Abstract
College student alcohol use and associated negative consequences are clear public health problems with consequences including damage to self, others, and institutions. This paper describes the protocol of a research study designed to answer a number of important questions in the development of an adaptive preventive intervention (API) to reduce high-risk drinking among first-year college students. The API is designed to educate students and to motivate heavy-drinking college students to engage in existing resources to support reducing high-risk alcohol use, by leveraging technology-based intervention modalities. The primary outcome is a reduction in binge drinking, with secondary outcomes of reducing negative alcohol-related consequences and increasing health services utilization. Adaptive preventive interventions have the potential to reduce the acute and long-term negative health consequences of young adult alcohol use.
Keywords: alcohol, drinking, online, adaptive, web, college
Introduction
College student alcohol use, with consequences including damage to self, others, and institutions [1,2], is a public health problem [3,4]. About 20% of college students have an alcohol use disorder [5]. First-year college students are at particularly high risk [6], and prevention is needed. Preventive interventions are divided into subcategories [7]. Universal interventions are intended for an entire population, and indicated interventions target individuals who are exhibiting signs of problem behavior [7]. Effective universal and indicated interventions for alcohol use are available [8], with brief motivational interventions showing the largest effects [8–11] reducing alcohol use and consequences among college students [12]. However, empirically-validated interventions are underutilized, partly because of college students’ perceptions that alcohol use is not problematic [13,14]. Further, young adults are often not offered counseling [15], and are less likely to be advised to reduce their alcohol use [16]. Internet-based versions of brief interventions, such as Web-BASICS, are resource-efficient and have effects that may be as good as in-person interventions [6,17]. Additionally, the majority of college students already use the internet to find health information [18,19]. Therefore, technology-based approaches to increase utilization of empirically-supported interventions by identifying students in need of indicated intervention and offering online and mobile content that is attractive to students.
A promising way to increase prevention and intervention engagement in a resource-efficient manner is to: 1) utilize a universal preventive intervention (given to everyone), 2) identify students at high risk who do not respond adequately to the universal intervention, and 3) encourage these students to access indicated intervention (and continue monitoring the students not (yet) identified as high risk). This approach is ‘adaptive’ [20] because information about the student in the course of the intervention is used to determine whether more resources should be invested to transition (i.e., bridge) them to indicated intervention. We refer to this as adaptive preventive intervention (API).1 API is conceptually consistent with multi-tiered intervention frameworks [21–23] and stepped-care approaches to intervention that provide low-intensity (minimal support) interventions that are augmented for individuals showing signs of non-response [24–28]. By providing appropriate intervention only to those who need it, when they need it, APIs have potential to cost-efficiently improve outcomes and increase the reach and scalability of alcohol use interventions [29,30].
There are several open scientific questions related to how best to operationalize an API to prevent or reduce drinking among first-year college students. A first key question is timing. Brief interventions are often offered after students arrive on campus (e.g., [31,32]), but an alternative is to offer them before classes begin to inoculate students with accurate information before they are bombarded by campus influences. Students who receive normative information have not escalated into college drinking yet, so there may be a window of opportunity to change their perceptions. A second key question is how best to transition such students (i.e., heavy drinkers) to evidence-based indicated interventions, which are often available on college campuses [8]. To address these questions, a sequential multiple assignment randomized trial (SMART) design is employed whereby participants are randomized at two stages: first to one of two points in time at which the universal intervention is offered; and, second, among students identified to be at high risk following universal intervention, to one of two intervention options for linking them to an indicated intervention [33,34]. The purpose of this paper is to describe the protocol for a SMART study involving sequential randomization yielding four APIs that are embedded in the experimental design.
Methods
Design Overview
This study (called M-bridge for participants) is the first to test and optimize different components of an API that transitions from universal to indicated resources to reduce heavy drinking and related consequences among college students. Two low-cost, low-burden technology-based universal interventions are personalized normative feedback (PNF) and self-monitoring (SM) of alcohol use [8]. Both are offered to all students in a combined universal preventive intervention (PNF+SM) but we will compare the timing of its delivery: before or after the start of the Fall college semester. Students who continue to drink heavily during the first semester of college despite PNF+SM are in need of indicated intervention. This study will compare two strategies for linking such students to indicated interventions: (1) resource emails to provide information about available online and in-person resources, maintaining student confidentiality and not requiring human interaction (i.e., a trained clinician), or (2) a more interactive, but costlier, approach involving an online dialogue with a health coach to motivate the student to utilize available resources.
M-bridge employs a SMART experimental design during the first year of college, with interventions taking place before and/or during the first semester and final follow-up the following fall (semester three). At baseline, 1/3 of participants will be randomized to the control group. Of those randomized to intervention, half (1/3 of the total sample) will be randomized to receive an API pre-college (early group) and half (1/3 of the total sample) will be randomized to receive an API during college (late group). The early group will begin their universal intervention (PNF+SM) prior to the start of the first semester, while the late group will begin during month one of the first semester. Students randomized to one of the API conditions who self-identify via SM as heavy drinkers (i.e., frequent binge drinking or high-intensity drinking) [35] are randomized a second time to receive an email that includes resource information (including a link to Web-BASICS) or an invitation to online health coaching. This randomization will occur as soon as a student flags for heavy drinking, so bridging to the indicated interventions will occur throughout the semester.
The sequential randomizations among students who were not assigned to “assessment only control” result in 4 APIs that are embedded in the trial by design (Figure 1 & Table 1).
Figure 1.
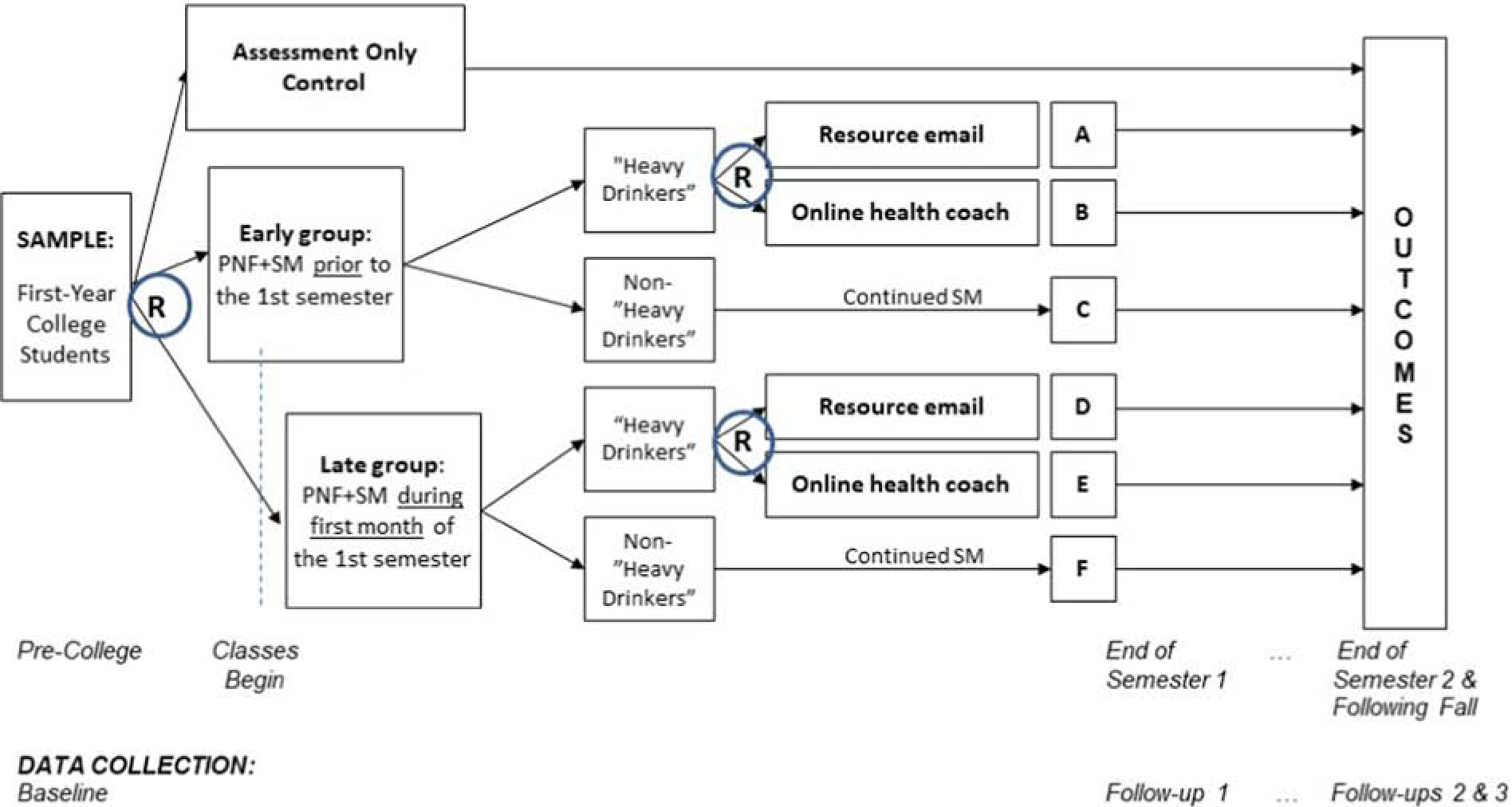
Study design
Table 1.
Four adaptive preventive interventions (API) embedded in the SMART. The shaded API (#1) is hypothesized to be optimal.
| API | Timing of PNF+SM | Heavy Drinker During First Semester? | Bridge to Indicated Resources | Cells (Figure 1) |
|---|---|---|---|---|
| 1 | Early group | Yes | Online health coach invitation | B+C |
| No | N/A (continued SM) | |||
| 2 | Early group | Yes | Resource email | A+C |
| No | N/A (continued SM) | |||
| 3 | Late group | Yes | Online health coach invitation | E+F |
| No | N/A (continued SM) | |||
| 4 | Late group | Yes | Resource email | D+F |
| No | N/A (continued SM) |
Aims
Aim 1 (Primary):
Examine the effect of APIs vs. assessment only on binge drinking (primary outcome) and negative drinking-related consequences and increased health services utilization (secondary outcomes). We hypothesized that students who are randomized to sequences of intervention consistent with any one of the API strategies will have reduced binge drinking (primary outcome) and reduced negative drinking-related consequences and increased health services utilization (secondary outcomes) compared to those randomized to assessment only up to one year later.
Aim 2 (Secondary):
Identify the most effective and cost-effective API of the four embedded in the SMART (see Table 1). We hypothesized that the API that provides PNF+SM before college followed by online health coaching for heavy drinkers (and continued monitoring for those who are not heavy drinkers) will lead to the lowest frequency of binge drinking and to greatest cost-effectiveness. This analysis corresponding to Aim 2 will also provide estimates of the effects of (a) the timing for PNF+SM universal prevention, and (b) the strategy (online health coach invitation [vs. resource email including a link for Web-BASICS]) for motivating heavy drinkers to utilize additional resources.
Aim 3 (Tertiary):
Identify ways to more specifically tailor the API by examining the effects of moderators, specifically pre-college (a) alcohol use norms or (b) intentions for college drinking, on the effect of the timing of PNF+SM; and college (c) high-intensity drinking (i.e., 8/10+ drinks for women/men) vs. binge (4/5+ drinks for women/men) during self-monitoring screening on the effect of resource email vs. online health coach in the transition to indicated intervention.
Participants and Setting
Incoming full-time college students aged 18–21 during academic year 2019–2020 at the University of Minnesota Twin Cities will be eligible for participation in M-bridge. Invitations will be sent to approximately 1,500 incoming first-year students randomly selected from the Registrar’s list of admitted students and invited to participate. A simple random sample will be drawn, which given the large sample size should be representative of the student demographics. We will compare demographics (i.e., race/ethnicity, age, gender, and college of enrollment) of the sample to the population from the Registrar’s list to ensure that there are no significant differences. Transfer students are not eligible for inclusion. As this is a pragmatic trial, no exclusion criteria were used. The University of Minnesota Twin Cities is a large (~31,000 undergraduates), public, comprehensive land-grant University located in Minneapolis and St. Paul, Minnesota. Approximately 90% of first-year students live on campus and the average ACT score is 28.
Enrollment, Consent, Randomization, and Research Assessments (Survey) Procedures
Students will be asked to participate in a baseline survey prior to their first semester of college (about 30 minutes in length) via mailed letter (with $5 pre-incentive enclosed) and email invitations. Based on prior experience, we estimate that 65% of contacted students will agree to participate, for a target N=700 students. The baseline survey will open for 3 weeks from the end of July until mid-August (classes begin 9/3/19). The beginning of the baseline survey will include online consent for the entire study. Participants will receive a $25 incentive after completing the survey.
Participants will be randomized using computer-generated, blocked randomization schemes for each of the two potential randomizations, available on a secure Web-based application. One third (1/3) of participants will be randomly assigned to assessment only control (no PNF+SM), and two thirds will be randomly assigned to APIs, which begin with PNF+SM. Of those assigned to APIs, half will be randomly assigned to the early group universal intervention (PNF+SM; students receive PNF 2 weeks before college classes start), and the other half will be assigned to late group universal intervention (PNF+SM; students receive PNF approximately 2 weeks after college classes start). That is, all participants will be randomly assigned initially to 1 of 3 groups in a 1:1:1 ratio: early group universal intervention vs. late group universal intervention vs. assessment only control.
Participants in the early group universal intervention will be invited to engage in PNF in mid-August and SM for 8 weeks from the beginning of September through the end of October; those in the late group universal intervention will be invited to PNF in mid-September and SM for 8 weeks from the beginning of October through the end of November. SM surveys will be sent to students every 2 weeks within the 8-week period. Email and text reminders will be sent 3 days after the survey is sent. Students may complete up to 4 SM surveys. Data from the SM will be collected using a secure Web-based application and used to determine whether the student is a “heavy drinker” (i.e., frequent binge drinking or high-intensity drinking, defined below). For each SM survey a participant completes, they will receive a $2 incentive and two entries to a drawing that will occur at the end of the semester (a total of 4 drawings for $500 each).
Students in the universal intervention groups who self-identify in SM as heavy drinkers are re-randomized to one of two approaches to motivate them to access indicated services: 1/2 to online health coach invitation vs. 1/2 to resource email. The second randomization will occur at the first reported occasion of binge or high-intensity drinking as soon as the survey is submitted, and participants will no longer receive SM surveys. Participants who do not report heavy drinking (including those with missing data) will continue to be sent SM surveys. Emails will be sent to randomized participants inviting them to utilize either online health coaching or Web-BASICS, with up to three email reminders sent over the course of Fall semester if they have not yet engaged. Wording of the email invitation and one of the reminders informs students that the invitation to participate is based on their previous survey responses.
The primary research outcome (survey-based report of binge drinking in the past month) and secondary research outcomes (alcohol-related consequences, health services utilization [e.g., online health coaching, Web-BASICS, campus clinics]) will be assessed with web-based surveys at the end of the first and second semesters of college and the following fall (one year later). Follow-up 1 at the end of Semester 1 (about 30 minutes), will be open the first 3 weeks of December (finals end 12/19/19). Follow-up 2 will be open during the last three weeks of Semester 2 (finals end 5/13/20). Follow-ups 1 and 2 will be open before and during finals week. Follow-up 3 the following fall will be open during the second and third week of classes (during September 2020). Participants will receive a $30 incentive after completing Follow-up 1, and a $35 incentive after completing Follow-ups 2 and 3.
All APIs will take place between August and December (i.e., immediately before or during first semester). Due to our questions about timing, and our design to move to indicated intervention immediately upon screening as a heavy drinking, there will be varying lengths of time in the intervention stages. However, the design and aims of the study are focused on the mode and timing versus the dosage of the interventions. While participants who flag early in the semester as a heavy drinker may have more time to engage with Web-BASICS or the online health coach, based on the scheduling of the SM surveys, there would be over 3 weeks for a participant who flags on the last possible day of SM surveys to engage with the bridging strategies and indicated interventions before Follow-up 1 closes.
Interventions
Universal Interventions
Personalized Normative Feedback (PNF).
Personalized normative feedback interventions target individuals’ perceived descriptive norms for alcohol use (i.e., their perceptions of peer alcohol use) by contrasting their perceptions with their own alcohol use and the actual normative behavior for their peer group. Norms will focus on prevalence of drinking, consuming 4/5+ drinks, total number of drinks consumed each week, and maximum drinks consumed. Normative information will be from the college student sample of the national Monitoring the Future (MTF) study [4] and the University of Minnesota Twin Cities campus [36]. Students will be sent a link to a website where they see their own personal responses in the feedback. Feedback will detail quantity and frequency of drinking (a) reported by the participant him/herself, (b) according to the participant’s perception of the descriptive norm for drinking quantity and frequency for the reference group (e.g., University of Minnesota first-year students, or typical college students), and (c) reflecting the actual descriptive norm for the reference group. For non-drinkers, the PNF will include the same information, even if they indicated no drinking. Prior work suggests that presenting personalized normative feedback as a component in mailed BASICS feedback to abstainers and light drinkers does not have an iatrogenic effect [37]. In fact, abstainers who received mailed BASICS feedback were twice as likely to remain abstinent from alcohol one year later than those in the assessment-only control group.
Participants will be sent email and text reminders 5 days after the PNF is sent if they have not yet clicked the link. The study team will have access to timestamps that indicate when participants accessed their PNF, how long they viewed each page of the PNF, and if they printed it.
Self-Monitoring (SM).
Students will be asked to self-report their alcohol use every in response to two main questions (frequency of 4/5+ drinking for women/men in the past 2 weeks, frequency of 8/10+ drinking for women/men in the past 2 weeks), as well as consequences of their drinking. The therapeutic role of SM is two-fold. First, SM facilitates deliberate attention to and reflection on the person’s actions, the conditions under which these actions occur, and their consequences [38,39]. Hence, SM of drinking behaviors and consequences has the potential to promote awareness of problematic drinking and need for health services. Second, SM affords the opportunity to obtain ongoing information concerning the target behavior, which can be used to inform timely intervention decisions [40]. Students will be asked to complete up to 4 self-monitoring surveys over the course of the semester.
Embedded Tailoring Variable
Every two weeks, as part of the SM intervention component, students are identified as “heavy drinkers” or not (including those who do not respond to the SM survey). They are identified as heavy drinkers if they respond to the SM and report (a) two or more occasions of consuming 4/5+ drinks for women/men in the past two weeks, or (b) one or more occasion of consuming 8/10+ drinks for women/men in the past two weeks.
Bridging Strategies
Online Health Coach Invitation.
As a way to promote engagement in indicated intervention resources, an online health coaching approach will be offered to students. An email will invite students to engage with a health coach who will correspond with them via a secure, confidential online text-based chat platform. Coaching will utilize motivational interviewing strategies to encourage students to consider their values and goals, the possibility of behavior change, and available services. When students click the link in the invitation or reminder emails, they will be taken to a welcome page with a brief introduction (i.e., “You may have some thoughts, questions, or just want to talk about some of the things you’ve shared with us on surveys. Like other students, you may find it helpful to connect.”) A short menu of options will be available to start a health coach chat with their own message or by selecting a topic of interest (i.e., “The stress in your life”, “Alcohol or drug use”, “Other questions or concerns”), and there will be a link to a list of other resources they can access. Students and coaches will post messages online and notifications of new messages will be sent to the intended recipient’s email with a log-in prompt. If students visit the health coach home page but do not start a chat, a health coach will reach out to them via email and invite them to participate. The goal of the dialogue is to motivate the student to access alcohol use interventions (e.g., Web-BASICS or an in-person health promotion consultation on campus). This approach is an adaptation of an effective intervention for offering students mental health services [41]. We will track engagement with the online health coach, as well as with subsequent interventions.
Resource Email.
In this approach, an email will be used to bridge students from universal to indicated interventions. The email will invite students to access resources to reflect on their wellness and alcohol use. The resources included in the email will be the same online and in-person options offered by the online health coach, including a link to Web-BASICS and contact information for in-person health promotion consultation services on campus.
Indicated Interventions
Web-BASICS.
Web-BASICS is delivered online and incorporates to individual participant data with the same motivational information and feedback as used in the in-person BASICS intervention (see [42]). Web-BASICS contains text and graphical feedback regarding students’ reported drinking quantity, frequency, peak alcohol consumption, and blood alcohol content (BAC), perceived norms of others’ drinking, risks for alcohol problems based on participant family history and consumption patterns, protective behaviors the participant already uses and others they might consider, and a tips page with a BAC chart, information on reduced-risk drinking, and where to get more information. Participants can print and/or view their individualized content online.
The version of Web-BASICS utilized in the present study is very similar to the BASICS feedback used in traditional in-person BASICS sessions, as well as Web-BASICS used previously (e.g., [43]). The approach taken is very similar to previous studies, in that students filled out a survey and then immediately following completion of the survey the students were presented with the Web-BASICS personalized feedback. The normative feedback was updated based on most current response to the feedback and may differ from the first time they saw the PNF feedback. Prior work with Web-BASICS indicates college students who received Web-BASICS reported significantly lower number of drinks on their peak occasion in the past month and fewer total drinking days in the past month relative to an assessment only control group; however, no differences were found for total drinks per week [43].
Health Promotion Consultation.
For students who prefer an in-person approach, a health promotion consultant is available to all students via a campus clinic. Health promotion consultation includes a confidential exploration of student drug and alcohol use. Health promotion consultants help students assess how their alcohol and other substance use affects their life and learn how to make healthier decisions.
Study Measures
Outcome variables
All study outcome variables are measured before college, at the end of the first and second semesters, and at the beginning of the third semester.
Binge drinking (primary).
The primary outcome is the frequency of consuming 4/5+ drinks for women/men within a two-hour period in the past 30 days [44].
Brief Young Adult Alcohol Consequences Questionnaire (B-YAACQ; secondary).
Alcohol-related consequences experienced by respondents will be measured by 24 items derived from the 48-item Young Adult Alcohol Consequences Questionnaire. The B-YAACQ [45] has items that tap the full range of the alcohol problems continuum from signs of excessive drinking to symptoms consistent with alcohol abuse and alcohol dependence.
Utilization of Health Services Survey (secondary).
We will track engagement with Web-BASICS and self-reported use of health promotion services (e.g., healthcare clinics, therapy, support groups, self-help resources, etc.) by respondents in the last 3 months, including when they started, if they are currently utilizing the service/resource, and how helpful it has been. We will also collect data regarding alcohol violations and any university-mandated alcohol interventions.
Moderator variables
In order to optimize the API, the following hypothesized moderators will be examined.
Pre-college alcohol use norms.
Perceptions of other college students’ drinking (i.e., percentage who used alcohol in last 30 days, number of drinks consumed in typical week in last 30 days, largest number of drinks consumed in last two weeks, and percentage who binge drank in last two weeks) will be measured at baseline (before college).
Pre-college intentions for college drinking.
Intentions to drink (i.e., frequency of drinking, number of drinks consumed during typical occasion, frequency of binge drinking, and frequency of feeling drunk) over the next 6 months in college will also be measured at baseline.
Binge and high-intensity drinking in college.
The SM surveys will include measures of college student binge drinking (consuming 4/5+ drinks for women/men) and high-intensity drinking (consuming 8/10+ drinks for women/men) in the last 2 weeks.
Statistical Analysis
All statistical analyses will follow the intention-to-treat principle, with all participants included in the analysis according to their randomized intervention regardless of interventions actually received. Pre-randomization variables will be compared to check for balance between groups at each randomization.
Primary aim analysis.
We will conduct the analysis for the primary aims after data are collected for Follow-up 2. The analyses of the primary outcome (number out of the last 30 days with binge drinking) will compare the main effect of participants randomized to APIs beginning with PNF+SM vs. control (no API) using all of the study data: 2/3 of the sample randomly assigned to receive an API (cells A-F in Figure 1) versus 1/3 of the sample randomly assigned to control. The primary contrast in this analysis is the marginal effect of API vs. control on change in the log-average number of heavy-drinking days from baseline to Follow-up 1 (end of the semester one). A repeated-measures, log-link model will be used to analyze the longitudinal outcome. Specifically, a marginal mean model (on the log-scale) with terms for the intercept, dummy indicators for time (e.g., baseline, Follow-up 1, and Follow-up 2), and all group (API vs. control)-by-time interactions. Model coefficients will be estimated using generalized estimating equations [46] with an exchangeable working correlation structure between time points. Robust (sandwich) variance estimators will be used for hypothesis testing and confidence intervals. The study’s primary hypothesis is that API results in a greater reduction in the log-mean number of binge drinking days per month versus control (no API) from baseline to Follow-up 1. This corresponds to testing the null hypothesis that the coefficient of the group-by-Follow-up 1r interaction term is zero. Statistical significance will be determined using a two-sided test with an α level of 0.05.
Similar models will be fit for secondary outcomes with appropriate changes to the link function: log link for maximum number of drinks in the last 30 days, identity link for alcohol-related consequences (B-YAACQ questionnaire), and logit link for utilization of health services (yes/no). For secondary outcomes we will use α = 0.05 for each outcome without correcting for multiple testing.
The primary analysis uses only data through Follow-up 2, but additional longitudinal through Follow-up 3 data are collected as part of the study. As secondary analyses, we will use the data to examine the temporal trend and sustainability of treatment effects (API vs. no API) for primary and secondary outcomes throughout follow-ups.
Aim 2 Analyses.
Data analyses comparing APIs and determining the optimal components of an API (Aim 2) consist of two parts. These analyses use only the 2/3 of the sample randomized to receive an API (cells A-F in Figure 1). In the first part, we will conduct further analyses to identify which is the best, in terms of the number of heavy drinking days (primary outcome), of the four APIs embedded in the SMART design (Table 1). We will use the data analysis method of Robins and colleagues [47,48], extended for use with end-of-study [49] and for repeated measures [50,51]. The four APIs differ in terms of two factors (each with two levels): timing of the PNF+SM intervention (early group A1 = 1 vs. late group A1 = − 1), and type of bridge intervention provided to students identified as heavy drinkers (online health coach invitation A2 = 1 vs. resource emails A2 = − 1). The four APIs do not differ in terms of the intervention provided to students not identified as heavy drinkers. Note that each student will contribute to the API(s) with which their randomization assignment is consistent. All non-heavy drinkers are consistent with two APIs. For example, those students in cell C (Figure 1) are consistent with API 1 and API 2 (Table 1). The (longitudinal) data of those participants would be included twice in the analysis; once with A1 = 1 and A2 = 1 and the other instance with A1 = 1 and A2 = −1. All heavy drinkers in this design are consistent with only one API. For example, those students in cell B (Figure 1) are consistent with API 1. Those students would be included once in the analysis with A1 = 1 and A2 = 1.
A 2×2 weighted log-linear repeated-measures regression model for the number of heavy drinking days will be used. The model will include terms for the intercept, time period, time period -by-[A1, A2, A1-by-A2] interaction terms, and will use a working exchangeable within-person correlation structure. Subjects will be weighted by the inverse of their probability of randomization (weight of 2 for non-heavy drinkers and 4 for heavy drinkers) [50,51]. The analysis will estimate the change in average number of heavy drinking days at each time point for each of the four embedded APIs (with 90% CIs) and will report which API led to the greatest improvements. Using the same model we will also report: (a) the main effect of PNF+SM timing (early group vs. late group) on change, and (b) the main effect of online health coaching vs. resource emails on change among heavy drinkers (averaged over timing of PNF+SM).
The second part of this analysis focuses on comparing the four APIs in terms of cost-effectiveness relative to control (no API) [52]. A cost-effectiveness analysis for comparing the implementation of the four APIs will be conducted from a societal perspective. Intervention costs include study staff time for PNF development, programming, and participant invitations and reminders (via email and text); SM survey development, participant invitations and reminders (via email and text); online health coach platform programming and maintenance, participant invitation and reminders (via email), and coach training, supervision, and engagement with participants; Web-BASICS platform programming and maintenance, and participant invitation and reminders (via email); and health promotion consultations provided by Boynton Health, as well as any other resources consumed associated with developing and delivering each API. Time will be documented by study staff as hours per week dedicated to each activity. The primary measure of implementation cost-effectiveness will be incremental cost per reduction in number of heavy (i.e., 4/5+) drinking days in the past month. This will be calculated as the difference in weighted mean cost per student involved in the APIs vs control divided by the weighted mean difference in number of heavy drinking days between the APIs vs. control. The uncertainty of each incremental cost effectiveness ratio will be estimated with the bootstrap [53].
Aim 3 analyses.
The analysis for Aim 3 will develop a more optimal API by examining whether (a) pre-college alcohol use norms or (b) baseline intentions for college drinking moderate the effect of the timing of PNF+SM; and whether (c) high-intensity drinking (i.e., 8/10+ drinks) vs. binge (i.e., 4/5+ drinks) reported during college in the self-monitoring survey moderate the effect of online health coaching. This analysis will use Q-learning [54,55], an extension of standard moderated regression analysis to multiple stages of intervention; it uses a backward induction (dynamic programming) logic that incorporates effects of future intervention decisions in the evaluation of time-varying moderators. The goal of this analysis is to understand whether and how (a) or (b) could be used at baseline to decide which students ought to receive PNF+SM prior to college vs. in the first month of college; and to understand whether and how (c) could be used to decide which self-identified heavy drinkers ought to receive an online health coach invitation vs. a resource email.
Sample size and power.
The primary study contrast is a main effects comparison between API approaches versus control (No API) on change in frequency of binge drinking (primary outcome) from baseline to the end of semester 1. Using a 2-sided, 2-sample t-test based on a Type-I error rate of 5%, a ratio of 2:1 in the randomized allocation of individuals to APIs vs. control (first randomization), a total of 570 students are needed to detect average differences > 1.0 to 1.15 days in past-month frequency of heavy drinking with > 80 to 90% power, respectively. Differences of 1 to 1.15 correspond to a small-to-moderate standardized effect size of d = 0.25 to 0.29 [56] in between-groups change in frequency of heavy drinking based on previous data with standard deviation of 4 days [R01AA022113, PI: Bacharach]. Based on the same study suggesting an average of 7.1 heavy-drinking days in the past month, an average 1-day reduction corresponds to a 14% reduction in heavy-drinking days. Reductions of less than 14% in the total number of heavy drinking days in the past month are not considered clinically significant because they would result in change of less than one occasion in the past month. Further, based on previous research (for a review see [57]) and our own pilot work, we hypothesize reductions in APIs relative to control with effect sizes > 0.25 (e.g., reported d ranged from 0.29 to 0.85 for PNF vs. assessment only) [57]. After accounting for an estimated study attrition rate of 15%, a total of at least N = 671 (570÷0.85) freshmen college students is needed. We anticipate this sample size is conservative but will invite N = 1,500 students, with an estimated response rate of 45%, giving us N = 675 participants.
Summary
Overview of Study
The M-Bridge study will conduct a sequential multiple assignment randomized trial to (a) test whether or not APIs that transition from universal to indicated resources reduce heavy drinking and related consequences among college students, and (b) provide evidence to optimize the API including the timing of the universal indication (pre-college versus after college) and components of the bridging strategy. Effective universal and indicated prevention interventions for college students have been developed [8,9,12,58–60]. However, there is scant evidence to guide the development of an API for heavy drinking among first-year college students.
Importance of APIs
This study is the first to develop and optimize an API using universal and indicated interventions for college drinking. To our knowledge, there is no empirically-supported API for college student drinking, although face validity of combining universal and indicated interventions (as proposed in the first stage of the APIs embedded in this trial) is supported in previous work [61,62]. This study will provide a solid foundation for the development of additional approaches for bridging universal and indicated interventions (consistent with stepped-care and tiered prevention approaches), to ensure that students receive the level of intervention they need. APIs can capitalize on resources efficiently by using universal intervention – in this case an online PNF+SM intervention – as a first line of defense for all students. Then, students who are indicated will be motivated to seek additional intervention resources, because of their higher-risk drinking and greater likelihood to benefit. That is, APIs are designed to take advantage of heterogeneity in response to an intervention by identifying early those participants who do not benefit adequately from initial intervention options and modifying the intervention to accommodate their needs. By providing appropriate level of intervention to those who need it, when they need it, adaptive interventions hold the promise of improving long-term outcomes for greater numbers of people, thereby increasing the reach and impact of alcohol use interventions [55,63].
APIs for heavy drinking among first-year college students have the potential to be high impact. About 20% of college students have an alcohol use disorder [5]. During the transition to college, students enter social networks that rely heavily on alcohol use [64,65], especially at the beginning of the academic year [66–68]. Many colleges and universities offer universal and indicated prevention interventions for their first-year students, but there is little data to help guide creation of an API.
Novel Aspects of Design
This trial is uniquely designed to answer the relevant questions for development of an API for heavy drinking. Because there is no empirically-supported API in this setting, we felt it important to establish whether APIs beginning with PNF+SM led to improved outcomes compared to no interventions. As a consequence, 1/3 of participants are randomized initially to an assessment-only control condition. Although control conditions are not required or even commonly used as part of SMART designs [69], initially randomizing some participants to one allows investigators to establish that APIs hold promise. Among those not in the control group, the two-stage randomization further allows us to collect data to optimize the API. In particular, intervention programs, and perhaps especially brief interventions, are most powerful when delivered to receptive participants at critical times for behavior change [70]. Therefore, the proposed design also seeks to understand the appropriate ‘windows of opportunity’ by first randomizing the start of the universal intervention which is a critical question for universities and other service providers attempting to address college alcohol use. Second, technology-based versions of brief interventions are resource-efficient and effects may be as good as in-person interventions [6,17]. Therefore, the second randomization among self-reported heavy drinkers examines whether technology-based approaches can be used to increase utilization of empirically-supported interventions.
Conclusions
This paper describes the protocol of a research project designed to promote health among first-year college students by testing and understanding how best to construct an adaptive sequence of preventive intervention strategies. The interventions considered are designed to prevent and identify high-risk alcohol use, as well as motivate heavy-drinking college students to access existing resources to support reducing high-risk alcohol use; in addition, the interventions leverage technology-based intervention modalities. The primary outcome is a reduction in binge drinking, with secondary outcomes of reducing negative alcohol-related consequences and increasing health services utilization. Adaptive preventive interventions have the potential to reduce both the acute negative health consequences (e.g., injury, alcohol poisoning) and long-term health consequences (e.g., alcohol use disorders) of young adult alcohol use, while seeking to leverage technology in order to use campus resources in the most efficient way possible.
Acknowledgements
This work was supported by the National Institute on Alcohol Abuse and Alcoholism grant R01AA026574 to M. Patrick. The content here is solely the responsibility of the authors and does not necessarily represent the official views of the sponsors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing interests
The authors declare no conflicts of interest.
References
- [1].Hingson R, Zha W, Weitzman ER, Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005, J. Stud. Alcohol Drugs, Suppl. (2009) 12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Perkins HW, Social norms and the prevention of alcohol misuse in collegiate contexts, J. Stud. Alcohol, Suppl. 63 (2002) 164–172. doi: 10.15288/jsas.2002.s14.164. [DOI] [PubMed] [Google Scholar]
- [3].Hingson R, White A, New research findings since the 2007 Surgeon General’s call to action to prevent and reduce underage drinking: A review, J. Stud. Alcohol Drugs 75 (2014) 158–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, Patrick ME , Monitoring the Future national survey results on drug use, 1975–2018: Volume II, College students and adults ages 19–60., Ann Arbor, MI, 2019. [Google Scholar]
- [5].Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, Olfson M, Mental health of college students and their non-college-attending peers: Results from the national epidemiologic study on alcohol and related conditions, Arch. Gen. Psychiatry 65 (2008) 1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Scott-Sheldon LAJ, Carey KB, Elliott JC, Garey L, Carey MP, Efficacy of alcohol interventions for first-year college students: A meta-analytic review of randomized controlled trials, J. Consult. Clin. Psychol 82 (2014) 177–188. doi: 10.1037/a0035192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Muñoz RF, Mrazek PJ, Haggerty RJ, Institute of Medicine report on prevention of mental disorders: Summary and commentary, Am. Psychol 51 (1996) 1116–1122. doi: 10.1037/0003-066X.51.11.1116. [DOI] [PubMed] [Google Scholar]
- [8].NIAAA, Planning Alcohol Interventions Using NIAAA’s CollegeAIM (NIH Publication No. 15-AA-8017), (2015). https://www.collegedrinkingprevention.gov/CollegeAIM/Resources/NIAAA_College_Matrix_Booklet.pdf.
- [9].Larimer ME, Cronce JM, Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999–2006, Addict. Behav 32 (2007) 2439–2468. doi: 10.1016/j.addbeh.2007.05.006. [DOI] [PubMed] [Google Scholar]
- [10].Miller WR, Rollnick S, Motivational interviewing: preparing people to change addictive behavior, Guilford Press, New York, 2002. [Google Scholar]
- [11].Tevyaw TO, Monti PM, Motivational enhancement and other brief interventions for adolescent substance abuse: foundations, applications and evaluations, Addiction. 99 (2004) 63–75. doi: 10.1111/j.1360-0443.2004.00855.x. [DOI] [PubMed] [Google Scholar]
- [12].Carey KB, Scott-Sheldon LAJ, Carey MP, DeMartini KS, Individual-level interventions to reduce college student drinking: A meta-analytic review, Addict. Behav 32 (2007) 2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Czyz EK, Horwitz AG, Eisenberg D, Kramer A, King CA, Self-reported barriers to professional help seeking among college students at elevated risk for suicide, J. Am. Coll. Heal 61 (2013) 398–406. doi: 10.1080/07448481.2013.820731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Wu LT, Pilowsky DJ, Schlenger WE, Hasin D, Alcohol use disorders and the use of treatment services among college-age young adults, Psychiatr. Serv 58 (2007) 192–200. doi: 10.1176/appi.ps.58.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hingson R, Heeren T, Edwards E, Saitz R, Young adults at risk for excess alcohol consumption are often not asked or counseled about drinking alcohol, J. Gen. Intern. Med 27 (2012) 179–184. doi: 10.1007/s11606-011-1851-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hingson R, Zha W, White A, Simons-Morton B, Screening and brief alcohol counseling of college students and persons not in school, JAMA Pediatr. 169 (2015) 1068–1070. doi: 10.1001/jamapediatrics.2015.2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Schwartz RP, Gryczynski J, Mitchell SG, Gonzales A, Moseley A, Peterson TR, Ondersma SJ, O’Grady KE, Computerized versus in-person brief intervention for drug misuse: A randomized clinical trial, Addiction. 109 (2014) 1091–1098. doi: 10.1111/add.12502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Escoffery C, Miner KR, Adame DD, Butler S, McCormick L, Mendell E, Internet use for health information among college students, J. Am. Coll. Heal 53 (2005) 183–188. doi: 10.3200/JACH.53.4.183-188. [DOI] [PubMed] [Google Scholar]
- [19].Horgan Á, Sweeney J, Young students’ use of the internet for mental health information and support, J. Psychiatr. Ment. Health Nurs 17 (2010) 117–123. doi: 10.1111/j.1365-2850.2009.01497.x. [DOI] [PubMed] [Google Scholar]
- [20].Collins LM, Murphy SA, Bierman KL, A conceptual framework for adaptive preventive interventions, Prev. Sci 5 (2004) 185–196. doi: 10.1023/B:PREV.0000037641.26017.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Fabiano GA, Evans SW, Introduction to the Special Issue of School Mental Health on Best Practices in Effective Multi-tiered Intervention Frameworks, School Ment. Health 11 (2019) 1–3. doi: 10.1007/s12310-018-9283-2. [DOI] [Google Scholar]
- [22].Kilgus SP, Reinke WM, Jimerson SR, Understanding mental health intervention and assessment within a multi-tiered framework: Contemporary science, practice, and policy, Sch. Psychol. Q 30 (2015) 159–165. doi: 10.1037/spq0000118. [DOI] [PubMed] [Google Scholar]
- [23].August GJ, Piehler TF, Miller FG, Getting “SMART” about implementing multi-tiered systems of support to promote school mental health, J. Sch. Psychol 66 (2018) 85–96. doi: 10.1016/j.jsp.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Borsari B, Hustad JTP, Mastroleo NR, Tevyaw TOL, Barnett NP, Kahler CW, Short EE, Monti PM, Addressing alcohol use and problems in mandated college students: A randomized clinical trial using stepped care, J. Consult. Clin. Psychol 80 (2012) 1062–1074. doi: 10.1037/a0029902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Borsari B, O’Leary Tevyaw T, Stepped Care: A Promising Treatment Strategy for Mandated Students, J. Stud. Aff. Res. Pract 42 (2011) 381–397. doi: 10.2202/1949-6605.1514. [DOI] [Google Scholar]
- [26].Borsari B, Tevyaw TO, Barnett NP, Kahler CW, Monti PM, Stepped care for mandated college students: A pilot study, Am. J. Addict 16 (2007) 131–137. doi: 10.1080/10550490601184498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Haaga DAF, Introduction to the special section on stepped care models in psychotherapy, J. Consult. Clin. Psychol 68 (2000) 547–548. doi: 10.1037/0022-006X.68.4.547. [DOI] [PubMed] [Google Scholar]
- [28].Sobell MB, Sobell LC, Stepped care as a heuristic approach to the treatment of alcohol problems, J. Consult. Clin. Psychol 68 (2000) 573–579. doi: 10.1037/0022-006X.68.4.573. [DOI] [PubMed] [Google Scholar]
- [29].McKay JR, Treating substance use disorders with adaptive continuing care, American Psychological Association, Washington, DC, 2009. doi: 10.1037/11888-000. [DOI] [Google Scholar]
- [30].Nahum-Shani I, Ertefaie A, Lu XL, Lynch KG, McKay JR, Oslin DW, Almirall D, A SMART data analysis method for constructing adaptive treatment strategies for substance use disorders, Addiction. 112 (2017) 901–909. doi: 10.1111/add.13743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Doumas DM, Kane CM, Navarro TB, Roman J, Decreasing heavy drinking in first-year students: Evaluation of a web-based personalized feedback program administered during orientation, J. Coll. Couns 14 (2011) 5–20. doi: 10.1002/j.2161-1882.2011.tb00060.x. [DOI] [Google Scholar]
- [32].Neighbors C, Lewis MA, Atkins DC, Jensen MM, Walter T, Fossos N, Lee CM, Larimer ME, Efficacy of web-based personalized normative feedback: A two-year randomized controlled trial, J. Consult. Clin. Psychol 78 (2010) 898–911. doi: 10.1037/a0020766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Murphy SA, Lynch KG, Oslin D, McKay JR, TenHave T, Developing adaptive treatment strategies in substance abuse research, Drug Alcohol Depend. 88 (2007). doi: 10.1016/j.drugalcdep.2006.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Almirall D, Nahum-Shani I, Sherwood NE, Murphy SA, Introduction to SMART designs for the development of adaptive interventions: with application to weight loss research, Transl. Behav. Med 4 (2014) 260–274. doi: 10.1007/s13142-014-0265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Patrick ME, Terry-McElrath YM, Kloska DD, Schulenberg JE, High-intensity drinking among young adults in the United States: Prevalence, frequency, and developmental change, Alcohol. Clin. Exp. Res 40 (2016) 1905–1912. doi: 10.1111/acer.13164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].University of Minnesota, 2018 College Student Health Survey Report: Health and Health-Related Behaviors, Minneapolis, MN, 2018. [Google Scholar]
- [37].Larimer ME, Lee CM, Kilmer JR, Fabiano PM, Stark CB, Geisner IM, Mallett KA, Lostutter TW, Cronce JM, Feeney M, Neighbors C, Personalized Mailed Feedback for College Drinking Prevention: A Randomized Clinical Trial, J. Consult. Clin. Psychol 75 (2007) 285–293. doi: 10.1037/0022-006X.75.2.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Bandura A, Health promotion from the perspective of social cognitive theory, Psychol. Heal 13 (1998) 623–649. doi: 10.1080/08870449808407422. [DOI] [Google Scholar]
- [39].Kanfer FH, Self-monitoring: Methodological limitations and clinical applications, J. Consult. Clin. Psychol 35 (1970) 148–150. doi: 10.1037/h0029874. [DOI] [Google Scholar]
- [40].Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, Murphy SA, Just-in-time adaptive interventions (JITAIs) in mobile health: Key components and design principles for ongoing health behavior support, Ann. Behav. Med 52 (2018) 446–462. doi: 10.1007/s12160-016-9830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].King CA, Eisenberg D, Zheng K, Czyz E, Kramer A, Horwitz A, Chermack S, Online suicide risk screening and intervention with college students: A pilot randomized controlled trial, J. Consult. Clin. Psychol 83 (2015) 630–636. doi: 10.1037/a0038805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA, Brief alcohol screening and intervention for college students, Guilford Press, New York, 1999. [Google Scholar]
- [43].Labrie JW, Lewis MA, Atkins DC, Neighbors C, Zheng C, Kenney SR, Napper LE, Walter T, Kilmer JR, Hummer JF, Grossbard J, Ghaidarov TM, Desai S, Lee CM, Larimer ME, RCT of web-based personalized normative feedback for college drinking prevention: Are typical student norms good enough?, J. Consult. Clin. Psychol 81 (2013) 1074–1086. doi: 10.1037/a0034087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].NIAAA, Recommended alcohol questions, (2018). https://www.niaaa.nih.gov/research/guidelines-and-resources/recommended-alcohol-questions.
- [45].Read JP, Kahler CW, Strong DR, Colder CR, Development and preliminary validation of the young adult alcohol consequences questionnaire, J. Stud. Alcohol 67 (2006) 169–177. doi: 10.15288/jsa.2006.67.169. [DOI] [PubMed] [Google Scholar]
- [46].Liang KY, Zeger SL, Longitudinal data analysis using generalized linear models, Biometrika. 73 (1986) 13–22. doi: 10.1093/biomet/73.1.13. [DOI] [Google Scholar]
- [47].Orellana L, Rotnitzky A, Robins JM, Dynamic regime marginal structural mean models for estimation of optimal dynamic treatment regimes, Part II: Proofs of results, Int. J. Biostat 6 (2010). doi: 10.2202/1557-4679.1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Robins J, Orellana L, Rotnitzky A, Estimation and extrapolation of optimal treatment and testing strategies, Stat. Med 27 (2008) 4678–4721. doi: 10.1002/sim.3301. [DOI] [PubMed] [Google Scholar]
- [49].Nahum-Shani I, Qian M, Almirall D, Pelham WE, Gnagy B, Fabiano GA, Waxmonsky JG, Yu J, Murphy SA, Experimental design and primary data analysis methods for comparing adaptive interventions, Psychol. Methods 17 (2012) 457–477. doi: 10.1037/a0029372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Almirall D, DiStefano C, Chang YC, Shire S, Kaiser A, Lu X, Nahum-Shani I, Landa R, Mathy P, Kasari C, Longitudinal effects of adaptive interventions with a speech-generating device in minimally verbal children With ASD, J. Clin. Child Adolesc. Psychol 45 (2016) 442–456. doi: 10.1080/15374416.2016.1138407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Lu X, Nahum-Shani I, Kasari C, Lynch KG, Oslin DW, Pelham WE, Fabiano G, Almirall D, Comparing dynamic treatment regimes using repeated-measures outcomes: Modeling considerations in SMART studies, Stat. Med 35 (2016) 1595–1615. doi: 10.1002/sim.6819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Crowley DM, Dodge KA, Barnett WS, Corso P, Duffy S, Graham P, Greenberg M, Haskins R, Hill L, Jones DE, Karoly LA, Kuklinski MR, Plotnick R, Standards of evidence for conducting and reporting economic evaluations in prevention science, Prev. Sci 19 (2018) 366–390. doi: 10.1007/s11121-017-0858-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].O’Brien B, Drummond MF, Labelle RJ, Willan A, In search of power and significance: Issues in the design and analysis of stochastic cost-effectiveness studies in health care, Med. Care 32 (1994) 150–163. doi: 10.1097/00005650-199402000-00006. [DOI] [PubMed] [Google Scholar]
- [54].Nahum-Shani I, Qian M, Almirall D, Pelham WE, Gnagy B, Fabiano GA, Waxmonsky JG, Yu J, Murphy SA, Q-learning: A data analysis method for constructing adaptive interventions, Psychol. Methods 17 (2012) 478–494. doi: 10.1037/a0029373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Nahum-Shani I, Ertefaie A, Lu XL, Lynch KG, McKay JR, Oslin DW, Almirall D, A SMART data analysis method for constructing adaptive treatment strategies for substance use disorders, Addiction. 112 (2017) 901–909. doi: 10.1111/add.13743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Cohen J, Statistical power analysis for the behavioral sciences, 2nd ed, Lawrence Erlbaum and Associates, Hillsdale, N.J., 1988. [Google Scholar]
- [57].Cronce JM, Larimer ME, Individual-focused approaches to the prevention of college student drinking, Alcohol Res. Heal 34 (2011) 210–221. [PMC free article] [PubMed] [Google Scholar]
- [58].Larimer ME, Cronce JM, Identification, prevention and treatment: A review of individual-focused strategies to reduce problematic alcohol consumption by college students, J. Stud. Alcohol 63 (2002) 148–163. doi: 10.15288/jsas.2002.s14.148. [DOI] [PubMed] [Google Scholar]
- [59].Larimer ME, Cronce JM, Lee CM, Kilmer JR, Brief intervention in college settings, Alcohol Res. Heal 28 (2004) 94–104. [PMC free article] [PubMed] [Google Scholar]
- [60].Spoth R, Greenberg M, Turrisi R, Preventive interventions addressing underage drinking: State of the evidence and steps toward public health impact, Pediatrics. 121 (2008) S311–S336. doi: 10.1542/peds.2007-2243E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Borsari B, Tevyaw TOL, Barnett NP, Kahler CW, Monti PM, Stepped care for mandated college students: A pilot study, Am. J. Addict 16 (2007) 131–137. doi: 10.1080/10550490601184498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, Somers JM, Williams E, Screening and brief intervention for high-risk college student drinkers: Results from a 2-year follow-up assessment, J. Consult. Clin. Psychol 66 (1998) 604–615. doi: 10.1037/0022-006X.66.4.604. [DOI] [PubMed] [Google Scholar]
- [63].McKay JR, Treating substance use disorders with adaptive continuing care, American Psychological Association, Washington, DC, 2009. [Google Scholar]
- [64].Hartzler B, Fromme K, Heavy episodic drinking and college entrance, J. Drug Educ 33 (2003) 259–274. doi: 10.2190/2L2X-F8E1-32T9-UDMU. [DOI] [PubMed] [Google Scholar]
- [65].Maggs JL , Alcohol use and binge drinking as goal-directed action during the transition to postsecondary education, in: Schulenberg J, Maggs J (Eds.), Heal. Risks Dev. Transitions Dur. Adolesc, Cambridge University Press, New York, 1997: pp. 345–371. [Google Scholar]
- [66].Del Boca FK, Darkes J, Greenbaum PE, Goldman MS, Up close and personal: Temporal variability in the drinking of individual college students during their first year, J. Consult. Clin. Psychol 72 (2004) 155–164. doi: 10.1037/0022-006X.72.2.155. [DOI] [PubMed] [Google Scholar]
- [67].Martens MP, Ferrier AG, Sheehy MJ, Corbett K, Anderson DA, Simmons A, Development of the Protective Behavioral Strategies Survey, J. Stud. Alcohol 66 (2005) 698–705. doi: 10.15288/jsa.2005.66.698. [DOI] [PubMed] [Google Scholar]
- [68].Tremblay PF, Graham K, Wells S, Harris R, Pulford R, Roberts SE, When do first-year college students drink most during the academic year? An internet-based study of daily and weekly drinking, J. Am. Coll. Heal 58 (2010) 401–411. doi: 10.1080/07448480903540465. [DOI] [PubMed] [Google Scholar]
- [69].Vock DM, Almirall D, Sequential Multiple Assignment Randomized Trial (SMART), Wiley StatsRef Stat. Ref. Online (2018). doi: 10.1002/9781118445112.stat08073. [DOI] [Google Scholar]
- [70].Nahum-Shani I, Hekler EB, Spruijt-Metz D, Building health behavior models to guide the development of just-in-time adaptive interventions: A pragmatic framework, Heal. Psychol 34S (2015) 1209–1219. doi: 10.1037/hea0000306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Almirall D, Lizotte DJ, Murphy SA, SMART design issues and the consideration of opposing outcomes: discussion of “Evaluation of viable dynamic treatment regimes in a sequentially randomized trial of advanced prostate cancer” by by Wang, Rotnitzky, Lin, Millikan, and Thall, J. Am. Stat. Assoc 107 (2012) 509–512. doi: 10.1080/01621459.2012.665615. [DOI] [PMC free article] [PubMed] [Google Scholar]


