Abstract
Background
Sleep quality is of paramount importance for human health. This multi-site study measures the proportion and types of self-reported sleep disorders in medical students and evaluates their association with academic performance by Grade Point Average (GPA).
Materials and methods
A cross-sectional survey was conducted on medical students from two medical schools in Jordan during the 2018/2019 academic year. The study utilized the SLEEP-50 questionnaire to estimate the proportion of several sleep disorders and their effects on daily functioning. Below average GPAs were considered poor academic performance.
Results
1041 medical students' online surveys were analyzed from two medical schools’ campuses, representing a 29.7% response rate. Their mean age was 22 ± 2.1 years (ranging from 18 to 37) and 52.6% were female. The mean body mass index was 24.2 ± 4.4 kg/m2. According to the SLEEP-50 questionnaire, the prevalence of sleep disorders among studied medical students ranged from 0.6% for sleep state misperception (SSM) to 23.1% for hypersomnia. Using binary logistic regression, after adjusting for gender and obesity, poor academic performance was associated with a risk for insomnia [adjusted odds ratio (OR) = 1.96, p < 0.001]; affective disorder [OR = 2.24, P < 0.001]; SSM [OR = 6.40, p = 0.045]; narcolepsy [OR = 9.54, p = 0.045]; and circadian rhythm disorders [OR = 2.03, p < 0.001].
Conclusion
Sleep disorders are common among medical students. Several sleep
disorders were associated with poor academic performance. Proper diagnosis and treatment of sleep disorders may remedy this issue.
Keywords: Sleep disorders, Medical students, Academic performance, Epidemiology, Sleep apnea, Insomnia
Highlights
-
•
Sleep disorders such as hypersomnia and insomnia are common among medical students.
-
•
Several sleep disorders have a negative association with their academic performance.
-
•
Insomnia, affective disorder, SSM, narcolepsy, and CRD are risk factors for poor academic performance.
-
•
Proper diagnosis and treatment of sleep disorders may improve the academic performance.
1. Introduction
Adequate sleep is important for human's mental and physical well-being and chronic sleep deprivation has been linked to impaired neurobehavioral functioning [1]. The prevalence of sleep disorders varies but reportedly affects 22%–65% of the general population [[2], [3], [4]]. Approximately, one-third of adults report some form of insomnia [5,6]. Obstructive sleep apnea (OSA) is found in approximately 16%–36% of the general population and is usually associated with insomnia or excessive sleepiness [[7], [8], [9]]. There is growing evidence on the presence of risk factors and symptoms of several sleep disorders among college students [10]. Several studies have found a relatively high prevalence of sleep-related complaints, e.g. inadequate sleep, difficulty falling asleep or maintaining sleep, early morning awakenings, poor sleep quality, early morning sleepiness, and daytime napping, among college students [[11], [12], [13], [14], [15]]. Previous studies also showed the detrimental impact of several sleep disorders, snoring, and daytime sleepiness on the academic performance of college students [[16], [17], [18], [19], [20], [21]].
Among college students, medical students are under particularly high levels of stress, hence the crucial need for adequate refreshing sleep (to maintain cognitive and physical well-being) to achieve their goals [22]. A previous study showed a high prevalence of symptoms and an elevated risk of several sleep disorders among medical students [12]. Our study sought to find out the proportion of different sleep disorders among medical students and to determine their association with academic performance.
2. Participants and methods
2.1. Study participants
Jordan is a small Middle Eastern country with six medical schools. The Doctor of Medicine curriculum in Jordanian universities is a six-year degree designed to provide undergraduates with basic biomedical sciences and clinical skills training. The present study is a cross-sectional survey that was conducted during the 2018/2019 academic year at two academic medical schools in the north of Jordan: Jordan University of Science and Technology (JUST) and Yarmouk University (YU). 2517 and 984 undergraduate medical students were the total number of registered medical students at JUST and YU, respectively. After obtaining institutional review board approval, the questionnaire was sent to all registered medical students by email. Participation was voluntary and students were informed their responses would be confidential. The students did not receive any incentives or rewards for their participation in the study. The questionnaire was distributed in its original version in the English language, the official teaching language in medical schools of Jordanian universities.
2.2. Study questionnaire and data collection
The validated SLEEP-50 questionnaire by Spoormaker et al. [23] was used in this study. The questionnaire consists of 50 questions which screen for 10 sleep disorders including OSA, insomnia, affective disorder, sleep state misperception (SSM), narcolepsy, restless leg syndrome/periodic limb movement disorder (RLS/PLMD), circadian rhythm disorder (CRD), sleepwalking, nightmares, and hypersomnia. The internal consistency of the SLEEP-50 scale is 0.85 and its test-retest reliability falls between 0.65 and 0.89 [23]. The SLEEP-50 has good sensitivity and specificity and the agreement between all clinical diagnoses and SLEEP-50-classifications is substantial (κ = 0.77) [23]. The questionnaire consists of nine sections, each with three to eight items inquiring about different sleep-related complaints. The response to each item (e.g. I am told that I snore) is rated as 1 (not at all), 2 (somewhat), 3 (rather much), and 4 (very much) based on the student's sleep quality in the four weeks prior to the completion of the questionnaire. A minimum score of three or four is necessary for a response to be significant, i.e. be considered a sleep complaint. Each sleep disorder requires at least one sleep complaint and a minimum sub-score to be defined. The latter is calculated by adding the scores of its related items (e.g for defining OSA, there are eight items with a score of 1–4 for each item. A total sub-score should be ≥ 15 and one or more of these items should be rated 3 or 4 to define OSA) (Table 1). An additional set of questions was used to collect university identification numbers (IDs), sociodemographic data, and students' sleep habits. Students were considered short, normal, and long sleepers based on whether they slept less than six, six to eight, or more than 8 hours a day, respectively [24]. In July of 2019, Grade Point Averages (GPAs) for the 2018/2019 academic year were provided by the registration office of each medical school. To protect confidentiality, the corresponding author was the only person who had access to GPAs. Academic grades are classified as below average (GPA ≤ 2.49), good (GPA 2.50–2.99), very good (GPA 3.00–3.49), excellent (GPA 3.50–3.99), and outstanding (GPA ≥ 4.00). Student’ academic performance was defined as poor if their GPA was below average.
Table 1.
Sleep disorders based on the SLEEP-50 questionnaire
| Disorder | Items | Subscore |
|---|---|---|
| Obstructive Sleep Apnea | 1–8 | ≥15 |
| Insomnia | 9–16 | ≥19 |
| Affective disorder | 10, 11, 43, 44 | ≥12 |
| Sleep state misperception | Insomnia, estimated hours slept <4 | ≥19 |
| Narcolepsy | 17–21 | ≥7 |
| Restless legs syndrome/Periodic limb movement disorder | 22–25 | ≥7 |
| Circadian rhythm disorder | 26–28 | ≥8 |
| Sleep walking | 29–31 | ≥7 |
| Nightmares | 32 33–35 |
≥3 ≥9 |
| Hypersomnia | 44–50 | No item or ≥15 on impact of sleep disorder on daily functioning |
| All sleep disorders | ≥15 on impact of sleep disorder on daily functioning |
Informed consent was obtained from the recruited participants. They were not involved in the design of this study, or the study steering committee, and they were not provided inputs on outcomes selection. All procedures performed in this study involving human participants were reviewed and ethically approved by the Institutional Review Board (IRB) and research and ethics committee at JUST. This study was conducted following the 1975 Helsinki declaration (including its later amendments). This work has been reported based on STROCSS 2019 guidelines, and research protocol was registered in the Research Registry with the unique identification number of 5841 [25].
2.3. Statistical analysis
The characteristics of participants were described using frequency and percentage for categorical variables and mean ± standard deviation for continuous variables. A chi-square test was used to assess the association between categorical variables. A binary logistic regression analysis was performed to identify the association between each sleep disorder and poor academic performance while adjusting for gender and obesity. Odds ratios (OR) and their 95% confidence intervals (95% CI) were reported. A p-value of less than 0.05 was considered statistically significant. Version 25.0 of the Statistical Package for Social Sciences Software was used for data analysis.
3. Results
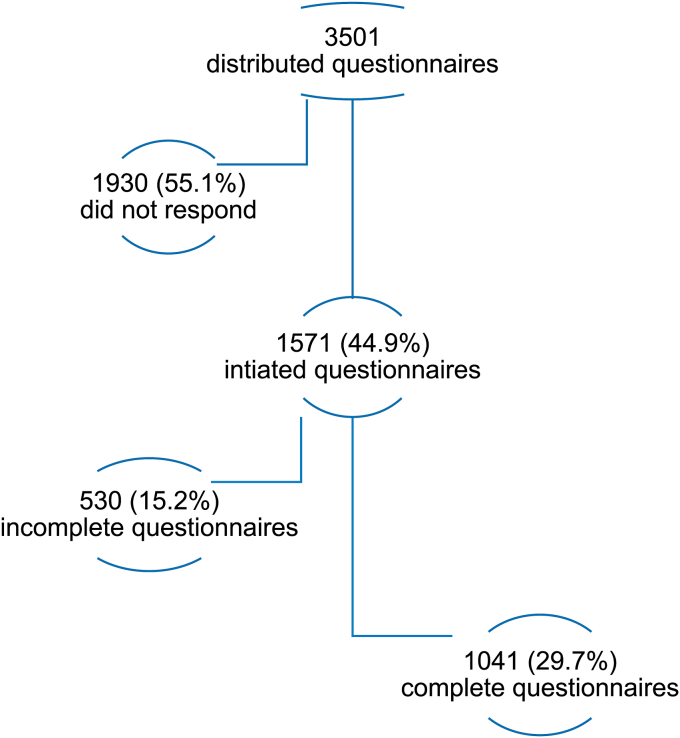
A total of 1571 students (44.9%) completed the online questionnaire. After data revision, 530 were excluded due to missing information or invalid university IDs. Data analysis was done on 1041 undergraduate medical students (29.7%). Their mean age was 22 ± 2.1 years (ranging from 18 to 37), and 52.6% were female (Fig. 1). The mean body mass index was 24.2 ± 4.4 kg/m2. The majority of students (713, 68.5%) were in their clinical (fourth to sixth) years (Table 2). More than one-quarter (320, 30.7%) of the students were short sleepers, more than half (565, 54.3%) were normal sleepers, and one-fifth (156, 15%) were long sleepers. Only 40 students (3.8%) were previously diagnosed with a sleep disorder: 28 had hypersomnia, 5 had OSA, 5 had insomnia, and 2 had RLS. Academic performance was outstanding/excellent in 18.5% of the students, very good in 39.1%, good in 23.5%, and below average in 18.8%. Poor academic performance was more frequent in male (P < 0.001) and obese students (P < 0.001).
Fig. 1.
Study participants.
Table 2.
Demographic distribution of undergraduate medical students.
| Total number of respondents = 1041 | |
|---|---|
| University | |
| JUST | 846 (81.3%) |
| Yarmouk University | 195 (18.7%) |
| Gender | |
| Male | 493 (47.4%) |
| Female | 548 (52.6%) |
| Age (year) mean ± SD | 22.1 ± 2.1 |
| Weight (Kg) mean ± SD | 70.0 ± 17.4 |
| Height (cm) mean ± SD | 169.2 ± 9.4 |
| BMI Kg/m2 mean ± SD | 24.2 ± 4.4 |
| Obese (BMI ≥ 30 kg/m2) | 98 (9.4%) |
| GPA mean ± SD | 3.3 ± 0.5 |
| School Year | |
| 2 | 164 (15.8%) |
| 3 | 164 (15.8%) |
| 4 | 195 (18.7%) |
| 5 | 238 (22.9%) |
| 6 | 280 (26.9%) |
JUST: Jordan University of Science and Technology
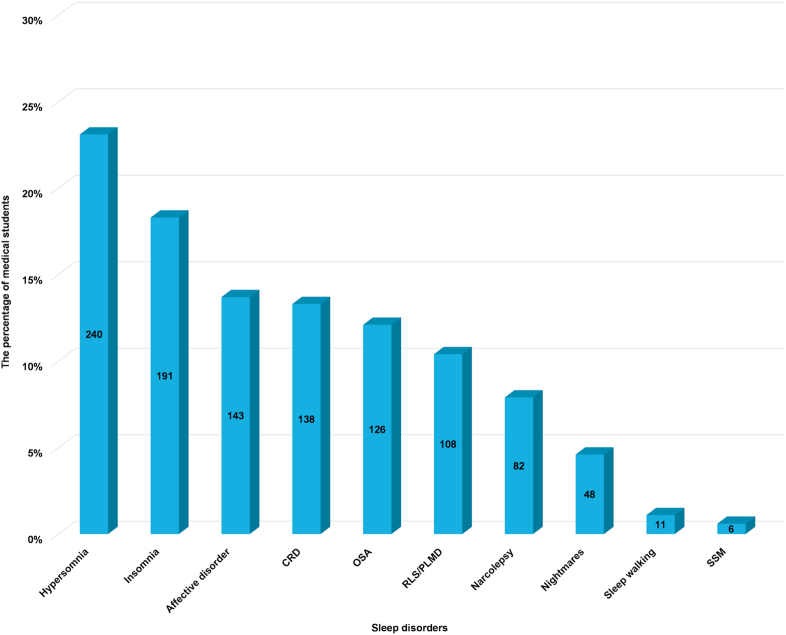
The use of the SLEEP-50 questionnaire showed that 689 students (66.2%) had at least one sleep disorder. Hypersomnia and insomnia were the most common sleep disorders (23.1% and 18.3%, respectively), followed by affective disorder (13.7%), CRD (13.3%), OSA (12.1%), RLS/PLMD (10.4%), narcolepsy (7.9%), nightmares (4.6%), sleepwalking (1.1%) and SSM (0.6%) (Fig. 2). Male medical students were at higher risk of OSA (76, 15.4%) compared with female students (50, 9.1%) with the unadjusted odds ratio (OR) of 1.815 (95% CI 1.242–2.654, p = 0.002). On the other hand, female students had a higher risk of RLS/PLMD (72, 13.1%) and nightmares (33, 6.0%) compared with male students (36, 7.3% and 15, 3.0%, respectively). The unadjusted OR for RLS/PLMD was 0.521 (95% CI = 0.342–0.793, p = 0.002), and 0.490 for nightmares (95% CI = 0.263–0.913, p = 0.022). There was no significant difference between males and females regarding insomnia (p = 0.694), affective disorder (p = 0.554), SSM (p = 0.897), narcolepsy (p = 0.337), CRD (p = 0.162), sleep walking (p = 0.090), or hypersomnia (p = 0.492) (Table 3).
Fig. 2.
The proportion of sleep disorders among undergraduate medical students as ordered from the highest to lowest proportion
Table 3.
The proportion of sleep disorders among undergraduate medical students by the effect of gender
| Sleep Disorder | Female n = 548 | Male n = 493 | p value (χ2) |
|---|---|---|---|
| OSA | 50 (9.1%) | 76 (15.4%) | 0.002 |
| Insomnia | 103 (18.8%) | 88 (17.8%) | 0.694 |
| Affective disorder | 72 (13.1%) | 71 (14.4%) | 0.554 |
| SSM | 3 (0.5%) | 3 (0.6%) | 0.897 |
| Narcolepsy | 39 (7.1%) | 43 (8.7%) | 0.337 |
| RLS/PLMD | 72 (13.1%) | 36 (7.3%) | 0.002 |
| CRD | 65 (11.9%) | 73 (14.8%) | 0.162 |
| Sleep walking | 3 (0.5%) | 8 (1.6%) | 0.090 |
| Nightmares | 33 (6.0%) | 15 (3.0%) | 0.022 |
| Hypersomnia | 131 (23.9%) | 109 (22.1%) | 0.492 |
OSA: obstructive sleep apnea; SSM: sleep state misperception; RLS/PLMD: restless leg syndrome/periodic limb movement disorder; CRD: circadian rhythm disorder.
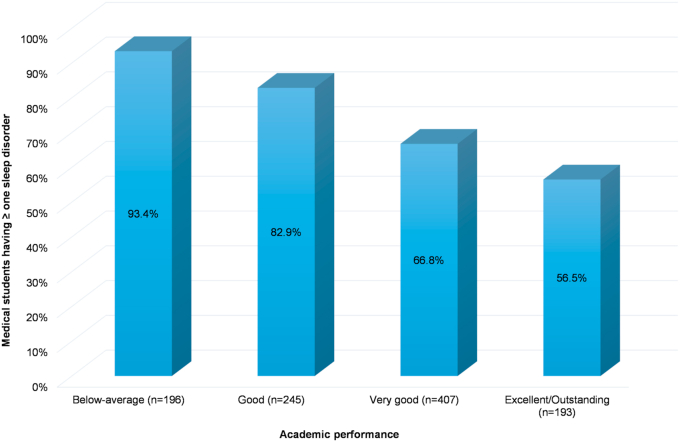
Students with below average academic performance more commonly had at least one sleep disorder when compared to those with very good/excellent/outstanding performance (p = 0.005) (Fig. 3). Students at high risk of OSA, insomnia, affective disorder, SSM, narcolepsy or CRD were more likely to have poor academic performance compared to those at lower risk for these sleep disorders (P < 0.05) (Table 4).
Fig. 3.
The percentage of medical students having ≥ one sleep disorder is inversely related to their academic performance.
Table 4.
Students’ characteristics and the association of sleep disorders with academic performance
| Variables, n (%) | Poor performance, GPA ≤ 2.49 (n = 196) | Good performance, GPA ≥ 2.50 (n = 845) | p value (χ2 test) |
|---|---|---|---|
| Gender: | <0.001 | ||
| Female | 81 (41.3%) | 467 (55.3%) | |
| Male | 115 (58.7%) | 378 (44.7%) | |
| Obesity (BMI ≥ 30 kg/m2) | 41 (20.9%) | 57 (6.7%) | <0.001 |
| School Year: | <0.001 | ||
| Second Year | 38 (19.4%) | 126 (14.9%) | |
| Third Year | 43 (21.9%) | 121 (14.3%) | |
| Fourth Year | 47 (24.0%) | 148 (17.5%) | |
| Fifth Year | 23 (11.7%) | 215 (25.4%) | |
| Sixth Year | 45 (23.0%) | 235 (27.8%) | |
| Academic level: | 0.001 | ||
| Preclinical | 81 (41.3%) | 247 (29.2%) | |
| Clinical | 115 (58.7%) | 598 (70.8%) | |
| Sleep Disorders: | |||
| OSA | 33 (16.8%) | 93 (11.0%) | 0.024 |
| Insomnia | 53 (27.0%) | 138 (16.3%) | <0.001 |
| Affective disorder | 45 (23.0%) | 98 (11.6%) | <0.001 |
| SSM | 4 (2.0%) | 2 (0.2%) | 0.003 |
| Narcolepsy | 51 (26.0%) | 31 (3.7%) | <0.001 |
| RLS/PLMD | 22 (11.2%) | 86 (10.2%) | 0.665 |
| CRD | 41 (20.9%) | 97 (11.5%) | <0.001 |
| Sleep walking | 4 (2.0%) | 7 (0.8%) | 0.135 |
| Nightmares | 11 (5.6%) | 37 (4.4%) | 0.458 |
| Hypersomnia | 38 (19.4%) | 202 (23.9%) | 0.176 |
OSA: obstructive sleep apnea; SSM: sleep state misperception; RLS/PLMD: restless leg syndrome/periodic limb movement disorder; CRD: circadian rhythm disorder.
Using binary logistic regression while adjusting for gender and obesity, several sleep disorders were significantly associated with poor academic performance: insomnia (adjusted OR 1.96; 95% CI 1.35–2.85; p < 0.001), affective disorder (adjusted OR 2.24; 95% CI 1.50–3.35; p < 0.001), SSM (adjusted OR 6.40; 95% CI 1.04–39.19; p = 0.045), narcolepsy (adjusted OR 9.54; 95% CI 5.83–15.60; p = 0.045), and CRD (adjusted OR 2.03; 95% CI 1.34–3.08; p < 0.001). Interestingly OSA, when adjusted for gender and obesity, did not show a significant association with poor academic performance (p = 0.117), while male gender and obesity were significantly associated with poor academic performance (adjusted OR 1.44; 95% CI 1.03–2.00; p = 0.031) and (adjusted OR 3.13; 95% CI 1.99–4.91; p < 0.001), respectively.
4. Discussion
This study aimed to discover the proportion of sleep disorders among medical students and examine their association with academic performance through the use of a well-validated screening tool. Approximately two-thirds of medical students were at risk of at least one sleep disorder, and several sleep disorders had a negative impact on academic performance. In this study, hypersomnia was more prevalent in medical students (23.1%) than in the general adult population (3.9%–16%), as reported in previous community-based studies [26,27]. Insomnia was also prominent in this study (18.3% of the medical students). Gaultney et al. study, using SLEEP-50 questionnaire that surveyed 1845 students enrolled in Introductory Psychology labs at a large state university in the United States, showed that insomnia was one of the most reported disorders (12%) [16]. Piro et al. study, using the same questionnaire, conducted on a smaller cohort, 316 students from medical colleges (medicine, nursing, dentistry, pharmacy, anesthesia, and medical laboratory sciences) at the public University of Duhok-Iraq, found that RLS was the most prevalent type of sleep disorder, affecting 30.7% of students, followed by insomnia (25.0%), CRD (19.6%), affective disorder (14.5%), and sleep apnea (13.6%) [28]. This variation in the prevalence rate of different sleep disorders could be attributed to the different studied cohorts, and different methods and designs used in the studies.
In regard to gender, the results of this study are congruent with previous studies on the general population which showed that the prevalence of OSA in men was double that in women [[29], [30], [31]]. Piro et al. showed that women were at greater risk for RLS/PLMD and nightmares, but there was no gender difference in the risk of OSA [28].
The present study also found that the percentage of medical students with at least one sleep disorder progressively increased as the GPA decreased. Academic performance was negatively associated with the presence of high risk for OSA, insomnia, affective disorder, SSM, narcolepsy, and CRD. Using binary logistic regression analysis adjusting for gender and obesity, poor academic performance was nine times higher in those at high risk for narcolepsy, six times higher in those at high risk for SSM, and twice higher in those at high risk for insomnia, affective disorder, or CRD. Interestingly, after adjusting for the effects of gender and obesity, OSA was not associated with poor academic performance. This may be explained by the fact that both the male gender and obesity are known major risk factors for OSA [32,33]. Male as well as obese medical students in our study were at higher risk of having poor academic performance. Therefore, adjusting for these two confounding variables would make the association between OSA and poor academic performance insignificant. Gaultney et al. study on college students showed that academic failure was linked to the risk of OSA, insomnia, and CRD [16]. However, this study did not adjust for the effects of confounding factors such as gender and obesity. Piro et al. study showed that insomnia, affective disorder, and having multiple sleep disorders were associated with lower GPA [28]. The latter study was limited by a small sample size, 316 students, and a different target population.
It is plausible to assume that the daytime sleepiness, low attention levels and impaired memory/decision making that follow a lack of proper sleep are the explanation for poor academic performance in medical students with sleep disorders [34,35].
Our study also showed that a significant percentage of medical students were short sleepers (30.7%). A cross-sectional survey of approximately 50,000 Norwegian college and university students showed that both sleeping less than 5 h and more than 10 h were associated with failing exams compared with those sleeping seven to 9 h [36]. Short sleep duration and poor sleep quality among medical students could be ascribed to their huge academic load, professional attitudes and habits, and poor awareness of sleep hygiene [10]. The consequences of such behavior can be detrimental to cognitive and behavioral performances [1,37].
This study has a few limitations that should be mentioned. Approximately one-third of all registered medical students were included in the analysis. Although this may create a nonresponse bias, studies have shown that the average response rate of email-based surveys ranges between 25 and 30% [38]. There is high percentage of participants from one college in comparison to the other (846 (81%) from JUST versus 195 (19%) from YU); this could be attributed to the different population size in these colleges (2517 at JUST versus 984 at YU). Although SLEEP-50 is a validated screening tool for the most prevalent DSM–IV–TR sleep disorders (sleep apnea, insomnia, RLS, PLMD, CRD, and nightmares), its predictive validity for SSM, narcolepsy, and affective disorder is limited [23]. Moreover, SLEEP-50 is not a confirmatory diagnostic test for the evaluated sleep disorders. Further studies that utilize more definitive diagnostic tools (e.g., polysomnography) are needed to better investigate the association between sleep disorders and academic performance.
The findings of the study are invaluable for college administrators, healthcare promoters, and health counselors to draw their attention to common sleep problems among medical students. The results of this study encourage the medical schools to increase awareness of the negative impact of sleep disorders on academic performance. Despite the need for further research to establish a cause–effect association, the responsible professionals for students’ health can take action to improve the sleep patterns of medical students. It is worth to inform medical students of the consequences of bad sleep habits and sleep disorders through awareness programs, and encourage students to consult with sleep physicians to diagnose and manage any suspected sleep disorders.
5. Conclusion
Sleep disorders, particularly hypersomnia and insomnia, are common among undergraduate medical students. Several sleep disorders such as insomnia, affective disorder, SSM, narcolepsy, and CRD are associated with poor academic performance. Prospective studies that further compare the academic performance of medical students (before and after the diagnosis and treatment of sleep disorders) will be useful to clarify the association between sleep disorders and poor academic performance. Establishing such association can emphasize the importance of diagnosing and treating sleep disorders among medical students and consequently improve the outcome of medical schools.
Funding
No Funding was received for this study.
Declaration of competing interest
Authors declare that they have no conflicts of interest.
Acknowledgement
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2020.08.046.
Contributor Information
Ahmed Yassin, Email: amyassin@just.edu.jo.
Abdel-Hameed Al-Mistarehi, Email: awalmistarehi18@med.just.edu.jo.
Othman Beni Yonis, Email: oabaniyonis@just.edu.jo.
Abdelwahab J. Aleshawi, Email: abdelwahhabjamal@yahoo.com.
Suleiman M. Momany, Email: smomani@just.edu.jo.
Basheer Y. Khassawneh, Email: basheerk@just.edu.jo.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Van Dongen H.P., Maislin G., Mullington J.M., Dinges D.F. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117–126. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 2.Kushida C.A., Nichols D.A., Simon R.D. Symptom-based prevalence of sleep disorders in an adult primary care population. Sleep Breath. 2000;4(1):9–14. doi: 10.1007/s11325-000-0011-3. [DOI] [PubMed] [Google Scholar]
- 3.Jewett M.E., Dijk D.J., Kronauer R.E., Dinges D.F. Dose-response relationship between sleep duration and human psychomotor vigilance and subjective alertness. Sleep. 1999;22(2):171–179. doi: 10.1093/sleep/22.2.171. [DOI] [PubMed] [Google Scholar]
- 4.Veldi M., Aluoja A., Vasar V. Sleep quality and more common sleep-related problems in medical students. Sleep Med. 2005;6(3):269–275. doi: 10.1016/j.sleep.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Chan-Chee C., Bayon V., Bloch J., Beck F., Giordanella J.P., Leger D. Epidemiology of insomnia in France. Rev. Epidemiol. Sante Publique. 2011;59:409–422. doi: 10.1016/j.respe.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Léger D., Partinen M., Hirshkowitz M., Chokroverty S., Hedner J. Characteristics of insomnia in a primary care setting: EQUINOX survey of 5293 insomniacs from 10 countries. Sleep Med. 2010;11:987–998. doi: 10.1016/j.sleep.2010.04.019. [DOI] [PubMed] [Google Scholar]
- 7.Khassawneh B., Ghazzawi M., Khader Y. Symptoms and risk of obstructive sleep apnea in primary care patients in Jordan. Sleep Breath. 2009;13(3):227–232. doi: 10.1007/s11325-008-0240-4. [DOI] [PubMed] [Google Scholar]
- 8.Senthilvel E., Auckley D., Dasarathy J. Evaluation of sleep disorders in the primary care setting: history taking compared to questionnaires. J Clin Sleep Med. 2011;7(1):41–48. [PMC free article] [PubMed] [Google Scholar]
- 9.Netzer N.C., Hoegel J.J., Loube D. Prevalence of symptoms and risk of sleep apnea in primary care. Chest. 2003;124(4):1406–1414. doi: 10.1378/chest.124.4.1406. [DOI] [PubMed] [Google Scholar]
- 10.Azad M.C., Fraser K., Rumana N. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med. 2015;11(1):69–74. doi: 10.5664/jcsm.4370. Published 2015 Jan 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hershner S.D., Chervin R.D. Causes and consequences of sleepiness among college students. Nat. Sci. Sleep. 2014;6:73–84. doi: 10.2147/NSS.S62907. Published 2014 Jun 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oginska H., Pokorski J. Fatigue and mood correlates of sleep length in three age-social groups: school children, students, and employees. Chronobiol. Int. 2006;23(6):1317–1328. doi: 10.1080/07420520601089349. [DOI] [PubMed] [Google Scholar]
- 13.Lund H.G., Reider B.D., Whiting A.B., Prichard J.R. Sleep patterns and predictors of disturbed sleep in a large population of college students. J. Adolesc. Health. 2010;46(2):124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 14.Kaur G., Singh A. Excessive daytime sleepiness and its pattern among Indian college students. Sleep Med. 2017 Jan;29:23–28. doi: 10.1016/j.sleep.2016.08.020. Epub 2016 Nov 11. [DOI] [PubMed] [Google Scholar]
- 15.Jr1 Buboltz WC., Brown F., Soper B. Sleep habits and patterns of college students: a preliminary study. J. Am. Coll. Health. 2001 Nov;50(3):131–135. doi: 10.1080/07448480109596017. [DOI] [PubMed] [Google Scholar]
- 16.Gaultney J.F. The prevalence of sleep disorders in college students: impact on academic performance. J. Am. Coll. Health. 2010;59(2):91–97. doi: 10.1080/07448481.2010.483708. [DOI] [PubMed] [Google Scholar]
- 17.Wolfson A.R., Carskadon M.A. Understanding adolescents' sleep patterns and school performance: a critical appraisal. Sleep Med. Rev. 2003;7(6):491–506. doi: 10.1016/s1087-0792(03)90003-7. [DOI] [PubMed] [Google Scholar]
- 18.Perez-Chada D., Perez-Lloret S., Videla A.J. Sleep disordered breathing and daytime sleepiness are associated with poor academic performance in teenagers. A study using the Pediatric Daytime Sleepiness Scale (PDSS) Sleep. 2007;30(12):1698–1703. doi: 10.1093/sleep/30.12.1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-mistarehi A.H.W., Ibnian A.M., Shaqadan S., Khassawneh B.Y. American Thoracic Society; 2019. The impact of sleep disorders on academic performance among medical students. C21 determinants of burnout and wellness among physicians and trainees. American Thoracic Society International Conference Abstracts; p. A4296. [DOI] [Google Scholar]
- 20.Curcio G., Ferrara M., De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med. Rev. 2006;10(5):323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Khassawneh B.Y., Alkhatib L.L., Ibnian A.M., Khader Y.S. The association of snoring and risk of obstructive sleep apnea with poor academic performance among university students. Sleep Breath. 2018 Sep;22(3):831–836. doi: 10.1007/s11325-018-1665-z. [DOI] [PubMed] [Google Scholar]
- 22.Wong J.G.W.S., Patil N.G., Beh S.L. Cultivating psychological well-being in Hong Kong's future doctors. Med. Teach. 2005;27:715–719. doi: 10.1080/01421590500237945. [DOI] [PubMed] [Google Scholar]
- 23.Spoormaker V.I., Verbeek I., van den Bout J., Klip E.C. Initial validation of the SLEEP-50 questionnaire. Behav. Sleep Med. 2005;3(4):227–246. doi: 10.1207/s15402010bsm0304_4. http://www.ncbi.nlm.nih.gov/pubmed/16190812 [DOI] [PubMed] [Google Scholar]
- 24.Stranges S., Dorn J.M., Shipley M.J. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am. J. Epidemiol. 2008;168(12):1353–1364. doi: 10.1093/aje/kwn337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Research Registry. https://www.researchregistry.com/register-now#home/registrationdetails/5f1adb0f31b128001570ca35/
- 26.Ohayon M.M. From wakefulness to excessive sleepiness: what we know and still need to know. Sleep Med. Rev. 2008;12:129–141. doi: 10.1016/j.smrv.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maurice M. Ohayon. Epidemiological overview of sleep disorders in the general population. Sleep Med Res. 2011;2:1–9. [Google Scholar]
- 28.Piro R.S., Alhakem S.S.M., Azzez S.S. Prevalence of sleep disorders and their impact on academic performance in medical students/University of Duhok. Sleep Biol. Rhythm. 2018;16:125. doi: 10.1007/s41105-017-0134-6. [DOI] [Google Scholar]
- 29.Bixler E.O., Vgontzas A.N., Lin H.M., Ten Have T., Rein J., Vela-Bueno A. Prevalence of sleep-disordered breathing in women: effects of gender. Am. J. Respir. Crit. Care Med. 2001;163:608–613. doi: 10.1164/ajrccm.163.3.9911064. [DOI] [PubMed] [Google Scholar]
- 30.Sharma S.K., Kumpawat S., Banga A., Goel A. Prevalence and risk factors of obstructive sleep apnea syndrome in a population of Delhi, India. Chest. 2006;130:149–156. doi: 10.1378/chest.130.1.149. [DOI] [PubMed] [Google Scholar]
- 31.Reddy E.V., Kadhiravan T., Mishra H.K. Prevalence and risk factors of obstructive sleep apnea among middle-aged urban Indians: a community-based study. Sleep Med. 2009;10(8):913–918. doi: 10.1016/j.sleep.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 32.Schwartz A.R., Patil S.P., Laffan A.M., Polotsky V., Schneider H., Smith P.L. Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc. Am. Thorac. Soc. 2008;5(2):185–192. doi: 10.1513/pats.200708-137MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Appleton S., Gill T., Taylor A. Influence of gender on associations of obstructive sleep apnea symptoms with chronic conditions and quality of life. Int. J. Environ. Res. Publ. Health. 2018;15(5):930. doi: 10.3390/ijerph15050930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kamdar B.B., Kaplan K.A., Kezirian E.J., Dement W.C. The impact of extended sleep on daytime alertness, vigilance, and mood. Sleep Med. 2004;5(5):441–448. doi: 10.1016/j.sleep.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 35.Killgore W.D., Lipizzi E.L., Kamimori G.H., Balkin T.J. Caffeine effects on risky decision making after 75 hours of sleep deprivation. Aviat Space Environ. Med. 2007;78(10):957–962. doi: 10.3357/asem.2106.2007. [DOI] [PubMed] [Google Scholar]
- 36.Vedaa Ø., Erevik E.K., Hysing M., Hayley A.C., Sivertsen B. Insomnia, sleep duration and academic performance: a national survey of Norwegian college and university students. Sleep Med. X. 2019;1:100005. doi: 10.1016/j.sleepx.2019.100005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kelly W., Kelly K.E., Clanton R.C. The relationship between sleep length and grade-point average among college students. Coll. Student J. 2001;35:84–86. [Google Scholar]
- 38.Yun G.W., Trumbo C.W. Comparative Response to a Survey Executed by Post, E-mail, & Web Form. Journal of Computer-Mediated Communication. 2000;6(1) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.