Abstract
Objective
Quantify the effect of the osseodensification Densah® protocol on the insertion torque, ISQ, and the removal torque of conical BioHorizons® implants.
Materials and methods
An ex vivo model over fresh pig tibia bone was used. Test group (TG) included 50 osteotomies using Densah® osseodensification protocol, and the control group (CG), 50 osteotomies using BioHorizons®’s recommended procedure. Conical BioHorizons® implants (3.8 × 10.5 mm) were implanted, verifying the insertion torque with a manual torque meter. ISQ values were registered with Ostell® device. Finally, implants were removed with manual reverse torque registering the values. Results were analyzed and compared with the Mann-Whitney test and t-test.
Results
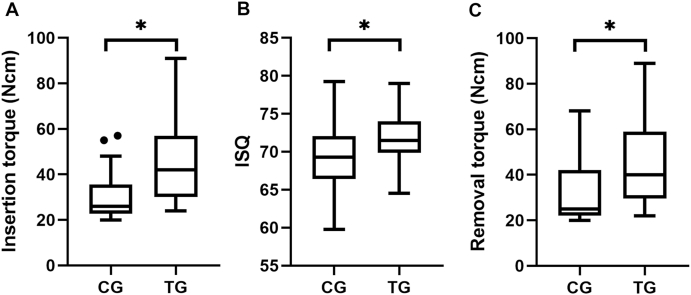
Median and interquartile range per group were as follows: insertion torque, CG: 26 (12) Ncm; TG: 42 (26) Ncm, removal torque, CG: 25 (20) Ncm; TG: 40 (28) Ncm, ISQ value, CG: 69.25 (5.5); TG: 71.5 (4). All variables were significantly higher (p ≤ 0.05) in the osseodensification group.
Conclusions
The Osseodensification technique may improve primary stability in the clinical scenario on tapered implants. Further human RCTs are necessary to validate this.
Keywords: Osseodensification, Densah, Dental implant stability
1. Introduction
Dental implant stability (absence of movement) is a critical factor described for reaching osseointegration and the use of immediate loading protocols.1 The absence of movement at the surgery time that is obtained by the friction between the implant and the bone walls is called primary stability, and the biologic stability achieved through the osseointegration process is called secondary stability.2 Primary stability depends on surgical factors (surgical technique and implant design) and patient factors (bone quality and quantity).3 Surgical techniques, including bicorticalization,4 under preparation of implant bed,5 and the use of osteotomes and condensers,6 can enhance primary stability with a considerable amount of success but with some drawbacks, like excessive compression, which hinders the secondary stability of the implant and its adequate osseointegration.7
Osseodensification (OD) is a universal drilling non-subtractive technique that could obtain better primary implant stability on low-density bone and allow implant insertion in thin ridge sites preventing the complications of the methods mentioned above.8 The system involves several drills that act in two ways; clockwise direction for cutting, and in the opposite direction for osseodensification. The cone-shaped drill has four or more cutting grooves at negative angles, which allows preserving bone by autografting bone particles against the bed walls, through an entry and exit movement. The pumping of saline solution facilitates plasticity and bone expansion. These drills combine the advantages of the osteotomes, with the speed and tactile control of the surgical drills, allowing to control the bone densification process.8, 9, 10
Until now, there are no preclinical articles that show the behavior of OD over BioHorizons® tapered internal implants primary stability. This information is critical previous to a randomized clinical trial using these implants and OD techniques. This study aimed to quantify the effect of the Densah® osseodensification protocol (Versah®, Jackson, Michigan, USA) on the insertion, removal torque, and RFA of BioHorizons® conical implants compared to conventional drilling protocol, using an ex vivo animal model.
2. Materials and methods
2.1. Sample
An experimental ex vivo study model was designed, using fresh commercially available cuts of pig tibia with three days since animal death. Bone samples were prepared by removing all types of attached soft tissues and exposing the flat surface of spongy bone, similar to the bone density type III-IV described by Lekholm and Zarb (see Fig. 1), with a transverse section.
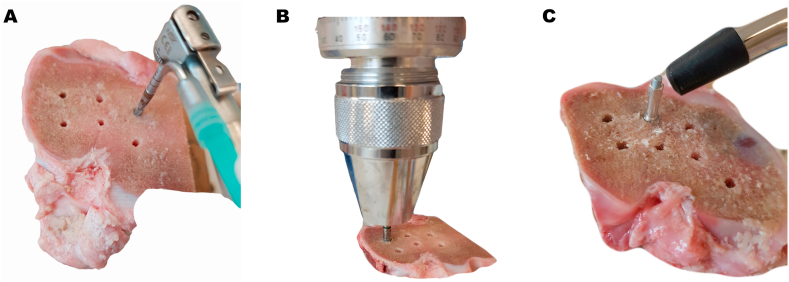
Fig. 1.
Images of implant beds drilling, torque, and ISQ measurement.
A: Drilling of implant beds, B: Torque measurement, C: ISQ measurement.
An arbitrary sample size of 100 osteotomies was selected, 50 assigned to the control group (conventional drilling protocol), and 50 to the test group (Densah® osseodensification protocol). Between 6 and 8 tibial osteotomies were prepared, first by drilling and then by installing BioHorizons® Tapered Internal implants (BioHorizons, Birmingham, Alabama, USA) of 3.8 mm in diameter and 10.5 mm in length.
2.2. Preparation of osteotomies
The samples were mounted on a wooden press where they were stable and without movement. A surgical motor with speed control, torque monitoring, and saline irrigation (NSK Surgic Pro, NSK Nakanishi Inc, Tochigi, Japan) was used. All osteotomies were performed at a minimum distance of 10 mm between them and from the tibial external cortical bone.
In the control group (CG), the osteotomies were performed with the manufacturer's original surgical system (BioHorizons® Tapered HD surgical system, BioHorizons®, Birmingham, Alabama, USA), using a 3-step sequence to progressively enlarge the preparation consisting on surgical drills of 2.0 mm, 2.5 mm and 3.2 mm, all 10.5 mm deep, under abundant saline irrigation, 1200 RPM clockwise, and 50Ncm torque (drill diameter as manufacturer informs it).11
In the test group (TG) the osteotomies were prepared with 10.5 mm deep using Densah® drills (Versah®, Jackson, Michigan, USA) in a sequence of 3 steps corresponding to the osseodensification for soft bone: a 2.0 mm pilot drill in a clockwise direction, VT1525 drill then VT2535 both in a counterclockwise direction, all 10.5 mm deep, under abundant saline irrigation, 1200 RPM, 50 N torque (Fig. 1A). All Densah® burs, excluding the pilot one, are tapered and have a patent thread design that gives them the osseodensification properties. VT2535 drill has a 3.0 mm diameter at 8 mm length with progressive widening up to 3.5 mm diameter at 11.5 mm length.12
BioHorizons tapered internal 3.8 × 10.5 mm implants were installed in each osteotomy, at a speed of 30 RPM and a torque of 30 Ncm, until the implant platform reaches 2–3 mm over bone level.
2.3. Insertion torque, RFA and removal torque
Implant insertion was continued manually using an analog Torque Gauge (Tohnichi Torque Gauge 45 ATG, Tohnichi MFG. CO., Tokyo, Japan), to register the peak value of the insertion torque (Ncm) by bringing the implant to the bone level position (Fig. 1B). The ISQ values were then assessed using the Ostell ISQ® instrument (Ostell, Gothenburg, Sweden), registering the value on the four faces of each implant (anterior, posterior, medial and lateral concerning the anatomical position of the tibia), and the average value of these measurements were assigned to each implant (Fig. 1C).
Finally, each implant was removed from its preparation manually through reverse torque (Tohnichi Torque Gauge 45 ATG, Tohnichi MFG. CO., Tokyo, Japan), registering the numerical value in Ncm.
2.4. Statistical analysis
A statistical analysis of the results was performed using STATA 14.2 software (StataCorp LLC, College Station, Texas, USA). The Shapiro Wilk test and histograms were performed to evaluate the distribution of the continuous variables (insertion and removal torque, and ISQ). The non-parametric Mann-Whitney test was applied to compare the insertion and removal torque between both groups, and an unpaired t-test to compare the ISQ values. A p-value of 0.05 was established as the level of significance. The graphics were created with GraphPad Prism 8.2.1 software (San Diego, CA, USA).
3. Results
The descriptive statistics of insertion torque, removal torque, and ISQ are in Table 1. A correlation between the ISQ values and the insertion torque, removal torque, and between the insertion and removal torque (see Fig. 2) was found, which expresses of a direct relationship between these values.
Table 1.
Description of insertion, removal torque, and ISQ values for both study groups.
| Variable | Protocol | P50 | IQR | min | max | N | p value |
|---|---|---|---|---|---|---|---|
| Insertion torque (Ncm) | CG | 26 | 12 | 20 | 57 | 50 | <0.001* |
| TG | 42 | 26 | 24 | 91 | 50 | ||
| Removal torque (Ncm) | CG | 25 | 20 | 20 | 68 | 50 | <0.001* |
| TG | 40 | 28 | 22 | 89 | 50 | ||
| ISQ | CG | 69.25 | 5.5 | 59.8 | 79.3 | 50 | <0.001** |
| TG | 71.5 | 4 | 64.5 | 79 | 50 |
CG: control group (standard protocol), TG: test group (osseodensification protocol), P50: median, IQR: interquartile range, *Mann-Whitney, ** t-test.
Fig. 2.
Scatter plot over three studied variables (insertion, removal torque and ISQ values).
A: Relation between ISQ and insertion torque, B: Relation between ISQ and removal torque, C: Relation between removal and insertion torque.
The values of the insertion torque, ISQ, and removal torque were found to be higher for the test Densah® osseodensification group (TG), with statistically significant value (p < 0.001) compared to the conventional drilling control group (CG) (Table 1 and Fig. 3).
Fig. 3.
Box plot comparing insertion, removal torque, and ISQ values among test and control groups.
CG: Control group, TG: Test group. A: Insertion torque box plot, B: ISQ box plot, C: Removal torque box plot.
4. Discussion
One of the main advantages of osseodensification (OD) technique is that due to autografting of bone particles during the implant bed drilling, it is possible to obtain a condensed living bone surrounding the implant.8 As a consequence, it could be an increase of primary implant stability with all the benefits associated with it. Our results show a significant increase of insertion, removal torque, and ISQ values for the OD group (TG) compared to control (CG) on BioHorizons® tapered internal implants inserted over a low-density bone (view Table 1 and Fig. 3).
It is frequent to find clinical situations in which medullary bone density is pretty light, such as maxilla and posterior mandible, a situation that is worst on elderly patients. Even if the actual implant surface treatments can reach predictable osseointegration with low or non-primary stability as long as they do not support early loading forces, higher primary stability helps to reach good secondary stability faster and predictable, allowing the use of immediate loading protocols.13,14 Besides, OD not only enhances primary stability, but it can also allow implant insertion over thin ridges avoiding ridge splitting technique and the use of osteotomes preventing their complications.8,15 Also, the majority of the complications described for osteotome technique (hammered or motorized) and under-drilling could be avoided using OD technique. That is why OD seems an excellent tool for implant placement.
There is preclinical research that also shows the increase of primary stability using OD technique. Working with a similar ex vivo model, Huwais and Meyer used osseodensification protocol on 72 straight-walled implants (4.1 and 6.0 of diameter, 11 mm long).8 Three different groups were compared: standard protocol, clockwise drilling with Densah® burs, and OD with Densah® burs, scoring insertion, removal torque, and ISQ values. OD group showed higher values than the other two groups for two variables: mean insertion torque 49 (±24) Ncm, mean removal torque 31 (±17) for 4.1 × 11 mm implants. The authors claimed that these values were almost double than the standard protocol. Our findings also show higher torque values using OD technique, with a superior removal torque. With the tapered design, higher stability is expected. Maybe this difference was not big enough in our case due to the smaller diameter of our test implants.
Other authors also show higher implant insertion torque for OD compared with standard drilling or other protocols. Lopez et al.16 obtained a mean of 65 Ncm for OD, compared to 35 Ncm for the control group using tapered implants over sheep spine. Lahens et al.17 over sheep ilium on an in vivo model, compare OD with Densah® burs, standard drilling, and clockwise Densah® drilling. Insertion torque was evaluated using parallel and tapered wall design implants (15 implants per group). OD shows higher insertion torque (mean 100 Ncm) than the control group (mean 25 Ncm).
On another publication, Trisi et al.18 studied the effects of osseodensification on Cortex® implants installed over sheep iliac crest. They found higher removal torque values for the OD protocol compared with a control group. One problem of their work was that the experimental group used bigger diameter implants (5.0 × 10 mm) compared with the control group (3.8 × 10 mm), having around 26% more bone contact area than the control.
Considering ISQ values, some authors find a better performance of OD protocol, but others not. Even there is data that shows better ISQ values and insertion torque for implants inserted with under-drilling compared to OD protocol.19 However, the authors conclude that OD was the only technique that effectively changes the bone density around implants.19 Huwais and Meyer did not find any difference between ISQ values using OD protocol compared to standard and clockwise Densah® burs.8 Conversely, we found significant ISQ values difference between OD protocol (TG) and CG. The reason could be our higher number of observations and fewer comparisons groups, showing more clearly, the possible difference between experimental groups. All the above mentioned preclinical studies used a smaller sample size per group than our current research.
A possible confusion factor that could explain the higher primary implant stability showed in our TG is that OD technique could under-drill the implant bed. In this research, both last drill used for test and control groups, before implant placement, were practically the same diameter (see materials and methods section), eliminating the under-drilling explanation about the results obtained. Taking into account the literature that shows a higher density of bone next to the implant using OD, we hypothesized that our results could be due to bone autografting.8
Scientific literature shows a series of different advantages gained by the osseodensification protocol proposed by Huwais. These can sum up as mechanics (higher primary stability, less micromovement), anatomic (more bone volume available after osteotomy preparation), and biologic (faster osseointegration process and more bone-implant contact) advantages.8,14,17,18 As to bone particles resulting from bone condensation, these would act as autologous grafting material with constant remodeling and osteogenic potential, forming bridges between the osteotomy and the implant surface.17,18 Further, this technique can produce safe and controlled bone expansion by the gradual and progressive compaction, taking advantage of the viscoelastic properties of soft bone without bone mass loss and complications described for classic bone expansion techniques.20
Clinical studies are less common, showing high success and survival percentage (>96.9%) of dental implants treated with OD technique during a short follow up period (up to 6 months).21, 22, 23 There is an agreement between those reports about the reduced morbidity and complications of OD protocol compared with other techniques. There is also a trend of higher primary implant stability using OD protocol compared with standard drilling. Also, there is a report of sinus lift using OD drills showing significant bone gain with trans-alveolar access.23 Nevertheless, clinical studies are case series mainly, and there is an essential lack of well designed randomized controlled clinical trials.
We utilized an ex vivo model using pig tibia bone that resembles low-density bone with homogenous cancellous and absence of cortical similar to class III-IV human bone. This approach allowed us to work with a higher number of observations, and with bone conditions similar to the clinical ones. Another advantage of our work is the use of BioHorizons® tapered internal implants, which have not been proven jet with OD technique. On the other hand, there are some disadvantages related to the less clinical validity of ex vivo works and the absence of osseointegration and follow up data. We believe that this work is crucial for continuing with randomized controlled clinical trials using Densah® osseodensification protocol and BioHorizons® implants.
5. Conclusions
Under this preclinical ex vivo design, the osseodensification Densah® protocol showed higher insertion, removal torques, and ISQ values on low-density bone compared to standard drilling recommended for BioHorizons® tapered internal implants. This information justified the need for good design randomized controlled trials and long term observational studies that supports the use of osseodensification as a standard treatment.
Ethics
The scientific board of the Faculty of Dentistry (Universidad de los Andes) approved the study protocol since no animal was harmed or euthanized during the study development.
Declaration of competing interest
There is no conflict of interest in this publication. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Felipe Cáceres, Email: fcaceres@uandes.cl.
Cristian Troncoso, Email: ctroncosolara@gmail.com.
Ramón Silva, Email: ramonsilva.barrios@gmail.com.
Nelson Pinto, Email: nelsonpinto@miuandes.cl.
References
- 1.Chen J., Cai M., Yang J., Aldhohrah T., Wang Y. Immediate versus early or conventional loading dental implants with fixed prostheses: a systematic review and meta-analysis of randomized controlled clinical trials. J Prosthet Dent. 2019;122(6):516–536. doi: 10.1016/j.prosdent.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont (IJP) 1998;11(5):491–501. [PubMed] [Google Scholar]
- 3.Javed F., Ahmed H.B., Crespi R., Romanos G.E. Role of primary stability for successful osseointegration of dental implants: factors of influence and evaluation. Interv Med Appl Sci. 2013;5(4):162–167. doi: 10.1556/IMAS.5.2013.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ivanoff C.J., Gröndahl K., Bergström C., Lekholm U., Brånemark P.I. Influence of bicortical or monocortical anchorage on maxillary implant stability: a 15-year retrospective study of Brånemark System implants. Int J Oral Maxillofac Implants. 2000;15(1):103–110. [PubMed] [Google Scholar]
- 5.Campos F.E., Gomes J.B., Marin C. Effect of drilling dimension on implant placement torque and early osseointegration stages: an experimental study in dogs. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2012;70(1):e43–50. doi: 10.1016/j.joms.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Summers R.B. A new concept in maxillary implant surgery: the osteotome technique. Compend Newtown Pa. 1994;15(2):154–156. 152. 158 passim; quiz 162. [PubMed] [Google Scholar]
- 7.Boustany C.M., Reed H., Cunningham G., Richards M., Kanawati A. Effect of a modified stepped osteotomy on the primary stability of dental implants in low-density bone: a cadaver study. Int J Oral Maxillofac Implants. 2015;30(1):48–55. doi: 10.11607/jomi.3720. [DOI] [PubMed] [Google Scholar]
- 8.Huwais S., Meyer E.G. A novel osseous densification approach in implant osteotomy preparation to increase biomechanical primary stability, bone mineral density, and bone-to-implant contact. Int J Oral Maxillofac Implants. 2017;32(1):27–36. doi: 10.11607/jomi.4817. [DOI] [PubMed] [Google Scholar]
- 9.Huwais S. Fluted osteotome and surgical method for use. January 3, 2013. https://patents.google.com/patent/US20130004918A1/en?oq=US2013%2f0004918
- 10.Huwais S. Enhancing implant stability with osseodensification— a case report with 2-year follow-up Implant Practice US. Implant Practice US. February 16, 2015. https://www.implantpracticeus.com/case-studies/enhancing-implant-stability-osseodensification-case-report-2-year-follow/
- 11.BioHorizons Tapered HD surgical system brochure. November 2018. https://vsr.biohorizons.com/GetDocument?DocumentId=61778
- 12.Versah . October 2019. Densah® bur & Versah® guided surgery system instructions for use. Brochure. [Google Scholar]
- 13.Norton M.R. The influence of low insertion torque on primary stability, implant survival, and maintenance of marginal bone levels: a closed-cohort prospective study. Int J Oral Maxillofac Implants. 2017;32(4):849–857. doi: 10.11607/jomi.5889. [DOI] [PubMed] [Google Scholar]
- 14.Al-Sabbagh M., Eldomiaty W., Khabbaz Y. Can osseointegration Be achieved without primary stability? Dent Clin North Am. 2019;63(3):461–473. doi: 10.1016/j.cden.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Waechter J., Leite F.R., Nascimento G.G., Carmo Filho L.C., Faot F. The split crest technique and dental implants: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2017;46(1):116–128. doi: 10.1016/j.ijom.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 16.Lopez C.D., Alifarag A.M., Torroni A. Osseodensification for enhancement of spinal surgical hardware fixation. J Mech Behav Biomed Mater. 2017;69:275–281. doi: 10.1016/j.jmbbm.2017.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lahens B., Neiva R., Tovar N. Biomechanical and histologic basis of osseodensification drilling for endosteal implant placement in low density bone. An experimental study in sheep. J Mech Behav Biomed Mater. 2016;63:56–65. doi: 10.1016/j.jmbbm.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Trisi P., Berardini M., Falco A., Podaliri Vulpiani M. New osseodensification implant site preparation method to increase bone density in low-density bone: in vivo evaluation in sheep. Implant Dent. 2016;25(1):24–31. doi: 10.1097/ID.0000000000000358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delgado-Ruiz R., Gold J., Somohano Marquez T., Romanos G. Under-drilling versus hybrid osseodensification technique: differences in implant primary stability and bone density of the implant bed walls. Materials. 2020;13(2):390. doi: 10.3390/ma13020390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jimbo R., Tovar N., Marin C. The impact of a modified cutting flute implant design on osseointegration. Int J Oral Maxillofac Surg. 2014;43(7):883–888. doi: 10.1016/j.ijom.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 21.Johnson E., Huwais S., Olin P. Presentation at the American Academy of Implant Dentistry 63rd Annual Meeting. 2014. Osseodensification increases primary implant stability and maintains high ISQ values during first six weeks of healing. Conf Poster. [Google Scholar]
- 22.Gaspar J., Esteves T., Gaspar R., Rua J., Mendes J.J. Osseodensification for implant site preparation in the maxilla- a prospective study of 97 implants. Poster. Clin Oral Implants Res. 2018;29(S17) doi: 10.1111/clr.48_13358. 163-163. [DOI] [Google Scholar]
- 23.Neiva R., Tanello B., Duarte W., Silva F. Osseodensification crestal sinus floor elevation with or without synthetic and resorbable calcium phosphosilicate putty. Clin Oral Implants Res. 2018;29(S17) doi: 10.1111/clr.331_13358. 446-446. [DOI] [Google Scholar]