1. INTRODUCTION
In the 1970s, DNA was shown to bind to type I, II, and IV collagens. Later in the 1990s, DNA complexed with collagen was shown to form self-assembled aggregates ranging from nanoparticles to micron sized fibers [1–4]. These interactions are ubiquitous for nucleic acids and; in fact, the complex protects DNA from enzymatic attack [4–8]. The physico-chemical properties of long (>1000 base pairs), random sequence double-stranded DNA-collagen complexes have been characterized by a number of groups, which has been used to inform the main application of these complexes, gene transfection [9–13]. Nucleic acid-collagen complexes (NACCs) for gene delivery applications use NACC nanoparticle aggregates to promote endocytosis and uptake of the gene cargo. Likewise, collagen scaffolds complexed with plasmid DNA have been used for the same purpose [8,14,15]. While double-stranded DNA-collagen interactions have been studied, few works have characterized the complexation of collagen and single-stranded DNA (ssDNA); especially, for ssDNA less than one hundred nucleotides in length. This size range is important for another structural form of nucleic acids, aptamers. These engineered single-stranded nucleic acid sequences are finding increased use in biomedical applications as both agonists and antagonists of biological processes, sensors, and therapies [16,17]. Our group has shown that short (15–90 nucleotides), monodisperse, random sequence ssDNA binds and forms ssDNA-collagen complex microfibers of disperse size. Hierarchical, fibrous architectures of biological macromolecules are necessary for regulating cellular phenotype [18]. Our NACC fibers demonstrated promise for tissue engineering applications by mediating healthy vascular cell behavior [19]. Together, NACCs using ssDNA could be a next-generation, multimodal biomaterial because of their tunable composition and structure.
Likewise, DNA non-specifically binds with calcium phosphate. DNA-calcium phosphate complexes have been utilized for gene delivery using calcium phosphate nanoparticles coated with plasmid DNA [20–23]. Beyond gene delivery, calcium phosphates, are used in bone substitutes and bone tissue engineering. Hydroxyapatite is the calcium phosphate crystal phase in the body, which in bone is organized among collagen fibrils. Paramount to the challenges facing bone tissue engineering is recapitulating this organization [24]. Biomimetic approaches have achieved aligned, intrafibrillar hydroxyapatite mineralization of collagen gels utilizing polyanionic species, namely polyaspartate [25–29]. This method relies on anionic species to form an amorphous precursor phase of calcium phosphate, which then can penetrate the D-spacings of collagen fibrils by capillary action, termed the polymer-induced liquid-precursor (PILP) process [26]. Coincidentally, DNA is a highly polyanionic biomacromolecule and extracellular DNA can be found in low abundance in native, intact bone [30]. For this reason, it has been hypothesized for extracellular DNA to contribute along with several other non-collagenous proteins in the biomineralization of hydroxyapatite in bone [24,30,31]. Ultimately, few groups have combined all three components (DNA, collagen, and calcium phosphate) together, mostly for improving gene delivery efficiency; however, these complexes have not been applied as strategies for bone tissue engineering [32–34].
Herein, we report for the first time the combination of short, monodisperse ssDNA and collagen to form mineralized self-assembled nucleic acid-collagen complex (NACC) fibers and 3D gels. These fibers and gels have promise not only as osteoconductive coatings and implants, in vitro 3D bone and calcified tissue models, but as coatings and scaffolds for any tissue using this simple, versatile biomaterial platform.
2. MATERIALS AND METHODS
2.1. NACC Fiber and Gel Synthesis.
Previously, we have shown that self-assembled ssDNA-collagen complex fibers are dependent on ssDNA sequence length and the ratio of ssDNA to collagen in solution [19]. NACC self-assemblies were synthesized by mixing different volume fractions (0 – 100%) of 0.3 to 3.0 mg/mL rat tail tendon type I collagen (Corning) with either 1 to 10 μm of a random sequence of ssDNA (5’– TAA AAC GCG CTT AAG CTG GTG TTA CTC GAG CGG TCT TCT A–3’) (Integrated DNA Technologies). 18 MΩ-cm at 25 °C deionized water was used for all dilutions, which was sterilized by autoclaving. The collagen was diluted to the desired concentration from its high concentration of ~10 mg/mL in 0.02N acetic acid to the working concentrations using sterile deionized water. The acetic acid concentration of the collagen working concentrations thus ranged from ~0.6 mN to ~6 mN. The ssDNA was reconstituted in sterile deionized water and diluted to the working concentrations using more sterile deionized water. The ssDNA sequence has a molecular weight of 12,302.0 g/mol and a GC content of 47.5%. NACCs spontaneously formed upon mixing and were incubated at room temperature overnight followed by storage in solution at 4 °C until needed.
2.2. ssDNA-Collagen Binding Assay.
The amount of ssDNA in the NACC self-assembled fibers for different volume fractions of type I collagen and ssDNA oligomer was assessed fluorometrically by measuring the intensity of a fluorescent DNA stain. Solutions of different volume fractions were diluted at a 1:2 volume ratio of fiber solution to SYBR Safe DNA stain (Invitrogen). The stain concentrate was diluted first at a 1:10,000 volume ratio in deionized water. Then the mixtures were incubated protected from light for 30 minutes at room-temperature. After incubation, the mixtures were centrifuged at 2000g for five minutes. Supernatant was plated in duplicate into black walled 96 well microplates and fluorescence intensity was measured by exciting at 488 nm and detecting at 520 nm using a UV-Vis Synergy H1 plate reader (BioTek). ssDNA in the supernatant was quantified using a standard curve fit with a 4-parameter logistic regression to correlate fluorescent intensity to ssDNA concentration. Bound ssDNA for the different volume fractions was calculated as the difference of the initial amount of ssDNA in the solution and the amount of ssDNA measured in the supernatant.
2.3. Surface Functionalization.
NACC fibers were immobilized to untreated polystyrene well plates (Eppindorf) using sulfo-SANPAH (Proteochem) heterobifunctional crosslinker. Briefly, well plates were treated with 20 μm sulfo-SANPAH diluted in deionized water and irradiated with 365 nm UV light for 10 minutes. UV light activates the nitrophenyl azide group of the crosslinker for bonding to the polystyrene surface. Then the wells were rinsed three times with sterile deionized water and incubated with the fiber solutions overnight at room-temperature. During incubation, the sulfo-NHS ester from the sulfo-SANPAH is able to non-specifically react with primary amines present on the NACC self-assembled fibers. Following incubation, the wells were rinsed three times with sterile deionized water and stored in deionized water at 4 °C until needed.
2.4. NACC Fiber Morphology.
NACC fiber morphology for the different volume fractions of type I collagen and ssDNA was qualitatively assessed by phase contrast and fluorescence microscopy using immobilized fibers. For fluorescence microscopy, immobilized fibers were stained with SYBR Safe DNA stain (Invitrogen) diluted at a 1:10,000 volume ratio in deionized water. The fibers were incubated with the stain protected from light for at least 30 minutes and then imaged using an epifluorescence Nikon TE-2000U inverted microscope.
2.5. Mineralization of Immobilized NACC Fibers.
Immobilized NACC fibers were mineralized by incubating overnight at room-temperature with 500 μL of mineralizing solution having a final concentration of 25 mm NaCl (Sigma Aldrich), 8 mm Na2HPO4 (Sigma Aldrich), 15 mm CaCl2 (Sigma Aldrich) added sequentially. Then the wells were rinsed with deionized water and stored at 4 °C in deionized water until needed.
2.6. Mineralization of Mobile (In Solution) NACC Fibers and Gels.
2.6.1. Synthesis and Mineralization in One-Step.
Mineralized NACC fibers were formed in a one-step process by preparing two precursor solutions: 1) ssDNA and CaCl2 and 2) collagen, NaCl, Na2HPO4 together. These two solutions were then mixed together to give an effective final concentration of 10 mm CaCl2, 36.67 mm NaCl, 4 mm Na2HPO4, 0.1 – 0.9 μm ssDNA, and 0.03 – 0.27 mg/mL collagen with a final volume of 250 μL.
Mineralized NACC gels were formed in a one-step process by preparing two precursor solutions: 1) ssDNA and CaCl2 and 2) collagen, NaCl, Na2HPO4 together. These two solutions were then mixed together to give an effective final concentration of 10 mm CaCl2, 36.67 mm NaCl, 4 mm Na2HPO4, 1 –9 μm ssDNA, and 0.3 – 2.7 mg/mL with a final volume of 500 μL.
2.6.2. Synthesis and Mineralization in Two-Steps.
Mineralized NACC fibers and gels were formed in a two-step process by preparing fibers and gels as previously described in Section 2.1. Then the fibers and gels were incubated in 250 μL and 500 μL of mineralizing solution with a final concentration 10 mm CaCl2, 36.67 mm NaCl, 4 mm Na2HPO4, respectively.
Mixtures were incubated at room-temperature and removed from the mineralization solution after 1, 3, and 6 days. This was done by centrifugation to pellet the assemblies, rinsing with deionized water, and then resuspending in 100% molecular biology grade ethanol (Fisher Scientific) thereafter for storage at room-temperature until analysis by either x-ray diffraction, transmission electron microscopy, or scanning electron microscopy. Resuspension in ethanol was done to facilitate sample preparation for those analysis techniques.
2.7. Alizarin Red Stain Assay.
After mineralization, immobilized NACC fibers were stained with 500 μL of 40 mm alizarin red stain (Sigma Aldrich) for 30 minutes at room temperature. Then washed with deionized water three times. Stained fibers were imaged by phase contrast microscopy. Then, 250 μL of 10% (w/v) cetylpyridinium chloride (Sigma Aldrich) was added to release the calcium-bound stain and agitated on an orbital shaker for 5 minutes. The solution was collected and centrifuged at 10,000g for 10 minutes. 100 μL aliquots of the supernatant were plated in duplicate and read at 550 nm using a Synergy H1 Spectrophotometer. Absorbance was converted to alizarin red stain concentration using a standard curve fit with a 4-parameter logistic regression model.
2.8. X-ray Diffraction.
The change in crystallinity of one- and two- step mineralized NACC gels incubated for 1, 3, and 6 days in mineralization solution was assessed by X-ray diffraction (XRD) using a Panalytical Xpert-Pro system. Gels were placed on a zero-background holder and irradiated by monochromatized Cu Kα X-ray radiation from an Empyrean Cu LFF DK406691 fixed anode X-ray tube, operated at 45 kV and 40 mA, together with a diffractometer scan step size of 2θ = 0.0167°, and a dwell time of 0.127 s step−1, over a 2θ range of 10 – 60°. Diffraction patterns were processed at the same time in Spectragryph v1.2.10 to perform background removal and smoothing using a 2nd order scattering baseline followed by a 100 interval, rectangular moving average filter.
2.9. Transmission Electron Microscopy and Selected Area Electron Diffraction.
NACC fiber ultrastructure was assessed by negative staining fibers with phosphotungstic acid. Fibers were synthesized by mixing 0.3 mg/mL rat tail tendon type I collagen in 6 mN acetic acid (Corning) diluted in sterile deionized water (20% volume fraction of mixture) with 1 μm ssDNA diluted in sterile deionized water (80% volume fraction of mixture). Fibers were formed for 1 hour at room-temperature and then were centrifuged at 2000g for 5 minutes. The supernatant was removed and replaced with 1% phosphotungstic acid aqueous staining solution (Electron Microscopy Sciences) at pH 7.0. Fibers were incubated in the staining solution for 1 hour at room-temperature and then pipetted onto lacey carbon copper grids (Electron Microscopy Sciences). The grids then were air-dried. Stained fibers were imaged by transmission electron microscopy (TEM). Fiber diameters were measured in Gwyddion 2.51 using line profiles defined perpendicular to the fiber longitudinal axis.
Crystallites from one- and two- step mineralized fibers incubated for 1, 3, and 6 days in mineralization solution were imaged and were assessed by TEM and selected area electron diffraction (SAED). Fiber solutions in ethanol were pipetted onto lacey carbon copper grids (Ted Pella) and the remaining ethanol was allowed to evaporate.
All imaging was performed using a FEI Tecnai F20 S/TEM operated between 80 – 200 keV in brightfield (BF) and SAED modes. Electron diffraction patterns were indexed in ImageJ (National Institute of Health).
2.10. Scanning Electron Microscopy and Energy Dispersive X-ray Spectroscopy.
NACC gel morphology of one- and two- step mineralized gels incubated for 6 days in mineralization solution was assessed by scanning electron microscopy (SEM). Gels were placed and were air-dried on circular cover glass and the cover glass then was adhered to SEM stubs using double-sided tape. Gels then were sputter coated with Au/Pd (7 kV, 10 mA, 30 mTorr, 60 s). SEM micrographs were taken using a Tescan MIRA3 field emission SEM with an operating voltage between 0.2 – 30 keV. The presence of calcium and phosphate in the gels was confirmed by energy dispersive X-ray spectroscopy (EDS) using a mounted EDAX Octane Pro EDS system. EDS spectra were collected at three separate points across the sample.
2.11. Cell Culture.
Human osteoblasts (HObs) (Cell Applications, Lot #3258, 52-year-old black female) were grown on tissue culture polystyrene in a humidified cell culture incubator kept at 37 °C and 5% CO2. Cells were cultured between passage number 4 – 6 in fully supplemented Osteoblast Growth Medium (Cell Applications). Media was exchanged every 2 – 3 days.
2.12. Mineralized NACC Fibers In Vitro.
20% volume fraction collagen solution NACC fibers were formed as previously described in Section 2.1. These fibers were immobilized to untreated polystyrene 24 well well-plates (Eppindorf) and mineralized as previously described in Section 2.3, 2.5. HObs were seeded in triplicate at 5,000 cells/cm in each well as well as on a tissue-culture polystyrene control (Corning). HObs were cultured for 3 days without media renewal. Phase images were taken daily. After 3 days, cells were rinsed in phosphate-buffered saline and fixed in 4% formalin for 15 minutes. Then rinsed three times with 5 minutes of agitation on an orbital shaker between rinses and stored in phosphate-buffered saline at 4 °C until immunocytochemistry was performed.
2.13. Immunocytochemistry.
Immunocytochemistry was performed to visualize HObs morphology and protein expression. Cells were permeabilized with 0.1% Triton-X 100 in phosphate-buffered saline (PBS) for 10 minutes, then rinsed 3 times with PBS, and blocked for 30 minutes with 1% bovine serum albumin (BSA) in PBST (0.1% Tween 20 in PBS). The cells then were incubated at 4 °C overnight with a primary antibody for osteopontin (abcam, ab69498) at a 1:200 dilution in 1% BSA in PBST. The cells then were rinsed 3 times with 1% BSA in PBST and were incubated for 1 hour at room-temperature in the dark with a secondary antibody (abcam, ab150080) at a 1:200 dilution in 1% BSA in PBST. Following incubation, the cells were rinsed 4 times with 1% BSA in PBST and were mounted using ProLong Diamond with DAPI (Invitrogen). In a similar manner, after the permeabilization step to stain for cytoskeletal F-actin, the cells were incubated with Texas-Red phalloidin (Invitrogen) following the manufacturer’s instructions and were mounted using ProLong Diamond with DAPI (Invitrogen). Fluorescence microscopy was conducted using an epifluorescence Nikon TE-2000U inverted microscopy.
2.14. Mineralized NACC Gels In Vitro.
NACC gels were prepared by mixing type I rat tail collagen in 0.02 N acetic acid to a final concentration of 0.6 mg/mL and ssDNA to a final concentration of 8 μm in complete Osteoblast Growth Medium (Cell Applications) to a final volume of 500 μL. HObs were seeded at 62,500 cells at passage 6. Gels were prepared in individual wells of a 24 well ultra-low attachment plate (Corning). The gels with embedded cells then were incubated overnight to promote cell attachment before mineralization (Figure S1). The gels were mineralized by adding in the following order sterile solutions of NaCl, Na2HPO4, and CaCl₂. Final concentrations were 25 mm NaCl, 8 mm Na2HPO4, and 15 mm CaCl₂ in a final volume of 500 μL. The solution was mixed in the well by pipetting up and down and swirling the well plate. The gel was incubated in this solution for ~10 minutes in a cell culture incubator. Then the solution was removed and was replaced with 1 mL Osteoblast Growth Medium. After 3 days of culture, gels were fixed in 4% formalin for 15 minutes. Then the gels were rinsed three times with 5 minutes of agitation on an orbital shaker between rinses and were stored in phosphate-buffered saline at 4 °C until needed. Gels were then stained with 40 mm alizarin red stain (Sigma Aldrich) for 30 minutes and were rinsed several times to remove unbound stain. Subsequently, the fixed gels were incubated in Hoescht 33342 (Invitrogen) following the manufacturer’s instructions. Phase contrast and fluorescence microscopy were conducted using an epifluorescence Nikon TE-2000U inverted microscope.
3. RESULTS
3.1. Synthesis and Mineralization of NACC Fibers and Gels.
Upon mixing dilute solutions of the ssDNA and type I collagen, ssDNA-collagen complexes spontaneously and rapidly self-assembled in aqueous solution. No assemblies were observed for either component on their own. Fibers formed (Figure 1a) by mixing the ssDNA and type I collagen above a mass fraction of ~9% ssDNA in solution. Self-assembled fibers formed when ssDNA-collagen binding was greater than ~5 pmol ssDNA/μg collagen (Figure 1b) below which nanoparticle aggregates persisted.
Figure 1.

A representative image of NACC fibers formed at ~14% mass fraction DNA in solution stained for DNA (a). ssDNA-collagen bindings on a mole per mass basis (b) as a function of mass fraction DNA in solution. A representative image of mineralized immobilized NACC fibers formed at ~14% mass fraction DNA in solution stained with alizarin red (c). Quantified alizarin red stain bound to the mineralized immobilized NACC fibers as a function of bound ssDNA/collagen on a mole per mass basis (d). Each data point in (b) and (d) was measured in triplicate and error bars are one standard deviation.
We next investigated whether these fibers would strongly bind and retain calcium phosphate mineral after forming. To do this, we immobilized the fibers to a polystyrene substrate using the heterobifunctional crosslinker sulfo-SANPAH. Fibers were immobilized to ease rinsing of the fibers during later processing and to remove unincorporated ssDNA and collagen. We then incubated the fiber functionalized surface in a solution of NaCl and Na2HPO4 and initiated mineralization by the addition of CaCl2. Within minutes, visible calcium phosphate precipitated (Video S1). Mineral bound to the fibers was visualized by staining for calcium using alizarin red stain (Figure 1c). Well plates conjugated with only collagen did not retain mineral nor were fibrous structures present prior to incubation with the mineralization solutions. Interestingly, the amount of bound calcium phosphate decreased with increased ssDNA-collagen binding (Figure 1d). DNA has an affinity for calcium phosphate through electrostatic interactions between the DNA phosphate backbone and the calcium exposed on the surface of calcium phosphate crystals [20]. At the same time, DNA has an avidity for collagen, through the combining of their hydration shells promoted by interactions between DNA’s phosphate backbone and CH2 groups on the collagen triple helix [35]. Because of these different interactions there may be competition between the calcium phosphate, ssDNA, and collagen species.
Interested by this and the potential interference of calcium phosphate precipitate on fiber formation, we investigated whether the formation of fibers and their mineralization would occur in a one-step synthesis process by mixing a solution of ssDNA and CaCl2 with a solution of collagen, NaCl, and Na2HPO4. As with the two-step synthesis (i.e. fibers formed and then mineralized), fiber formation readily occurred (<10 minutes) and these fibers displayed a bound mineral phase.
Not only NACC fibers, but also 3D gels were able to be produced. By increasing the ssDNA and collagen concentrations by 10 times, we achieved the spontaneous and rapid formation of NACC gels (Figure 2). The gels had a loose network structure when suspended in solution. To make a more compact structure, the gels could be densified by centrifugation. The gels were visualized as NACCs and not simply precipitated collagen by staining the gels with a green fluorescent DNA stain and then imaging under blue light (Figure 2). As with the fibers, the gels were mineralizable by both the one- and the two- step approach. Thus, NACCs can be prepared in both 2D and 3D formats and both are mineralizable. We have tested several other ssDNA sequences and observed their ability to form mineralized NACC fibers and gels in a similar capacity as the ssDNA sequence presented (data not shown). Owing to their ubiquity, these fibers and gels have promise for not only bone tissue engineering, but as coatings and scaffolds for any tissue using this versatile biomaterial platform by substituting the collagen type I for other tissue-specific collagens and the ssDNA for functional DNA aptamers.
Figure 2.

ssDNA fluorescently stained using SYBR Safe DNA stain (Invitrogen) to visualize the NACC gel after formation in 0.6 mL microcentrifuge tubes.
To visualize the fiber ultrastructure, unmineralized fibers were negatively stained using phosphotungstic acid and imaged by TEM. This stain is widely used for visualizing the D-spacing of aligned collagen fibrils [36]. Unexpectedly, solid, compact fibrils were not observed. We saw masses of very thin “spaghetti-like” fibrils consisting of highly intermixed, curved chains (Figure 3a). Furthermore, no crossbanding pattern was observed for these complexes as previously has been described for large (2980 base pair), random sequences of dsDNA-collagen complexes, which were formed by mixing 0.75 mg/mL collagen and 0.1 mg/mL dsDNA [37]. Fibril diameters were measured from high resolution TEM micrographs using line profiles of pixel intensity drawn perpendicular to the fibril longitudinal axis (Figure 3b, inset). The complex fibrils had a mean diameter of 7.38 ± 1.27 nm (n = 12). Because the NACC formed a divergent configuration from that of native collagen fibrils, it was even more necessary to characterize the mineralized state of these complexes.
Figure 3.

TEM micrographs of 1% phosphotungstic acid stained NACC fibrils (a) and high resolution TEM micrographs of those fibrils with an inset representative line profile of an individual fibril (b).
3.2. Characterization of NACC Mineralization.
To characterize the mineralization of the NACC fibers and gels in more detail, a combination of XRD, TEM, SAED, SEM, and EDS was performed. XRD patterns of two-step mineralized gels (Figure 4a) displayed peaks indictive of the hydroxyapatite (HAP) (002) plane at ~26° and a large peak at ~32° assigned to the combination of the HAP (211), (112), and (300) planes [26]. No other peaks were discernable, which was attributed to excessive peak broadening from nanocrystalline crystallites and a favorable “poorly crystalline” character [26,38]. Such patterns are akin to early stage bone formation [26]. In comparison, as expected unmineralized gels showed a large amorphous hump. The diffraction patterns for the two-step mineralized gels minimally changed after 24 hours of incubation in the mineralizing solution indicating that mineralization had ceased. Brightfield TEM of mineralized fibers confirmed nanocrystalline calcium phosphate (Figure 4b). The crystallites were randomly oriented with plate-like morphology indicative of the HAP phase [26]. XRD patterns for one-step mineralized NACC gels mimicked the patterns of the two-step mineralized gels. However, the one-step mineralized gels incubated in mineralizing solution for 1 day showed a difference by the presence of a slight overlaid amorphous hump from 20 – 32° (Figure 5a). After 1 day of incubation in mineralization solution, TEM images of one-step mineralized NACC fibers had contrast indicative of mineral accumulation as compared to unmineralized fibers as well as SAED patterns for HAP (Figure 5b–c). However, these fibers were not overrun with HAP platelets seen for the two-step mineralization process after 1 day of incubation. One-step mineralized fibers after 1 day of incubation in mineralizing solution, resembled those of early stage PILP mineralization of collagen using polyaspartate without a cross-banding pattern [26]. Individual complex nanofibrils observed in the unmineralized condition (Figure 3a) were unable to be identified in the mineralized condition suggesting the mineral phase was interpenetrating and acting to coalesce them into thicker bundles.
Figure 4.

Characterization of mineralized NACCs. XRD patterns for two-step mineralized NACCgels after 1, 3, and 6 days in mineralization solution (a). A representative TEM micrograph of two-step mineralized NACC fibers after 6 days in mineralization solution (b) with a representative SAED pattern (inset).
Figure 5.

X-ray diffraction pattern of one-step mineralized NACC gel (a). Transmission electron micrograph of one-step mineralized incubated in mineralizing solution for 1 day (b) and unmineralized (c) NACC fibers with their associated small area electron diffraction patterns (b-c insets).
Hydroxyapatite and octacalcium phosphate (OCP) have extremely similar d-spacings making it difficult to determine crystalline phase exclusively from diffraction patterns for randomly oriented crystallites [26,39]. SAED patterns for mineralized fibers (Figure 4b, inset) were indexed and were compared to reported d-spacings for native bone and calcium phosphate references (Table 1). The indices were comparable to those of native bone; though, no arcing was observed in the SAED patterns (Figure 4b, inset), which was expected for randomly oriented mineralized fibers [40]. Suspected OCP flakes were observed when imaging the mineralized fibers by TEM (Figure S2). These crystallites were thought to be OCP because they melted under the 200 keV beam. OCP has been shown to undergo a phase transition to HAP due to localized heating from the TEM electron beam [41]. Meanwhile, the other crystallites (Figure 4b) were stable under the 200 keV electron beam suggesting they are electron beam stable HAP. As our observation of such “meltable” crystallites was very infrequent during TEM and based upon their instability under the 200 keV beam, we believe the observed crystallites (Figure 4b) and their SAED patterns belong to HAP.
Table 1.
Indexed d-spacings for random ssDNA and HAP aptamer mineralized fibers and their comparison to native bone, HAP, and OCP
| NACC | Bonea | HAPa | OCPa | ||
|---|---|---|---|---|---|
| d/Å | d/Å | d/Å | hkl | d/Å | hkl |
| 3.44 | 3.44 | 3.44 | (002) | 3.43 | (002) |
| 3.14 | 3.10 | 3.08 | (210) | 3.05 | (312) |
| 2.81 | 2.80 | (211) | 2.83 | (710) | |
| 2.78 | 2.77 | 2.78 | (112) | 2.77 | (322) |
| 2.71 | 2.72 | (300) | 2.69 | (700) | |
| 2.28 | 2.26 | 2.26 | (310) | 2.26 | (620) |
| 1.95 | 1.92 | 1.94 | (222) | 1.95 | (822) |
| 1.84 | 1.84 | 1.84 | (213) | 1.84 | (642) |
| 1.72 | 1.72 | 1.72 | (004) | 1.72 | (004) |
SEM of 6 day mineralized gels revealed a topographically rich surface akin to that of native extracellular matrix (ECM) with pits, pores, and striations (Figure 6) [42,43]. Individual fibers were less visible being more of an isotropic fibrous agglomerate (Figure 6a). At the surface of the mineralized NACC gels, the same nanometer sized HAP crystallites observed by TEM were present (Figure 6b). EDS confirmed the presence of Ca and P incorporated in the gel (Figure S3). Calcium phosphate phases have Ca to P ratios ranging anywhere from 0.5 – 2.5 with 1.67 for HAP, 1.5 to 1.67 for Ca-deficient HAP, and 1.33 for OCP, respectively [24]. Integration of the EDS Ca and P peaks ranged from 0.95 to 1.40 for the local Ca/P ratio across the sample. At first this suggested the potential mixture of several calcium phosphate phases present in the gel running counter to the XRD and SAED results. Though, we attributed the reduced Ca/P ratio to the ssDNA present in the NACC because the phosphate backbone of ssDNA would be able to elevate the P content in the EDS spectrum and thus artificially reduce the Ca/P ratio specific to the calcium phosphate mineral. Together, the combination of porosity, mineral, and nanotopography are suggestive of a favorable surface for bone tissue engineering.
Figure 6.

Representative SEM micrographs of the surface of a random ssDNA two-step mineralized gel after 6 days in mineralization solution (a) with higher magnification micrographs of central region designated (b).
Collectively, this data shows that the synthesis route had a negligible effect on the mineralization of NACCs. The incorporation of HAP into NACC fibers and gels and their structure suggests it to be a highly osteoconductive biomaterial platform requiring investigation of the biological response to their biophysical cues.
3.3. NACC Fibers Spur an Osteoblast-to-Osteocyte-like Morphology.
We cultured primary human osteoblasts (HObs) on immobilized NACC fibers in both the unmineralized and mineralized state to observe their response to the fiber biophysical cues. Remarkably, the HObs readily attached and within 24 hours began to display an osteocytic-like morphology indicated by formation of extensive dendritic processes (Figure 7) [44]. In comparison, few dendritic processes were observed for HObs on TCP (Figure 7a, d). Both the unmineralized and the mineralized NACC fibers supported dendritic process formation, which was made more clear by staining for cytoskeletal F-actin (Figure 8a, b). HObs qualitatively reduced in spreading and produced several long, thin extensions. As this behavior was independent of the mineralization state of the fibers, this suggests the NACC fiber topography was the dominant mediator of this change in HOb morphology. In a similar manner, immunofluorescence staining for osteopontin appeared to be similar for the HObs cultured on immobilized unmineralized and mineralized NACC fibers (Figure 8c, d). From this short-term investigation, we observed that HObs were able to attach and interrogate unmineralized and mineralized NACC fibers and that their response was mediated more so by the fiber topography than the fiber mineralization state. Until this point only the response of human umbilical vein endothelial cells to unmineralized NACC fibers had been reported. These preliminary results are hopeful for NACC fibers as biomaterial coatings.
Figure 7.

Representative phase contrast microscope images of HObs taken over 2 days of culture on tissue culture polystyrene (a, d), unmineralized (b, e), and mineralized (c, f) immobilized NACC fibers.
Figure 8.

Representative immunocytochemistry fluorescence microscope images of HObs taken after 3 days of culture stained for cytoskeletal F-actin (a, b) and osteopontin (c, d) on unmineralized and mineralized immobilized NACC fibers.
3.4. Osteoblasts Assemble Cell-Laden NACC Gels.
Going further, we were interested in HOb behavior in a 3D environment made using the NACC gels. Gels were synthesized by embedding the cells in a cell culture media-collagen solution followed by the addition of the ssDNA to initiate NACC formation. This formed a loose cell-laden NACC gel suspension at day 0, which within 1 day was aggregated by the encapsulated HObs and further densified by day 2 (Figure 9).
Figure 9.
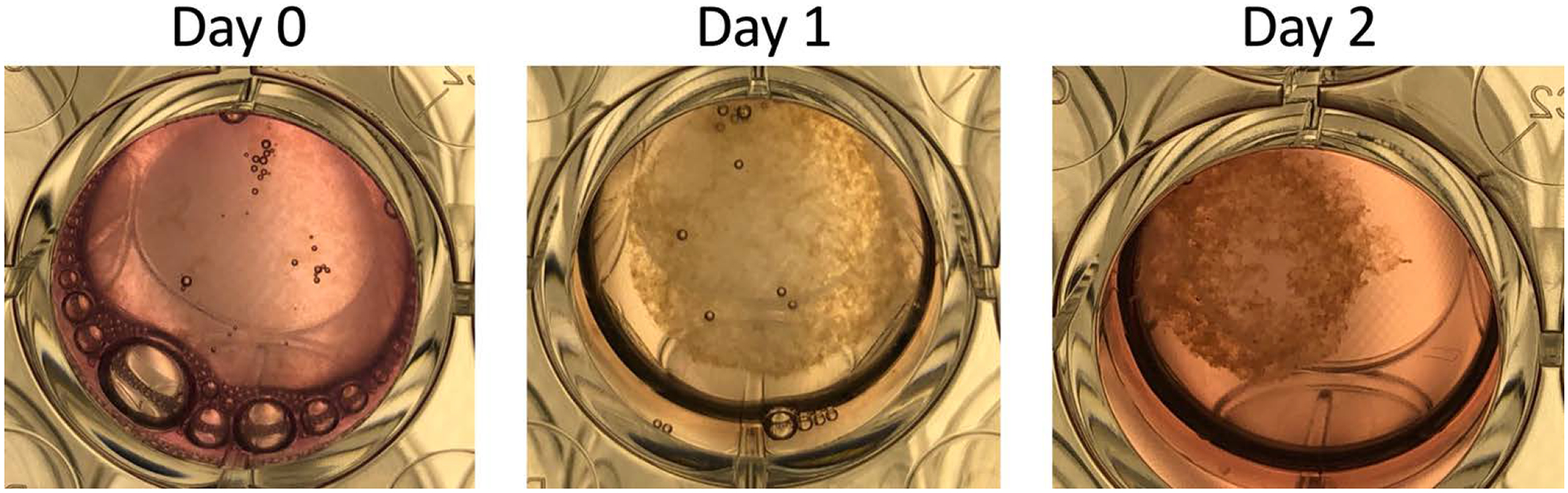
HObs aggregated the dispersed NACC gel into a dense tissue over a 2 day period.
Cells took on the same dendritic morphology as for the 2D environment as well as forming an interconnected network throughout the gel (Figure 10a). After 3 days the NACC gels were solid tissue (Figure 10b). Moreover, after the cell-driven aggregation, we resuspended the gels in mineralization solution following our two-step mineralization procedure. From this we were able to produce a mineralized gel with embedded osteoblasts. In the same fashion as the unmineralized gels, after 3 days of culture, the mineralized gels were densified into solid tissue (Figure 11). Each cell densified gel had a contractile appearance with “curls” and “ruffles” across their surface. The incorporated HAP in the gels was confirmed by staining with alizarin red stain. The stained mineralized gels had a dark, blood red color while the unmineralized gels retained only a faint pink coloration at the time of imaging from the stain, which continued to leach into the surrounding solution afterwards. The cell distributions were visualized in the cell densified gels by staining for cell nuclei (Figure 10c, Figure 11b), which revealed a qualitative difference in cell number being higher for the unmineralized gels; though, this may be an artifact of the mineral obscuring fluorescent intensity for underlying cells through the gel thickness. These preliminary results are hopeful for NACC gels as a 3D biomaterial platform.
Figure 10.

A representative image of live HObs stained with calcein AM (Invitrogen) following the manufacturer’s instructions after 24 hours of culture in the NACC gel (a). Microscopy image of the fixed unmineralized cell densified NACC gel (b) with associated composite images of the embedded cell nuclei stained with Hoescht 33342 (c). Scale bar in (b-c) is 3000 μm.
Figure 11.

Microscopy image of the fixed mineralized cell densified random NACC gel (a) with associated composite images of the embedded cell nuclei stained with Hoescht 33342 (b). Scale bar in (a-b) is 3000 μm.
4. DISCUSSION
We are the first to report the synthesis and utility of mineralized NACC fibers and gels for their use in bone tissue engineering. It should be appreciated the simplicity and rapidity for synthesizing these ECM-mimetics. Simply put, they are made by mixing two solutions: a ssDNA solution with a collagen solution. The synthesis time is seconds to minutes. These complexes can be stored in a dry-state or aqueous-state in physiological buffer at room-temperature for extended periods of time [8]. Moreover, these complexes are customizable being non-specific for DNA sequence such that DNA aptamer sequences designed as agonists or antagonists could be used [16,45]. Similarly, they are non-specific for other collagens such that atelocollagen, type II collagen, and type IV collagen could be used [1–4]. These properties are paramount to achieving off-the-shelf, one-step, intra-operative tissue engineering solutions [46]. Being multimodal (particles, fibers, gels) enables this biomaterial platform to support a breadth of applications from nucleic acid delivery (particles), coatings (fibers), and scaffolds (gels).
Importantly, is the promise of supplementing these architectures with other native biomolecules or additives to engineer more mimetic and functional ECM [47–49]. We have started to do this by incorporating nanocrystalline hydroxyapatite into the complex for producing a mineralized ECM. Our short (40 nucleotide), monodisperse, random sequence ssDNA NACC fibers and gels retained a nanocrystalline HAP mineral phase after incubation with a mineralizing solution of calcium phosphate. The mineralization was largely extrafibrillar leading to NACCs covered in randomly oriented HAP. Self-assembled peptide amphiphile nanofibers have been mineralized with the HAP platelet c-axis aligned in the nanofiber longitudinal direction, such that our NACC fibrils may also be able to achieve such an arrangement by aligning the nanofibrils from their naturally curled state [50]. Previously, we showed that ssDNA length plays an integral role in the formation of NACC fibers as well as the relative amount of both collagen and ssDNA in the NACC synthesis mixture [19]. Specifically, the number of ssDNA oligomers bound in the complex is greater for shorter ssDNA. Here we showed that the amount of calcium phosphate depended on the amount of bound ssDNA (Figure 1d); thus, it is conceivable that the length of the ssDNA oligomer could be used to tune the amount of bound mineral and may lead to unique mineralized NACC structures and properties. For instance, PILP-mineralization shows a molecular weight dependence favoring larger aspartate molecules for slowing crystal growth and stabilizing an amorphous calcium phosphate phase [51,52]. Similarly, DNA has been used to template crystal growth of nanoparticles [53]. It should be noted that the interactions between DNA and calcium phosphate are between the phosphate backbone of the DNA and surface calcium atoms [20]. It is conceivable that other ceramic phases and compositions could be incorporated into NACCs by taking advantage of this interaction with other multivalent, surface bound species. In the context of bone tissue engineering this ubiquity for short, monodisperse ssDNA to mineralize as a DNA-collagen complex enables DNA with added functionality derived from its sequence to form the complex without losing mineralizing potential. Hence, future investigations are required to evaluate the maintenance of DNA secondary structures in both unmineralized and mineralized NACCs.
TEM revealed our NACCs to be hierarchical “spaghetti-like” nanofibrils (curled, intermixed fibrils at multiple length scales) with mean diameter of ~7 nm. This would suggest the nanofibrils are on the scale of individual complex structures based on the model for the dsDNA-collagen complex being a central dsDNA double helix surrounded by five collagen triple helices [35]. However, the nanofibril curls were across 10s and not 1000s of nanometers, which is contrary to the rigidity of a collagen triple helix with a length of 300 nm [35]. Collagen triple helices are unstable at body-temperature and for type I collagen from rat tail tendon the denaturation point is as low as 28 °C [54]. Paired with our TEM observations of fibril curvature and mean diameter, we propose our NACC nanofibrils are not exclusively formed with triple helix collagen but could have type I collagen monomeric chains to support the observed extreme fibril curvature. Likewise, ssDNA can take on predictable 3D structures based on their environment, which has been used for the generation of DNA aptamers. For these reasons, we hypothesize that the ssDNA acts as a bridge between the collagen and hydroxyapatite. Because ssDNA can bind both species via interactions with its phosphate backbone and ssDNA can take on a collection of 3D structures, it is conceivable that ssDNA NACCs can organize into more diverse arrangements than the singular organization proposed for dsDNA NACCs. Nonetheless, more detailed modeling of short ssDNA-collagen complex interactions needs to be completed to resolve the molecular arrangement of the species that form them.
Mineralization was achieved as easily as the fiber and gel synthesis by either a one-step or two-step process. One-step mineralization enables the complete production of the mimetic ECM at once while the two-step process enables temporal control of the mineralization process. This temporal control enables this platform for possibly evaluating the effects of progressive tissue calcification, for instance in the context of heart valvular and blood vessel calcification. Mineralization completed within 24 hours indicated by both XRD patterns and TEM micrographs. Aspartate-based PILP mineralization requires appreciably more time to complete, suggesting that ssDNA-based mineralization works at an accelerated rate. Though, in our current synthesis method they do not form a biomimetic, intrafibrillar mineral phase that is achieved by PILP mineralization [26,28,55]. Our NACCs though demonstrate ECM mimetic nanotopographic pits, pores, and “poorly crystalline” HAP crystallites critical to successful osseointegration of biomaterials [46]. Solution conditions may influence NACC formation and mineralization as well. For our studies we only tested within a narrow window of ionic strength and pH. Collagen fibrillogenesis is known to be regulated not only by temperature but also by ionic strength and pH [56,57]. It is likely that the NACC formation and mineralization processes will show ionic strength and pH dependencies due to screening effects from surrounding ions as well as changes in the charge state of both collagen and DNA from protonation effects [58,59]. Similarly, molecular crowders could influence the NACC self-assembly process by inhibiting DNA and collagen mobility and confining them [60]. All these factors could be used to further control NACC properties.
Especially exciting is that NACCs rapidly promoted osteoblast morphological changes characteristic of an osteocyte-like morphology. Osteocytes regulate bone remodeling and thus inducing differentiation towards this cell type is ideal for facilitating osseointegration of a scaffold [49]. Differentiation is a multistep process in which osteoblasts migrate into mineralized matrix and produce an interconnected network of dendritic processes [44,61,62]. Because dendritic process formation was advanced by immobilized NACC fibers as compared to tissue culture polystyrene, this modality could be a successful osteoconductive coating for both orthopedic and dental implants leading to a quicker recovery and favorable integration of the implant. Further studies are necessary to elucidate the maturation of bone cells with unmineralized and mineralized NACC biomaterials. It should be appreciated that the cellular response to NACCs has been cell-specific. In our previous work using human umbilical vein endothelial cells, the cells remodeled NACC fibers into larger tubulogenic-like structures without a tremendous change in cellular morphology i.e. dendritic process formation [19]. While, in 2D culture the human osteoblasts expressed significant change in cellular morphology with little NACC fiber agglomeration and remodeling. Surprisingly, the osteoblasts demonstrated similar responses independent of NACC mineralization. Immunostaining for osteopontin was invariant with mineralization. Osteopontin is a non-collagenous protein that is heavily expressed by mature osteoblasts at sites of bone remodeling [63]. The similar expression of osteopontin between unmineralized and mineralized NACC fibers could be the result of its functional multiplicity. A highly phosphorylated form of the protein associates rapidly with hydroxyapatite for osteoclast signaling whereas a low phosphorylated form is synthesized prior to bone deposition [63]. In this way, the HObs cultured with the mineralized NACC fibers could have been expressing the highly phosphorylated form. Whereas the HObs cultured with the unmineralized NACC fibers could have been expressing the low phosphorylated form of osteopontin as the HObs would be preparing those fibers for mineralization. Nonetheless, further characterization of the biological response of not only osteoblasts, but other cell types to NACCs is necessary for establishing their utility for broader tissue engineering applications.
NACC biomaterials should be useful in a number of bone tissue engineering applications. There is a significant need for in vitro models to aid in drug discovery. This platform could be used as an in vitro model for tissue calcification by using other cell types such as vascular smooth muscle cells instead of osteoblasts to model vascular calcification. Only recently, has a biomimetic mineralized cell-laden model been developed focusing on mesenchymal stem cell differentiation [55]. Future investigations of our system should be used to evaluate mesenchymal stem cell differentiation to compare the efficacy of our cell-assembled mineralized NACCs to this aim. Bone is an electomechanical material with this property derived from its composition. Collagen is a piezoelectric material and hydroxyapatite is a flexoelectric material [64,65]. Mechanical stimulation is beneficial to bone repair because it stimulates osteocyte activity for regulating osteoblasts and osteoclasts. Osteocyte ion channels can be activated by piezoelectric currents generated following such mechanical stimulation [66]. Several strategies have been used to make biocompatible, electroactive biomaterials that can take advantage of these processes to stimulate bone healing [66–70]. DNA also has piezoelectric properties [71]. Thereby, mineralized NACCs may also be able to enhance bone repair by taking advantage of their similarities in compositional, structural, and electromechanical properties with those of native bone. Additionally, there is a need for addressing hard/soft interfaces paramount to effective connective tissue regeneration [72,73]. Such interfaces could be formed by utilizing our two-step mineralization process with a concentration gradient [74]. Combined with the proven mineralized cell-assembled tissue structures, NACC gels could be used as cell-laden large defect fillers. At the same time, the one-step synthesis and mineralization process could be used as a strategy for injecting mineralized NACCs for point-of-site administration [75–77]. Pertinent to tissue engineering, is potential for developing cell-assembled pre-vascularization by co-culture of endothelial and osteogenic cells [46]. Osteoblasts exert an angiogenic microenvironment by their secretion of vascular endothelial growth factor [78]. Likewise, osteoblasts produce nitric oxide, which supports a healthy, vasodilatory endothelial cell phenotype [79]. Because of the demonstrated rapidly-formed cell-assembled tissue structures, we are hopeful this platform could quickly generate pre-vascularized mineralized bone tissue using peripheral blood derived endothelial progenitor cells as an autologous endothelial cell source and adipose-derived or bone marrow derived mesenchymal stem cells as an autologous osteogenic cell source [46]. Nonetheless, further investigations are necessary to show the potential for NACC-based biomaterials to make these translational hopes a reality.
5. CONCLUSIONS
Here we show the rapid and facile synthesis of NACC microfibers and macro gels as a new class of naturally-derived functional biomaterials for tissue engineering and regenerative medicine applications. Adding a mineralization solution before or after complex synthesis generates an interpenetrating hydroxyapatite phase affording the system temporal control of the mineralization process. These nanofibrous complexes remarkably resemble native extracellular matrix architecture with pits, pores, and striations. Bone cells actively remodeled and matured supporting the mineralized variant of these complexes as a potentially highly osteoconductive biomaterial. Although this work focuses on bone tissue engineering, NACCs should be viewed as a biomaterial platform with broad applicability and potential to improve therapeutic outcomes in biomedical applications.
Supplementary Material
ACKNOWLEDGEMENTS
This work was supported in part by the National Science Foundation-CBET CAREER award (1453098) provided to Josephine B. Allen and in part by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number F31HL147445 to Bryan D. James. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank the staff at the University of Florida Nanoscale Research Facility for their continued excellence in service especially engineer Kristy Schepker for her help performing the XRD measurements and associate engineer Nicholas Rudawski for his help in taking the TEM and SEM micrographs.
REFERENCES
- [1].Izui S, Lambert PH, Miescher PA, In vitro demonstration of a particular affinity of glomerular basement membrane and collagen for DNA. A possible basis for a local formation of DNA-anti-DNA complexes in systemic lupus erythematosus., J. Exp. Med 144 (1976) 428–43. doi: 10.1084/jem.144.2.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Rosenberg AM, Hunt DW, Petty RE, The binding of DNA to native type II collagen., J. Rheumatol 10 (1983) 925–9. http://www.ncbi.nlm.nih.gov/pubmed/6663596. [PubMed] [Google Scholar]
- [3].Rosenberg AM, Prokopchuk PA, The binding of dsDNA and ssDNA to human types I, II and IV collagens., J. Rheumatol 13 (1986) 512–6. http://www.ncbi.nlm.nih.gov/pubmed/3488402. [PubMed] [Google Scholar]
- [4].Kitamura H, Iwamoto C, Sakairi N, Tokura S, Nishi N, Marked effect of DNA on collagen fibrillogenesis in vitro., Int. J. Biol. Macromol 20 (1997) 241–4. doi: 10.1016/S0141-8130(97)00021-4. [DOI] [PubMed] [Google Scholar]
- [5].Horgan C, Johnson RJ, Gauthier J, Mannik M, Emlen W, Binding of double-stranded DNA to glomeruli of rats in vivo., Arthritis Rheum. 32 (1989) 298–305. doi: 10.1002/anr.1780320311. [DOI] [PubMed] [Google Scholar]
- [6].Carlson JA, Hodder SR, Ucci AA, Madaio MP, Glomerular localization of circulating single-stranded DNA in mice. Dependence on the molecular weight of DNA, J. Autoimmun 1 (1988) 231–241. doi: 10.1016/0896-8411(88)90029-7. [DOI] [PubMed] [Google Scholar]
- [7].Campos PF, Craig OE, Turner-Walker G, Peacock E, Willerslev E, Gilbert MTP, DNA in ancient bone – Where is it located and how should we extract it?, Ann. Anat. - Anat. Anzeiger 194 (2012) 7–16. doi: 10.1016/j.aanat.2011.07.003. [DOI] [PubMed] [Google Scholar]
- [8].Sano A, Maeda M, Nagahara S, Ochiya T, Honma K, Itoh H, Miyata T, Fujioka K, Atelocollagen for protein and gene delivery., Adv. Drug Deliv. Rev 55 (2003) 1651–77. doi: 10.1016/j.addr.2003.08.005. [DOI] [PubMed] [Google Scholar]
- [9].Kandamchira A, Kanungo I, Fathima NN, Dielectric behaviour and conformational stability of collagen on interaction with DNA., Int. J. Biol. Macromol 51 (2012) 635–9. doi: 10.1016/j.ijbiomac.2012.06.039. [DOI] [PubMed] [Google Scholar]
- [10].de Campos Vidal B, Mello MLS, Variable collagen-DNA complex formation in vitro as assessed by optical anisotropy and infrared microspectroscopy, Int. J. Biol. Macromol 131 (2019) 510–519. doi: 10.1016/j.ijbiomac.2019.03.092. [DOI] [PubMed] [Google Scholar]
- [11].Pidaparti RM, Svintradze DV, Shan Y, Yokota H, Optimization of hydrogen bonds for combined DNA/collagen complex, J. Theor. Biol 256 (2009) 149–156. doi: 10.1016/j.jtbi.2008.09.013. [DOI] [PubMed] [Google Scholar]
- [12].Mrevlishvili GM, Svintradze DV, Complex between triple helix of collagen and double helix of DNA in aqueous solution, Int. J. Biol. Macromol 35 (2005) 243–245. doi: 10.1016/j.ijbiomac.2005.02.004. [DOI] [PubMed] [Google Scholar]
- [13].Mrevlishvili GM, Svintradze DV, DNA as a matrix of collagen fibrils, Int. J. Biol. Macromol 36 (2005) 324–326. doi: 10.1016/j.ijbiomac.2005.07.006. [DOI] [PubMed] [Google Scholar]
- [14].Honma K, Ochiya T, Nagahara S, Sano A, Yamamoto H, Hirai K, Aso Y, Terada M, Atelocollagen-Based Gene Transfer in Cells Allows High-Throughput Screening of Gene Functions, Biochem. Biophys. Res. Commun 289 (2001) 1075–1081. doi: 10.1006/bbrc.2001.6133. [DOI] [PubMed] [Google Scholar]
- [15].Ochiya T, Takahama Y, Nagahara S, Sumita Y, Hisada A, Itoh H, Nagai Y, Terada M, New delivery system for plasmid DNA in vivo using atelocollagen as a carrier material: the Minipellet, Nat. Med 5 (1999) 707–710. doi: 10.1038/9560. [DOI] [PubMed] [Google Scholar]
- [16].Zhou J, Rossi J, Aptamers as targeted therapeutics: current potential and challenges., Nat. Rev. Drug Discov 16 (2017) 181–202. doi: 10.1038/nrd.2016.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Zhang Y, Lai B, Juhas M, Recent Advances in Aptamer Discovery and Applications, Molecules. 24 (2019) 941. doi: 10.3390/molecules24050941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Burla F, Mulla Y, Vos BE, Aufderhorst-Roberts A, Koenderink GH, From mechanical resilience to active material properties in biopolymer networks, Nat. Rev. Phys 1 (2019) 249–263. doi: 10.1038/s42254-019-0036-4. [DOI] [Google Scholar]
- [19].James BD, Saenz S, van Gent A, Allen JB, Oligomer Length Defines the Self-Assembly of Single-Stranded DNA–Collagen Complex Fibers, ACS Biomater. Sci. Eng 6 (2020) 213–218. doi: 10.1021/acsbiomaterials.9b01435. [DOI] [PubMed] [Google Scholar]
- [20].Okazaki M, Yoshida Y, Yamaguchi S, Kaneno M, Elliott JC, Affinity binding phenomena of DNA onto apatite crystals, Biomaterials. 22 (2001) 2459–2464. doi: 10.1016/S0142-9612(00)00433-6. [DOI] [PubMed] [Google Scholar]
- [21].Graham FL, van der Eb AJ, A new technique for the assay of infectivity of human adenovirus 5 DNA, Virology. 52 (1973) 456–467. doi: 10.1016/0042-6822(73)90341-3. [DOI] [PubMed] [Google Scholar]
- [22].Jordan M, Schallhorn A, Wurm FM, Transfecting Mammalian Cells: Optimization of Critical Parameters Affecting Calcium-Phosphate Precipitate Formation, Nucleic Acids Res. 24 (1996) 596–601. doi: 10.1093/nar/24.4.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Olton D, Li J, Wilson ME, Rogers T, Close J, Huang L, Kumta PN, Sfeir C, Nanostructured calcium phosphates (NanoCaPs) for non-viral gene delivery: Influence of the synthesis parameters on transfection efficiency, Biomaterials. 28 (2007) 1267–1279. doi: 10.1016/j.biomaterials.2006.10.026. [DOI] [PubMed] [Google Scholar]
- [24].Pina S, Oliveira JM, Reis RL, Natural-Based Nanocomposites for Bone Tissue Engineering and Regenerative Medicine: A Review, Adv. Mater 27 (2015) 1143–1169. doi: 10.1002/adma.201403354. [DOI] [PubMed] [Google Scholar]
- [25].Gower LB, Biomimetic Model Systems for Investigating the Amorphous Precursor Pathway and Its Role in Biomineralization, Chem. Rev 108 (2008) 4551–4627. doi: 10.1021/cr800443h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Olszta MJ, Cheng X, Jee SS, Kumar R, Kim Y-Y, Kaufman MJ, Douglas EP, Gower LB, Bone structure and formation: A new perspective, Mater. Sci. Eng. R Reports 58 (2007) 77–116. doi: 10.1016/j.mser.2007.05.001. [DOI] [Google Scholar]
- [27].Thula TT, Rodriguez DE, Lee MH, Pendi L, Podschun J, Gower LB, In vitro mineralization of dense collagen substrates: A biomimetic approach toward the development of bone-graft materials, Acta Biomater. 7 (2011) 3158–3169. doi: 10.1016/j.actbio.2011.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Nudelman F, Lausch AJ, Sommerdijk NAJM, Sone ED, In vitro models of collagen biomineralization, J. Struct. Biol 183 (2013) 258–269. doi: 10.1016/j.jsb.2013.04.003. [DOI] [PubMed] [Google Scholar]
- [29].Su W, Ma L, Ran Y, Ma X, Yi Z, Chen G, Chen X, Li X, Alginate-Assisted Mineralization of Collagen by Collagen Reconstitution and Calcium Phosphate Formation, ACS Biomater. Sci. Eng (2020) acsbiomaterials.9b01841. doi: 10.1021/acsbiomaterials.9b01841. [DOI] [PubMed] [Google Scholar]
- [30].Goldberga I, Li R, Chow WY, Reid DG, Bashtanova U, Rajan R, Puszkarska A, Oschkinat H, Duer MJ, Detection of nucleic acids and other low abundance components in native bone and osteosarcoma extracellular matrix by isotope enrichment and DNP-enhanced NMR, RSC Adv. 9 (2019) 26686–26690. doi: 10.1039/C9RA03198G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Wojtas M, Lausch AJ, Sone ED, Glycosaminoglycans accelerate biomimetic collagen mineralization in a tissue-based in vitro model, Proc. Natl. Acad. Sci (2020) 201914899. doi: 10.1073/pnas.1914899117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Perez RA, Ginebra MP, Spector M, Cell response to collagen-calcium phosphate cement scaffolds investigated for nonviral gene delivery, J. Mater. Sci. Mater. Med 22 (2011) 887–897. doi: 10.1007/s10856-011-4308-5. [DOI] [PubMed] [Google Scholar]
- [33].Tenkumo T, Vanegas Sáenz JR, Takada Y, Takahashi M, Rotan O, Sokolova V, Epple M, Sasaki K, Gene transfection of human mesenchymal stem cells with a nano-hydroxyapatite-collagen scaffold containing DNA-functionalized calcium phosphate nanoparticles, Genes to Cells. 21 (2016) 682–695. doi: 10.1111/gtc.12374. [DOI] [PubMed] [Google Scholar]
- [34].Keeney M, van den Beucken JJJP, van der Kraan PM, Jansen JA, Pandit A, The ability of a collagen/calcium phosphate scaffold to act as its own vector for gene delivery and to promote bone formation via transfection with VEGF165, Biomaterials. 31 (2010) 2893–2902. doi: 10.1016/j.biomaterials.2009.12.041. [DOI] [PubMed] [Google Scholar]
- [35].Svintradze DV, Mrevlishvili GM, Metreveli N, Jariashvili K, Namicheishvili L, Skopinska J, Sionkowska A, Collagen–DNA Complex, Biomacromolecules. 9 (2008) 21–28. doi: 10.1021/bm7008813. [DOI] [PubMed] [Google Scholar]
- [36].Tzaphildou M, Negative staining electron microscopy of collagen fibrils, Micron Microsc. Acta 17 (1986) 201–213. doi: 10.1016/0739-6260(86)90047-X. [DOI] [Google Scholar]
- [37].Kaya M, Toyama Y, Kubota K, Nodasaka Y, Ochiai M, Nomizu M, Nishi N, Effect of DNA structure on the formation of collagen-DNA complex., Int. J. Biol. Macromol 35 (2005) 39–46. doi: 10.1016/j.ijbiomac.2004.11.005. [DOI] [PubMed] [Google Scholar]
- [38].Holder CF, Schaak RE, Tutorial on Powder X-ray Diffraction for Characterizing Nanoscale Materials, ACS Nano. 13 (2019) 7359–7365. doi: 10.1021/acsnano.9b05157. [DOI] [PubMed] [Google Scholar]
- [39].Brown WE, Smith JP, Lehr JR, Frazier AW, Octacalcium Phosphate and Hydroxyapatite: Crystallographic and Chemical Relations between Octacalcium Phosphate and Hydroxyapatite, Nature. 196 (1962) 1050–1055. doi: 10.1038/1961050a0. [DOI] [Google Scholar]
- [40].Rhee S-H, Suetsugu Y, Tanaka J, Biomimetic configurational arrays of hydroxyapatite nanocrystals on bio-organics, Biomaterials. 22 (2001) 2843–2847. doi: 10.1016/S0142-9612(01)00028-X. [DOI] [PubMed] [Google Scholar]
- [41].Xin R, Leng Y, Wang N, In situ TEM examinations of octacalcium phosphate to hydroxyapatite transformation, J. Cryst. Growth 289 (2006) 339–344. doi: 10.1016/j.jcrysgro.2005.11.010. [DOI] [Google Scholar]
- [42].Brody S, Anilkumar T, Liliensiek S, Last JA, Murphy CJ, Pandit A, Characterizing Nanoscale Topography of the Aortic Heart Valve Basement Membrane for Tissue Engineering Heart Valve Scaffold Design, Tissue Eng. 12 (2006) 413–421. doi: 10.1089/ten.2006.12.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Liliensiek SJ, Nealey P, Murphy CJ, Characterization of endothelial basement membrane nanotopography in rhesus macaque as a guide for vessel tissue engineering, Tissue Eng Part A. 15 (2009) 2643–2651. doi: 10.1089/ten.TEA.2008.0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Dallas SL, Bonewald LF, Dynamics of the transition from osteoblast to osteocyte, Ann. N. Y. Acad. Sci 1192 (2010) 437–443. doi: 10.1111/j.1749-6632.2009.05246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Ramaswamy V, Monsalve A, Sautina L, Segal MS, Dobson J, Allen JB, DNA Aptamer Assembly as a Vascular Endothelial Growth Factor Receptor Agonist, Nucleic Acid Ther. 25 (2015) 227–234. doi: 10.1089/nat.2014.0519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Amini AR, Laurencin CT, Nukavarapu SP, Bone Tissue Engineering: Recent Advances and Challenges, Crit. Rev. Biomed. Eng 40 (2012) 363–408. doi: 10.1615/CritRevBiomedEng.v40.i5.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Webber MJ, Appel EA, Meijer EW, Langer R, Supramolecular biomaterials, Nat. Mater 15 (2016) 13–26. doi: 10.1038/nmat4474. [DOI] [PubMed] [Google Scholar]
- [48].Mouw JK, Ou G, Weaver VM, Extracellular matrix assembly: a multiscale deconstruction, Nat. Rev. Mol. Cell Biol 15 (2014) 771–785. doi: 10.1038/nrm3902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Prince E, Kumacheva E, Design and applications of man-made biomimetic fibrillar hydrogels, Nat. Rev. Mater 4 (2019) 99–115. doi: 10.1038/s41578-018-0077-9. [DOI] [Google Scholar]
- [50].Hartgerink JD, Beniash E, Stupp SI, Self-assembly and mineralization of peptide-amphiphile nanofibers., Science (80-.). 294 (2001) 1684–8. doi: 10.1126/science.1063187. [DOI] [PubMed] [Google Scholar]
- [51].Quan BD, Sone ED, The effect of polyaspartate chain length on mediating biomimetic remineralization of collagenous tissues, J. R. Soc. Interface 15 (2018) 20180269. doi: 10.1098/rsif.2018.0269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Jee S-S, Thula TT, Gower LB, Development of bone-like composites via the polymer-induced liquid-precursor (PILP) process. Part 1: Influence of polymer molecular weight, Acta Biomater. 6 (2010) 3676–3686. doi: 10.1016/j.actbio.2010.03.036. [DOI] [PubMed] [Google Scholar]
- [53].Laramy CR, O’Brien MN, Mirkin CA, Crystal engineering with DNA, Nat. Rev. Mater 4 (2019) 201–224. doi: 10.1038/s41578-019-0087-2. [DOI] [Google Scholar]
- [54].Leikina E, Mertts MV, Kuznetsova N, Leikin S, Type I collagen is thermally unstable at body temperature, Proc. Natl. Acad. Sci 99 (2002) 1314–1318. doi: 10.1073/pnas.032307099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Thrivikraman G, Athirasala A, Gordon R, Zhang L, Bergan R, Keene DR, Jones JM, Xie H, Chen Z, Tao J, Wingender B, Gower L, Ferracane JL, Bertassoni LE, Rapid fabrication of vascularized and innervated cell-laden bone models with biomimetic intrafibrillar collagen mineralization, Nat. Commun 10 (2019) 3520. doi: 10.1038/s41467-019-11455-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Li Y, Asadi A, Monroe MR, Douglas EP, pH effects on collagen fibrillogenesis in vitro: Electrostatic interactions and phosphate binding, Mater. Sci. Eng. C 29 (2009) 1643–1649. doi: 10.1016/j.msec.2009.01.001. [DOI] [Google Scholar]
- [57].Holmes DF, Capaldi MJ, Chapman JA, Reconstitution of collagen fibrils in vitro; the assembly process depends on the initiating procedure, Int. J. Biol. Macromol 8 (1986) 161–166. doi: 10.1016/0141-8130(86)90020-6. [DOI] [Google Scholar]
- [58].Freudenberg U, Behrens SH, Welzel PB, Müller M, Grimmer M, Salchert K, Taeger T, Schmidt K, Pompe W, Werner C, Electrostatic Interactions Modulate the Conformation of Collagen I, Biophys. J 92 (2007) 2108–2119. doi: 10.1529/biophysj.106.094284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Lipfert J, Doniach S, Das R, Herschlag D, Understanding Nucleic Acid–Ion Interactions, Annu. Rev. Biochem 83 (2014) 813–841. doi: 10.1146/annurev-biochem-060409-092720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Hata Y, Sawada T, Serizawa T, Macromolecular crowding for materials-directed controlled self-assembly, J. Mater. Chem. B 6 (2018) 6344–6359. doi: 10.1039/C8TB02201A. [DOI] [PubMed] [Google Scholar]
- [61].Bonewald LF, The amazing osteocyte, J. Bone Miner. Res 26 (2011) 229–238. doi: 10.1002/jbmr.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Dallas SL, Prideaux M, Bonewald LF, The Osteocyte: An Endocrine Cell … and More, Endocr. Rev 34 (2013) 658–690. doi: 10.1210/er.2012-1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Sodek J, Chen J, Nagata T, Kasugai S, Todescan R, Li IW, Kim RH, Regulation of osteopontin expression in osteoblasts., Ann. N. Y. Acad. Sci 760 (1995) 223–41. doi: 10.1111/j.1749-6632.1995.tb44633.x. [DOI] [PubMed] [Google Scholar]
- [64].Minary-Jolandan M, Yu M-F, Uncovering Nanoscale Electromechanical Heterogeneity in the Subfibrillar Structure of Collagen Fibrils Responsible for the Piezoelectricity of Bone, ACS Nano. 3 (2009) 1859–1863. doi: 10.1021/nn900472n. [DOI] [PubMed] [Google Scholar]
- [65].Vasquez-Sancho F, Abdollahi A, Damjanovic D, Catalan G, Flexoelectricity in Bones, Adv. Mater 30 (2018) 1705316. doi: 10.1002/adma.201705316. [DOI] [PubMed] [Google Scholar]
- [66].Kao F-C, Chiu P-Y, Tsai T-T, Lin Z-H, The application of nanogenerators and piezoelectricity in osteogenesis, Sci. Technol. Adv. Mater 20 (2019) 1103–1117. doi: 10.1080/14686996.2019.1693880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Chen-Glasser M, Li P, Ryu J, Hong S, Piezoelectric Materials for Medical Applications, in: Piezoelectricity - Org. Inorg. Mater. Appl., InTech, 2018. doi: 10.5772/intechopen.76963. [DOI] [Google Scholar]
- [68].Chen J, Yu M, Guo B, Ma PX, Yin Z, Conductive nanofibrous composite scaffolds based on in-situ formed polyaniline nanoparticle and polylactide for bone regeneration, J. Colloid Interface Sci 514 (2018) 517–527. doi: 10.1016/j.jcis.2017.12.062. [DOI] [PubMed] [Google Scholar]
- [69].Xie M, Wang L, Ge J, Guo B, Ma PX, Strong Electroactive Biodegradable Shape Memory Polymer Networks Based on Star-Shaped Polylactide and Aniline Trimer for Bone Tissue Engineering, ACS Appl. Mater. Interfaces 7 (2015) 6772–6781. doi: 10.1021/acsami.5b00191. [DOI] [PubMed] [Google Scholar]
- [70].Li L, Yu M, Ma PX, Guo B, Electroactive degradable copolymers enhancing osteogenic differentiation from bone marrow derived mesenchymal stem cells, J. Mater. Chem. B 4 (2016) 471–481. doi: 10.1039/C5TB01899D. [DOI] [PubMed] [Google Scholar]
- [71].Yi Z, Shuhui Z, Jianxun W, Influence of orientation on the piezoelectric properties of deoxyribonucleic acid, Ferroelectrics. 101 (1990) 129–139. doi: 10.1080/00150199008016509. [DOI] [Google Scholar]
- [72].Seidi A, Ramalingam M, Elloumi-Hannachi I, Ostrovidov S, Khademhosseini A, Gradient biomaterials for soft-to-hard interface tissue engineering, Acta Biomater. 7 (2011) 1441–1451. doi: 10.1016/j.actbio.2011.01.011. [DOI] [PubMed] [Google Scholar]
- [73].Patel S, Caldwell J-M, Doty SB, Levine WN, Rodeo S, Soslowsky LJ, Thomopoulos S, Lu HH, Integrating soft and hard tissues via interface tissue engineering, J. Orthop. Res 36 (2018) 1069–1077. doi: 10.1002/jor.23810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Lausch AJ, Chong LC, Uludag H, Sone ED, Multiphasic Collagen Scaffolds for Engineered Tissue Interfaces, Adv. Funct. Mater 28 (2018) 1804730. doi: 10.1002/adfm.201804730. [DOI] [Google Scholar]
- [75].Kretlow JD, Young S, Klouda L, Wong M, Mikos AG, Injectable Biomaterials for Regenerating Complex Craniofacial Tissues, Adv. Mater 21 (2009) 3368–3393. doi: 10.1002/adma.200802009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Munarin F, Guerreiro SG, Grellier MA, Tanzi MC, Barbosa MA, Petrini P, Granja PL, Pectin-Based Injectable Biomaterials for Bone Tissue Engineering, Biomacromolecules. 12 (2011) 568–577. doi: 10.1021/bm101110x. [DOI] [PubMed] [Google Scholar]
- [77].Kondiah P, Choonara Y, Kondiah P, Marimuthu T, Kumar P, du Toit L, Pillay V, A Review of Injectable Polymeric Hydrogel Systems for Application in Bone Tissue Engineering, Molecules. 21 (2016) 1580. doi: 10.3390/molecules21111580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Hu K, Olsen BR, Osteoblast-derived VEGF regulates osteoblast differentiation and bone formation during bone repair, J. Clin. Invest 126 (2016) 509–526. doi: 10.1172/JCI82585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].van’T Hof RJ, Ralston SH, Nitric oxide and bone, Immunology. 103 (2001) 255–261. doi: 10.1046/j.1365-2567.2001.01261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


