Abstract
The unprecedented for modern medicine pandemic caused by the SARS-COV-2 virus (“coronavirus”, Covid-19 disease) creates in turn new data on the management and survival of cardiac arrest victims, but mainly on the safety of CardioPulmonary Resuscitation (CPR) providers. The Covid-19 pandemic resulted in losses of thousands of lives, and many more people were hospitalized in simple or in intensive care unit beds, both globally and locally in Greece. More specifically, in victims of cardiac arrest, both in- and out- of hospital, the increased mortality and high contagiousness of the SARS-CoV-2 virus posed new questions, of both medical and moral nature/ to CPR providers. What we all know in resuscitation, that we cannot harm the victim and therefore do the most/best we can, is no longer the everyday reality. What we need to know and incorporate into decision-making in the resuscitation process is the distribution of limited human and material resources, the potentially very poor outcome of patients with Covid-19 and cardiac arrest, and especially that a potential infection of health professionals can lead in the lack of health professionals in the near future. This review tries to incorporate the added skills and precautions for CPR providers in terms of both in- and out- hospital CPR.
Keywords: CPR, COVID-19, Resuscitation, ALS, BLS
Graphical abstract

Coronaviruses are a group of viruses that usually cause respiratory infections of varying severity in humans and animals. In Wuhan (China), at the end of 2019 and in the beginning of 2020, there was a series of pneumonia cases which, on January 9 2020, the Chinese health authorities announced was due to a new coronavirus strain (2019-nCoV, later SARS-CoV-2). During the following months, the transmission of the virus around the world led to a pandemic, with the main characteristics being its high contagiousness, even in pre- or asymptomatic stages, and its high mortality, especially for older adults or patients with comorbidities.
The unprecedented for modern medicine pandemic caused by the SARS-COV-2 virus (“coronavirus”, Covid-19) creates new data on the survival of cardiac arrest victims, but mainly on the safety of Cardiopulmonary Resuscitation (CPR) providers. Of particular importance, especially during CPR, is that the mode of virus transmission is aerogenous, with droplets exhaled through the patient's mouth and nose reaching the rescuer's mucosa via the resulting aerosol that suspends for a long time in closed spaces or even on surfaces. Healthcare professionals during Advanced Life Support (ALS), as well as non-healthcare professionals that provide Basic Life Support (BLS) can be exposed during CPR to this new virus, which is characterized by high contagiousness. Consequently, they need to take protective measures and adjust their actions based on the new data, especially as long as there is a lack of effective tools for its prevention and treatment (vaccines, anti-viral drugs, immunotherapy).1, 2, 3
During the pandemic, there was a dramatic increase in deaths around the world in affected countries. In countries with a proven increase in deaths, this was accompanied by a simultaneous increase in out-of-hospital cardiac arrests (OHCA), both in time and in geographical incidence. For example, in Italy, this increase in OHCA was 58% compared to the corresponding period last year, while in the district of New York (USA), calls to Emergency Medical Services (EMS) quadrupled (i.e. increased by 400% www.nbcnewyork.com/news/..../2368678/).1 , 2
The above data show the increased need for extensive CPR performance in the community by health professionals and by educated citizens. In addition, there is a need for early and clear adjustment of the guidelines for CPR performance both at a national (Hellenic Society of Cardiology, National Public Health Organization) and global level (European Resuscitation Council, American Heart Association) in order to reassure the efficacy and safety of rescuers. With reservation to the scientific data available so far and in line with global recommendations, we need to re-examine the safest methods to perform CPR in victims of both out-of-hospital and in-hospital cardiac arrest.3 , 4
1. Recommendations for performing CPR and/or defibrillation in an out-of-hospital environment
Every time CPR is performed, especially on an unknown patient, there is a risk of cross-infection, which is particularly related to rescue breathings. Normally, this risk is very low and is considered negligible compared to the fact that the victim of cardiac arrest will die if no effective help is given. In any case, based on the existing guidelines, the first thing to do is call for help immediately (National Emergency Medical Services, tel number 112/166), informing them that there is a victim of sudden cardiac arrest (SCA) (“victim is dead”, “victim is not breathing” etc.). The bystanders and the first close responders to an SCA (e.g. specialized staff at the workplace, coaches etc.), who are called to provide initial care, which may include CPR, should already have specific orders from their employers which should be unique to the workplace. It is already advised (European Resuscitation Council - ERC Guidelines 2015) that if you are untrained or unable to provide rescue breathings, you can give CPR only with chest compressions (i.e. continuous chest compressions at a rate of at least 100-120 per minute). In times of a pandemic outbreak and depending on the local and national epidemiological data concerning the probability that the victim has Covid-19, it is suggested that some modifications should be considered such as the recognition of SCA by searching for the absence of signs of life and the absence of normal breathing. However, it is better to completely avoid listening to or feeling breath sounds by placing your ear and cheek near the victim's mouth. Immediately afterwards, cover the victim's face (mouth and nose) with a cloth of his/her own or even yours. If you have doubts about the confirmation of cardiac arrest, start chest compressions until help arrives (or obviously until the patient shows signs of life such as a reaction with movements). Make sure an ambulance is on its way. If you suspect Covid-19, inform the Emergency Medical Services center in the beginning when you call 112/166. As it is well known, we perform CPR continuously only with chest compressions (i.e. continuous chest compressions at a rate of at least 100-120 per minute). Special emphasis is needed on the existence of AED (automated external defibrillator). Early and correct use of AED by an adequately trained person significantly increases the chances of survival of the victim while not increasing the risk of infection of the rescuer. If the rescuer has access to personal protective equipment (PPE; e.g. protective mask, disposable gloves, eye protection), it must be worn before CPR initiation. Even the use of a mask (medical or not) reduces the chances of inhaling respiratory droplets.5 However, it should be mentioned that in terms of OHCA in suspected Covid-19 victims in nursing homes (which has increased incidence during the pandemic in some countries), the first responders who are called to provide CPR to these victims have already been in contact with them for a long period of time, with the relative risk of transmission preceding the arrest. Therefore, in these cases, when CPR initiation is delayed so that the rescuer who has already been in contact (and possibly contaminated) can wear PPE, it can be fatal and probably does not further protect the responder from airborne contamination. Although there are no official universal guidelines about this topic, it seems reasonable that it can be discussed in extent in each place.
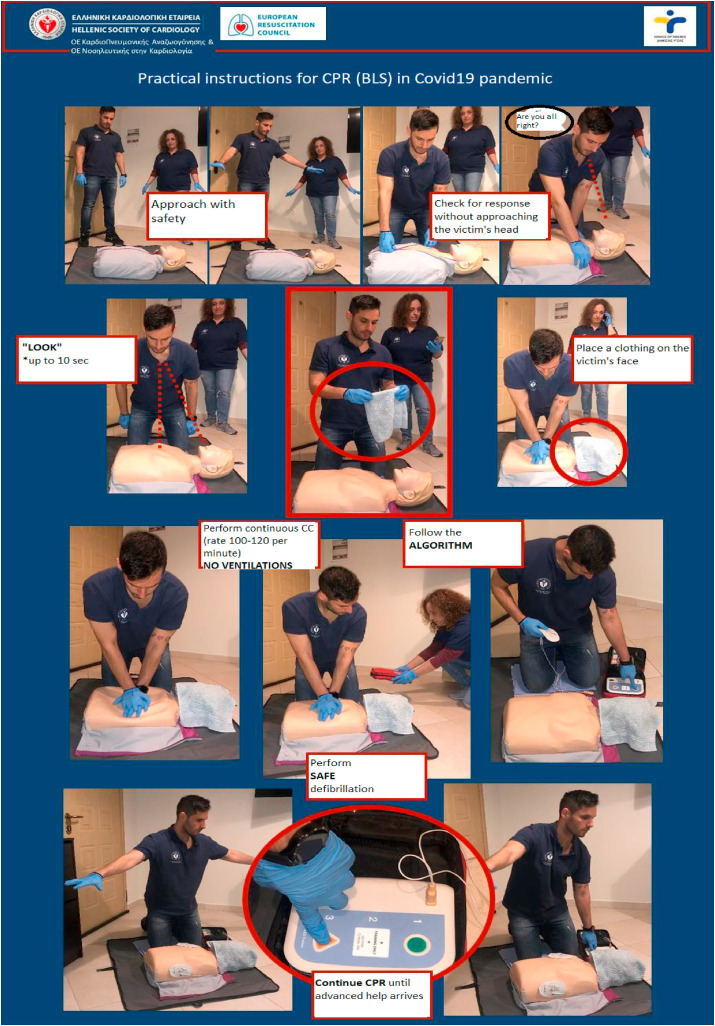
After performing CPR only with chest compressions, all rescuers must wash their hands thoroughly with soap and water. Alcohol-based hand sanitizer gels are a convenient alternative.1 They should also seek further advice from the National Public Health Organization (EODY - https://eody.gov.gr/neos-koronaios-covid-19/). The above instructions for first lay responders have been visualized in Greece by the Hellenic Society of Cardiology in a video (https://youtu.be/ooAlPXRimfc), as well as in a poster format (Fig. 1 ).
Figure 1.
Practical instructions for adjusted basic CPR (Basic Life Support) performed by early responders during Covid- 19 pandemic. Thanks to RNs. Mrs E. Stamatopoulou, Mr D. Aragiannis, and Mrs E. Sigala.
2. CPR from health professionals in a hospital setting and other organized health structures (e.g. Emergency Medical Services means of transfer)
The coronavirus is thought to spread mainly in a manner similar to influenza, from person to person through close contact and droplets. The basic principles of infection control and protection from droplets are the main control strategies and should be strictly followed. Aerosol transmission may also occur. Attention to hand hygiene and to the retention of respiratory secretions produced by coughing and sneezing are the cornerstones of effective infection control. Patients with deteriorating conditions with possible or suspected Covid-19 infection should be preferentially transferred to negative-pressure rooms to minimize risk of exposure to providers during CPR.6
All people suspected or confirmed of having Covid-19 infection should follow the instructions for infection control and use of PPE (see National Public Health Organization, EODY instructions). All those involved should keep in mind that during CPR, there is always the possibility that rescuers may be exposed to body fluids. Further, procedures such as tracheal intubation or βαventilation are also likely to create infectious aerosol. The use or not of PPE for victims, depending on the degree to which they are suspected to have an infection, is decided in advance. Interventional procedures on the airway should be performed by experienced individuals (e.g. introduction of supraglottic airway devices or tracheal intubation). These individuals should only practice the skills for airway management (e.g. bag-mask ventilation) for which they have been trained. Tracheal intubation or the insertion of a supraglottic airway device should only be performed by people who are experienced and capable of performing this procedure. In any case, airway management and ventilation, whether non-invasive or invasive (e.g. tracheal intubation by an anesthesiologist) are procedures of high-risk for dispersion of droplets and/or aerosol from the victim, and therefore protection measures that are taken should be of the highest level of security. Several national anesthesiology societies across the world have issued clear and detailed instructions on the matter.7 , 8
However, any case of difficult airway management is accompanied by widespread dispersal of infected aerosol throughout the surrounding area; this should be taken into account, and other attendees should be adequately protected. Participants in CPR (ideally members of the resuscitation team) should be trained in safe but rapid dressing /removal of PPE and avoidance of infection.
2.1. Recommendations for CPR in healthcare facilities in patients a) with diseases similar to Covid-19 infection or b) with confirmed Covid-19
Patients with Covid-19 infection or Covid-19-like disease (pending laboratory documentation) who are at risk for acute deterioration or cardiac arrest should be identified early. Appropriate measures must be taken in time to prevent SCA and avoid unprotected/uncovered CPR. The use of monitoring systems and early activation on clinical deterioration will allow the early detection of such patients. The best approach to manage cardiac arrest is to prevent it, as there are clear clinical signs of deterioration, such as hypoxia and hypotension, in 50-80% of the cases.
Although in Greece, there is no relevant legislation on the decision of no resuscitation (DNR - do not resuscitate), CPR performance in China in 136 hospitalized patients with Covid-19 pneumonia who presented cardiac arrest (with the relative risks of transmission to staff) led to the survival of only four.9
The level of PPE to be used in order to evaluate a patient, to initiate chest compressions, and to assess heart rhythm in the regular intervals of two minutes is determined by the National Guidelines. In any case, as few as possible and only the absolutely necessary healthcare professionals should participate in the ALS, while it should ideally take place in a special, negative pressure isolation room.
The need for PPE may delay CPR initiation for patients with Covid-19. Review of the relevant procedures (including PPE availability in resuscitation carts), along with theoretical training and practice, will minimize these delays. Staff safety is of paramount importance. In cardiac arrest that is likely to be of hypoxemic cause, early ventilation with oxygen is usually recommended. Passive oxygenation should be provided by a non-rebreathing mask covered by a surgical mask.6 However, any action or invasive procedure on the airway that is performed without proper protection with PPE will put the rescuer at significant risk of infection. Therefore, in hypothetical hypoxemic arrest, initiation of chest compression-only CPR seems to be safer. The procedure of cardiac arrest recognition includes the search and confirmation of the absence of signs of life and the absence of normal breathing, as previously mentioned. If there is doubt about the diagnosis of cardiac arrest, the recommendation is to start chest compressions until more experienced help arrives.
CPR starts only with chest compressions, and the patient’s underlying heart rhythm should be checked as soon as possible. A mechanical compression device (LUCAS device, AutoPulse) should be used as soon as available.4 , 6 , 10 Mouth-to-mouth ventilation, including the use of a pocket-mask, is avoided. If oxygen is already administered to the patient with a face mask (Venturi type), the mask remains on the patient’s face during chest compressions.
Bystanders who are not healthcare professionals (already wearing full PPE) may be able to provide support while chest compressions are ongoing and before the resuscitation team arrives. The rest (team members and support staff) must wear full PPE before taking over the CPR procedure from those who initially responded to the cardiac arrest.
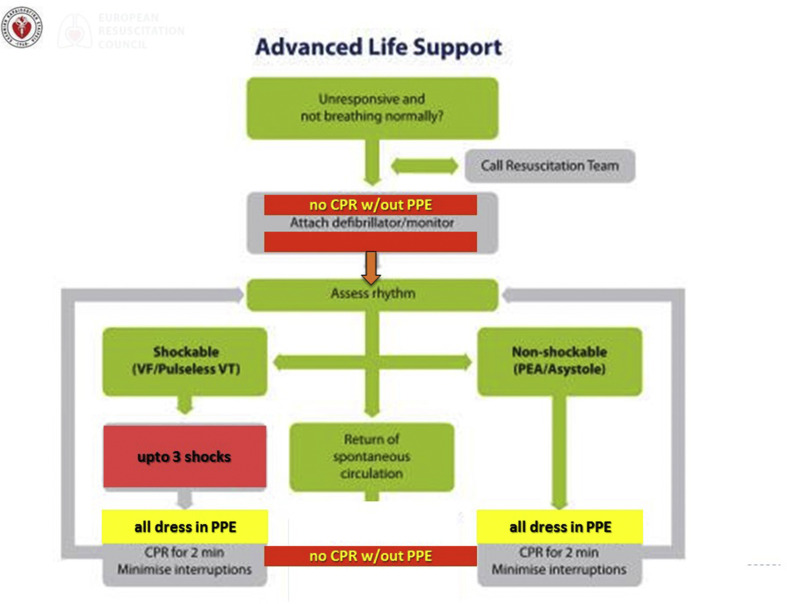
If there is a shockable rhythm, defibrillation should be given quickly; early Return of Spontaneous Circulation (ROSC) can prevent the need for invasive airway management and invasive ventilation. In cases where defibrillation is not performed with self-adhesive defibrillation pads but with handheld defibrillator paddles, we emphasize the non-disconnection of the closed breathing circuit in order to reduce the possibility of airborne dispersion from the victim’s respiratory secretions. In adjustment of the basic ALS algorithm, at shockable rhythms, we deliver not only one but up to three shocks in the attempt to restore the rhythm (Fig. 2 ). Patients may present cardiac arrest caused either directly by Covid-19 infection or by a comorbidity. It is important to identify any reversible causes (e.g. thrombotic events such as acute myocardial infarction or pulmonary embolism) before discussing with members of the group the possibility of discontinuing CPR.
Figure 2.
Adjusted algorithm of advanced in-hospital CPR (ALS) (from Hellenic Society of Cardiology) in Covid-19 pandemic. Key points of change are shown in red: a) do not start ALS CPR without PPE b) immediate rhythm check and up to 3 defibrillation attempts.
At the end of CPR, the equipment used during CPR is discarded or sterilized, following local recommendations. All work surfaces used for airway management/resuscitation should also be cleaned accordingly. Specifically, ensure that the equipment used in the airway procedures (e.g. laryngoscopes, face masks) is not left on the patient’s pillow but placed on a tray.
All PPE must be safely removed. Hand hygiene plays a very important role in reducing transmission. After performing CPR, even only with chest compressions, all rescuers should wash their hands thoroughly with soap and water. Alcohol-based hand sanitizer gels or even pure alcohol are an alternative solution.5 , 9 , 11 , 12 The above instructions have been visualized in a video by the Hellenic Society of Cardiology (https://youtu.be/L98gv0w4iwo) (special thanks to Drs A Synetos and M Kalogridaki).
The Covid-19 pandemic resulted in the loss of thousands of lives, and many more people are hospitalized in simple beds or in intensive care units, both globally and in locally in Greece. More specifically, in victims of cardiac arrest, both in- and out- of hospital, the increased mortality and the high contagiousness of the SARS-CoV-2 virus raised new questions, of both medical as well as of moral nature for CPR rescuers. What we all learn in resuscitation, that we cannot harm the victim and therefore do the most/best we can, is no longer true in everyday reality. While until recently, CPR with simple precautions and skills, was completely harmless to the members of the group, this is no longer valid. What we need to think about now and incorporate into decision-making in the resuscitation process is the distribution of our limited human and material resources, the potentially very poor outcome of patients with Covid-19 and cardiac arrest, and especially that a potential infection of health professionals can lead to lack of health professionals in the near future. This shortage can lead to multiple deaths from the initial death we tried to prevent.
Although this was not fully perceived in Greece due to successful restriction of the Covid-19 pandemic (sick and hospitalized patients, fatalities) during the so-called first wave, globally, the moral compass with regard to resuscitation shifted considerably. The Hippocratic balance of “benefit or do no harm” of the acceptable risks for patients and healthcare professionals (physicians, nurses) has clearly shifted, and modern medicine has changed with it.
Conflict of interest
All authors report no relevant conflict of interest.
Footnotes
Peer review under responsibility of Hellenic Society of Cardiology.
References
- 1.Baldi E., Sechi G.M., Mare C., et al. Out-of-Hospital Cardiac Arrest during the Covid-19 Outbreak in Italy. N Engl J Med. 2020 doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fritz Z., Perkins G.D. Cardiopulmonary resuscitation after hospital admission with covid-19. BMJ. 2020;369:m1387. doi: 10.1136/bmj.m1387. [DOI] [PubMed] [Google Scholar]
- 3.Kramer D.B., Lo B., Dickert N.W. CPR in the Covid-19 Era - An Ethical Framework. N Engl J Med. 2020 doi: 10.1056/NEJMp2010758. [DOI] [PubMed] [Google Scholar]
- 4.Latsios G., Antonopoulos A., Vogiatzakis N., et al. Successful primary PCI during prolonged continuous cardiopulmonary resuscitation with an automated chest compression device (AutoPulse) Int J Cardiol. 2016;225:258–259. doi: 10.1016/j.ijcard.2016.10.023. [DOI] [PubMed] [Google Scholar]
- 5.Nolan J.P., Monsieurs K.G., Bossaert L., et al. European Resuscitation Council COVID-19 guidelines executive summary. Resuscitation. 2020;153:45–55. doi: 10.1016/j.resuscitation.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chahar P., Marciniak D. Cardiopulmonary resuscitation in COVID-19 patients. Cleve Clin J Med. 2020 Jun 11 doi: 10.3949/ccjm.87a.ccc040. [DOI] [PubMed] [Google Scholar]
- 7.Tao K.M., Hu Y., Zhu X.F., Zhang Y.C., Yang Y., Lu Z.J. Cardiac arrest during emergency intubation in an elderly patient with confirmed coronavirus disease 2019. J Clin Anesth. 2020;66:109951. doi: 10.1016/j.jclinane.2020.109951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang M., Dong H., Lu Z. Role of anaesthesiologists during the COVID-19 outbreak in China. Br J Anaesth. 2020;124:666–669. doi: 10.1016/j.bja.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shao F., Xu S., Ma X., et al. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation. 2020;151:18–23. doi: 10.1016/j.resuscitation.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Latsios G., Mpompotis G., Tsioufis K., et al. Advanced cardiopulmonary resuscitation (CPR) in the Catheterization Laboratory: Consensus document of the Working Groups of 1) Cardiopulmonary Resuscitation/Acute Cardiac Care and 2) Hemodynamic and Interventional Cardiology, Hellenic Cardiological Society. Hellenic J Cardiol. 2017;58:396–400. doi: 10.1016/j.hjc.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Perkins G.D., Morley P.T., Nolan J.P., et al. International Liaison Committee on Resuscitation: COVID-19 consensus on science, treatment recommendations and task force insights. Resuscitation. 2020;151:145–147. doi: 10.1016/j.resuscitation.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edelson D.P., Sasson C., Chan P.S., et al. Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19: From the Emergency Cardiovascular Care Committee and Get With The Guidelines-Resuscitation Adult and Pediatric Task Forces of the American Heart Association. Circulation. 2020;141:e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]