered an important risk factor for postoperative morbidity and mortality that leads to a decrease in the number of emergency surgeries in elderly patients (23,24). Regarding previous anal/rectum surgery, our results can be related to the fact that, in this kind of procedure, there is no rectum remaining and only rarely the patients need additional surgery (25).
What concerns to CD is that colic disease was the only risk factor for reoperation (Table 5), as also evidenced in previous studies that identified disease location and extension as risk factors for surgical recurrence in patients with CD (7,26). Colectomy or proctocolectomy performed in the first surgery was found to be protective against reoperation in patients with CD which is in accordance with the prognosis of the patients submitted to this kind of procedure.
The key strengths of this study are the utilization of an administrative database with national coverage, ensuring the representativeness of the data to a nationwide scale and the novelty of this study in mainland Portugal.
The study had, however, some limitations. First, as already stated, we were not able to take into account multistage procedures. Second, the retrospective and registry-based design might have led to data misclassification by inaccurate coding and validation and to eventual underreporting. For example, disease extent is not mandatory, thus frequencies in the columns may not sum up to 100% because of missing data. Third, our data set lacks patients with CD with a classification of upper disease because ICD-9-CM does not use this classification. Nevertheless, several studies have already validated the suitability of the ICD-9-CM coding system in the IBD context (27–29). Fourth, unfortunately and unlike the ICD-10-CM classification, ICD-9-CM does not allow the codification of biological treatment, and therefore, we could not possibly consider this factor in our analysis. Furthermore, only public hospitals were included in this study, therefore private hospitalizations were not considered. Finally, we only used the 2009 expenditure tables with the 3M APR-DRGversion 21 that may underappreciate any price fluctuations regarding IBD-related charges that occurred subsequently. Any DRG changes were also not considered.
In conclusion, reoperation should be closely monitored and an effort on reducing or controlling the identified risk factors should be performed to improve not only the quality of life of patients but also the quality of care, with consequent reduction of the burden of IBD to the healthcare system.
CONFLICTS OF INTEREST
Guarantor of the article: Fernando Magro, MD, PhD.
Specific author contributions: M.S. was involved in data analysis, interpretation of data, and writing the manuscript. C.C.D. was involved in conception and design of the study, data analysis, interpretation of data, and revising the manuscript. F.M. was involved in the conception and design of the study, interpretation of data, and revising the manuscript. All authors reviewed and approved the final manuscript.
Financial support: This work was supported by “Fundação para a Ciência e Tecnologia,” Portugal (grant number PD/BD/142890/2018 to M.S.) and GEDII (Portugal IBD Study Group).
Potential competing interests:F.M. received fees, for presenting, from: AbbVie, Ferring, Falk, Hospira, PharmaKern, MSD, Schering, Lab. Vitoria, Vifor, and OmPharma. All other authors have nothing to declare.
Study Highlights.
WHAT IS KNOWN
✓ In the context of increasing prevalence and given its chronic nature and unpredictable disease course, the impact of IBD in healthcare systems is increasing exponentially so that it became a considerable economic and social burden.
✓ The numbers and impact of recurrent surgery, in IBD patients, are now being explored by several authors and the reoperations rates vary between 17% and 38%.
WHAT IS NEW HERE
✓ This is the first study of its kind conducted in a Southern-European country.
✓ IBD patients seem to be submitted to less reoperations since we observed a 1.7-fold decrease in the reoperation rate, by adjusting the reoperation numbers for the forecasted population of IBD patients.
✓ IBD-related reoperation charges reached 6.7 M€ during the study period.
✓ Risk factors for reoperation include urgent hospitalization, in patients with UC, and colic disease in patients with Crohn's disease.
TRANSLATIONAL IMPACT
✓ To obtain an accurate scenario of reoperations among IBD patients, it is mandatory to adjust the number of reoperations to the prevalence of the disease. Reoperation and its risk factors should be closely monitored in order to decrease the burden of IBD to the healthcare system.
Supplementary Material
ACKNOWLEDGEMENTS
The authors thank the Portuguese Ministry of Health's Central Administration for the Health System (ACSS) for providing access to the data set and the Center for Health Technology and Services Research (CINTESIS) for providing the conditions to perform this study. The authors thank Paula Pinto, PharmD, PhD (PMA–Pharmaceutical Medicine Academy), for providing medical writing and editorial assistance.
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at http://links.lww.com/CTG/A392 and http://links.lww.com/CTG/A393
REFERENCES
- 1.Seyedian SS, Nokhostin F, Malamir MD. A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease. J Med Life 2019;12(2):113–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loftus EV. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology 2004;126(6):1504–17. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan GG. The global burden of IBD: From 2015 to 2025. Nat Rev Gastroenterol Hepatol 2015;12(12):720–7. [DOI] [PubMed] [Google Scholar]
- 4.Burisch J, Jess T, Martinato M, et al. The burden of inflammatory bowel disease in Europe. J Crohns Colitis 2013;7(4):322–37. [DOI] [PubMed] [Google Scholar]
- 5.Santiago M, Magro F, Correia L, et al. What forecasting the prevalence of inflammatory bowel disease may tell us about its evolution on a national scale. Therap Adv Gastroenterol 2019;12:1756284819860044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamat N, Ganesh Pai C, Surulivel Rajan M, et al. Cost of illness in inflammatory bowel disease. Dig Dis Sci 2017;62(9):2318–26. [DOI] [PubMed] [Google Scholar]
- 7.Frolkis AD, Lipton DS, Fiest KM, et al. Cumulative incidence of second intestinal resection in Crohn's disease: A systematic review and meta-analysis of population-based studies. Am J Gastroenterol 2014;109(11):1739–48. [DOI] [PubMed] [Google Scholar]
- 8.Lee SM, Han EC, Ryoo SB, et al. Long-term outcomes and risk factors for reoperation after surgical treatment for gastrointestinal Crohn disease according to anti-tumor necrosis factor-α antibody use: 35 years of experience at a single institute in Korea. Ann Coloproctol 2015;31(4):144–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vester-Andersen MK, Vind I, Prosberg MV, et al. Hospitalisation, surgical and medical recurrence rates in inflammatory bowel disease 2003-2011—A Danish population-based cohort study. J Crohns Colitis 2014;8(12):1675–83. [DOI] [PubMed] [Google Scholar]
- 10.Dias CC, Pereira Rodrigues P, Fernandes S, et al. The risk of disabling, surgery and reoperation in Crohn's disease—A decision tree-based approach to prognosis. PLoS One 2017;12(2):e0172165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scaringi S, Di Bella A, Boni L, et al. New perspectives on the long-term outcome of segmental colectomy for Crohn's colitis: An observational study on 200 patients. Int J Colorectal Dis 2018;33(4):479–85. [DOI] [PubMed] [Google Scholar]
- 12.Zhou J, Li Y, Gong J, et al. Frequency and risk factors of surgical recurrence of Crohn's disease after primary bowel resection. Turk J Gastroenterol 2018;29(6):655–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pinho I, Santos JV, Dinis-Ribeiro M, et al. Burden of digestive diseases in Portugal: Trends in hospitalizations between 2000 and 2010. Eur J Gastroenterol Hepatol 2015;27(3):279–89. [DOI] [PubMed] [Google Scholar]
- 14.Dias CC, Santiago M, Correia L, et al. Hospitalization trends of the inflammatory bowel disease landscape: A nationwide overview of 16 years. Dig Liver Dis 2019;51(7):952–60. [DOI] [PubMed] [Google Scholar]
- 15.Central Administration of the Health System. Terms of reference for the contracting of health care in the Portuguese SNS (National Health Service) for 2017. 2017. [Google Scholar]
- 16.INE. Instituto Nacional de Estatística. (https://www.ine.pt/xportal/xmain?xpgid=ine_main&xpid=INE&xlang=pt). Accessed December 9, 2019.
- 17.Candido FD, Fiorino G, Spadaccini M, et al. Are surgical rates decreasing in the biological era in IBD? Curr Drug Targets 2019;20(13):1356–62. [DOI] [PubMed] [Google Scholar]
- 18.Burr NE, Lord R, Hull MA, et al. Decreasing risk of first and subsequent surgeries in patients with Crohn's disease in England from 1994 through 2013. Clin Gastroenterol Hepatol 2019;17(10):2042–9. [DOI] [PubMed] [Google Scholar]
- 19.Ananthakrishnan AN, McGinley EL, Binion DG, et al. A nationwide analysis of changes in severity and outcomes of inflammatory bowel disease hospitalizations. J Gastrointest Surg 2011;15(2):267–76. [DOI] [PubMed] [Google Scholar]
- 20.Olivera P, Spinelli A, Gower-Rousseau C, et al. Surgical rates in the era of biological therapy: Up, down or unchanged? Curr Opin Gastroenterol 2017;33(4):246–53. [DOI] [PubMed] [Google Scholar]
- 21.Shinagawa T, Hata K, Ikeuchi H, et al. Rate of reoperation decreased significantly after year 2002 in patients with Crohn's disease. Clin Gastroenterol Hepatol 2020;18(4):898–907.e5. [DOI] [PubMed] [Google Scholar]
- 22.Costa J, Magro F, Caldeira D, et al. Infliximab reduces hospitalizations and surgery interventions in patients with inflammatory bowel disease: A systematic review and meta-analysis. Inflamm Bowel Dis 2013;19(10):2098–110. [DOI] [PubMed] [Google Scholar]
- 23.Louis DJ, Hsu A, Brand MI, et al. Morbidity and mortality in octogenarians and older undergoing major intestinal surgery. Dis Colon Rectum 2009;52(1):59–63. [DOI] [PubMed] [Google Scholar]
- 24.Turrentine FE, Wang H, Simpson VB, et al. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg 2006;203(6):865–77. [DOI] [PubMed] [Google Scholar]
- 25.Kunitake H, Poylin V. Complications following anorectal surgery. Clin Colon Rectal Surg 2016;29(1):14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nguyen V, Kanth R, Gazo J, et al. Management of post-operative Crohn's disease in 2017: Where do we go from here? Expert Rev Gastroenterol Hepatol 2016;10(11):1257–69. [DOI] [PubMed] [Google Scholar]
- 27.Thirumurthi S, Chowdhury R, Richardson P, et al. Validation of ICD-9-CM diagnostic codes for inflammatory bowel disease among veterans. Dig Dis Sci 2010;55(9):2592–8. [DOI] [PubMed] [Google Scholar]
- 28.Rezaie A, Quan H, Fedorak RN, et al. Development and validation of an administrative case definition for inflammatory bowel diseases. Can J Gastroenterol 2012;26(10):711–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shiff NJ, Jama S, Boden C, et al. Validation of administrative health data for the pediatric population: A scoping review. BMC Health Serv Res 2014;14:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.