Abstract
Background
Schistosomiasis, globally, is significant public as well as veterinary health problem as it is associated with a wide range of clinical conditions in humans and animals. Schistosomiasis is mostly caused by the following species of genus Schistosoma: Schistosoma japonicum, Schistosoma haematobium, Schistosoma mekongi, Schistosoma intercalatum Schistosoma guineensis, Schistosoma malayensis and Schistosoma mansoni. S. japonicum might be considered as the most pathogenic among these species as the clinical disease caused by this parasite ranges from mild diarrhea, nausea, Katayama fever, portal hypertension, splenomegaly and ascites to liver cirrhosis and fibrosis. S. japonicum has been commonly encountered in China, the Philippines and Indonesia. According to WHO, at least 220.8 million people required preventive treatment for schistosomiasis in 2017 but only 102.3 million people were reported to have been treated. To our knowledge, there are no cases reported from Nepal. Hence, this is the first reported case of S. japonicum in Nepal.
Case presentation
A case of acute schistosomiasis due to S. japonicum was identified in CIWEC Hospital and Travel Medicine Center, Kathmandu, Nepal. The patient arrived with gastrointestinal symptoms without any pre-existing chronic illness with no evidence of travel outside of Spain since last August, but had travelled to many other countries 2 years ago. Timely diagnosis by stool routine and microscopic examination and formal-ether concentration technique led to successful treatment of the disease.
Conclusion
As the parasite has not been reported to date in Nepal, many people are unaware of its mode of infection and pathogenesis. Many laboratory workers are heedless with the egg of the parasite due to which this parasite might be misdiagnosed or undiagnosed. This case report might help laboratory workers to be sentient about the parasite and further diagnosis in future.
Keywords: Schistosoma japonicum, Schistosomiasis, first case report, CIWEC Hospital, Nepal
Background
Genus Schistosoma (blood fluke) belongs to phylum Platyhelminthes, class Trematoda, subclass Digenea and family Schistosomatidae. Schistosomiasis is one of the oldest known diseases in human history caused due to schistosomes. Many species of genus Schistosoma have been discovered from long ago. Schistosoma japonicum, causing Katayama disease, was first recognized by Akira Fujinami in 1847. Fujinami and Nakamura were the first to report skin infection by S. japonicum cercariae in different mammals in 1909 [1]. The worm was discovered by Fujiro Katsurada in 1904 [2]. It was described in the snail host by Miyairi and Suzuki in 1913 and later the life cycle was described by Leiper et al. [3, 4].
Schistosoma species are dioecious trematodes. The adult schistosomes live in pairs and are approximately 1 to 2 cm long [4]. The eggs of schistosomes are the diagnostic base for the laboratory and species identification. S. japonicum might be considered as the most pathogenic species among all species of schistosomes being a causative agent for a wide range of complications like Katayama fever, liver cirrhosis, pulmonary fibrosis, portal hypertension, splenomegaly and neuroschistosomiasis [4].
Schistosomiasis is generally prevalent in tropical and subtropical regions, especially in poor communities where there is no proper access to safe drinking water and adequate sanitation. It is estimated by WHO, that at least 90 % of those requiring treatment for schistosomiasis live in Africa. S. japonicum has been commonly encountered in China, the Philippines, Indonesia, etc [3, 5, 6]; to date, we are not aware of any documented case acquired in Nepal. Therefore, we report the first case of Schistosomiasis caused by S. japonicum at CIWEC Hospital and Travel Medicine Center, Kathmandu, Nepal.
The CIWEC hospital is a specialized clinic for travellers situated in Kathmandu and is a geo sentinel surveillance site. CIWEC Hospital sees around 8000 patients per year, predominantly travellers. Approximately 30 % of the case load consists of diarrheal disease; altitude-related illness and febrile illness make up significant parts of the caseload.
A written informed consent has been taken from the patient for necessary investigations and case publication in scientific journals.
Case presentation
A 23-year-old female presented at CIWEC hospital as an out-patient on 8 August 2018, with clinical symptoms of passage of loose watery stools, four–five episodes per day from the previous 2 days with no blood or mucus in the stool as per macroscopic observation. It was associated with fever one episode one day prior to arrival to hospital, which resolved on its own. She had one episode of vomiting on the day of arrival to the hospital. She felt bloated and had a lot of gurgling sounds in her abdomen. Her appetite was normal and she had no nausea. She had no history of any chronic or pre-existing illness.
Regarding her travel history, she had not visited different countries in Europe since 2 years ago. There was no history of travel outside of Spain since last August. She is a non-vegetarian, which would include eating fish on and off in her diet. She had arrived in Nepal in July and had been working as a volunteer in two orphanages in Kathmandu. She admitted that she was not very punctual with her hand hygiene as she would often play with the soil and mud in the orphanage.
Physical examination showed blood pressure 110/60 mmHg, temperature 38.3 o C, and pulse rate 111 per minute, respiration rate 18 per minute. The patient was given paracetamol orally for fever management.
After physical examination, blood and stool samples were collected for laboratory investigations.
Haematological investigation
The haematological investigations showed that blood cell parameters and indices were in the acceptable range (Table 1).
Table 1.
|
Complete blood count |
Results |
|---|---|
|
Haemoglobin (12–16 g dl−1) |
12.7 g dl−1 |
|
Total red cell count (4.2–5.2×106 µl−1) |
4.27×106 µl−1 |
|
Hematocrit (37–48 %) |
37.5 % |
|
MCV (80–100 fl) |
87.8 fl |
|
MCH (27–32 pg) |
29.7 pg |
|
MCHC (32–36 %) |
33.9% |
|
Total white cell count (4–10×10 3 µl−1) |
5.3×10 3 µl−1 |
|
Differential Leucocyte count |
|
|
Neutrophils (40–70 %) |
55 |
|
Lymphocyte (20–45 %) |
43 |
|
Monocyte (2–10 %) |
02 |
|
Eosinophil (0–6 %) |
00 |
|
Basophil (0–2 %) |
00 |
|
Platelet count (150–450×103 µl−1) |
248×103 µl−1 |
Biochemical findings
All the biochemical parameters, i.e. blood glucose, BUN, creatinine, electrolytes, liver enzymes and pancreatic enzymes were also found normal. (Table 2)
Table 2.
|
Tests (reference range) |
Results/findings |
|---|---|
|
Glucose, random (70–140 mg dl−1) |
85 mg dl−1 |
|
Renal function tests |
|
|
Blood Urea Nitrogen (7–21 mg dl−1) |
7.1 mg dl−1 |
|
Serum creatinine (0.6–1.4 mg dl−1) |
0.8 mg dl−1 |
|
Sodium (135–146 mEq l−1) |
139 mEq l−1 |
|
Potassium (3.5–5.2 mEq l−1) |
4.2 mEq l−1 |
|
Liver function tests |
|
|
Total bilirubin (<1.4 mg dl−1) |
0.3 mg dl−1 |
|
SGOT (AST) (<40 IU l−1) |
15 IU l−1 |
|
SGPT (ALT) (<40 IU l−1) |
16 IU l−1 |
|
ALP (90–460 IU l−1) |
113 IU l−1 |
|
Total Protein (6–8 gm dl−1) |
6.5 gm d−1 |
|
Albumin (3.3–5.5 gm dl−1) |
3.5 gm dl−1 |
|
Pancreatic function test |
|
|
Serum amylase (25–90 IU l−1) |
29 IU l−1 |
C-reactive protein: Negative (less than 5 mg l−1)
Stool examination
Stool examination was performed by direct wet mount method and formal ether concentration method. Stool was collected from the patient and direct wet mount and formal ether concentration techniques were performed.
Macroscopically, the stool colour was brown and was soft in consistency without any evidence of visible blood.
On microscopic examination, pus cells, mucus and red blood cells were not seen in direct wet mount of stool. However, there were plenty of eggs of S. japonicum (Figs 1–6) observed, which was spotted by Medical Technologist of CIWEC Hospital, Lainchaur and confirmed by the Clinical Microbiologist of National Public Health Laboratory (Reference Laboratory), Government of Nepal, Teku.
Fig. 1.
Width of S. japonicum egg (x100).
Fig. 2.
Length of S. japonicum egg (x100).
Fig. 3.

S. japonicum egg where the red arrow indicates a knob (x40).
Fig. 4.

S. japonicum egg where the red arrow indicates a knob (x40).
Fig. 5.
S. japonicum egg where the red arrow indicates a knob (x100).
Fig. 6.
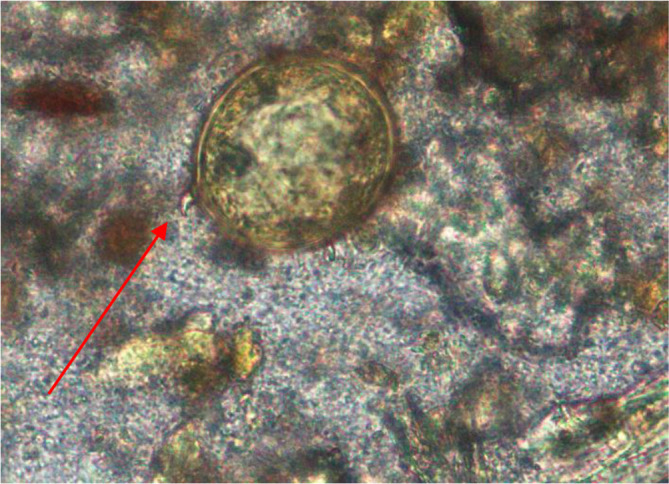
S. japonicum eggwhere the red arrow indicates a knob (x100).
The egg of the parasite was clear and pale yellow colour with a knob at one end (indicated by the red arrow in the images) (Figs 3–6). The eggs measured approximately 60–65 µm in length and 50–55 µm in breadth (Figs 1 and 2).
Follow up
Physical examination
The patient had no complaint of fever, headaches and abdominal bloating. Her temperature, pressure and pulse were also normal.
Stool examination
The stool was processed for routine and microscopic examination and also concentration technique was performed. The eggs of S. japonicum were not present.
Blood tests
Patient refused the blood test on her follow up.
Discussion
Many species of schistosomes have been reported from neighbouring countries of Nepal [7]. But only a few cases have been reported from Nepal to date since these parasites are uncommon in Nepal. Eggs with the appearance of Schistosoma mansoni have been reported in the inhabitants of Dhanusha district, Nepal, by Sherchand et al. and the seroprevalance for schistosomes of 18 % was found in the same district in 1996–1997, and 22.7 in the following year, i.e. 1998 in a follow-up study [8]. Devkota et al. confirmed the presence of Schistosoma indicum species by mitochondrial cytochrome oxidase I, 12S, 16S and 28S sequences (3675 bp) analysis of cercariae recovered from snails in Terai and hilly regions of Nepal from 2007 to 2014 [9]. But no cases of S. japonicum have been reported to date in Nepal – which might be due to the lack of the appropriate intermediate host, i.e. snail (Oncomelania spps) [8].
The first living case of S. japonicum in Malaysia has been reported by Murugasu et al. in 1973 in a patient with nephrotic syndrome. Leshem et al. diagnosed 7 out of 12 travellers with acute schistosomiasis caused by S. japonicum in 2009 in Laos [10]. The current case is also associated with a traveller having a history of recent arrival in Nepal with symptoms of acute schistosomiasis.
The source of infection is contact with fresh water contaminated with the cercariae and the mode of infection is skin penetration. The appropriate intermediate host, i.e. snail (Oncomelania spps) is required for the development of miracidium hatched from eggs excreted in the stool of definitive hosts like humans and other mammals [11]. The present case shows the symptoms of acute schistosomiasis and the stool examination also revealed the eggs of S. japonicum.
S. japonicum is susceptible to antihelminthic drugs and the drug of choice for acute schistosomiasis is Praziquantel (single dose) [4]. Due to the timely diagnosis and successful treatment of patient, the disease did not progress and other complications were avoided.
Conclusion
The clinical condition due to the infestation of the parasite ranges from asymptomatic carrier to liver cirrhosis. The clinical symptoms and presentation of the disease are also similar to other helminthic infestation, hence only the careful examination of the stool, probably concentration technique along with the direct examination might increase the sensitivity of the detection of the egg of parasite, which help in appropriate treatment of the disease.
Funding information
The authors received no specific grant from any funding agency.
Acknowledgements
We are thankful to the director of CIWEC Hospital Travel Medicine Center, Dr. Prativa Pandey who encouraged to write this paper. We appreciate Dr. Shanta Manandhar for taking the clinical history of the patient. We are also very grateful to Head of Department of Laboratory, Mrs. Shristi Shakya for providing all the required instruments and reagents for the case study and Medical Laboratory Technologist, Mr. Ramachandra Rajah, Mr. Ananta Pokharel, Mr. Saran Maharjan and Mr. Keshav Joshi for helping in case study. We are grateful to Mr. Shyam Kumar Mishra for recommending this journal for publication and Ms. Meera Hada for editing the languages, grammars and vocabulary. We are also very thankful to all the staffs of CIWEC Hospital Travel Medicine Center who are directly or indirectly involved in the case report.
Author contributions
Dipendra Bajracharya spotted the parasite in the laboratory of CIWEC Hospital in the clinical sample and prepared the manuscript. Dr Durga Bhandari dealt with the patient, the whole clinical history was written by him and he also assisted for the submission. Mr Sanjeet Pandit is a Clinical Microbiologist and he confirmed the egg of the parasite and assisted with the submission by editing the manuscript.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Ethical statement
Ethics approval and consent to participate and publish: the ethical approval and consent from patient has been taken from the patient and is available on request. The patient data are confidential however, the clinical samples have been preserved for the further analysis are available on request.
Footnotes
Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; bp, base pair; fl, femtoliter; g/dL, gram per deciliter; IU/L, International Unit per liter; µl, microliter; µm, micrometer; MCH, mean corpuscular hemoglobin; MCHC, mean corpuscular hemoglobin concentration; MCV, mean corpuscular volume; mEq/L, miliequivalent per liter; mg/dL, milligram per deciliter; mmHg, millimeter of mercury; pg, pictogram; SGOT, serum glutamic oxaloacetic transaminase; SGPT, serum glutamate pyruvate transaminase.
References
- 1.Carabin H, Johansen MV, Friedman JF, McGarvey ST, Madsen H, et al. Zoonotic schistosomosis (schistosomiasis). 2011;1(January). Available from. 2011.
- 2.Katsurada F. Schistosomiasis japonica. Zentralblatt fur Bakteriol Parasitenkunde, Infekt und Hyg Abt I. 1913;72(4/5):363–79. Available from: https://www.cabdirect.org/cabdirect/abstract/19142900427 . 1913
- 3.FEG C. In: Topley and Wilson’s Parasitology. 9th ed. Albert B, Max S, editors. Oxford University Press; 1930. [Google Scholar]
- 4.Gillespie SH, Pearson RD. Principles and Practice of Clinical Parasitology Principles and Practice of Clinical Parasitology. John Wiley and Sons Ltd: 2001. [Google Scholar]
- 5.Zhou X-N, Guo J-G, Wu X-H, Jiang Q-W, Zheng J, et al. Epidemiology of schistosomiasis in the people's Republic of China, 2004. Emerg Infect Dis. 2007;13:1470–1476. doi: 10.3201/eid1310.061423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murugasu R, Wang F, Dissanaike AS. Schistosoma japonicum-type infection in Malaysia--report of the first living case. Trans R Soc Trop Med Hyg. 1978;72:389–391. doi: 10.1016/0035-9203(78)90133-5. [DOI] [PubMed] [Google Scholar]
- 7.Agrawal MC. Introduction BT - Schistosomes and Schistosomiasis in South Asia. India: Springer India; 2012. pp. 1–6. [Google Scholar]
- 8.Sherchand JB, Ohara H, Sherchand S, Matsuda H. The suspected existence of Schistosoma mansoni in Dhanusha district, southern Nepal. Ann Trop Med Parasitol. 1999;93:273–278. doi: 10.1080/00034983.1999.11813423. [DOI] [PubMed] [Google Scholar]
- 9.Devkota R, Brant SV, Loker ES. The Schistosoma indicum species group in Nepal: presence of a new lineage of schistosome and use of the Indoplanorbis exustus species complex of snail hosts. Int J Parasitol. 2015;45:857–870. doi: 10.1016/j.ijpara.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leshem E, Meltzer E, Marva E, Schwartz E. Travel-related schistosomiasis acquired in Laos. Emerg Infect Dis. 2009;15:1823–1826. doi: 10.3201/eid1511.090611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drasar BS. In: Topley & Wilson’s Microbiology and Microbial infections. 9th ed. Albert B, Max S, editors. Oxford University Press; 1932. [Google Scholar]





