Abstract
Purpose
Transitional cell carcinomas of the lacrimal sac are rare with less than 55 cases reported in the literature. These tumors typically present with a medial canthal mass and epiphora.
Observations
Here we describe a 63-year-old male who presented originally with complaints of dry eye and chronic epiphora. Over the next six months the patient noted the onset of a right medial canthal mass with tenderness and purulent lacrimal reflux. The patient was scheduled for surgery, and a lacrimal sac mass was identified. After excisional biopsy, the mass was diagnosed as transitional cell carcinoma and the patient subsequently underwent right lacrimal sac excision and medial maxillectomy. He was treated post-operatively with chemotherapy and radiation and has undergone subsequent reconstruction for lid malposition and lacrimal obstruction. There has been no recurrence of the cancer over a five-year period, with no evidence of distant metastasis.
Conclusions and importance
Transitional cell carcinomas of the lacrimal sac can be aggressive and in general carry a poor prognosis. Physicians should have a high index of suspicion in patients presenting with medial canthal mass to avoid delayed diagnosis.
Keywords: Transitional cell carcinoma, Lacrimal sac, Carcinoma, Medial canthal mass
Highlights
-
•
Lacrimal sac carcinomas are typically of epithelial origin.
-
•
Epithelial carcinomas include squamous cell, adenocarcinoma, or transitional cell.
-
•
Transitional cell carcinomas of the lacrimal sac are rare.
-
•
Lacrimal sac carcinomas typically present with medial canthal mass and epiphora.
-
•
Transitional cell carcinomas of the lacrimal sac carry poor prognosis.
1. Case presentation
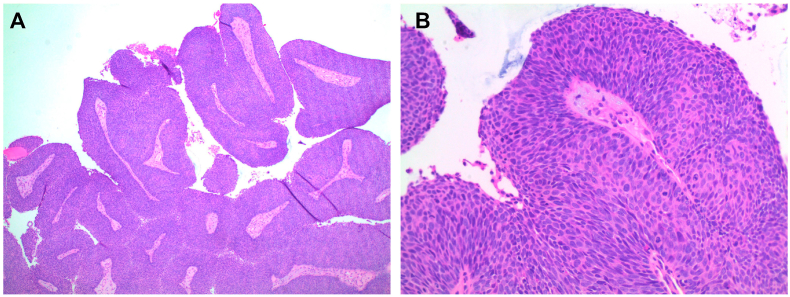
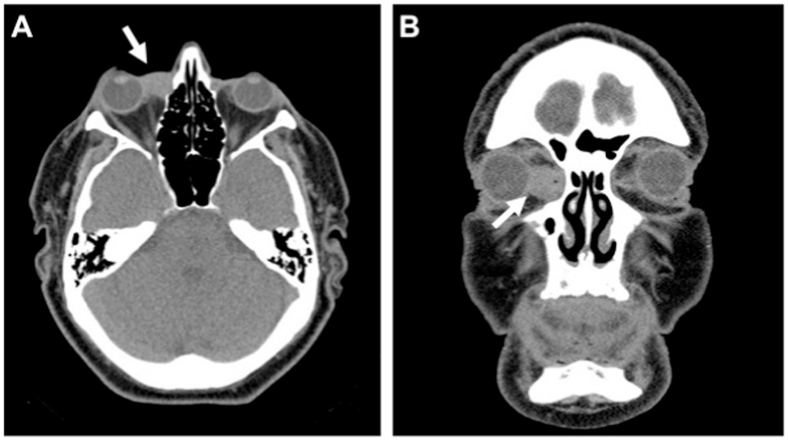
The patient is a 63-year-old male who presented with a six-month history of dry eye and epiphora. His clinical status progressed over the next several months, with increasing tenderness of the right upper eyelid and development of a right medial canthal mass. There were no visual acuity changes. He was treated for suspected lacrimal infection with possible abscess, however despite treatment the mass continued to enlarge and became erythematous with granulation tissue extruding from the lower punctum. He was referred for definitive treatment, and was taken to the operating room for probable dacryocystorhinostomy with stent placement. During the procedure the lacrimal sac was found to contain a papillomatous and cauliflower-like lesion, which filled the entire lacrimal sac. The mass could not be easily dissected off the lacrimal sac wall, and with as much resection of visible tumor as possible the lesion was removed. The remainder of the surgical procedure and postoperative recovery was uneventful. The pathology report revealed a papillomatous lesion with both endophytic and exophytic features with extensive full thickness dysplasia and atypia with mitotic figures extending to near the surface. The cells were basaloid with rare foci suggesting gland formation favoring transitional cell carcinoma (Fig. 1A). Fig. 1B shows islands of tumor within the stroma with associated desmoplasia consistent with invasion; however, invasion was not present on the frozen section tissue. CT scans revealed a soft tissue mass in the medial canthus of the right orbit in the region of the lacrimal sac of approximately 1.5 cm × 1.8 cm x 1.6 cm in dimension (Fig. 2A–B). It was noted to extend into the lacrimal duct and into the orbit displacing the globe without proptosis. There was evidence of right lacrimal bone enlargement. PET scan and further evaluation showed no evidence of distant disease, indicating the lacrimal mass was the primary tumor. The rarity of the transitional cell carcinoma of the lacrimal sac, coupled with the aggressive nature of this tumor, necessitated a multidisciplinary approach, which was unavailable to the authors at the time of presentation. To obtain the optimal results, the patient was referred to a tertiary care center for further treatment. Surgical excision of the tumor included complete right lacrimal sac resection with excision of entire medial canthal area, canalicular system, and lacrimal sac as well as requiring complete superior medial maxillectomy. The mass was completely excised and demonstrated no lymphovascular or perineural invasion. The tumor was positive for FGFR3 expression which is typically associated with non-invasive and low-grade transitional cell carcinomas.1 The patient underwent radiation with 60 Gy in 30 fractions over approximately four weeks and subsequent chemotherapy treatment with Cisplatin. He has since undergone reconstructive surgery for lid malposition two years after completing chemotherapy and radiation including right upper eyelid ptosis and two retraction repairs of lower eyelid. He underwent conjunctivo-dacryocystorhinostomy with a Jones tube. However due to lack of bony fixation, the Jones tube migrated and was ultimately removed. To date, he has had no reoccurrence of the transitional cell carcinoma over a five-year period and has experienced continuous tearing but minimal visual defects otherwise.
Fig. 1.
Surgical pathology of transitional cell carcinoma A. H&E, 40x. B. H&E, 200x.
Fig. 2.
CT image of the sinuses with contrast demonstrating the tumor (white arrow) in the medial canthus of the right orbit in the region of the lacrimal sac A. Axial view. B. Coronal view.
2. Discussion
Primary tumors of the lacrimal sac are rare and are most commonly of epithelial origin (73%).2 Epithelial cancers of the lacrimal sac are sub-divided into squamous cell carcinoma, adenocarcinoma, or transitional cell carcinoma.3 Epithelial tumors are likely to be malignant (55–75%) and transitional cell carcinomas carry the worst prognosis with an average mortality rate of 37–44%.2,4, 5, 6 Transitional cell carcinoma of the lacrimal sac is extremely rare and typically presents as metastasis from a distant site; less than 55 cases of transitional cell carcinoma and one case of combined transitional cell carcinoma and adenocarcinoma have been reported in a review of the literature.4,7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19 The most common presenting symptoms include medial canthal mass, epiphora, and rarely epistaxis or dacromenorrhea with an average age of presentation at 47–50 years.4,20,21 Lacrimal sac tumors are often misdiagnosed as dacrocystitis and 43% are reportedly not discovered until dacryocystorhinostomy.5 Late diagnosis may have serious consequences including delayed treatment and progression of disease with higher recurrence rates.3,22 While medial maxillectomy with excision of as much of the lacrimal system as possible is the preferred surgical treatment for lacrimal sac tumors, a multidisciplinary approach offers an optimal result for this type of neoplasm.2 A systematic evaluation (clinical/radiological/hematological) is mandatory prior to definitive treatment, and in many cases, a more radical surgery or radiotherapy may be the most appropriate treatment of aggressive tumors. However, given the propensity for regional metastasis seen in larger, infiltrative malignant lesions, we believe that in addition to a wide local excision (medial maxillectomy/orbital exenteration/paranasal sinus resection) and application of radiotherapy as appropriate, a concomitant staging or therapeutic regional lymphadenectomy that may include ipsilateral parotidectomy and selective neck dissection should be considered.
3. Conclusions
The unique presentation of this tumor reminds all lacrimal surgeons that despite the rarity of lacrimal sac tumors, the lacrimal surgeon should be aware of the potential for lacrimal malignancy, and be mindful of unusual anatomic presentations during surgical exploration.
Patient consent
The patient consented to publication of the case and accompanying images in writing.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The authors of the present manuscript hereby declare they have no conflict of interest or any financial interest in this publication.
Acknowledgements
None.
Contributor Information
Hayley V. Miller, Email: hvmiller@email.sc.edu.
John D. Siddens, Email: john.siddens@prismahealth.org.
References
- 1.Akanksha M., Sandhya S. Role of FGFR3 in urothelial carcinoma. Iran J Pathol. 2019 Spring;14(2):148–155. doi: 10.30699/IJP.14.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parmar D.N., Rose G.E. Management of lacrimal sac tumours. Eye. 2003;17:599–606. doi: 10.1038/sj.eye.6700516. [DOI] [PubMed] [Google Scholar]
- 3.Krishna Y., Coupland S.E. Lacrimal sac tumors—a review. Asia Pac J Ophthalmol. 2017;6(2):173–178. doi: 10.22608/APO.201713. [DOI] [PubMed] [Google Scholar]
- 4.Azari A.A., Kanavi M.R., Saipe N. Transitional cell carcinoma of the lacrimal sac presenting with blood tears. JAMA Ophthalmol. 2013;131(5):689–690. doi: 10.1001/jamaophthalmol.2013.2907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flanagan J.C., Stokes D.P. Lacrimal sac tumors. J Ophthalmol. 1978;85(12):1282–1287. doi: 10.1016/s0161-6420(78)35554-8. [DOI] [PubMed] [Google Scholar]
- 6.Preechawai P., Della Roccad R.C., Della Rocca D. Transitional cell carcinoma of the lacrimal sac. J Med Assoc Thai. 2005;88(Suppl 9):S138–S142. [PubMed] [Google Scholar]
- 7.Alabiad C.R., Weed D.T., Walker T.J. En bloc resection of lacrimal sac tumors and simultaneous orbital reconstruction: surgical and functional outcomes. Ophthalmic Plast Reconstr Surg. 2014;30(6):459–467. doi: 10.1097/IOP.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 8.Ali M.J., Bothra N., Nalid M.N. Transitional cell carcinoma of lacrimal sac. Ophthalmic Plast Reconstr Surg. 2018;34(3) doi: 10.1097/IOP.0000000000000937. [DOI] [PubMed] [Google Scholar]
- 9.Anderson K.K., Lessner A.M., Hood I., Mendenhall W., Stringer S., Warren R. Invasive transitional cell carcinoma of the lacrimal sac arising in an inverted papilloma. Arch Ophthalmol. 1994;112(3):306–307. doi: 10.1001/archopht.1994.01090150036014. [DOI] [PubMed] [Google Scholar]
- 10.El-Sawy T., Frank S.J., Hanna E. Management of lacrimal sac/nasolacrimal duct carcinomas. Ophthalmic Plast Reconstr Surg. 2013;29(6):454–457. doi: 10.1097/IOP.0b013e31829f3a73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Erickson B.P., Modi Y.S., Ko M.J. Transitional cell-type papillary carcinoma of the lacrimal sac manifesting as a medial canthal skin lesion. Orbit. 2014;33(5):378–381. doi: 10.3109/01676830.2014.894541. [DOI] [PubMed] [Google Scholar]
- 12.Eweiss A.Z., Lund V.J., Jay A., Rose G. Transitional cell tumours of the lacrimal drainage apparatus. Rhinology. 2013;51(4):349–354. doi: 10.4193/Rhino13.016. [DOI] [PubMed] [Google Scholar]
- 13.Islam S., Thomas A., Eisenberg R.L., Hoffman G.R. Surgical management of transitional cell carcinoma of the lacrimal sac: is it time for a new treatment algorithm? J Plast Reconstr Aesthetic Surg. 2012;65(2):e33–e36. doi: 10.1016/j.bjps.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 14.Lee L.N., Scott A.R., Chan A.W., Frankenthaler R.A. Management of transitional cell carcinoma of the lacrimal sac: a multidisciplinary approach to orbit sparing treatment. Laryngoscope. 2010;120 doi: 10.1002/lary.21625. S161-S161. [DOI] [PubMed] [Google Scholar]
- 15.Lüchtenberg M., Emmerich K.H. Tränensackhydrops mit Epiphora am rechten Auge. Tansitionalzellkarzinom des Tränensacks [Hydrops of the lacrimal sac with epiphora of the right eye. Transitional cell carcinoma of the lacrimal sac] Ophthalmologe. 1999;96(4):274–275. doi: 10.1007/s003470050406. [DOI] [PubMed] [Google Scholar]
- 16.Jones H., Thornhill C. Transitional celled carcinoma of the lacrimal sac. J Laryngol Otol. 1969;83(4):397–401. doi: 10.1017/s0022215100070481. [DOI] [PubMed] [Google Scholar]
- 17.Mihailovic N., Steenken J., Elges S. [Masquerade lacrimal duct stenosis: prevalence of lacrimal sac tumors]. Der Ophthalmologe. Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2020 May;117(5):439–444. doi: 10.1007/s00347-019-00971-z. [DOI] [PubMed] [Google Scholar]
- 18.Nomura T., Maki D., Matsumoto F. A rare case of coexisting lacrimal sac adenocarcinoma and transitional cell carcinoma. Ear Nose Throat J. 2018;97(10-11):e32–e35. [PubMed] [Google Scholar]
- 19.Vickers J.L., Matherne R.J., Allison A.W. Transitional cell neoplasm of the nasolacrimal duct associated with human papillomavirus type 11. J Cutan Pathol. 2010;37(7):793‐796. doi: 10.1111/j.1600-0560.2009.01351.x. [DOI] [PubMed] [Google Scholar]
- 20.Stefanyszyn M.A., Hidavat A.A., Pe’er J.J., Flanagan J.C. Lacrimal sac tumors. Ophthalmic Plast Reconstr Surg. 1994;10(3):169–184. doi: 10.1097/00002341-199409000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Karim R., Ghabrial R., Lin B. Transitional cell carcinoma of the lacrimal sac. Clin Ophtalmol. 2009;3:587–591. doi: 10.2147/opth.s7706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ni C., D'Amico D.J., Fan C.Q., Kuo P.K. Tumors of the lacrimal sac: a clinicopathological analysis of 82 cases. Int Ophthalmol Clin. 1982;22(1):121–140. doi: 10.1097/00004397-198202210-00010. [DOI] [PubMed] [Google Scholar]