Abstract
Objective
To explore the effect of COVID-19 outbreak on the treatment time of patients with ST-segment elevation myocardial infarction (STEMI) in Hangzhou, China.
Methods
We retrospectively reviewed the data of STEMI patients admitted to the Hangzhou Chest Pain Center (CPC) during a COVID-19 epidemic period in 2020 (24 cases) and the same period in 2019 (29 cases). General characteristics of the patients were recorded, analyzed, and compared. Moreover, we compared the groups for the time from symptom onset to the first medical contact (SO-to-FMC), time from first medical contact to balloon expansion (FMC-to-B), time from hospital door entry to first balloon expansion (D-to-B), and catheter room activation time. The groups were also compared for postoperative cardiac color Doppler ultrasonographic left ventricular ejection fraction (LVEF),the incidence of major adverse cardiovascular and cerebrovascular events (MACCE),Kaplan-Meier survival curves during the 28 days after the operation.
Results
The times of SO-to-FMC, D-to-B, and catheter room activation in the 2020 group were significantly longer than those in the 2019 group (P < 0.05). The cumulative mortality after the surgery in the 2020 group was significantly higher than the 2019 group (P < 0.05).
Conclusion
The pre-hospital and in-hospital treatment times of STEMI patients during the COVID-19 epidemic were longer than those before the epidemic. Cumulative mortality was showed in Kaplan-Meier survival curves after the surgery in the 2020 group was significantly different higher than the 2019 group during the 28 days.The diagnosis and treatment process of STEMI patients during an epidemic should be optimized to improve their prognosis.
Keywords: COVID-19, Acute ST-segment elevation myocardial infarction, Treatment time, 2019-nCoV, SARS-CoV-2
1. Introduction
Multiple cases of pneumonia patients, infected with a novel coronavirus (SARS-CoV-2), were discovered in Wuhan City, Hubei, China, since December 2019 [1,2]. With the spread of the epidemic, confirmed cases were found in other provinces in China and most countries around the world. As of May 10, 2020, there were 3,917,366 confirmed cases worldwide, and 274,361 deaths, far exceeding the number of people affected by atypical pneumonia or the Middle East respiratory syndrome (MERS) [3,4]. The National Health Commission of China quickly announced the disease as a Class B infectious disease, as stipulated in the Chinese law on the Prevention and Control of Infectious Diseases. It also required the activation of preventive and control measures of Class A infectious diseases [5].
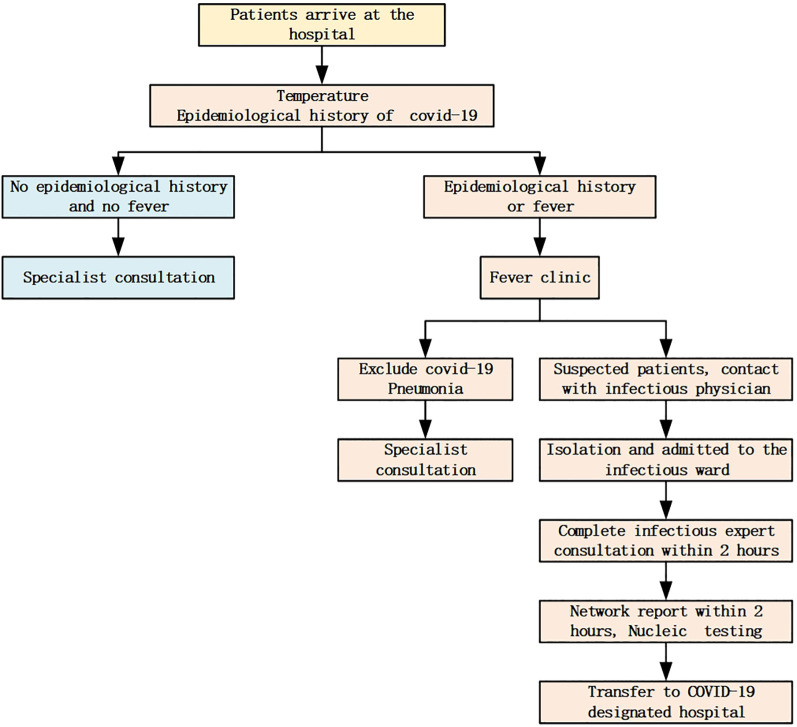
On January 23, 2020, the closure of Wuhan City was announced. Before this, on January 20, 2020, the Hangzhou Chest Pain Center (CPC) has formulated a procedure for patient consultation under the preventive and control measures of COVID-19 (Fig. 1 ). The epidemic occurred during the transition from winter to spring, a period of a high incidence of cardiovascular disease. As is well known, cardiovascular diseases are the leading cause of adult death in China [6]. Acute myocardial infarction is a disease that requires race against time, with treatment that should be administered within minutes [7]. On January 27, 2020, the Hangzhou CPC developed an ST-segment elevation myocardial infarction (STEMI) treatment process for this special period (Fig. 2 ), striving to prevent and control the epidemic while optimizing the treatment. This action followed the STEMI merger strategy for the management of SARS-CoV-2 infection in the People's Hospital of Wuhan University [8]. As part of the improved cooperation with the hospital, we carried out fever diagnoses and disease treatment.
Fig. 1.
The patient consultation process during the control of the COVID-19 outbreak in Hangzhou CPC.
Fig. 2.
The treatment process of suspected or confirmed COVID-19 patients with STEMI.
However, we hypothesized that the COVID-19 epidemic might have interfered with diagnosing and treating acute myocardial infarction. To clarify this issue, we performed a retrospective study comparing STEMI patients at the Hangzhou CPC during the COVID-19 epidemic (January 20 to April 20, 2020) with those during the corresponding period in 2019. We aimed to explore the impact of COVID-19 on the treatment time of STEMI patients and provide a solid base in support of standardizing the treatment process of STEMI patients during an epidemic situation such as COVID-19.
2. Materials and methods
2.1. Research subjects
Clinical data of STEMI patients who visited the Hangzhou CPC were collected. Inclusion criteria: (1) At least one of the following persistent chest pain-related symptoms, including ischemic chest pain onset <12 h, chest pain did not pass within 24 h, or hemodynamic instability; (2) Electrocardiogram (ECG) showing ≥2 leads ST-segment elevation of >1 mV or newly emerged left bundle branch block with elevated myocardial markers that meets STEMI diagnostic criteria [9]; (3) Patients that agreed to undergo coronary angiography (CAG) examination and percutaneous coronary intervention (PCI) treatment, or such agreement was provided by the accompanying family members. Exclusion criteria: (1) Patients who died before the CAG and revascularization treatment; (2) Patients who underwent thrombolysis or autolysis before hospitalization (3) Patients who refused to undergo CAG examination and PCI treatment.
2.2. Grouping method
STEMI patients treated between January 20 and April 20, 2020, were assigned to the 2020 group. STEMI patients treated during the same period in 2019 were assigned to the 2019 group. The time nodes were as recorded in the dedicated institutional database.
2.3. Observation indicators
General characteristics included age, sex, drinking history, smoking history, hypertension, diabetes, hypercholesterolemia, obesity, family history of coronary heart disease, history of myocardial infarction, location of myocardial infarction, Killip classification, and left ventricular ejection fraction (LVEF). Time and prognostic indicators included symptom onset to the first medical contact (SO-to-FMC), time from the first medical contact to the first electrocardiogram (FMC-to-ECG), time from first medical contact to first balloon expansion (FMC-to-B), time from hospital door entry to first balloon expansion (D-to-B), and catheter room activation time; major adverse cardiovascular and cerebrovascular events (MACCE) occurring during the 28 days after surgery were also collected. MACCE events included non-fatal myocardial infarction, cardiac death, target vessel revascularization, and stroke. Cardiac death refers to death due to myocardial ischemia, leading to cardiac arrest before the loss of other functions; target vessel revascularization refers to lesions in the original stent area and the coronary arteries within 5 mm from both ends of such stent. It also includes lesions in the area outside the target lesion, located in the main branch corresponding to the revascularized coronary artery; stroke refers to cerebral hemorrhage or cerebral infarction [10]. This study was approved by the Human Study Ethics Committee of the Affiliated Hospital of Hangzhou Normal University.
2.4. Statistical analysis
Data analysis was performed using the R program (v3.60). An independent sample t-test was used for group comparisons. The Kaplan-Meier survival curve was used to estimate the survival rate. Wilcoxon signed-rank test was used to compare the survival rate between the two groups. Continuous variables are presented as mean ± standard deviation. Differences with P < 0.05 were considered statistically significant.
3. Results
3.1. Comparison of the patients' characteristics and general clinical data between the two groups
A total of 24 patients in the 2020 group and 29 patients in the 2019 group were showed in Table 1 . The baseline data and risk factors relating to coronary heart disease were analyzed in both groups.There were no statistical significance in terms of age,sex,drinking history, smoking history, hypertension, diabetes, hypercholesterolemia, obesity, and family history of coronary heart disease in the two groups. With one patient in each group having a history of myocardial infarction, the difference was insignificant. The groups also did not differ in the myocardial infarction location, Killip classification, and LVEF.
Table 1.
Comparison of general characteristics between the two groups.
| 396,040 | 28-02-2019 | STEMI | Perforation after interval, death | 2 |
| 395,836 | ######### | STEMI | 0 | 10 |
| 395,983 | ######### | STEMI | 0 | 8 |
| 393,535 | ######### | STEMI | pericardial tamponade, cardiogenic shock | 17 |
| 393,682 | ######### | STEMI | 0 | 6 |
| 392,970 | ######### | STEMI | death on the second day after PCI | 12 |
| 393,973 | ######### | STEMI | 0 | 7 |
| 394,267 | ######### | STEMI | 0 | 7 |
| 394,242 | ######### | STEMI | malignant arrhythmia, atrioventricular block | 12 |
| 394,155 | ######### | STEMI | malignant arrhythmia, defibrillation 18 times | 21 |
| 394,033 | ######### | STEMI | 0 | 9 |
| 394,144 | ######### | STEMI | 0 | 6 |
| 394,799 | ######### | STEMI | 0 | 12 |
| 346,499 | ######### | STEMI | 0 | 8 |
| 395,079 | ######### | STEMI | 0 | 7 |
| 395,651 | ######### | STEMI | influenza in the hospital | 28 |
| 395,642 | ######### | STEMI | enlarged heart, heart failure | 12 |
| 395,509 | ######### | STEMI | 0 | 8 |
| 394,329 | ######### | STEMI | gastrointestinal bleeding, platelet suppression, plasma transfusion | 15 |
| 394,086 | ######### | STEMI | 0 | 9 |
| 397,618 | ######### | STEMI | 0 | 6 |
| 398,040 | ######### | STEMI | small amount of fluid in the pericardial cavity | 13 |
| 398,831 | ######### | STEMI | apical ventricular aneurysm, small amount of pericardial effusion | 22 |
| 398,705 | ######### | STEMI | 0 | 18 |
| 400,081 | ######### | STEMI | 0 | 12 |
| 399,544 | ######### | STEMI | 0 | 9 |
| 400,968 | ######### | STEMI | 0 | 8 |
| 401,508 | ######### | STEMI | 0 | 9 |
| 401,755 | ######### | STEMI | 0 | 8 |
3.2. Comparison of the treatment times and prognosis between the two groups
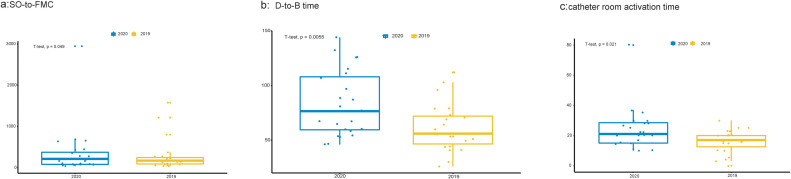
The average SO-to-FMC time was 319.4 ± 89.5 min in the 2020 group and 261.5 ± 87.3 min in the 2019 group (P = 0.049; Fig. 3a). The average D-to-B time in the 2020 and 2019 groups was 83.3 ± 29.7 and 61.1 ± 21.9 min, respectively (P = 0.006 Fig. 3b); The average catheter room activation time for patients in the 2020 group was 24.2 ± 14.1 min, and it was 16.1 ± 7.7 min in the 2019 group (P = 0.021; Fig. 3c). The results show that all three time measures were longer in 2020.
Fig. 3.
(a) Comparison of symptom onset to the first medical contact (SO-to-FMC) time between the groups; (b) Comparison of the time from hospital door entry to first balloon expansion (D-to-B) between the groups; (c) Comparison of catheter room activation time between the groups.
3.3. Comparison of MACCE and survival analysis between the groups
The longest follow-up time in the two groups was 28 days. Data on major adverse cardiovascular and cerebrovascular events (MACCE) occurring during the 28 days after the surgery were collected. There were three MACCE in the 2020 group, two deaths from cardiogenic shock, one death frommalignant arrhythmia; there were two MACCE in the 2019 group, one death from posterior septal perforation, and one death from malignant arrhythmia. The Kaplan-Meier survival curves for the two groups are shown in Fig. 4 . The cumulative mortality after the surgery in the 2020 group was significantly higher than the 2019 group (P = 0.028).
Fig. 4.
Kaplan-Meier survival curves for the two groups.
4. Discussion
Acute myocardial infarction can lead to sudden death, and continuous myocardial ischemia can eventually develop into heart failure [11]. Studies have shown that early reperfusion therapy is the key to the successful treatment of STEMI. The mortality rate within one hour of successful reperfusion in STEMI patients is only 1.6% [12]. With every 30-min increase in the time to reperfusion, the 1-year mortality rate increases by 7.5% [13,14]. Therefore, it is particularly important to shorten the reperfusion time for STEMI patients. The STEMI rescue process includes pre-hospital and in-hospital segments. The main evaluation indicator of pre-hospital rescue in the Chinese CPC evaluation system is the SO-to-FMC time, while the evaluation indicators of in-hospital rescue are mainly the D-to-B and catheter room activation times. In 2019, the average SO-to-FMC time in 763 standard CPC in China was 310.96 min. The D-to-B time required a monthly average of fewer than 90 min, and a catheter room activation time of fewer than 30 min [15]. The Hangzhou CPC has reached the above assessment indicators. However, through our comparative study, it was found that the above-mentioned rescue times during the COVID-19 epidemic in 2020 were longer than those in 2019. The detailed performance was as follows: the average SO-to-FMC time of the 2020 group was 319.4 min, which is significantly longer than the 261.478 min of the 2019 group; the average D-to-B time of the 2020 group was 83.3 min, which is significantly longer than the 61.1 min of the 2019 group; The average catheter room activation time for the 2020 group was 24.2 min, which is significantly longer than the 16.1 min of the 2019 group. Moreover, these prolongations increased the probability of an MACCE occurrence within the first 28 days after the operation. This is a grave consequence, requiring an urgent retrospective analysis and formulation of new guidelines.
Based on these results, we think that the reasons for the delay in STEMI treatment times can be summarized along the following lines. First, patients delayed their visit to the hospital because they feared becoming infected with SARS-CoV-2. This delay resulted in a significant prolongation of the SO-to-FMC time. During the epidemic, ordinary patients with non-emergency cardiovascular diseases were advised to avoid hospital admission as much as possible. After the epidemic was contained, they were admitted to the hospital for treatment. The patients, especially the elderly, often cannot distinguish between emergency and non-emergency events. Moreover, the patients were extremely anxious about the spread of COVID-19, so they delayed seeking medical help, and attempted to relieve the chest pain symptoms by taking quick-acting rescue pills or other drugs. These patients did not call for help until it was already intolerable. Second, after the patients have arrived at the hospital gates, the FMC-to-ECG and D-to-B times were further prolonged because of the COVID-19 screening of the patient and the accompanying family members during the epidemic. They had to be screened for body temperature and were asked for epidemiological history before entering the hospital. The epidemiologic history included information about visiting Wuhan City and its surrounding areas within the past 14 days, other travel histories, community or living history, contact with COVID-19 patients (nucleic acid test-positive) within the past 14 days, and contact with patients with fever or respiratory symptoms from Wuhan and the surrounding areas, or from communities with reported cases within the past 14 days. Information on sexually-transmitted illnesses was also gathered. Application of the health codes in Hangzhou required that anybody entering the hospital would complete this epidemiological history and show a healthy green code at the entrance. After entering the emergency department, the patients had to go through a lung CT examination to exclude COVID-19 infection before entering the catheterization room. The above process caused a significant delay in the D-to-B time. Third, the medical staff, especially at the emergency department, paid much attention to the screening of COVID-19 patients, ignoring, to some extent, the assessment of patients with chest pain symptoms. As a result, patients whose symptoms were not too evident at the beginning, or only had chest tightness, had to wait before starting the diagnosis and treatment process, resulting in an extension of the D-to-B time.
The Hangzhou CPC has devised the following improvement plan based on the study's results and the analysis of the above reasons. First, while preventing the spread of the epidemics, it is necessary to educate the medical staff in the network and community hospitals associated with the CPC of our hospital. Furthermore, it is necessary to carry out multimedia education of the general public. Using WeChat and similar social media, news headlines, etc., it is possible to attract people's attention through specific case reports, thus shortening the SO-to-FMC time; Second, for the in-hospital treatment process, the time of temperature measurement can be shortened by installing an infrared thermometer. Third, the accompanying family members can prepare the health code and green code in advance and present them at admission. This can shorten the epidemiological history investigation time. Fourth, it is also possible to reduce the missed diagnosis and delayed events by training the medical staff in the emergency department on how to handle patients with chest pain. Finally, the lung CT examination should be faster for these patients, thereby shortening the D-to-B time. We believe that through optimization of the above measures and procedures, the total treatment time for STEMI patients could be shortened, and their prognosis could thus be improved.
Funding
The presented study were supported by Hangzhou Science and Technology Bureau Fund (No. 20191203B96; No. 20191203B105), Zhejiang Medicine and Health Technology Project (No. 2020KY716) and Hangzhou City Health Science and Technology Project (0020190887).
Declaration of Competing Interest
The authors have no conflicts of interest or financial ties to disclose.
Acknowledgment
Our team would like to express our sincere gratitude to the medical staff all over the world who are fighting on the front lines against COVID-19.
References
- 1.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jin Y.H., Cai L., Cheng Z.S., Cheng H., Deng T., Fan Y.P., et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res. 2020;7(1):4. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li J.Y., You Z., Wang Q., et al. The epidemic of 2019-novel-coronavirus (2019-nCoV) pneumonia and insights for emerging infectious diseases in the future. Microbes Infect. 2020;22(2):80–85. doi: 10.1016/j.micinf.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Word Heath Organization Coronavirus Disease (COVID-2019) Situation Reports. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/;
- 5.Lin L., Li T.S. Interpretation of “Guidelines for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infection by the National Health Commission (Trial Version5)”. Chin Med J. 2020;100(11):805–807. doi: 10.3760/cma.j.cn112137-20200205-00199. [DOI] [PubMed] [Google Scholar]
- 6.Hu Shengshou, Yang Yuejin, Zheng Zhe, et al. Summary of "Chinese Cardiovascular Disease Report 2018". Chin J Circ. 2019;034(003):209–220. [Google Scholar]
- 7.Viana M., Laszczyńska O., Araújo C., et al. Patient and system delays in the treatment of acute coronary syndrome. Rev Port Cardiol. 2020;39(3):123–131. doi: 10.1016/j.repc.2019.07.007. [published online ahead of print, 2020 May 6] [DOI] [PubMed] [Google Scholar]
- 8.Hubei Province Acute Cardiovascular Disease Medical Treatment Center . Hubei Heart Treatment Center; 2020. Suggestions on management strategies for ST-segment elevation acute myocardial infarction (STEMI) combined with novel coronavirus infection [S]http://www.365heart.com/wap1/newwap1/shownews.asp?id=143198 [in Chinese] [Google Scholar]
- 9.Ibanez B., James S., Agewall S., et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39(2):119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 10.Wei T.F., Zhao B., Liu P.L., et al. Impact of symptom onset to first medical contact time on the prognosis of patients with acute ST-segment elevation myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi. 2017;45(5):393–398. doi: 10.3760/cma.j.issn.0253-3758.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Dharma S., Dakota I., Andriantoro H., et al. Association of gender with clinical outcomes of patients with acute ST-segment elevation myocardial infarction presenting with acute heart failure. Coron Artery Dis. 2020 Apr 22 doi: 10.1097/MCA.0000000000000892. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y., Yu B., Han Y., et al. Protocol of the China ST-segment elevation myocardial infarction (STEMI) Care Project (CSCAP): a 10-year project to improve quality of care by building up a regional STEMI care network. BMJ Open. 2019;9(7) doi: 10.1136/bmjopen-2018-026362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vogel B., Claessen B.E., Arnold S.V., et al. ST-segment elevation myocardial infarction. Nat Rev Dis Primers. 2019;5(1):39. doi: 10.1038/s41572-019-0090-3. [DOI] [PubMed] [Google Scholar]
- 14.Liu P., Lin F., Zhang J.X., et al. Effects of target value management for quality control indexes in chest pain center on efficiency and effectiveness of in-hospital treatment for STEMI patients. Chin J Emerg Med. 2019;28(4):498–503. doi: 10.3760/cma.j.issn.1671-0282.2019.04.020. [DOI] [Google Scholar]
- 15.2019 China Chest Pain Center Quality Control Report. 2019. http://www.chinacpc.org/download/tool/e0de489277cb51dae9b927203a617a76.pdf