Abstract
Purpose:
Respiratory hazards of farming have been identified for centuries, with little focus on gender differences. We used data from the AGRICOH consortium, a collective of prospective cohorts of agricultural workers, to assess respiratory disease prevalence among adults in 18 cohorts representing over 200,000 farmers, farm workers, and their spouses from six continents.
Methods:
Cohorts collected data between 1992–2016 and ranged in size from 200 to >128,000 individuals; 44% of participants were female. Farming practices varied from subsistence farming to large scale industrial agriculture. All cohorts provided respiratory outcome information for their cohort based on their study definitions. The majority of outcomes were based on self-report using standard respiratory questionnaires; the greatest variability in assessment methods was associated with chronic obstructive pulmonary disease (COPD).
Results:
For all three respiratory symptoms (cough, phlegm, and wheeze), the median prevalence in men was higher than in women, with the greatest difference for phlegm (17% vs. 10%). For asthma, women had a higher prevalence (7.8% vs 6.5%), with the difference associated with allergic asthma. The relative proportion of allergic asthma varied among cohorts. In two of eight cohorts for women and two of seven cohorts for men, allergic asthma was more common than non-allergic asthma.
Conclusions:
These findings indicate that respiratory outcomes are common among farmers around the world despite differences in agricultural production. As women in the general population are at higher risk of asthma, exploring gender differences in occupational studies is critical for a deeper understanding of respiratory disease among agricultural workers.
Introduction
Agricultural work is an occupation represented by both men and women, though little formal comparison of respiratory disease prevalence by gender has been conducted. Work in agriculture has been associated with respiratory diseases as early as the mid-1500’s [1]. Even as farm work becomes more industrialized, there continues to be evidence of increased respiratory risk for agricultural workers. Factors contributing to increased risk of respiratory diseases and symptoms include frequent exposure to dusts, microorganisms, toxic gases (e.g. diesel motor exhaust, welding fumes, ammonia, hydrogen sulfide, and carbon dioxide), and pesticides [2]. Agricultural activities vary by region and thus, exposures will also vary. While respiratory diseases have been a concern among farming populations for many centuries, recent studies have focused on differences between allergic vs. non-allergic phenotypes [3–7] due to the reduced risk of allergy associated with growing up on a farm [8].
Agricultural workers include both farmers who are owners and operators and farm workers (local and migrant). Women often have an active role in farm production activities but in some populations are not regarded as farmers, and as a result, the impact of their occupational exposures may be under-represented. Agricultural work remains an occupation that people often begin at young ages.
While many papers have been published related to the respiratory health of agricultural workers, few, if any, have attempted to integrate data from across continents and farming practices to characterize the global respiratory health implications of agricultural work. In 1998, the American Thoracic Society published a research statement on Respiratory Hazards of Agriculture [1]. In this seminal work, extensive detail was provided on the specific respiratory outcomes, as well as the range of exposures experienced by agricultural workers primarily in developed countries. However, respiratory hazards of women and agricultural work in low and middle income countries were not well represented. A limited amount of literature has been published assessing gender differences in the incidence and/or prevalence of respiratory symptoms and diseases among farming populations, and nearly all of these studies focus of populations in either the United States or Europe [9–11]. Although there has not been a multi-country study to estimate the global burden of respiratory disease among farmers, the numerous cohort studies that have been conducted around the world can help start to address this gap in knowledge.
The AGRICOH consortium was created in 2006 as a collaborative effort to assess relationships between farming exposures and health outcomes. Currently 29 cohorts are participating and they include a diverse range of types of farming from all continents [12]. To assess the prevalence of respiratory disease and symptoms among diverse farming populations and to explore differences between men and women, we focused on common respiratory endpoints from AGRICOH cohorts with respiratory outcome information.
Methods
Study Population
The AGRICOH consortium consists of 29 cohorts from around the world (http://agricoh.iarc.fr/). We focused on adults for this analysis because we were interested in occupational exposures. Fourteen cohorts were excluded from this analysis: four did not include adults, eight did not collect respiratory outcome information, and two were unable to provide data. All eligible AGRICOH cohorts agreed to participate. Additionally, three farming cohorts outside of AGRICOH, but which included AGRICOH investigators, were also identified for inclusion, resulting in 18 cohorts for this analysis [13–29]. These cohorts cumulatively represent 211,232 people. The data presented includes farming populations around the world, including those of low and middle income countries with different socioeconomic settings, spanning from 1992 to 2016.
Data Collection
For this project, we developed a structured reporting form to collect standardized demographic and outcome information (see supplement 1). All cohorts were asked to provide summary statistics on their cohorts; raw data were not collected. All cohorts except the Agricultural Health Study (AHS) provided prevalence estimates for data collected at enrollment. For the AHS, data from the most recent AHS interview were included because this information was more complete than the enrollment information.
Cohort Demographic Information
The data collection form requested information on cohort: sample size and calendar year of data collection, as well as summary statistics regarding age distribution, gender, smoking status (current/past/never), and body mass index (BMI, <20, 20-<25, 25 - <30, and ≥30). We also collected data on the participant types (farmer, farm worker, subsistence farmer), role of women in cohort (full time farmers, help on farm, spouses), type of livestock raised (poultry, beef cattle, dairy cattle, pork, other), type of farming (row crops, vegetables, orchards, other), and grain handling. We applied the World Bank Atlas method to determine country economy classifications, categorized by gross national income (GNI) per capita: low-income (≤$1,025), lower-middle-income ($1,026-$4,035), upper-middle-income ($4,036–12,475), and high income (≥$12,476) [30].
Respiratory Outcome Information
Cohorts were asked to provide prevalence and 95% confidence interval information for three respiratory symptoms (cough, phlegm, and wheeze) and two respiratory diseases (asthma and chronic obstructive pulmonary disease (COPD)). Asthma was further classified as either allergic or non-allergic, based on each cohort’s definition.
Outcome definitions varied by cohort with most using standard respiratory questionnaires (e.g., American Thoracic Society Questionnaire [31] and European Community Respiratory Health Survey [32]). Some studies collected only self-reported outcome information while others incorporated clinical measurements as well. All symptom information was self-reported. Asthma was reported as either ever asthma or asthma in the past 12 months. All but one study relied on self-reported doctor’s diagnosis of asthma, while the remaining study included a broader definition of having had an history in the past year of an attack of shortness of breath, an asthma attack, using asthma medication or having a positive bronchodilator test conducted by study staff [16].
COPD definition was most variable among the cohorts (supplement 1). Fifteen cohorts provided information on COPD prevalence. This information was based on self-report (67%, 10/15 cohorts), spirometry (27%, 4/15 cohorts), or an inclusive definition of either spirometry or self-report (7%, 1/15 cohorts). Among the 11 studies that used self-report to ascertain COPD status, definitions for COPD included: doctor diagnosis of COPD alone (27%); doctor diagnosis of chronic bronchitis alone (45%); the combination of doctor diagnosis of COPD, chronic bronchitis, or emphysema (18%); or self-reported history of COPD alone (9%).
Among seven cohorts reporting both allergic and non-allergic asthma, definitions for allergic asthma were asthma with hay fever (29%), asthma with hay fever and/or eczema (14%), asthma with rhinitis and other allergic diseases (14%), asthma with positive Phadiatop test (14%), asthma with atopy or fractional exhaled nitric oxide (FeNO) >50 ppb (14%), or asthma with three or more positive responses to a skin-prick test (14%).
Statistical Analysis
Our statistical analysis focused on descriptive statistics of health outcomes. We integrated the summary statistics from all cohorts to create summary tables. To describe the distribution of respiratory outcomes among the cohorts, we calculated the median, interquartile range (IQR), and total range for prevalence of respiratory symptoms and diseases, for cohorts as a whole and then by gender. Reported medians were not weighted by cohort size, and reflect the 50th percentile of individual cohort prevalence estimates. To assess the relative prevalence of allergic to non-allergic asthma, gender-stratified prevalence ratios and corresponding 95% confidence intervals were calculated for each cohort. Analysis was completed in SAS 9.4 and figures developed in R.
Results
Cohort Characteristics
A total of 18 cohorts from 11 countries participated, including 118,520 men and 92,712 women (N=211,232) from both crop and livestock farming populations. Cohorts had a wide geographic spread, including populations from six continents (Figure 1). Participants include farmers, farm workers, subsistence farmers, and rural residents. Agricultural activities range from large scale industrial agriculture to rural fruit and farmworkers in Africa (supplement 2). The majority of the cohorts were based in high-income countries (14/18, 78%), while three (17%) were based in upper-middle-income, and one (6%) in a low-income country.
Figure 1:
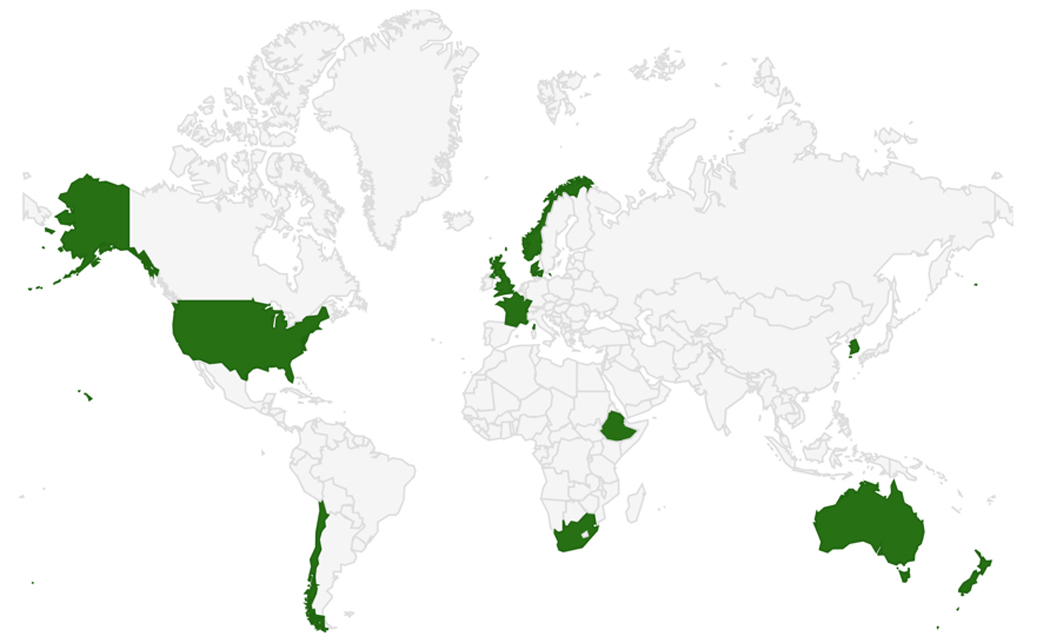
World map of included AGRICOH Countries
The cohorts ranged in size from 206 to 128,388 participants: six (33%) included fewer than 1,000 participants; ten studies (56%) included 1,000–10,000 participants; and two (11%) included greater than 10,000 participants (Table 1). The majority of cohorts featured a greater proportion of males; however, two cohorts (KwaZulu-Natal Crop Farmers [14] and Western Cape Fruit Farm Workers [15]) included only female farm workers. The median proportion of males among cohorts was 60% (Interquartile Range (IQR): 44–78%). Among all cohorts, ages ranged from 15 to 105 years, with a median cohort-specific age of 51 years (IQR: 40.7–55.5).
Table 1:
Characteristics of the AGRICOH cohorts that included respiratory outcomes
| Cohort | Country | Sample Size | Year‡ | Male (%) | Mean Age (std) | Age Range | Smoking (%)+ |
BMI (%)+ |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Never | Past | Current | <20 | 20 - <25 | 25 - <30 | ≥30 | ||||||||
| Africa | ||||||||||||||
| Ethiopia13 | Ethiopia | 206 | 2014 | 69 | 27 (7) | 15–57 | 95 | 0 | 5 | 32 | 56 | 11 | 1 | |
| KwaZulu-Natal Crop Farmers14 | South Africa | 911 | 2006 | 0 | 42 (13) | 18–82 | 94 | 0 | 6 | NR | NR | NR | NR | |
| Western Cape Fruit Farm Workers15 | South Africa | 211 | 2009 | 0 | 37 (12) | 17–73 | 50 | 0 | 50 | 17 | 28 | 22 | 33 | |
| North West Poultry Workers16 | South Africa | 230 | 2012 | 68 | 37 (9) | 21–68 | 56 | 1 | 43 | 17 | 48 | 17 | 17 | |
| Asia | ||||||||||||||
| KMCC17 | Korea | 8,431 | 2004 | 44 | 58 (10) | 19–91 | 60 | 11 | 29 | 14 | 65 | 18 | 3 | |
| Europe | ||||||||||||||
| AGRICAN18 | France | 128,388 | 2007 | 56 | 65 (15) | 20–105 | 65 | 27 | 9 | 4 | 37 | 44 | 15 | |
| BM3R19 | France | 5,095 | 2013 | 59 | 57 (9) | 40–75 | 65 | 22 | 14 | 4 | 46 | 31 | 19 | |
| FERMA20 | France | 473 | 2012 | 71 | 47 (12) | 18–78 | 55 | 24 | 21 | 8 | 45 | 29 | 17 | |
| Franche-Comte Farmers21 | France | 915 | 2006 | 74 | 55 (11) | 30–80 | 62 | 24 | 15 | 2 | 49 | 32 | 17 | |
| Norwegian Farmers22 | Norway | 4,735 | 2009 | 60 | 49 (11) | 21–69 | 50 | 22 | 28 | 2 | 43 | 44 | 11 | |
| PIPAH23 | United Kingdom | 4,536 | 2014 | 98 | 54 (12) | 19–88 | 65 | 26 | 9 | 2 | 41 | 44 | 13 | |
| SUS Study24 | Denmark | 1,964 | 1992 | 88 | 19 (3) | 17–49 | 70 | 0 | 30 | NR | NR | NR | NR | |
| North America | ||||||||||||||
| AHS* | USA | 39,464 | 2016 | 53 | 65 (11) | 32–104 | 68 | 27 | 5 | 3 | 22 | 40 | 35 | |
| Farmer Health Study25 | USA | 1,947 | 1993 | 90 | 54 (13) | 21–90 | 55 | 32 | 12 | NR | NR | NR | NR | |
| KCRHS26 | USA | 1,256 | 1997 | 44 | 52 (16) | 18–92 | 62 | 24 | 15 | 3 | 31 | 31 | 36 | |
| Oceania | ||||||||||||||
| New Zealand27 | New Zealand | 4,288 | 2005 | 52 | 49 (11) | 20–93 | 58 | 30 | 12 | 4 | 36 | 44 | 17 | |
| Victorian Grain Farmers28 | Australia | 1,102 | 1995 | 100 | 51 (13) | 19–90 | 57 | 13 | 30 | NR | NR | NR | NR | |
| South America | ||||||||||||||
| MAUCO29 | Chile | 7,080 | 2015 | 39 | 54 (10) | 36–77 | 45 | 23 | 31 | 1 | 16 | 44 | 40 | |
Data not yet published
Percentages may not add up to 100% due to rounding
If multiple years included in cohort, the last year of data collection is provided
BMI, body mass index; NR, not reported
KMCC, Korean Multi-center Cancer Cohort; AHS, Agricultural Health Study; GDMSP, Grain Dust Medical Surveillance Program; KCRHS, Keokuk County Rural Health Study
Covariates
We collected data on two common risk factors for respiratory outcomes: smoking and body mass index (BMI). The prevalence of smoking varied among the cohorts. The prevalence of current smoking ranging between 5% and 50%, with a median of 15% (IQR: 9%−30%) (Table 1 and supplement 3). There were no apparent differences in smoking prevalence between industrialized and non-industrialized countries or by geographic region. Smoking varied by gender, with current smoking prevalence consistently higher among males (median = 17% [IQR: 9%−30%]) compared to females (median = 11% [IQR: 7%−22%]). For BMI, the proportion of obese individuals ranged from 1% to 40% (median = 17% [IQR: 13%−33%]), and overweight individuals ranged from 11% to 44% (median = 31% [IQR: 21%−44%]). Higher proportions of underweight participants were more common among KMCC [17] and African cohorts [13–16] (Table 1 and supplement 4).
Respiratory Symptoms
We collected data on cough, phlegm, and wheeze. Most cohorts collected data on all three of these outcomes (10 of 18); 72% of cohorts provided data on cough, 61% on phlegm, and 61% on wheeze. Respiratory symptoms were common in all cohorts (Supplement 5a). The median prevalence was 18.6% (IQR: 14.4–30.0%) for cough, 13.3% (IQR: 7.8–18.8%) for phlegm, and 15.0% (IQR: 8.8–16.1%) for wheeze. Farmworkers from South Africa (Western Cape Fruit Farm Workers [15] and North West Poultry Workers [16]) and France (FERMA [20]) had the highest prevalence of cough and phlegm among all cohorts. Western Cape Fruit Farm workers also had the highest prevalence of wheeze (31%), while the farmers in the AHS in the United States had the second highest prevalence of wheeze (22%). When the data were stratified by gender (Figures 2a, 2b, 2c, Supplement 5b), males were more likely to report respiratory symptoms than females, though the IQR for the median values overlapped between males and females.
Figure 2:
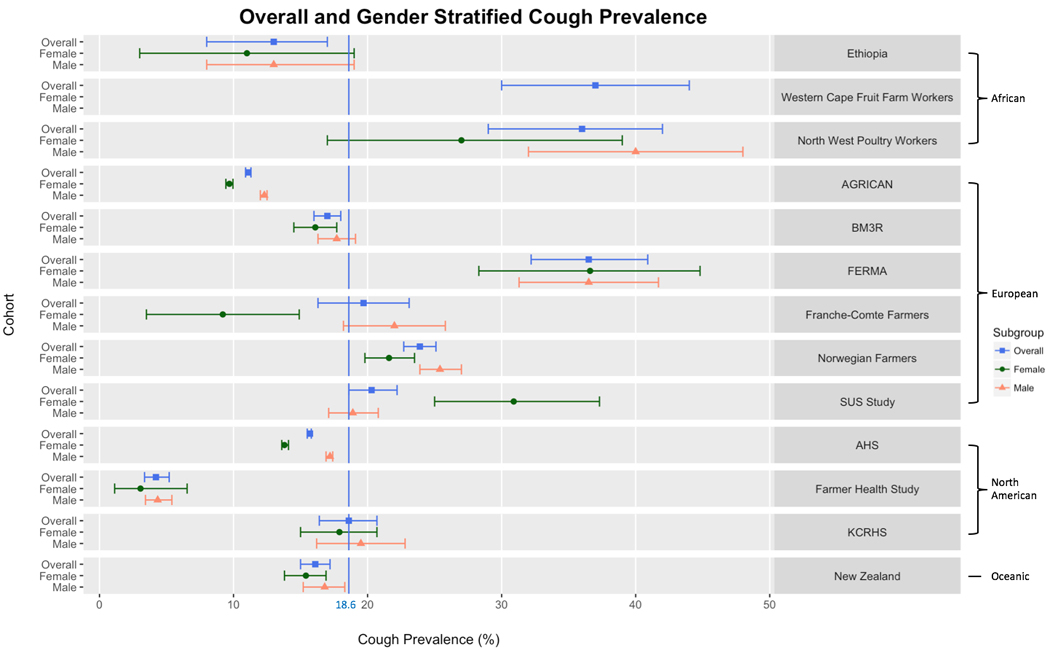
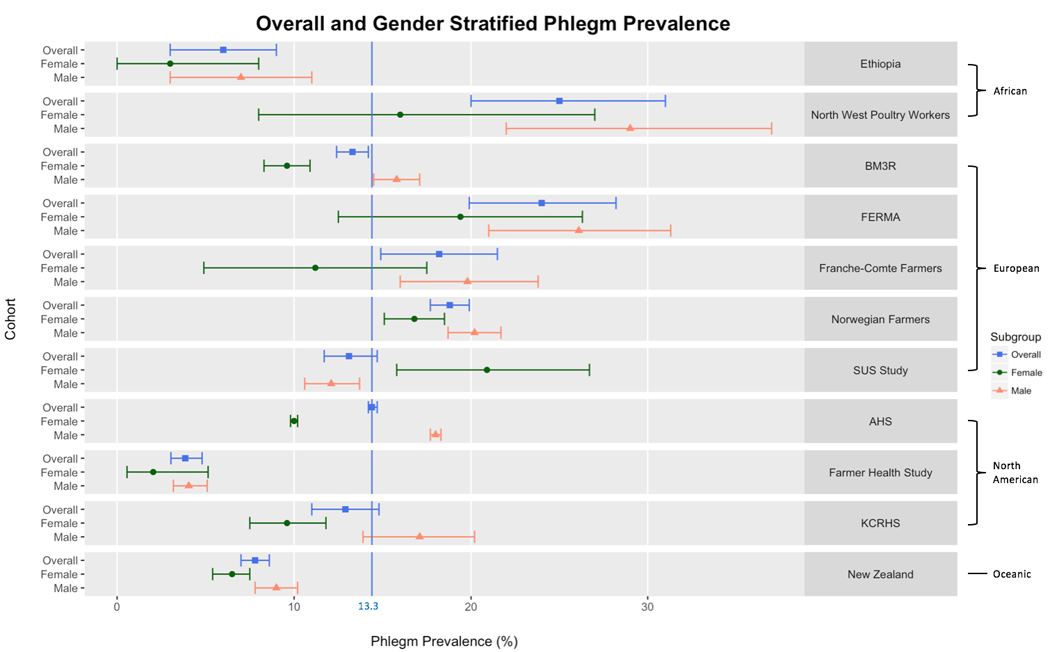
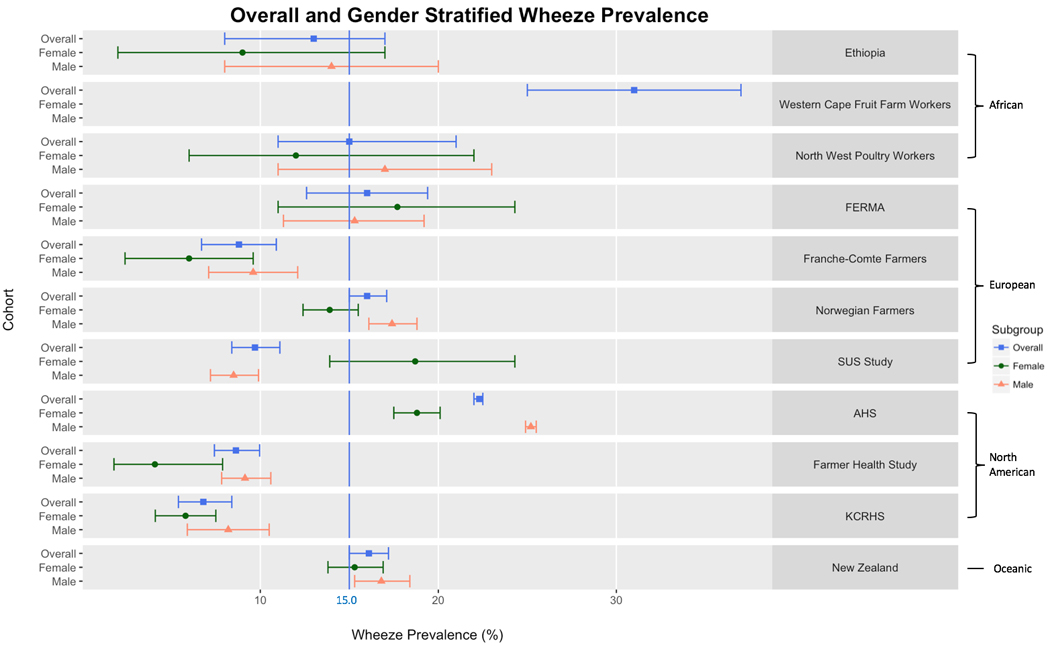
Overall and gender-stratified (a) cough prevalence, phlegm prevalence (b), and wheeze prevalence (c) among AGRICOH cohorts.
Respiratory Diseases
We collected data on asthma, allergic asthma, non-allergic asthma, and COPD based on each cohort’s definitions (Supplement 6a). All cohorts provided data on asthma, and 39% provided information on allergic phenotypes. 83% of cohorts provided information on COPD.
The median prevalence of asthma was 7.2% (IQR 5.7%−10.1%) with individual study values ranging from 0.5% in the Ethiopian [13] cohort to 16.0% among Victorian Grain Farmers [28] in Australia. Differences in asthma prevalence by gender did not follow the same trend as observed for symptoms (Figures 3a and 3b). The median prevalence was slightly higher among females (7.8% [IQR:6.5%−10.5%]) compared with males (6.5% [IQR: 4.0%−11.3%]).
Figure 3:
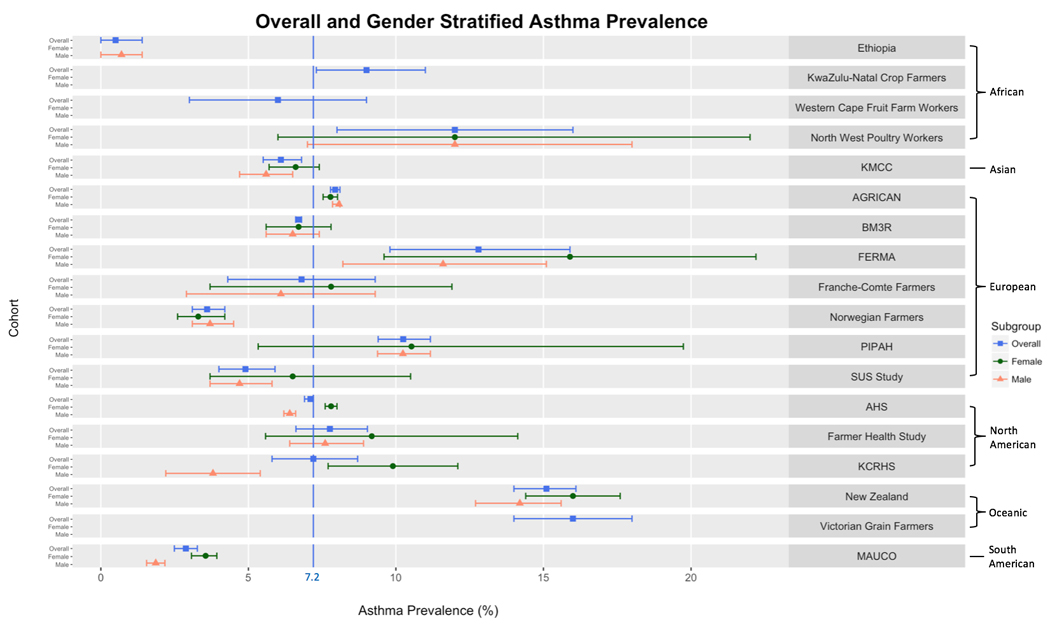
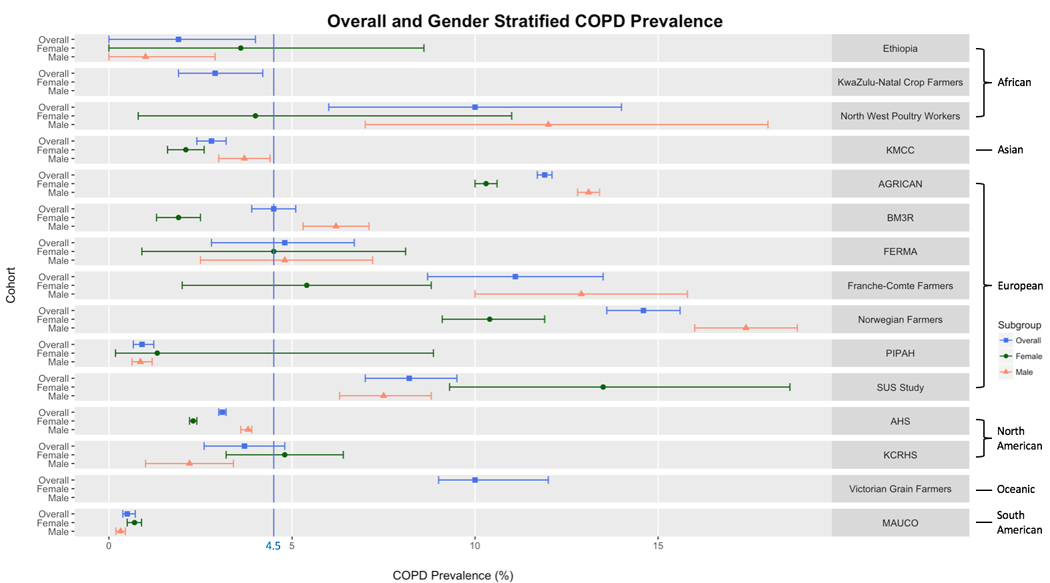
Overall and gender-stratified asthma prevalence (a) and COPD prevalence (b) among AGRICOH cohorts.
In the seven cohorts with data on allergic and non-allergic asthma, allergic asthma (5.0% [IQR:3.0%−5.1%]) was more common than non-allergic asthma (2.0% [IQR:1.9%−7.0%]). This trend persisted after stratifying by gender; the median prevalence of allergic and non-allergic asthma among females was 5.5% and 3.5%, respectively, while among men, the median prevalence was 3.6% for both allergic and non-allergic asthma. Among the gender-stratified results, we also observed that women had higher prevalence ratios (PRs) than men, comparing allergic to non-allergic asthma (Figure 4). Upon aggregating data across all cohorts, women (PR: 1.01 [95% CI: 0.95–1.06]) had a significantly higher prevalence ratio of allergic to non-allergic asthma compared to men (PR: 0.76 [95% CI: 0.72–0.82]), indicating that allergic asthma and non-allergic asthma prevalence were similar in women, but that men were less likely to have allergic asthma.
Figure 4:
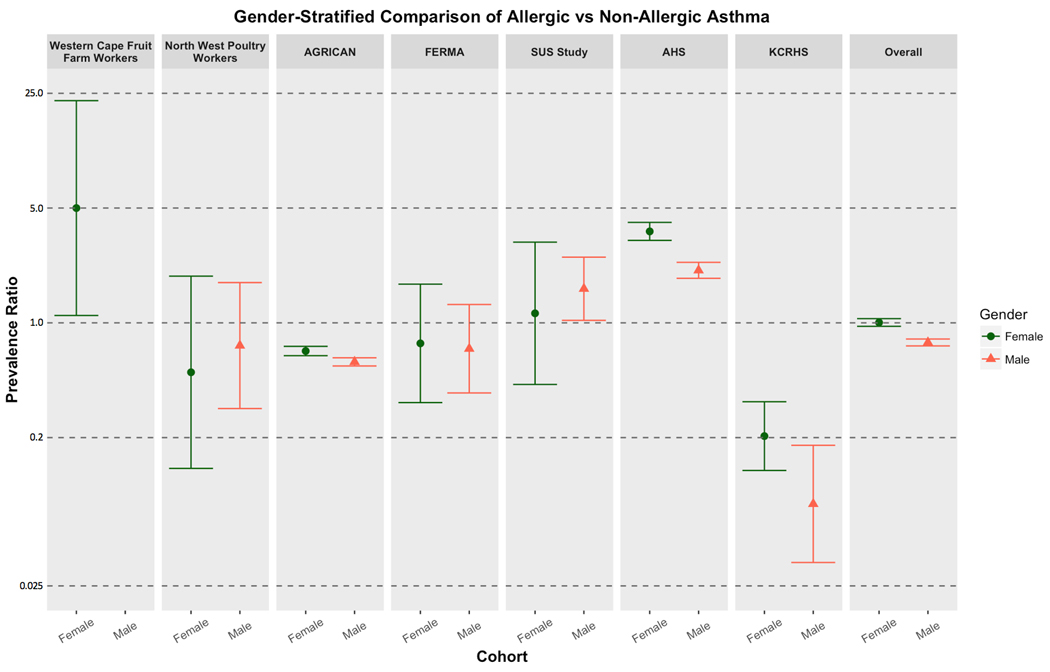
Gender-stratified ratio of allergic vs. non-allergic asthma within AGRICOH cohorts.
Information on COPD was provided by 14 of 18 cohorts. One third of the cohorts used spirometry to classify COPD; the remaining two thirds used self-reported doctor diagnosis of at least one of these three outcomes (chronic bronchitis, emphysema, or COPD). The median prevalence of COPD among all cohorts was 4.5% [IQR: 2.8%−10.0%]) with COPD prevalence ranging from 0.5% in the MAUCO [29] cohort to 14.6% among Norwegian [22] farmers. The studies that reported using spirometry to estimate COPD prevalence had values ranging from 1.9% to 14.6% [median = 10.0% [IQR: 4.5%−11.1%]; studies that used self-reported prevalence had values ranging from 0.5 to 11.9% for COPD [median = 3.7% [IQR: 2.8%−10.0%]. When we stratified the COPD data by gender, the median prevalence for males was 5.5% (IQR: 1.9%−12.2%) and for females was 4.0% (IQR: 2.0%−7.9%) (Supplement 6b).
Discussion
Using the data from 18 agricultural cohorts from around the world, we sought to characterize the prevalence of respiratory symptoms and diseases among the AGRICOH consortium as indicators of respiratory health among farmers worldwide with particular focus on differences by gender. In this analysis, respiratory symptoms were common and higher among men than women; while respiratory diseases were less common and women had a higher prevalence of asthma and men had higher prevalence of COPD. Although farming practices differ around the world, we found that the prevalence of these respiratory outcomes did not vary substantially between cohorts with any notable trends by region.
The 18 cohorts included here represent a small subset of agricultural workers worldwide. No comprehensive study of agricultural workers using a common protocol around the world has been conducted. While large, our sample is by no means comprehensive and the representation between developed and developing countries is uneven. Some cohorts included a relatively small number of farmers and focused only on specific types of farming, such as the all-female Western Cape Fruit Farmers [15] cohort in South Africa, while others featured much larger populations that included a wide variety of types of farming activities as well as spouses of farmers (e.g., AHS, AGRICAN, and Norwegian Farmers). Overall, the average age among our cohort members (56.8 years) is similar to the average age of farmers in both developed countries and across Africa (60 years), as reported by the Food and Agriculture Organization of the United Nations in 2014 [33].
Overall, males reported more respiratory symptoms than women, but this was not true for every cohort. In general population samples, such as the National Health and Nutrition Examination Survey (NHANES) in the United States, the prevalence of wheeze and cough is similar in men and women while the prevalence of phlegm is much more common in men [34]. Here we observe greater differences between men and women in cohorts limited to specific farm activities, such as poultry work, with a high potential for exposure to respiratory irritants (e.g., Northwest Poultry Workers). We were unable to evaluate specific farming practices due to both the small number of cohorts and the complex exposure experience of individuals within the larger cohorts (e.g., AHS, AGRICAN). Occupational exposures and the types of tasks that men are more likely to engage in may contribute to this higher outcome prevalence [3]. Smoking is more common in men, and that may also contribute to some of the observed differences. However, in our study sample, there is more variability in the prevalence of symptoms by cohort rather than between men and women, suggesting different baseline rates of symptoms in different populations as well as differences in type of farming and related exposures.
Asthma prevalence was higher in women agricultural workers, likely due to the higher prevalence of allergic asthma in women. Similarly, women around the world have a higher prevalence of asthma than men. In an earlier analysis of AHS data from 2005–2010, women in the AHS had more asthma than men in the AHS, but lower prevalence of asthma compared to the US population [35]. This may be due to factors associated with who becomes a farmer (for example, people with a history of asthma may choose a different profession) as well as agricultural exposures that appear to reduce allergic outcomes in farmers and their families [3,8,36]. The prevalence of asthma among our cohorts ranged from <1% to 16% with a median prevalence of 7.2%. Globally, asthma prevalence in adults aged 18–45 from 70 countries in 2002–2003 ranged from 0.2 (China) to 21% (Australia) with an overall prevalence of 4.3% [37]. While that study did not include all the same countries included here, it suggests that farmers may have a higher prevalence of asthma than the general population. Surprisingly, we observed a higher prevalence of allergic asthma than non-allergic asthma in the cohorts with data on this outcome (5.0% vs. 2.0%); this difference may have been due to higher prevalence of asthma in women and that women had a higher prevalence of allergic asthma. There is an extensive literature suggesting that farmers have a lower prevalence of allergic asthma [3,4,38]. We cannot evaluate whether our findings are due to the diversity of our cohorts over continents and agricultural practices, or due the primarily cross-sectional data used, or the fact that allergy may have been assigned based on questionnaire information. Future studies should focus on better characterization of allergic asthma.
The COPD results highlight the challenge of combining data across cohorts when disease definitions vary greatly, as has been reported by others [39]. Among the 15 cohorts that evaluated COPD prevalence, six different definitions of COPD were employed. COPD is classified based both on symptoms (chronic cough and phlegm) as well as airway obstruction as assessed through spirometry [40]. COPD encompasses the spectrum of obstructive diseases and includes chronic bronchitis and emphysema. Not all cohorts used spirometry to diagnose COPD, but rather relied on doctor diagnosis of COPD. This will capture individuals who have been diagnosed accurately by their physician, but will miss those who have not had this detailed clinical work up; suggesting a sensitive, but not specific outcome. Additionally, it will capture those who received a diagnosis but did not meet the clinical criteria, creating false positives [41]. Within an individual cohort, these biases may behave in the same manner, but between cohorts the factors that influence diagnosis and over reporting may differ making it almost impossible to combine across these studies.
Although this study importantly characterizes farming cohorts around the world, it does feature some limitations. Comparability between cohorts may be limited due to differences in study year, ranging from 1992 to 2016. Cohorts ranged from small, focused cohorts with detailed information on a specific type of agriculture to large studies that include farmers engaged in a wide variety of activities. In choosing to include as many cohorts as possible, we forfeit the ability to focus on specific types of agriculture or agricultural practices. Participating cohorts provided demographic and symptom and disease metadata, but did not share participant-level data. As a result, the prevalence estimates reported are not adjusted or standardized to account for important confounding variables such as smoking, age, status, income, education, and farming practices. While the AGRICOH consortium includes cohorts from around the world, the analysis was limited to those 15 cohorts, and three additional ones that evaluated respiratory symptoms and diseases around the world. Consequently, our descriptive analysis only features study populations from 11 countries, and more work is needed to truly characterize the global burden of respiratory outcomes in agricultural workers. Given that this study included only farmers, we were unable to make direct comparisons to the general public and assess the impact of agricultural production on respiratory health. The lack of national data on asthma prevalence makes it difficult to compare both within countries by occupation and between countries with regard to national prevalence. Global data on asthma prevalence will allow more rigorous analysis of variability by occupation and country.
International collaborative research provides valuable opportunities to investigate symptom and disease burden across many regions and geographic settings and diverse study populations. Future research would greatly benefit from sharing of participant-level data, allowing estimates to be standardized or adjusted for important confounders such as what is being done by the OMEGA NET consortium [42], and improving comparability between cohorts by applying common protocols like the ISAAC study for children [43] and the new DEGREE study for epidemiologic studies in low and middle income populations [44]. Data harmonization and standardization are not trivial tasks and we were unable to perform these at this time.
Asthma and COPD are important contributors to morbidity and mortality worldwide [39]. Our analysis shows that farmers and agricultural workers are impacted by these health outcomes. Agriculture represents a complex exposure environment and respiratory diseases are multi-factorial in nature. As a result, it is difficult to identify specific etiologic factors that contribute to or protect against respiratory disease. However, in these diverse cohorts, adult respiratory disease and symptoms were common and, it is likely that occupation contributed to these outcomes. The United Nation’s International Labour Organization estimated in 2009 that there were about 1.07 billion people employed in agriculture around the world, accounting for nearly 35% of the global workforce [45]. Therefore, understanding the global impacts of agricultural production on respiratory health is critical.
Supplementary Material
Acknowledgements:
This work was supported by Dr. Hoppin’s startup funds at NC State University. The Keokuk County Rural Health Study was supported by Grants # U07/CCU706145 (Round 1) and #U50 OH07548 (Round 2 and Round 3) from the National Institute for Occupational Safety and Health to the Great Plains Center for Agricultural Health, The University of Iowa. This research was supported in part by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences (Z01-ES049030). KwaZulu-Natal was supported by the South African Netherlands Research Program on Alternatives in Development (SANPAD) and the South African Medical Research Council (SA MRC) – grant number 04/15. MAUCO was supported by Conicyt – FONDAP No 15130011.
References
- 1.Schenker MB, Christiani D, Cormier Y, et al. Respiratory health hazards in agriculture. Am J Respir Crit Care Med. 1998;158(5):S1–S76. [DOI] [PubMed] [Google Scholar]
- 2.Kirkhorn SR, Garry VF. Agricultural lung diseases. Environ Health Perspect. 2000. August;108 Suppl 4:705–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eduard W, Douwes J, Omenaas E, et al. Do farming exposures cause or prevent asthma? Results from a study of adult Norwegian farmers. Thorax. 2004. May;59(5):381–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eduard W, Omenaas E, Bakke PS, et al. Atopic and non-atopic asthma in a farming and a general population. Am J Ind Med. 2004. October;46(4):396–9. [DOI] [PubMed] [Google Scholar]
- 5.Hoppin JA, Umbach DM, London SJ, et al. Pesticides and atopic and nonatopic asthma among farm women in the Agricultural Health Study. Am J Respir Crit Care Med. 2008. January 1;177(1):11–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoppin JA, Umbach DM, London SJ, et al. Pesticide use and adult-onset asthma among male farmers in the Agricultural Health Study. Eur Respir J. 2009. December;34(6):1296–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoppin JA, Umbach DM, Long S, et al. Pesticides Are Associated with Allergic and Non-Allergic Wheeze among Male Farmers. Environ Health Perspect. 2016. July 06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.von Mutius E. The environmental predictors of allergic disease. J Allergy Clin Immunol. 2000;105(1 Pt 1):9–19. [DOI] [PubMed] [Google Scholar]
- 9.Schachter EN, Zuskin E, Moshier EL, et al. Gender and respiratory findings in workers occupationally exposed to organic aerosols: a meta analysis of 12 cross-sectional studies. Environ Health. 2009. January 12;8:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Senthilselvan A, Chenard L, Ulmer K, et al. Excess respiratory symptoms in full-time male and female workers in large-scale swine operations. Chest. 2007. April;131(4):1197–204. [DOI] [PubMed] [Google Scholar]
- 11.Motika CA, Papachristou C, Abney M, et al. Rising prevalence of asthma is sex-specific in a US farming population. J Allergy Clin Immunol. 2011. October;128(4):774–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leon ME, Beane Freeman LE, Douwes J, et al. AGRICOH: a consortium of agricultural cohorts. International journal of environmental research and public health. 2011. May;8(5):1341–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Negatu B, Kromhout H, Mekonnen Y, et al. Occupational pesticide exposure and respiratory health: a large-scale cross-sectional study in three commercial farming systems in Ethiopia. Thorax. 2017. June;72(6):498–499. [DOI] [PubMed] [Google Scholar]
- 14.Naidoo S, London L, Burdorf A, et al. Agricultural activities, pesticide use and occupational hazards among women working in small scale farming in Northern KwaZulu-Natal, South Africa. Int J Occup Environ Health. 2008. Jul-Sep;14(3):218–24. [DOI] [PubMed] [Google Scholar]
- 15.Mwanga HH, Dalvie MA, Singh TS, et al. Relationship between Pesticide Metabolites, Cytokine Patterns, and Asthma-Related Outcomes in Rural Women Workers. Int J Environ Res Public Health. 2016. September 27;13(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ngajilo D, Singh T, Ratshikhopha E, et al. Risk factors associated with allergic sensitization and asthma phenotypes among poultry farm workers. Am J Ind Med. 2018. March 25. [DOI] [PubMed] [Google Scholar]
- 17.Yoo KY, Shin HR, Chang SH, et al. Korean Multi-center Cancer Cohort Study including a Biological Materials Bank (KMCC-I). Asian Pac J Cancer Prev. 2002;3(1):85–92. [PubMed] [Google Scholar]
- 18.Baldi I, Robert C, Piantoni F, et al. Agricultural exposure and asthma risk in the AGRICAN French cohort. Int J Hyg Environ Health. 2014. Apr-May;217(4–5):435–42. [DOI] [PubMed] [Google Scholar]
- 19.Guillien A, Puyraveau M, Soumagne T, et al. Prevalence and risk factors for COPD in farmers: a cross-sectional controlled study. Eur Respir J. 2016. January;47(1):95–103. [DOI] [PubMed] [Google Scholar]
- 20.Audi C, Baiz N, Maesano CN, et al. Serum cytokine levels related to exposure to volatile organic compounds and PM2.5 in dwellings and workplaces in French farmers - a mechanism to explain nonsmoking COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:1363–1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gainet M, Thaon I, Westeel V, et al. Twelve-year longitudinal study of respiratory status in dairy farmers. Eur Respir J. 2007. July;30(1):97–103. [DOI] [PubMed] [Google Scholar]
- 22.Eduard W, Pearce N, Douwes J. Chronic bronchitis, COPD, and lung function in farmers: the role of biological agents. Chest. 2009. September;136(3):716–725. [DOI] [PubMed] [Google Scholar]
- 23.Harding AH, Fox D, Chen Y, et al. Prospective Investigation of Pesticide Applicators’ Health (PIPAH) study: a cohort study of professional pesticide users in Great Britain. BMJ Open. 2017. October 10;7(10):e018212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sigsgaard T, Hjort C, Omland O, et al. Respiratory health and allergy among young farmers and non-farming rural males in Denmark: the SUS study. J Agromedicine. 2004;9(2):223–38. [PubMed] [Google Scholar]
- 25.Schenker MB, Farrar JA, Mitchell DC, et al. Agricultural dust exposure and respiratory symptoms among California farm operators. J Occup Environ Med. 2005. November;47(11):1157–66. [DOI] [PubMed] [Google Scholar]
- 26.Merchant JA, Stromquist AM, Kelly KM, et al. Chronic disease and injury in an agricultural county: The Keokuk County Rural Health Cohort Study. J Rural Health. 2002. Fall;18(4):521–35. [DOI] [PubMed] [Google Scholar]
- 27.Douwes J, Travier N, Huang K, et al. Lifelong farm exposure may strongly reduce the risk of asthma in adults. Allergy. 2007. October;62(10):1158–65. [DOI] [PubMed] [Google Scholar]
- 28.Macfarlane E, Chapman A, Benke G, et al. Training and other predictors of personal protective equipment use in Australian grain farmers using pesticides. Occup Environ Med. 2008. February;65(2):141–6. [DOI] [PubMed] [Google Scholar]
- 29.Ferreccio C, Roa JC, Bambs C, et al. Study protocol for the Maule Cohort (MAUCO) of chronic diseases, Chile 2014–2024. BMC Public Health. 2016. February 04;16:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Development Indicators 2017. Washington, D.C.: World Bank; 2017. [Google Scholar]
- 31.Ferris BG. Epidemiology Standardization Project (American Thoracic Society). Am Rev Respir Dis. 1978. December;118(6 Pt 2):1–120. [PubMed] [Google Scholar]
- 32.Heinrich J, Richter K, Frye C, et al. [European Community Respiratory Health Survey in Adults (ECRHS)]. Pneumologie. 2002. May;56(5):297–303. [DOI] [PubMed] [Google Scholar]
- 33.FAO. Food Security for sustainable development and urbainzation. 2014. [Google Scholar]
- 34.(CDC) Centers for Disease Control and Prevention NCfHS. NHANES 1999–2000 Data Files 2005. [cited 2005 October 19, 2005]. Available from: http://www.cdc.gov/nchs/about/major/nhanes/nhanes99_00.htm
- 35.Hoppin JA, Umbach DM, Long S, et al. Respiratory disease in United States farmers. Occup Environ Med. 2014;71(7):484–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vogelzang PF, van der Gulden JW, Tielen MJ, et al. Health-based selection for asthma, but not for chronic bronchitis, in pig farmers: an evidence-based hypothesis. Eur Respir J. 1999;13(1):187–9. [DOI] [PubMed] [Google Scholar]
- 37.To T, Stanojevic S, Moores G, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012. March 19;12:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elholm G, Schlunssen V, Doekes G, et al. Become a farmer and avoid new allergic sensitization: adult farming exposures protect against new-onset atopic sensitization. J Allergy Clin Immunol. 2013. November;132(5):1239–41. [DOI] [PubMed] [Google Scholar]
- 39.Collaborators GBDCRD. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017. September;5(9):691–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Luize AP, Menezes AM, Perez-Padilla R, et al. Assessment of five different guideline indication criteria for spirometry, including modified GOLD criteria, in order to detect COPD: data from 5,315 subjects in the PLATINO study. NPJ Prim Care Respir Med. 2014. October 30;24:14075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bobadilla A, Guerra S, Sherrill D, et al. How accurate is the self-reported diagnosis of chronic bronchitis? Chest. 2002. October;122(4):1234–1239. [DOI] [PubMed] [Google Scholar]
- 42.Turner MC, Mehlum IS. Greater coordination and harmonisation of European occupational cohorts is needed. Occup Environ Med. 2018. July;75(7):475–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.ISAAC Steering Committee. International Study of Asthma and Allergies in Childhood. ISAAC Phase One Manual. : Auckland/Munster; 1993. [Google Scholar]
- 44.Caplin B, Jakobsson K, Glaser J, et al. International Collaboration for the Epidemiology of eGFR in Low and Middle Income Populations - Rationale and core protocol for the Disadvantaged Populations eGFR Epidemiology Study (DEGREE). BMC Nephrol. 2017. January 3;18(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kapsos S, Sparreboom T. The challeng of a jobs recovery. Geneva: International Labour Office; 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


