Dear Editor,
In our recent publication, we have highlighted that hyperglycemia in patients without known diabetes had a worse impact on COVID-19 outcome than hyperglycemia in patients with known diabetes [1]. The adverse prognostic role of hyperglycemia without diabetes and new-onset diabetes is extremely consistent in the literature [2], [3], [4], [5], [6].
Commenting upon our paper, Dr. Li has elegantly argued that at least part of the effect of hyperglycemia on COVID-19 outcome may be confounded by glucocorticoid therapy being used in patients with more severe forms of disease [5], [7]. This is particularly important because glucocorticoid therapy is being recommended for COVID-19 patients needing invasive ventilation, especially in the intensive care unit [8].
There are several reasons why we believe that glucocorticoid therapy was not affecting our findings.
First, we used admission glucose levels to define diabetes status and the degree of hyperglycemia was always referred to laboratory values closest to the hospital admission date. Therefore, even if more patients with newly-diagnosed diabetes have received glucocorticoids during the hospital stay, this did not affect our definition of diabetes and glucose levels collected before initiation of such therapy.
Rather, we were concerned that admission hyperglycemia could be due to pre-hospital glucocorticoid therapy because some patients could be treated with glucocorticoids at home before requiring hospitalization. In fact, in multivariable model 2, we adjusted for sex, age and pre-existing conditions or pre-hospital medications associated with COVID-19 severity in model 1, including glucocorticoids. As reported also in this model, the association between hyperglycemia and COVID-19 severity was confirmed.
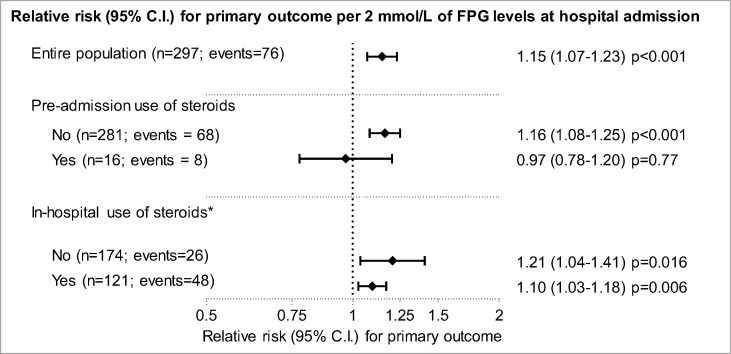
Finally, to better clarify this issue, we now present a new analysis, where the effect of hyperglycemia on COVID-19 outcome is shown according to pre-admission and in-hospital use of glucocorticoids.
Fig. 1 shows that adverse outcome was significantly more common every 2 mmol of higher admission fasting plasma glucose also when the analyses was restricted to patients without pre-hospital use of glucocorticoids. Conversely, the analyses among those using glucocorticoids, strongly limited by the small sample size (n = 16), yielded a null association between hyperglycemia and COVID-19 severity with very large confidence interval (overlapping with that of other groups). However, the lack of the association in this group would be in line with the notion that pre-admission glucocorticoids caused hyperglycemia upon admission and were a proxy of severity, thereby nullifying the prognostic effect of hyperglycemia. On the other side, the effect of hyperglycemia on COVID-19 outcome was statistically significant in both patients with and in those without in-hospital use of glucocorticoids.
Fig. 1.
Association between admission fasting plasma glucose (FPG) and COVID-19 severity by use of glucocorticoids before or during hospitalization. Estimates were adjusted for age and sex. *Data on in hospital-use of steroids was not available for two patients.
It should be noted that the frequent use of glucocorticoids among people with newly-diagnosed diabetes may exacerbate hyperglycemia. If hyperglycemia truly plays a negative role on COVID-19 outcomes, glucocorticoids should be used carefully in these patients [9]. In fact, iatrogenic hyperglycemia may counterbalance the benefits of glucocorticoid therapy, such that anti-inflammatory drugs devoid of such effect may be preferred.
Disclosures
None.
Acknowledgments
Acknowledgements
None.
Data availability
Original data are available from the corresponding author at a reasonable request.
Funding
The study was supported by the University of Padova (CA.RI.PA.RO. Grant COVIDIMED).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contribution statement
Study design: MLM, GPF, FB, PF, AA. Data collection and analysis: GPF, MLM, BMB, AM, LB, MCC, MV, ES, GA, SP, FF, DF, LR, GV, SM, GC, FG, ST, AMC, AV, PF, RV, AA. Manuscript writing: GPF, MLM, FB. Manuscript revision: AM, PF, RV, AA. All authors approved the final version of the manuscript.
References
- 1.Fadini G.P., Morieri M.L., Boscari F., Fioretto P., Maran A., Busetto L. Newly-diagnosed diabetes and admission hyperglycemia predict COVID-19 severity by aggravating respiratory deterioration. Diab Res Clin Pract. 2020;168:108374. doi: 10.1016/j.diabres.2020.108374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh A.K., Singh R. Hyperglycemia without diabetes and new-onset diabetes are both associated with poorer outcomes in COVID-19. Diab Res Clin Pract. 2020;108382 doi: 10.1016/j.diabres.2020.108382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fadini G.P., Morieri M.L., Longato E., Avogaro A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest. 2020;43:867–869. doi: 10.1007/s40618-020-01236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu B., Jin S., Wu L., Hu C., Wang Z., Bu L. J-shaped association between fasting blood glucose levels and COVID-19 severity in patients without diabetes. Diab Res Clin Pract. 2020;168:108381. doi: 10.1016/j.diabres.2020.108381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ceriello A. Hyperglycemia and COVID-19: what was known and what is really new? Diab Res Clin Pract. 2020;108383 doi: 10.1016/j.diabres.2020.108383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu S.P., Zhang Q., Wang W., Zhang M., Liu C., Xiao X. Hyperglycemia is a strong predictor of poor prognosis in COVID-19. Diab Res Clin Pract. 2020;167:108338. doi: 10.1016/j.diabres.2020.108338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li G. Inpatient use of glucocorticoids may mediate the detrimental effect of new onset hyperglycemia on COVID 19 severity. Diab Res Clin Pract. 2020;168 doi: 10.1016/j.diabres.2020.108441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horby P., Lim W.S., Emberson J.R., Mafham M., Bell J.L., Linsell L. Dexamethasone in hospitalized patients with covid-19 – preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korytkowski M., Antinori-Lent K., Drincic A., Hirsch I.B., McDonnell M.E., Rushakoff R. A pragmatic approach to inpatient diabetes management during the COVID-19 pandemic. J Clin Endocrinol Metab. 2020;105 doi: 10.1210/clinem/dgaa342. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Original data are available from the corresponding author at a reasonable request.