Abstract
To discover immune factors that can predict the progression of COVID-19, we evaluated circulating immune cells and plasma cytokines in COVID-19 patients. We found that T cells, including CD4+ T cells and CD8+ T cells, were significantly decreased in severe COVID-19 symptoms but not in mild symptoms, in comparison with healthy people. T cells remained at a low level after recovery from severe COVID-19. CD4+CD25+CD127low Treg-enriched cells were significantly increased in either mild or severe COVID-19 patients, regardless of recovery or not. Moreover, in either mild or severe COVID-19 patients, Treg-enriched cells up-regulated CD25 and down-regulated CD127. After recovery, CD25 was partially down-regulated but still higher than the normal level, while CD127 returned to the normal level in mild patients but not severe patients. B cells were decreased in mild patients and further decreased in severe patients, and remained low after recovery. NK cells were decreased only in severe COVID-19, with a tendency to return to the normal level after recovery. Plasma IL-6 and IL-10 were both elevated in severe patients but not in mild patients. After recovery, IL-6 remained higher than its normal level, while IL-10 returned to the normal level. Binary logistic regression analysis indicated that CD4+ T cells, B cells, IL-6, and IL-10 were significantly associated with COVID-19 severity. Therefore, these parameters are indicators of COVID-19 severity. Dynamic monitoring of these parameters would benefit therapy planning and prognosis evaluation.
Abbreviations: COVID-19, Coronavirus disease 2019; EDTA, Ethylenediaminetetraacetic acid; G-CSF, Granulocyte colony-stimulating factor; IFN, Interferon; IL, Interleukin; IP-10, Interferon gamma-induced protein 10; MCP-1, Monocyte chemoattractant protein-1; MIP-1A, Macrophage inflammatory protein 1 alpha; NK cells, Natural killer cells; NKT cells, Natural killer T cells; PBS, Phosphate-buffered saline; Tregs, Regulatory T cells; Th1, T helper 1; Th2, T helper 2; TNF, Tumor necrosis factor; WBC, White blood cells
Keywords: COVID-19, SARS-CoV-2, Immune cells, Cytokines, Inflammation
1. Introduction
Characterizing the pathophysiological changes and immune reactions during COVID-19 progression is important for designing efficacious therapies. Current evidence suggests that the causative agent of COVID-19, i.e. the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), triggers pulmonary recruitment of immune cells, production of immune complexes, and subsequent damage of infected tissues [1]. Lymphopenia and increased neutrophil-lymphocyte ratio were observed in the peripheral blood of COVID-19 patients [2]. Meanwhile, pro-inflammatory cytokines such as IL-1β, IL-6, IFN-γ, MCP-1, MIP-1A, and TNF-α were elevated in the blood plasma of COVID-19 patients [3], [4], [5]. These pro-inflammatory cytokines causes the cytokine storm that triggers severe inflammation, prevents gas exchange, and even leads to death.
Besides, previous studies have indicated that immune cells undergo noticeable functional changes after SARS-CoV-2 infection. Increased blood CD14+CD16+ inflammatory monocytes were found in patients with severe symptoms [6]. In addition, it has been suggested that elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict the severe progression of COVID-19 [7]. Interestingly, SARS-CoV-2 spike glycoprotein (S)-reactive CD4+ T cells are present in 83% of COVID-19 patients but also in 35% of healthy people [8]. The function of NK and CD8+ T cells was exhausted in COVID-19 patients [9]. However, whether these changes are significantly associated with the severity of COVID-19 is not clear. To design effective therapy for COVID-19, it is important to find the cellular or humoral factors that can predict the severity of COVID-19. In this study, we comprehensively quantified circulating immune cells and plasma cytokines in COVID-19 patients in Guangzhou, China, aiming to find the factors most relevant to COVID-19severity. Our data suggest that CD4+ T cells, B cells, IL-6, and IL-10 are predictors of COVID-19 severity.
2. Materials and methods
2.1. Patients
This investigation was approved by the Ethics Committee of Guangzhou Eighth People’s Hospital. From late February to late April 2020, COVID-19 patients who had mild/moderate or severe symptoms were recruited in the study. The diagnosis was made according to standard criteria in the New Coronavirus Pneumonia Diagnosis and Treatment Plan (trial version 6) published by the National Health Committee of the People's Republic of China. The diagnosis was further substantiated by the throat swab test using the standard SARS-CoV-2 nuclear acid test kit. Patients were divided into 4 groups: (1) Mild group: 80 patients with mild or moderate symptoms such as fever, pneumonia on chest CT scan, and respiratory tract symptoms. Respiratory rate >30 beats/min, or mean oxygen saturation <93%. (2) Severe group: 22 patients with any of the following symptoms: respiratory rate > 30 beats/min, the ratio of PaO2 to FiO2 <300, peripheral capillary oxygen saturation ≤93%, respiratory distress or failure demanding ventilation, Shock, combined organ failure, ICU admission, pulmonary pathological deterioration. (3) Mild-recovery group: 61 patients recovered from mild or moderate COVID-19. (4) Severe-recovery group: 6 patients recovered from severe COVID-19. The patients, either with mild/moderate or severe symptoms, were considered recovered when their body temperature turned normal for 3 days, respiratory rate <30 beats/min, mean oxygen saturation >93%, no pneumonia on chest CT scans, and SARS-CoV-2 nuclear acid testing results became negative twice when sampling at least one day apart. Seventy-nine healthy individuals, who had negative SARS-CoV-2 nucleic acid testing results and no symptoms, were enrolled as healthy control. Informed consent was obtained from all patients and healthy individuals. The basic demographic data of the patients and control subjects are shown in Table 1 .
Table 1.
Demographics and baseline parameters.
| Control | Mild | Mild-recovery | Severe | Severe-recovery | |
|---|---|---|---|---|---|
| Age (Mean) | 43.4 | 44.5 | 44.1 | 66.2 | 63.6 |
| Gender | |||||
| Female – no. (%) | 39 (49.4) | 33 (41.3) | 34 (55.7) | 12 (54.5) | 4 (66.7) |
| Male – no. (%) | 40 (50.6) | 47 (58.7) | 27 (44.3) | 10 (45.5) | 2 (33.3) |
| Underlying conditions – no. (%) | |||||
| Hypertension | 4 (5.1) | 6 (7.5) | 2 (3.3) | 4 (18.2) | 1 (16.7) |
| Cardiac disease | 1 (1.2) | 3 (3.8) | 1 (1.6) | 3 (13.6) | 1 (16.7) |
| Renal disease | 0 | 1 (1.3) | 0 | 0 | 0 |
| Diabetes mellitus | 2 (2.5) | 0 | 0 | 0 | 0 |
| Obesity | 1 (1.2) | 0 | 0 | 3 (13.6) | 1 (16.7) |
| Pulmonary disease | 0 | 0 | 0 | 2 (9.1) | 0 |
| Cancer | 0 | 0 | 0 | 0 | 0 |
| Compromised immune system | 0 | 0 | 0 | 0 | 0 |
| Liver disease | 0 | 2 (2.5) | 0 | 1 (4.5) | 0 |
2.2. Sample collection
On the day of hospital admission, 2–4 ml of venous blood was collected from each patient by venipuncture. The same amount of venous blood was collected one day after recovery. The venipuncture was performed once at a time. The An XN-A1 automatic blood analyzer (Sysmex) was used to count leukocytes, lymphocytes, and neutrophils.
2.3. Flow cytometry analysis
To quantify leukocyte populations, erythrocytes were first lysed by resuspending 100 µl of whole blood in ten volumes of Red Blood Cell (RBC) Lysis Buffer (Thermo Fisher) at room temperature for 5 min. Cells were then washed twice with phosphate-buffered saline (PBS), and incubated in the Multitest 6-Color TBNK Reagent or Multitest CD3/CD8/CD45/CD4 mix (both from BD Biosciences) following the manufacturer’s manuals. After two PBS washes, cells were resuspended in 500 µl of ice-cold PBS. BD Trucount™ Absolute Counting Tubes, which carry known fluorescent beads, were applied as a standard to quantify the absolute cell number.
To evaluate regulatory T cells, blood leukocytes were stained with FITC-conjugated CD4 antibody, Violet 450-conjugated CD127 antibody, PerCP-Cy5.5-conjugated CD45 antibody, and APC-conjugated CD25 antibody (5 µg/ml each, BD Biosciences) for 15 min on ice in the dark. After two PBS washes, cells were resuspended in 500 µl of ice-cold PBS and then loaded on a BD FACSCanto Plus. Single cells were first gated between FSC-A and FSC-H. Intact cells were then gated among single cells based on FSC-A and SSC-A. Leukocyte populations were distinguished according to the surface marker staining. The data were assessed using the BD FACSDivaTM software. Isotype controls were also set to ensure specific staining of antibodies (Supplemental Fig. 1).
2.4. Cytometric bead array
The whole blood was centrifuged at 500 × g for 5 min at 4 °C, followed by careful collection of blood plasma. Cytokines were measured using the Human Th1/Th2 Cytokine Kit II (Guangzhou Weimi Bio-Tech) following the manufacturer’s instructions. In this assay, six bead populations with distinct fluorescence intensities are coated with PE-conjugated capture antibodies specific for IL-2, IL-4, IL-6, IL-10, TNF-α, and IFN-γ, respectively. Therefore, the fluorescence intensity of each bead population, which is detected in the Allophycocyanin channel, reveals the identity of each cytokine. The intensity of PE fluorescence reveals the concentration of each cytokine. The limits of detection are as follows: IL-2 (2.6 pg/ml), IL-4 (4.2 pg/ml), IL-6 (6.4 pg/ml), IL-10 (2.8 pg/ml), TNF-α (9.1 pg/ml), IFN-γ (6.1 pg/ml). Samples were evaluated on the BD FACSCanto Plus and the data were analyzed using the FCAP Array Software v3.0.
2.5. Statistics
The data were shown as mean ± standard deviation and compared by GraphPad Prism 6.0. The non-parametric Kruskal-Wallis test or One-way ANOVA with post-hoc Tukey HSD test was applied to compare the mean differences among groups. To determine independent predictors of COVID-19 severity, binary logistic regression analysis was performed. P < 0.05 was regarded as statistically significant.
3. Results
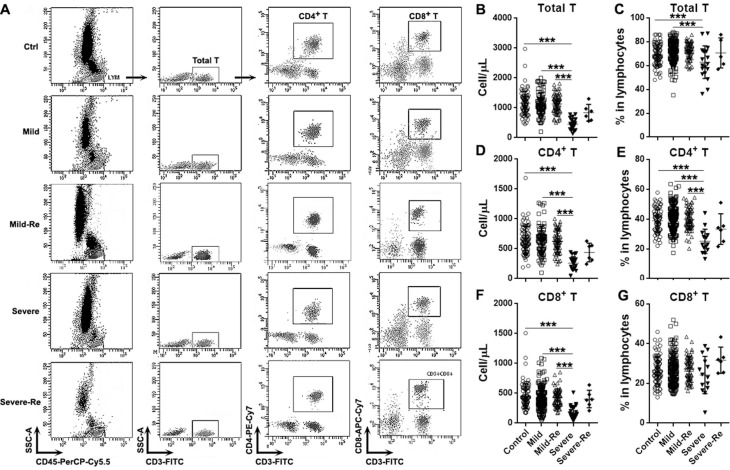
3.1. T cells are reduced in severe COVID-19 patients
To characterize the immune status of COVID-19 patients, we first quantified CD3+ T cells and T cell subsets in the peripheral blood. As shown in Fig. 1 A and B, in comparison with healthy control, the total T cell number in mild COVID-19 patients was normal. However, total T cells were decreased in severe COVID-19 patients. T cell number remained low when severe COVID-19 patients recovered. Similarly, the proportion of total T cells was decreased in severe COVID-19 patients rather than mild COVID-19 patients, and it returned to the normal level after recovery (Fig. 1C). Furthermore, the number and proportions of CD4+ T cells were not altered in mild COVID-19 patients but remarkably reduced in severe COVID-19 patients. After recovery from severe COVID-19, the number and proportion of CD4+ T cell were still reduced (Fig. 1D and E). A similar change of CD8+ T cell number was also seen in severe COVID-19 patients, whereas CD8+ T cell proportion was not significantly altered in either mild or severe COVID-19 patients (Fig. 1F and G).
Fig. 1.
Cellularity of circulating T cells in COVID-19 patients. (A) Representative flow cytometry dot plots showing total T cells, CD4+ T cells, and CD8+ T cells in peripheral blood. Ctrl: healthy control. Mild: mild COVID-19 patients. Mild-Re: recovered mild COVID-19 patients. Severe: severe COVID-19 patients. Severe-Re: recovered severe COVID-19 patients. (B and C) Total T cell numbers (B) and proportions (C). (D and E) CD4+ T cell numbers (D) and proportions (E). (F and G) CD8+ T cell numbers (F) and proportions (G). ***, p < 0.001.
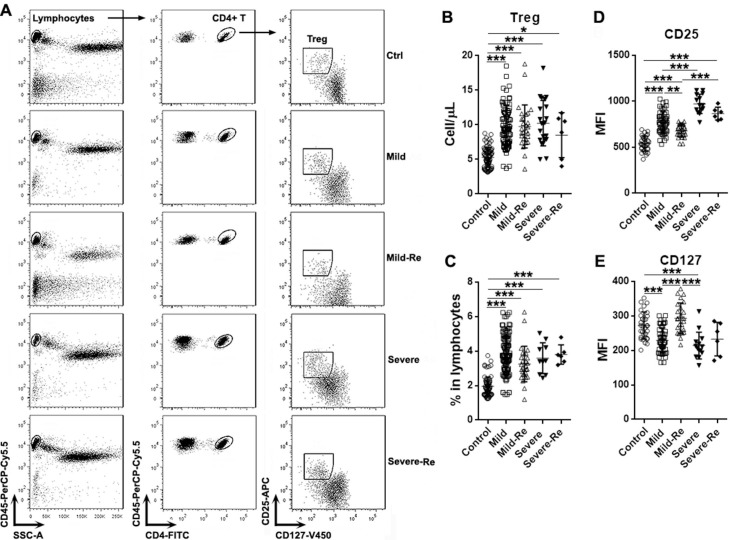
3.2. Treg-enriched cells are increased in COVID-19 patients
Tregs are crucial for immune tolerance and anti-inflammation responses. To check if Treg number was changed in COVID-19, we examined circulating CD4+CD25+CD127low cells which are broadly considered a Treg-enriched population (Fig. 2 A). As indicated in Fig. 2B and C, the number and proportion of CD4+CD25+CD127low cells were increased in both mild and severe COVID-19 patients, in comparison with the control group. No significant difference in the number or proportion of CD4+CD25+CD127low cells were seen between mild and severe COVID-19 patients. Interestingly, these cells remained at higher levels even after recovery.
Fig. 2.
Changes of Treg-enriched cells in COVID-19 patients. (A) Gating strategy for blood Treg-enriched cells. (B) Numbers of Treg-enriched cells. (C) Percentages of Treg-enriched cells in lymphocytes. (D and E) Mean fluorescence of CD25 (D) and CD127 (E) in Treg-enriched cells. *, p < 0.05; **, p < 0.01; ***, p < 0.001.
To evaluate Treg function, we measured the expression of CD25 (a Treg activation marker) and CD127 (a Treg inhibition marker) on the surface of CD4+CD25+CD127low cells. We found that CD25 expression was remarkably increased in mild COVID-19 patients and further increased in severe COVID-19 patients (Fig. 2D). After recovery, CD25 expression was partially down-regulated but still higher than the normal level (Fig. 2D). Moreover, CD25 expression in recovered severe COVID-19 patients was still higher than that in recovered mild COVID-19 patients (Fig. 2D). However, CD127 expression was notably down-regulated in both mild and severe COVID-19 patients, in comparison to the control (Fig. 2E). No difference in CD127 expression was seen between mild COVID-19 patients and severe COVID-19 patients. After recovery, CD127 expression returned to the normal level in mild COVID-19 patients but remained lower in severe COVID-19 patients (Fig. 2E).
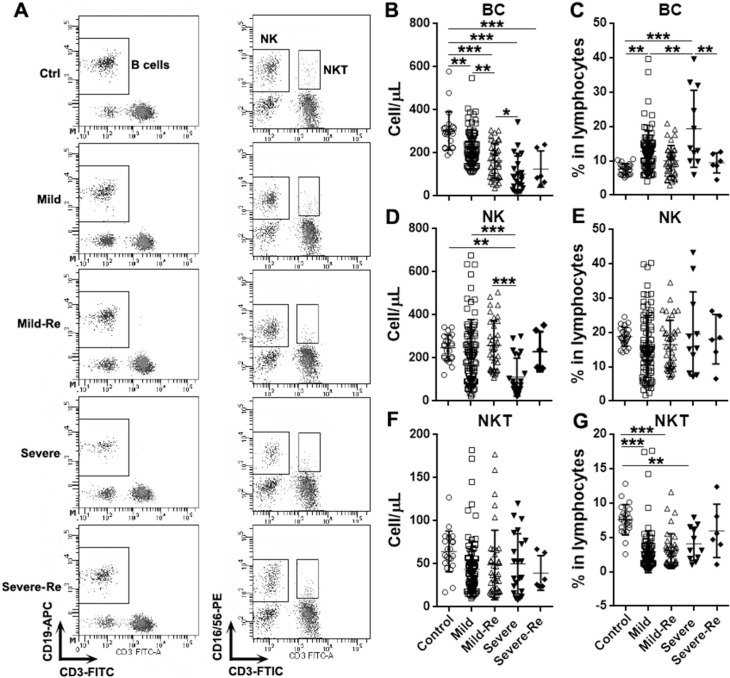
3.3. B cells and NK cells are decreased in COVID-19 patients
We also quantified circulating CD19+ B cells, CD3-CD16/56+ NK cells, and CD3+CD16/56+ NKT cells in patients (Fig. 3 A). B cell number was significantly decreased in mild COVID-19 patients and was further decreased in severe COVID-19 patients (Fig. 3B). Surprisingly, B cell number became much lower in recovered mild COVID-19 patients. (Fig. 3B). On the contrary, B cell proportion was significantly increased in both mild and severe COVID-19 patients (Fig. 3C). Furthermore, B cell proportion in severe COVID-19 patients was higher than that in mild COVID-19 patients (Fig. 3C). In recovered patients, B cell proportion returned to the normal level (Fig. 3C). NK cell number was significantly decreased only in severe COVID-19 patients, and it returned the normal level after recovery (Fig. 3D). However, NK cell proportion was not significantly changed in patients (Fig. 3E). No significant change of NKT cell number was observed (Fig. 3F), whereas NKT cell proportion was comparably attenuated in mild and severe COVID-19 patients regardless of recovery (Fig. 3G).
Fig. 3.
Cellularity of circulating B cells, NK cells, and NKT cells. (A) Gating strategy for B cells, NK cells, and NKT cells. (B and C) B cell numbers (B) and proportions (C). (D and E) NK cell numbers (D) and proportions (E). (F and G) NKT cell numbers (F) and proportions (G). *, p < 0.05; **, p < 0.01; ***, p < 0.001.
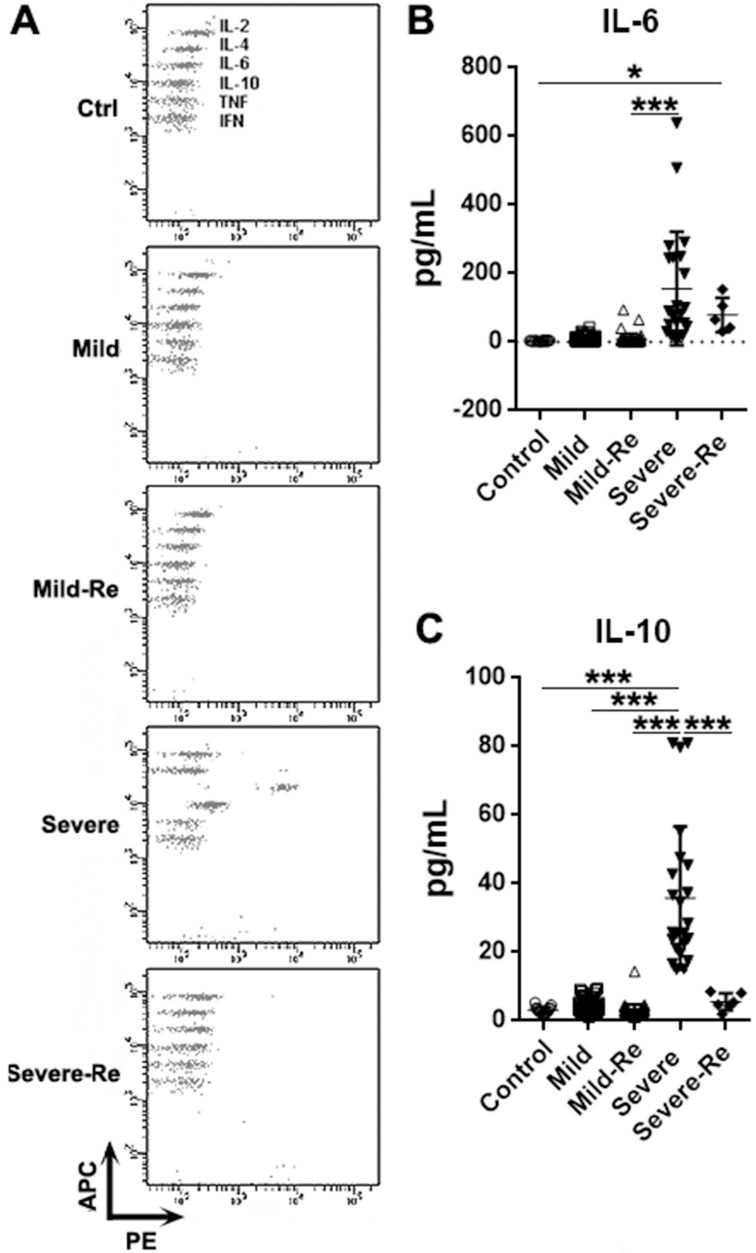
3.4. IL-6 and IL-10 are up-regulated in severe COVID-19 patients
To assess immune and inflammatory responses, we quantified cytokines including IL-2, IL-4, IL-6, IL-10, TNF-α, and IFN-γ in blood plasma (Fig. 4 A). To our surprise, the concentrations of IL-2, IL-4, TNF-α, and IFN-γ in all COVID-19 patients were under their detection thresholds (Data not shown), suggesting that plasma IL-2, IL-4, TNF-α, and IFN-γ are extremely low. IL-6 and IL-10, however, were considerably up-regulated in severe COVID-19 patients rather than mild COVID-19 patients (Fig. 4B and 4C). After recovery, IL-6 was partially down-regulated but still higher than the baseline level (Fig. 4B), while IL-10 returned to its baseline level (Fig. 4C).
Fig. 4.
Cytokine expression in COVID-19 patients. (A) Representative flow cytometry dot plots showing the quantification of plasma cytokines. (B & C) Concentrations of plasma IL-6 (B) and IL-10 (C). *, p < 0.05; ***, p < 0.001.
3.5. CD4+ T cells, B cells, IL-6, and IL-10 indicate disease severity
Binary logistic regression analysis was conducted to find the indicators of the severity of COVID-19. Only the data of mild patients and severe patients were analyzed, because severe COVID-19 patients showed the most significant changes of the parameters tested. The data of recovered patients were not included in this analysis because the sample size of recovered severe COVID-19 patients was too small. We found that CD4+ T cell number was an independent indicator of COVID-19 severity (Table 2 ). In addition, B cell number, IL-6, and IL-10 expression were also indicators of COVID-19 severity (Table 2). The number of CD8+ T cells, Tregs, and NK cells were not strongly associated with COVID-19 severity (Table 2).
Table 2.
Binary logistic regression for indicated parameters.
| β | S.E. | Wald | df | Sig. | Exp(B) | 95% C.I. for EXP(B) |
|||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| CD4+ T | -0.010 | 0.003 | 9.614 | 1 | 0.002 | 0.990 | 0.985 | 0.996 | |
| CD8+ T | -0.009 | 0.004 | 4.404 | 1 | 0.036 | 0.991 | 0.983 | 0.999 | |
| Tregs | 0.026 | 0.054 | 0.238 | 1 | 0.626 | 1.027 | 0.923 | 1.142 | |
| BC | -0.020 | 0.005 | 18.079 | 1 | 0.000 | 0.980 | 0.971 | 0.989 | |
| NK | -0.004 | 0.003 | 2.250 | 1 | 0.134 | 0.996 | 0.990 | 1.001 | |
| IL-6 | 0.094 | 0.021 | 20.938 | 1 | 0.000 | 1.099 | 1.055 | 1.144 | |
| IL-10 | 0.241 | 0.083 | 8.325 | 1 | 0.004 | 1.272 | 1.080 | 1.498 | |
4. Discussion
This study shows that conventional T cells, B cells, and NK cells are reduced in COVID-19 patients. Our data are consistent with the lymphopenia reported by recent research [10], [11], [12]. The decrease of blood lymphocytes is probably due to the recruitment of reactive lymphocytes into the lung tissue. It is also possible that lymphocytes are sensitive to SARS-CoV-2 induced cell death. However, whether SARS-CoV-2 can infect immune cells is not clear. Our study also reveals the increase of Treg-enriched cells in all COVID-19 patients, suggesting that unlike conventional T cells, Tregs are either staying or proliferating in the blood of patients to suppress systemic inflammation. Furthermore, the higher CD25 expression and lower CD127 expression are indicative of enhanced Treg function in COVID-19 patients. However, the role of Tregs in COVID-19 remains unclear. High Treg activity might inhibit inflammation and alleviate tissue damage mediated by the cytokine storm. In the future, it will be important to test the anti-inflammatory and immunoregulatory activity of Tregs to ascertain the role of Tregs in the progression of COVID-19.
The cytokine storm could cause the death of COVID-19 patients. Increased plasma IL-1β, IL-1RA, IL-7, IL-8, IL-9, IL-10, G-CSF, GMCSF, IFN-γ, IP-10, MCP1, MIP-1A, MIP-1B, IL-2, and TNF-α [3]. However, we did not observe high levels of IL-2 and TNF-α in enrolled patients. This suggests that the systemic inflammation in Guangzhou patients might be different from the systemic inflammation in Wuhan patients. However, we did observe higher plasma IL-6 and IL-10 in severe COVID-19 patients. IL-6 is a cytokine that can be either pro-inflammatory or anti-inflammatory [13]. The sources of IL-6 include monocytes, macrophages, mesenchymal cells, endothelial cells, fibroblasts, and many other cells in response to various stimuli. [14]. It has been reported that macrophages produce IL-6 upon stimulation with SARS-coronavirus spike protein [15]. Therefore, activated macrophages are likely the major source of IL-6 in COVID-19 patients. Another important source of IL-6 could be pro-inflammatory Th17 cells. It has been shown that the proportion of Th17 cells is increased in COVID-19 cases [16]. Besides, other cell types including B cells, dendritic cells, fibroblasts, and endothelial cells might also contribute to IL-6 production. IL-10, which is broadly considered an anti-inflammatory cytokine, is produced by alternatively activated macrophages, dendritic cells, conventional T cells, and Tregs during viral infection [17]. Perhaps these cells secret IL-10 after SARS-CoV-2 infection.
Surprisingly, IFN-γ stayed low in all COVID-19 patients. It is a crucial anti-viral cytokine produced by T cells, NK cells, NKT cells, professional antigen-presenting cells such as macrophages, dendritic cells, and B cells [18]. It has been reported that IFN-γ-related cytokine storm was induced after SARS coronavirus infection [19]. Further investigations are needed to test whether IFN-γ in the lung is elevated while plasma IFN-γ remains unchanged. Moreover, IFN-γ can downregulate the expression of the SARS coronavirus receptor ACE2 [20]. SARS-CoV-2 binds to the same receptor of infect target cells [21]. Hence, the potential effect of IFN-γ against SARS-CoV-2 infection deserves more research.
Taken together, our study sheds light on the immune profile of COVID-19 patients in Guangzhou, China. We also identified CD4+ T cells, B cells, IL-6, and IL-10 as good predictors of COVID-19 severity. Hence, dynamic evaluation of these factors is an accurate and convenient approach to monitor the progression of COVID-19, and prompts physicians to take necessary measures to prevent the deterioration of COVID-19.
5. Conclusions
CD4+ T cells, B cells, IL-6, and IL-10 are predictors of COVID-19 severity. Dynamic monitoring of these parameters would benefit therapy planning and prognosis evaluation.
Author contributions
Yaling Shi designed the study and wrote the paper. Xing Chen and Jide Huang collected samples and performed most immune cell detection. Ying Huang and Jiabin Chen conducted cytokine assays. Yingyi Huang did the statistical analysis. Xiaowen Jiang evaluated Tregs.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The study is supported by the Guangzhou Science and Technology Program, China (Grant number: 202008010008).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.humimm.2020.08.006.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Felsenstein S., Herbert J.A., McNamara P.S., Hedrich C.M. COVID-19: Immunology and treatment options. Clin. Immunol. 2020;215 doi: 10.1016/j.clim.2020.108448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y., Xie C., Ma K., Shang K., Wang W., Tian D.S. Dysregulation of immune response in patients with coronavirus, (COVID-19) in Wuhan, China. Clin. Infect. Dis. 2019;71(2020):762–768. doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with, novel coronavirus in Wuhan China. Lancet. 2019;395(2020):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Conti P., Ronconi G., Caraffa A., Gallenga C.E., Ross R., Frydas I., Kritas S.K. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J. Biol. Regulators Homeostatic Agents. 2020;34:327–331. doi: 10.23812/CONTI-E. [DOI] [PubMed] [Google Scholar]
- 5.Zhang B., Zhou X., Qiu Y., Song Y., Feng F., Feng J., Song Q., Jia Q., Wang J. Clinical characteristics of 82 cases of death from COVID-19. PloS one. 2020;15 doi: 10.1371/journal.pone.0235458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.B.F. Yonggang Zhou, Xiaohu Zheng, Dongsheng Wang, Changcheng Zhao, Yingjie qi, Rui Sun, Zhigang Tian, Xiaoling Xu, Haiming Wei, Pathogenic T cells and inflammatory monocytes incite inflammatory storm in severe COVID-19 patients, Natl. Sci. Rev., (2020) nwaa041. [DOI] [PMC free article] [PubMed]
- 7.Zheng H.Y., Zhang M., Yang C.X., Zhang N., Wang X.C., Yang X.P., Dong X.Q., Zheng Y.T. Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients. Cell. Mol. Immunol. 2020;17:541–543. doi: 10.1038/s41423-020-0401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braun J., Loyal L., Frentsch M., Wendisch D., Georg P., Kurth F., Hippenstiel S., Dingeldey M., Kruse B., Fauchere F., Baysal E., Mangold M., Henze L., Lauster R., Mall M.A., Beyer K., Rohmel J., Voigt S., Schmitz J., Miltenyi S., Demuth I., Muller M.A., Hocke A., Witzenrath M., Suttorp N., Kern F., Reimer U., Wenschuh H., Drosten C., Corman V.M., Giesecke-Thiel C., Sander L.E., Thiel A. SARS-CoV-2-reactive T cells in healthy donors and patients with COVID-19. Nature. 2020 doi: 10.1038/s41586-020-2598-9. [DOI] [PubMed] [Google Scholar]
- 9.Zheng M., Gao Y., Wang G., Song G., Liu S., Sun D., Xu Y., Tian Z. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell. Mol. Immunol. 2020;17:533–535. doi: 10.1038/s41423-020-0402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diao B., Wang C., Tan Y., Chen X., Liu Y., Ning L., Chen L., Li M., Liu Y., Wang G., Yuan Z., Feng Z., Zhang Y., Wu Y., Chen Y. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19) Front. Immunol. 2020;11:827. doi: 10.3389/fimmu.2020.00827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan L., Wang Q., Zhang D., Ding J., Huang Q., Tang Y.Q., Wang Q., Miao H. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transd. Targeted Therapy. 2020;5:33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen G., Wu D., Guo W., Cao Y., Huang D., Wang H., Wang T., Zhang X., Chen H., Yu H., Zhang X., Zhang M., Wu S., Song J., Chen T., Han M., Li S., Luo X., Zhao J., Ning Q. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Investig. 2020;130:2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scheller J., Chalaris A., Schmidt-Arras D., Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim. Biophys. Acta. 1813;2011:878–888. doi: 10.1016/j.bbamcr.2011.01.034. [DOI] [PubMed] [Google Scholar]
- 14.Tanaka T., Narazaki M., Kishimoto T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb. Perspect. Biol. 2014;6 doi: 10.1101/cshperspect.a016295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang W., Ye L., Li B., Gao B., Zeng Y., Kong L., Fang X., Zheng H., Wu Z., She Y. Up-regulation of IL-6 and TNF-alpha induced by SARS-coronavirus spike protein in murine macrophages via NF-kappaB pathway. Virus Res. 2007;128:1–8. doi: 10.1016/j.virusres.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., Tai Y., Bai C., Gao T., Song J., Xia P., Dong J., Zhao J., Wang F.S. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rojas J.M., Avia M., Martin V., Sevilla N. IL-10: a multifunctional cytokine in viral infections. J. Immunol. Res. 2017;2017:6104054. doi: 10.1155/2017/6104054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kak G., Raza M., Tiwari B.K. Interferon-gamma (IFN-gamma): exploring its implications in infectious diseases. Biomol. Concepts. 2018;9:64–79. doi: 10.1515/bmc-2018-0007. [DOI] [PubMed] [Google Scholar]
- 19.Huang K.J., Su I.J., Theron M., Wu Y.C., Lai S.K., Liu C.C., Lei H.Y. An interferon-gamma-related cytokine storm in SARS patients. J. Med. Virol. 2005;75:185–194. doi: 10.1002/jmv.20255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Lang A., Osterhaus A.D., Haagmans B.L. Interferon-gamma and interleukin-4 downregulate expression of the SARS coronavirus receptor ACE2 in Vero E6 cells. Virology. 2006;353:474–481. doi: 10.1016/j.virol.2006.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Letko M., Marzi A., Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat. Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.