Abstract
Introduction
This systematic review and meta-analysis aimed to evaluate the prevalence of coronavirus disease 2019 (COVID-19) and its impact on mortality in patients with hip fracture.
Methods
We performed a systematic literature search in PubMed, Cochrane Central Database, and medRvix from inception up to July 13, 2020 on research articles that enrolled hip fracture patients who had information on COVID-19 and clinically validated definition of death.
Results
A total of 984 participants from 6 studies were included in our study. The pooled prevalence of COVID-19 was 9% [95% CI: 7–11%]. The mortality rate in patients with concomitant hip fracture and COVID-19 was found to be 36% (95% CI: 26–47%), whereas the mortality rate in hip fracture without COVID-19 is 2% (95% CI: 1–3%). Meta-analysis showed that COVID-19 was associated with a seven-fold increase in risk (RR 7.45 [95% CI: 2.72, 20.43], p < 0.001; I2: 68.6%) of mortality in patients with hip fracture. Regression-based Harbord’s test showed no indication of small-study effects (p = 0.06).
Conclusion
The present meta-analysis showed that COVID-19 increased the risk of mortality in patients with hip fracture.
Trial registration
This study is registered with PROSPERO, July 21, 2020, number CRD42020199618. Available from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020199618.
Keywords: COVID-19, Hip fracture, Proximal femur fracture, Hip surgery, Mortality
1. Introduction
To date, the transmission and impact of Coronavirus Disease 2019 (COVID-19) have been more devastating than that of its predecessors, severe acute Respiratory Syndrome (SARS) and Middle East respiratory syndrome (MERS).1 The current pandemic has stretched the capacity of healthcare providers worldwide in providing medical services to the breaking point, not only due to the surge in the numbers of patients but also because certain groups of people are at a higher risk of worse outcomes. Patients with hip fractures are among the highest risk groups for developing severe COVID-19, because they are typically elderly, have disproportionate body composition, lower bone mineral density, and reduced mobility, and frequently suffer from chronic illnesses.2, 3, 4, 5, 6, 7
Hip fracture patients with underlying comorbidities, such as hypertension, diabetes, chronic lung disease, and cardiovascular and cerebrovascular diseases, are particularly vulnerable to developing complications from COVID-19 infection, even death.8, 9, 10, 11, 12, 13, 14, 15, 16 Furthermore, healthcare workers, including surgeon and staff in the operating theatre, have a markedly increased risk of contracting the SARS-Coronavirus-2 (SARS-CoV-2) as a result of the surgical management of patients with this pathology.17 Moreover, considering the widespread implementation of lockdown, post-operative follow-up and rehabilitation represent additional challenges for both patients and healthcare providers. This systematic-review and meta-analysis aimed to evaluate the prevalence of COVID-19 and its impact on mortality in patients with hip fracture.
2. Methods
This study is registered with PROSPERO, July 21, 2020, number CRD42020199618.
2.1. Eligibility criteria
Research articles that enrolled hip fracture patients who had information on COVID-19 and the clinically validated definition of death were included in this study. Abstract-only publications, review articles, commentaries, letters, and case reports were not included. In addition, we excluded studies that did not report key exposures or outcomes of interest.
2.2. Search strategy and study selection
We performed a systematic literature search in PubMed, Cochrane Central Database, and medRvix from inception up until July 13, 2020 using the following keywords: (“COVID-19” OR “SARS-CoV-2” OR “Coronavirus” OR “2019-nCoV”) AND (“Fracture” OR “Trauma”). After removal of duplicate records, two authors independently screened the titles and abstracts of the remaining articles based on the inclusion and exclusion criteria.
2.3. Data extraction
Data extraction was carried out independently by two authors using standardized extraction forms that included author, year, study design, number of subjects, age, sex, hypertension, diabetes mellitus, cardiovascular diseases, periprocedural complications, percentage of surgery, percentage of thromboembolic events, and mortality.
In this meta-analysis, the outcome of interest was mortality, which is defined as non-survivor or death. The exposure in this meta-analysis was hip fracture or proximal femur fracture, where the diagnosis follows the included studies’ definition. In this study, patients were identified as COVID-19-positive cases if they had a positive oropharyngeal or nasopharyngeal swab test with real-time reverse transcription polymerase chain reaction (RT-PCR) for SARS-CoV-2 before, during, or after hospitalization for their hip fracture.
2.4. Statistical analysis
Meta-analysis was performed using STATA 16.0 (Statacorp LLC). Prevalence of COVID-19 and incidence of mortality were calculated and expressed as proportion and percentage. Risk ratios (RRs) and its 95% confidence intervals (CIs) were calculated for calculated for dichotomous outcomes using a random-effects model. p-value for effect estimate was two-tailed, and the statistical significance was set at ≤0.05. Heterogeneity was assessed using I,2 a value of >50% or p-value <0.10 indicated a statistically significant heterogeneity. Regression-based Harbord’s test was used to evaluate the small study effects.
3. Results
3.1. Baseline characteristics and study selection
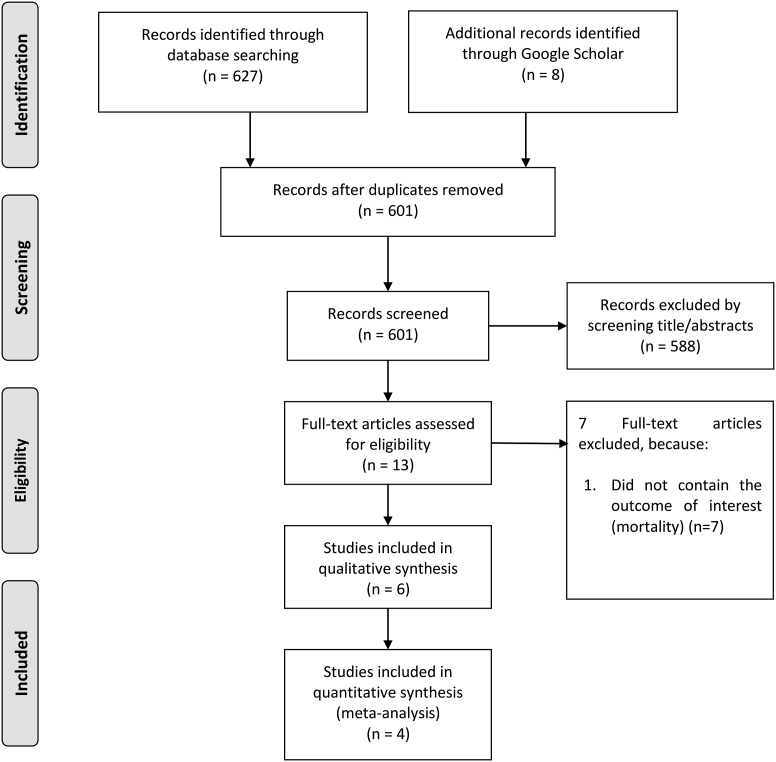
A total of 627 results were obtained, 601 records were screened after removal of duplicates. There were 13 potentially eligible records. Among them, 7 articles were excluded because they did not contain the outcome of interest (mortality). Ultimately, 6 clinical studies involving 984 participants were included in the systematic review and 4 in the meta-analysis.2, 3, 4, 5, 6, 7 [Fig. 1]. The baseline characteristics of the included studies is displayed in Table 1.
Fig. 1.
PRISMA flowchart.
Table 1.
Characteristics of the included studies.
| Authors | Study Design | Number of Subjects | Age (Mean/Median) (Years) | Female | Hypertension | Diabetes Mellitus | Cardiovascular Diseases | Periprocedural Complications | Undergo Surgery (%) | Thromboembolic Events (%) | Mortality (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Egol (2020) | Prospective Cohort | 17 vs 107 | 82.4 vs 83.4 | 5/17 vs 73/107 | 11/17 vs 67/107 | 7/17 vs 20/107 | 8/17 vs 40/107 | Sepsis, bacterial pneumonia, viral pneumonia, DVT/PE, MI, stroke, acute respiratory failure, cardiac arrest, AKI, decubitus ulcer, UTI, anemia, hypotension, atrial fibrillation | 76.5 vs 100 | 11.8 vs 2.8 | 35.3 vs 0.9 |
| LeBrun (2020) | Retrospective Cohort | 9 vs 40 | 86.5 vs 84.7 | 6/9 vs 38/40 | N/A | 3/9 vs 14/40 | 1/9 vs 8/40 (MI) | Pneumonia (any cause), DVT/PE, stroke, MI, cardiac arrhythmia, UTI, decubitus ulcer, anemia, acute respiratory failure | 78 vs 100 | N/A | 56 vs 4 |
| Vives (2020) | Retrospective Cohort | 23 vs 39 | 87 vs 85.2∗ | 8/13 vs 94/123∗ | N/A | N/A | N/A | N/A | 38.5 vs 96.7∗ | N/A | 30.4 vs 10.3 |
| Cheung (2020) | Retrospective Cohort | 10 vs 0 | 79.7 vs 0 | 8/10 vs 0/0 | 7/10 vs 0/0 | 3/10 vs 0/0 | 2/10 vs 0/0 | Atypical pneumonia, anemia, blood transfusion, VTE, prolonged hypoxia requiring supplemental O2, respiratory failure, AKI | 100 vs 0 | 1/10 vs 0/0 | 10 vs 0 |
| Hall (2020) | Retrospective Cohort | 27 vs 290 | 83.6 vs 80.4 | 13/27 vs 198/290 | N/A | N/A | N/A | N/A | 92.6 vs 95.9 | N/A | 33.3 vs 82.8 |
| Kayani (2020) | Retrospective Cohort | 82 vs 340 | 71.9 vs 72.7 | 51/82 vs 204/340 | N/A | N/A | N/A | Respiratory infection, AKI, septic shock, MI, ARDS, multiorgan dysfunction, severe metabolic acidosis, coagulation dysfunction | 100 vs 100 | N/A | 30.5 vs 10.3 |
∗compares non-survivor group vs survivor group.
This table compares COVID-19 (+) group vs COVID-19 (−) group.
DVT/PE: Deep venous thrombosis/Pulmonary embolism; MI: Myocardial infarction; AKI: Acute kidney injury; UTI: Urinary tract infection; VTE: Venous thromboembolism.
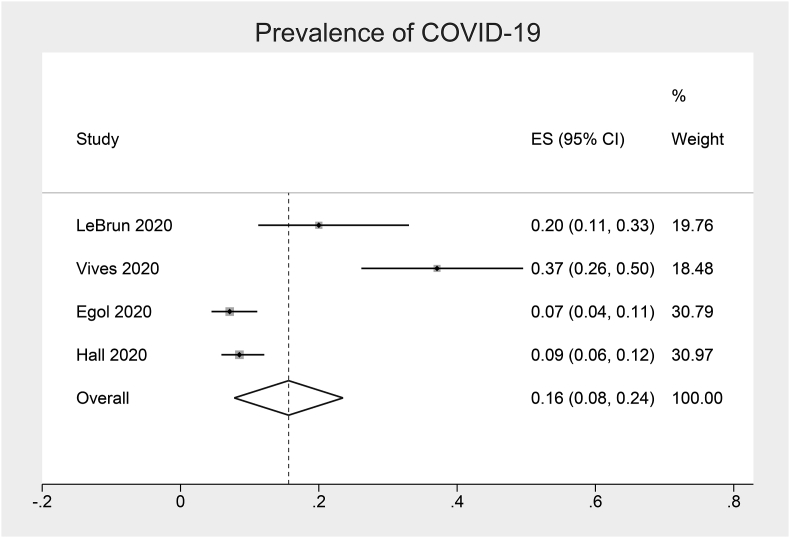
Prevalence of COVID-19 in patients with hip fracture.
We found that the pooled prevalence of COVID-19 was 9% [95% CI: 7–11%] [Fig. 2]. Moreover, the mortality rate in patients with hip fracture and concomitant COVID-19 was found to be 36% (95% CI: 26–47%), whereas the mortality rate in hip fracture without COVID-19 is 2% (95% CI: 1–3%).
Fig. 2.
Prevalence of COVID-19 in patients with hip fracture.
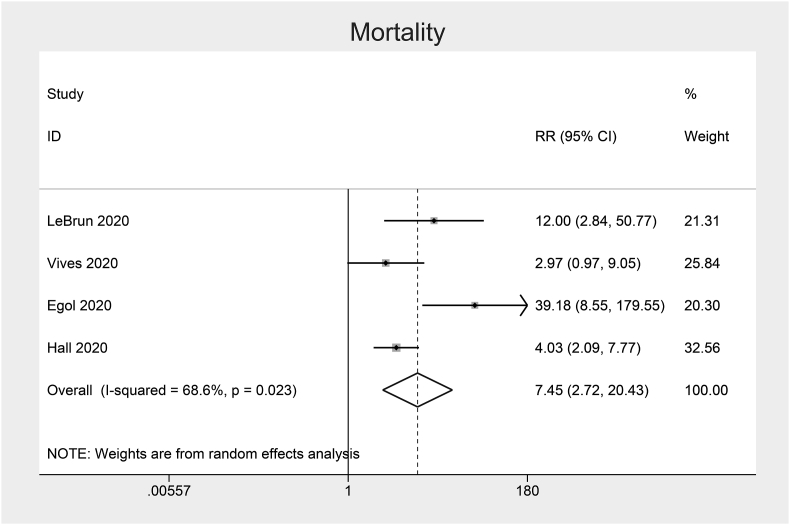
3.2. Mortality in patients with hip fracture
Meta-analysis showed that COVID-19 was associated with a seven-fold increase in risk (RR 7.45 [95% CI: 2.72, 20.43], p < 0.001; I2: 68.6%, p = 0.022) [Fig. 3] of mortality in patients with hip fracture.
Fig. 3.
Forest-plot showing the association between COVID-19 and mortality in patients with hip fracture.
3.3. Adverse events in patients undergoing hip surgery
In patients undergoing hip surgery (n = 739), postoperative mortality rates was found higher in those with COVID-19 positive (28%) compared to the COVID-19 negative counterparts (10.3%). Furthermore, those who were COVID-19 positive had increased risk of postoperative complications (85.9%) and increased length of hospitalization (mean 13.2 days) compared to those who were COVID-19 negative. We only included subjects from two studies by Cheung et al. and Kayani et al., because the remainder of the studies did not enclose detailed data related to the COVID-19 status, surgical treatment option, and post-operative adverse events.
3.4. Publications bias
Regression-based Harbord’s test showed no indication of small-study effects (p = 0.06). Funnel plot analysis was not performed due to lack of studies.
4. Discussion
Hip fractures, also known as proximal femur fractures, are the most common trauma-related fractures.18 This type of fracture are among the most commonly encountered fractures in COVID-19 cases.19 The hip joint consists of the femoral head (ball) and the acetabulum (socket), where the femoral neck connects the femoral head to the proximal part of the femoral shaft and attaches to the intertrochanteric region. Fractures in any of these locations are called hip fractures. In terms of anatomic location, hip fractures are classified as intracapsular (femoral neck and head) and extracapsular (intertrochanteric and subtrochanteric fractures). The management usually involves a multidisciplinary approach which includes addressing underlying medical conditions, providing appropriate surgical fixation, and promoting early mobilization and rehabilitation to ensure a return to basic functional mobility, maintenance of activities of daily livings (ADLs), and independence.20,21 Hip fractures substantially increase the risk of death and major morbidity in the elderly.22,23
Meta-analysis demonstrated that COVID-19 was associated with increased risk of mortality in patients with hip fracture. Worldwide, the mortality rate of patients with COVID-19 is mostly around 3–4%, and mortality in the pooled analysis of hip fracture patients without COVID-19 is 4%, both are markedly lower than the 36% found for patients with hip fracture and concomitant COVID-19. There are several possible reasons to explain this phenomenon. Coagulopathy in COVID-19 is associated with a markedly increased the risk of venous thromboembolism (VTE) and disseminated intravascular coagulation (DIC).24,25 Endothelial cells dysregulation and platelets and leukocytes activation result in excessive thrombin generation and inhibition of fibrinolysis both locally and systemically, causing fibrin deposition with subsequent tissue damage and microangiopathy.26 These factors, combined with lack of physical activity and reduced mobility associated with hip fractures, predispose patients to a higher risk of thromboembolic complications.2, 3, 4, 5, 6, 7,27
Injuries and associated surgical procedures associated with this pathology can cause inflammation and subsequent release of inflammatory cytokines which potentiate COVID-19 induced inflammation, possibly leading to cytokine storm. Virus-driven cytokine storm can lead to serious complications, including acute respiratory distress syndrome (ARDS) and multiple organ dysfunction (e.g. acute liver injury, acute kidney injury), which are several possible causes of inpatient mortality.28 Furthermore, major vascular injuries can deteriorate the hemodynamic conditions of the patient, and adjacent nerve injuries can cause weakness or paralysis which further aggravating their disability. Perioperative blood transfusions, surgical site infection, and urinary tract infection are also associated with an increased risk of death in hip fractures.22 Nevertheless, there are several factors that commonly coexists in patients with hip fracture, namely advanced age, obesity, and various comorbidities which are associated with increased severity and mortality of COVID-19.8, 9, 10, 11,14,15,29,30 Because of reduced functional reserves and weakened immune function, these individuals are more adversely affected by SARS-COV-2 infection. The poor prognosis can be attributed to a combination of these factors rather than purely attributed to a single factor.
The presence of surgery is indeed a risk factor for SARS-CoV-2 transmission to medical personnel through inhalation of infectious aerosols or viable viruses in the surgical smoke. Therefore, regardless of the presence of fever, cough, shortness of breath, or other acute respiratory infection symptoms, all candidates for surgery should be considered as possible COVID-19 cases. To avoid unexpected casualties to the patient, surgeon, or staff, screening and monitoring for COVID-19 in all surgical patients should be mandatory. Shortages of surgeons and staff due to nosocomial spread can be serious issue if disease prevention, mitigation, and containment are not carried out properly. In addition to the presence of more than three pre-existing comorbidities, smoking, which is associated with increased severity in COVID-19, was found to independently increase postoperative mortality rates in COVID-19 patients.7,14 After surgery, thromboembolic events can occur in patients due to restricted mobility. In certain cases, postoperative pulmonary complications could be observed within a few days or weeks after surgery.17
Post-operative management, including follow-up and rehabilitation, should be arranged cautiously. Moving back and forth to healthcare facilities increases the risk of contracting SARS-CoV-2 for susceptible individuals.31, 32 An online survey showed that the need for clinical and radiological follow-up as well as sutures removal was avoided during such pandemic, given that controlling COVID-19 transmission has been a major focus for most countries.33 Currently, teleconsultation and telerehabilitation facilities are being utilized widely, and the clinical outcomes of this virtual option are not inferior to the standard face-to-face appointments for the majority of cases.34,35 These audiovisual-guided sessions have been found to improve the effectiveness of post-operative follow-up and rehabilitation, increase patient satisfaction, and enhance Quality-Adjusted Life Years (QALYs) gained. Furthermore, this online-based service is more cost-effective and help reduce travel expenses and save time.36,37 However, certain cases still require in-person appointments, such as removal of plates and implants.
As hip fracture patients with concomitant COVID-19 may suffer from hypercoagulability, the use of anticoagulants and/or antiplatelets is crucial in preventing adverse outcomes.24,25 Furthermore, limited activity and function related to the fracture side contributes to the rise in D-dimer levels and hence the development of serious, life-threatening thromboembolic complications.38 Given their limited mobility, simple exercises are recommended to preserve muscle strength and flexibility and maintain fitness level while avoiding surgery-associated complications and secondary risks due to prolonged stay in bed. Such high-risk individuals should aim to maintain their performance of ADLs during the rehabilitation period. Promoting rapid mobilization while maintaining a physically active lifestyle are advised to every patient who undergoes hip surgery as it can improve the immune function, reduce the risk of illnesses, and eventually lower the risk of mortality.22, 27, 39, 40, 41
During the COVID-19 pandemic, the number of motor vehicle accident has plummeted due to extensive lockdown, travel bans, and imposed quarantine which have led to a drastic reduction in the load of fracture patients worldwide. However, patients with lower energy and more porous bones are still seeking treatment in emergency service with the incidence of fragility fractures remains unaffected.19 An observational study in Spain demonstrated that the number of osteoporotic hip fractures remained stable over the course of the outbreak even though the frequency of most emergency traumatology visits declined.42 On the other hand, an observational study in Italy showed that the number of hip fractures decreased during the outbreak, due to restrictions imposed nationally, but the number of complications and deaths has increased significantly.43
Due to an emergency situation, elective surgeries have been suspended to limit the spread of COVID-19. Given that urgent and emergency surgeries are still running as normal, developing contingency plans for reallocating resources are required to maintain these services even when the pandemic worsens.33,44 Under such a pandemic, the main approach of most orthopaedic surgeon was to preserve the hospital resources, reduce the risk of in-hospital transmission, and protect their colleagues and staff. In numerous countries, surgical activities for various fractures are still being abandoned despite the availability of guidelines and protocols due to lack of experience in managing such patients, shortage of resources, limited access to negative pressure operation theatres, and stress and anxiety related to COVID-19.19 Separating COVID-19 or non-COVID-19 wards and setting up a “COVID-19” operating room are suggested to handle surgical emergency cases with positive or undetermined swab results.45 Various risk stratification tools that mortality and morbidity risk of patients have been developed to predict 30-day mortality risk after surgery, with the Nottingham Hip Fracture Score (NFHS) having reasonable discrimination and providing the most promising results.23
Hip surgery can contribute to the patient’s overall stability, enhanced physiological ventilation, seated mobilization, and general comfort in bed.46 It has been found that the reduced time to surgery (within 24 h of emergency room admission) in elderly patients with hip fracture significantly decreases 1-year mortality and morbidity.47 Moreover, studies found that delays in surgery for more than 24 h after hospital admission may increase the odds of 30-day all-cause mortality and complication in hip fracture patients.19,48,49 During the COVID-19 pandemic, any delays in attending medical services may prove detrimental, especially in cases related to fractures and trauma.50 Suboptimal management may cause devastating complications such as fracture malunion or nonunion, avascular necrosis, or fixation hardware failure.20 Even worse, the risk of poor outcomes is exacerbated by the patients’ characteristics, including advanced age and the presence of comorbidities.8, 9, 10, 11,14,25,28 Therefore, these patients may require priority for early surgery even more than usual, which can help reduce the length of hospitalization and decrease the risks of nosocomial infection, post-operative adverse events, and in-hospital mortality.
Hip fractures are devastating injuries that frequently cause chronic disability and may lead to premature death, especially in the elderly. Considering the rapid growth of the elderly population, these fractures will become one of the biggest public health problems in the future. The elderly have weaker, more porous bones and are more prone to falls due to poor balance, side effects from medications, and difficulty maneuvering around environmental hazard. This study emphasizes that there is a higher mortality rate in patients with a hip fracture and an associated positive test for COVID-19. However, regardless of the COVID-19 status, hip fracture patients can do well during this pandemic if given proper monitoring and treatment, and can eventually be discharged home.
A proper algorithm for the treatment of hip fractures during the pandemic must be implemented, starting from the use of personal protective equipment by patients and health workers, emergency room isolation, hospital admission, peri-operative protocols, to inpatient protocols.42 Restarting elective surgery in the midst of COVID-19 pandemic is particularly challenging and extra precautions must be taken so that the elective procedure pathways can be safely resumed and patients can be effectively managed with a low risk of SARS-CoV-2 infection. A two week self-isolation period is required before elective surgery to minimize the risk of contracting COVID-19, which is consistent with the observed incubation period of up to 14 days.51 Fast track or accelerated care pathway for hip fracture patients will ultimately reduce the total length of hospitalization without increasing the rates of mortality or complication in the short and long term.18
Limitation of this systematic review and meta-analysis include limited sample size and the wide CI of the effect estimates.
5. Conclusion
The present meta-analysis emphasized that COVID-19 increased the risk of mortality in patients with hip fracture. Physicians treating COVID-19 positive patients should counsel the patient and his/her families of the significantly increased risks of poor outcomes after hip fracture. We define a new high-risk population with a hip fracture with concomitant SARS-CoV-2 infection who had significantly increases the rates of inpatient mortality, partly due to older age and comorbidity profiles. Appropriate management, including infection-control measures, hospital admission protocols, early surgery, and adequate monitoring, follow-up, and rehabilitation, is the best measure to minimize the risk of mortality and other adverse events in hip fracture patients during such pandemic.
Funding
None
CRediT authorship contribution statement
Michael Anthonius Lim: confirm being the only contributors of this work and have approved it for publication. Raymond Pranata: confirm being the only contributors of this work and have approved it for publication.
Declaration of competing interest
The authors declare that they possess no commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgment
None.
Contributor Information
Michael Anthonius Lim, Email: lim.michael.a@gmail.com.
Raymond Pranata, Email: raymond_pranata@hotmail.com.
References
- 1.Petrosillo N., Viceconte G., Ergonul O., Ippolito G., Petersen E. COVID-19, SARS and MERS: are they closely related? Clin Microbiol Infect. 2020;26(6):729–734. doi: 10.1016/j.cmi.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muñoz Vives J.M., Jornet-Gibert M., Cámara-Cabrera J. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic: preliminary results of the Spanish HIP-covid observational study. J Bone Joint Surg Am. May 2020 doi: 10.2106/JBJS.20.00686. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Egol K.A., Konda S.R., Bird M.L. Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a New York city perspective. J Orthop Trauma. May 2020 doi: 10.1097/BOT.0000000000001845. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.LeBrun D.G., Konnaris M.A., Ghahramani G.C. Hip fracture outcomes during the COVID-19 pandemic: early results from New York. J Orthop Trauma. May 2020 doi: 10.1097/BOT.0000000000001849. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheung Z.B., Forsh D.A. Early outcomes after hip fracture surgery in COVID-19 patients in New York City. J Orthop. 2020;21:291–296. doi: 10.1016/j.jor.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall A.J., Clement N.D., Farrow L. IMPACT-Scot report on COVID-19 and hip fractures. Bone Joint J. 2020;7:1–10. doi: 10.1302/0301-620X.102B9.BJJ-2020-1100.R1. Published online July. [DOI] [PubMed] [Google Scholar]
- 7.Kayani B., Onochie E., Patil V. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Joint J. 2020;7:1–10. doi: 10.1302/0301-620X.102B9.BJJ-2020-1127.R1. Published online July. [DOI] [PubMed] [Google Scholar]
- 8.Pranata R., Lim M.A., Huang I., Raharjo S.B., Lukito A.A. Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: a systematic review, meta-analysis and meta-regression. JRAAS - J Renin-Angiotensin-Aldosterone Syst. 2020;(April-June):1–11. doi: 10.1177/14703203209268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang I., Lim M.A., Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia – a systematic review, meta-analysis, and meta-regression: diabetes and COVID-19. Diabetes Metab Syndr Clin Res Rev. 2020;14(4):395–403. doi: 10.1016/j.dsx.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim M.A., Huang I., Yonas E., Vania R., Pranata R. A wave of non-communicable diseases following the COVID-19 pandemic. Diabetes Metab Syndr Clin Res Rev. 2020;14(5):979–980. doi: 10.1016/j.dsx.2020.06.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pranata R., Huang I., Lim M.A., Wahjoepramono P.E.J., July J. Impact of cerebrovascular and cardiovascular diseases on mortality and severity of COVID-19 - systematic review, meta-analysis, and meta-regression. J Stroke Cerebrovasc Dis. 2020 doi: 10.1016/j.jstrokecerebrovasdis.2020.104949. Published online May 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pranata R., Lim M.A., Yonas E., Siswanto B.B., Meyer M. Out-of-hospital cardiac arrest prognosis during the COVID-19 pandemic. Intern Emerg Med. 2020 doi: 10.1007/s11739-020-02428-7. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pranata R., Tondas A.E., Huang I. Potential role of telemedicine in solving ST-segment elevation dilemmas in remote areas during the COVID-19 pandemic. Am J Emerg Med. 2020;8 doi: 10.1016/j.ajem.2020.06.012. Published online June. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pranata R., Soeroto A.Y., Huang I., Lim M.A., Santoso P. Effect of chronic obstructive pulmonary disease and smoking on the outcome of COVID-19. Int J Tubercul Lung Dis. 2020 doi: 10.5588/ijtld.20.0278. Published online. [DOI] [PubMed] [Google Scholar]
- 15.Huang I., Pranata R. Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis. J Intensive Care. 2020;8(1):36. doi: 10.1186/s40560-020-00453-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pranata R., Permana H., Huang I. The use of renin angiotensin system inhibitor on mortality in patients with coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Diabetes Metab Syndr Clin Res Rev. 2020 doi: 10.1016/j.dsx.2020.06.047. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blouhos K., Boulas K.A., Paraskeva A. Understanding surgical risk during COVID-19 pandemic: the rationale behind the decisions. Front Surg. 2020;7:33. doi: 10.3389/fsurg.2020.00033. https://www.frontiersin.org/article/10.3389/fsurg.2020.00033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gomez M., Marc C., Talha A. Fast track care for pertrochanteric hip fractures: how does it impact length of stay and complications? Orthop Traumatol Surg Res. 2019;105(5):979–984. doi: 10.1016/j.otsr.2019.04.017. [DOI] [PubMed] [Google Scholar]
- 19.Kumar Jain V., Lal H., Kumar Patralekh M., Vaishya R. Fracture management during COVID-19 pandemic: a systematic review. J Clin Orthop Trauma. 2020;11:S431–S441. doi: 10.1016/j.jcot.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheehan S.E., Shyu J.Y., Weaver M.J., Sodickson A.D., Khurana B. Proximal femoral fractures: what the orthopedic surgeon wants to know. Radiographics. 2015;35(5):1563–1584. doi: 10.1148/rg.2015140301. [DOI] [PubMed] [Google Scholar]
- 21.Mittal R., Banerjee S. Proximal femoral fractures: principles of management and review of literature. J Clin Orthop trauma. 2012;3(1):15–23. doi: 10.1016/j.jcot.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Velez M., Palacios-Barahona U., Paredes-Laverde M., Ramos-Castaneda J.A. Factors associated with mortality due to trochanteric fracture. A cross-sectional study. Orthop Traumatol Surg Res. 2019;106(1):135–139. doi: 10.1016/j.otsr.2019.06.022. [DOI] [PubMed] [Google Scholar]
- 23.de Jong L., Mal Klem T., Kuijper T.M., Roukema G.R. Validation of the Nottingham Hip Fracture Score (NHFS) to predict 30-day mortality in patients with an intracapsular hip fracture. Orthop Traumatol Surg Res. 2019;105(3):485–489. doi: 10.1016/j.otsr.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 24.Yin S., Huang M., Li D., Tang N. Difference of coagulation features between severe pneumonia induced by SARS-CoV2 and non-SARS-CoV2. J Thromb Thrombolysis. 2020 doi: 10.1007/s11239-020-02105-8. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang I., Pranata R., Lim M.A., Oehadian A., Alisjahbana B. C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis. Ther Adv Respir Dis. 2020;14 doi: 10.1177/1753466620937175. 1753466620937175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lillicrap D. Disseminated intravascular coagulation in patients with 2019-nCoV pneumonia. J Thromb Haemostasis. 2020;18(4):786–787. doi: 10.1111/jth.14781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lim M.A., Pranata R. Sports activities during any pandemic lockdown. Ir J Med Sci. 1971 doi: 10.1007/s11845-020-02300-9. Published online 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lim M.A., Pranata R., Huang I., Yonas E., Soeroto A.Y., Supriyadi R. Multiorgan failure with emphasis on acute kidney injury and severity of COVID-19: systematic review and meta-analysis. Can J Kidney Heal Dis. 2020;7 doi: 10.1177/2054358120938573. 2054358120938573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pranata R., Huang I., Lukito A.A., Raharjo S.B. Elevated N-terminal pro-brain natriuretic peptide is associated with increased mortality in patients with COVID-19: systematic review and meta-analysis. Postgrad Med. 2020:137884. doi: 10.1136/postgradmedj-2020-137884. Published online May 2020:postgradmedj. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pranata R., Lim M.A., Yonas E. Body mass index and outcome in patients with COVID-19: a dose-response meta-analysis. Diabetes Metab. 2020 doi: 10.1016/j.diabet.2020.07.005. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lim M.A., Pranata R. The importance of COVID-19 prevention and containment in hemodialysis unit. Clin Med Insights Circulatory, Respir Pulm Med. 2020;14 doi: 10.1177/1179548420939256. 1179548420939256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lim M.A. Hemodialysis centers among the highest risk areas for COVID-19 transmission. American Journal of Preventive Medicine and Public Health. 2020;6(4):109–110. doi: 10.5455/ajpmph.20200502092630. [DOI] [Google Scholar]
- 33.Thaler M., Khosravi I., Hirschmann M.T. Disruption of joint arthroplasty services in Europe during the COVID-19 pandemic: an online survey within the European Hip Society (EHS) and the European Knee Associates (EKA) Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1712–1719. doi: 10.1007/s00167-020-06033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lim M.A., Pranata R. Teleorthopedic: a promising option during and after the coronavirus disease 2019 (COVID-19) pandemic. Front Surg. 2020;7(62):1–4. doi: 10.3389/fsurg.2020.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lim M.A., Pranata R. Letter to the editor regarding ‘The challenging battle of mankind against COVID-19 outbreak: is this global international biological catastrophe the beginning of a new era?’ – is telehealth the future of orthopaedic and rehabilitation in post-COVID-19 era. J Orthop Surg. 2020;28(3):1–3. doi: 10.1177/2309499020947840. [DOI] [PubMed] [Google Scholar]
- 36.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16(1):483. doi: 10.1186/s12913-016-1717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buvik A., Bergmo T.S., Bugge E., Smaabrekke A., Wilsgaard T., Olsen J.A. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21(2) doi: 10.2196/11330. e11330-e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mi B., Chen L., Xiong Y., Xue H., Zhou W., Liu G. Characteristics and early prognosis of COVID-19 infection in fracture patients. J Bone Joint Surg Am. 2020;102(9):750–758. doi: 10.2106/JBJS.20.00390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schwellnus M., Soligard T., Alonso J.-M. How much is too much? (Part 2) International Olympic Committee consensus statement on load in sport and risk of illness. Br J Sports Med. 2016;50(17) doi: 10.1136/bjsports-2016-096572. 1043 LP - 1052. [DOI] [PubMed] [Google Scholar]
- 40.Nielsen H.G. Current Issues in Sports and Exercise Medicine. IntechOpen; 2013. Exercise and immunity. Ch. 4. [DOI] [Google Scholar]
- 41.Lim M.A. Exercise Addiction and COVID-19-Associated Restrictions. Journal of Mental Health. 2020 doi: 10.1080/09638237.2020.1803234. [DOI] [PubMed] [Google Scholar]
- 42.Nuñez J.H., Sallent A., Lakhani K. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020;51(7):1414–1418. doi: 10.1016/j.injury.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maniscalco P., Poggiali E., Quattrini F. Proximal femur fractures in COVID-19 emergency: the experience of two Orthopedics and Traumatology Departments in the first eight weeks of the Italian epidemic. Acta Biomed. 2020;91(2):89–96. doi: 10.23750/abm.v91i2.9636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liebensteiner M.C., Khosravi I., Hirschmann M.T., Heuberer P.R. Joint-Surgery B of the A-S of A and, Thaler M. Massive cutback in orthopaedic healthcare services due to the COVID-19 pandemic. Knee Surg Sports Traumatol Arthrosc. April 30, 2020:1–7. doi: 10.1007/s00167-020-06032-2. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Giuntoli M., Bonicoli E., Bugelli G., Valesini M., Manca M., Scaglione M. Lessons learnt from COVID 19: an Italian multicentric epidemiological study of orthopaedic and trauma services. J Clin Orthop Trauma. 2020;11(4):721–727. doi: 10.1016/j.jcot.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Catellani F., Coscione A., D’Ambrosi R., Usai L., Roscitano C., Fiorentino G. Treatment of proximal femoral fragility fractures in patients with COVID-19 during the SARS-CoV-2 outbreak in northern Italy. J Bone Joint Surg Am. 2020;102(12) doi: 10.2106/JBJS.20.00617. e58-e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Delaveau A., Saint-Genez F., Gayet L.-E., Paccalin M., Ounajim A., Vendeuvre T. Impact of time to surgery in upper femoral fracture in orthogeriatrics. Orthop Traumatol Surg Res. 2019;105(5):975–978. doi: 10.1016/j.otsr.2019.04.018. [DOI] [PubMed] [Google Scholar]
- 48.Nyholm A.M., Gromov K., Palm H., Brix M., Kallemose T., Troelsen A. Time to surgery is associated with thirty-day and ninety-day mortality after proximal femoral fracture: a retrospective observational study on prospectively collected data from the Danish fracture Database collaborators. J Bone Joint Surg Am. 2015;97(16):1333–1339. doi: 10.2106/JBJS.O.00029. [DOI] [PubMed] [Google Scholar]
- 49.Grigoryan K.V., Javedan H., Rudolph J.L. Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma. 2014;28(3) doi: 10.1097/BOT.0b013e3182a5a045. https://journals.lww.com/jorthotrauma/Fulltext/2014/03000/Orthogeriatric_Care_Models_and_Outcomes_in_Hip.13.aspx [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lim M.A., Pranata R. Disaster Med Public Health Prep; 2020. Impending Catastrophe of Delayed Fracture Management during the COVID-19 Pandemic; pp. 1–5. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Trowbridge S., Wignadasan W., Davenport D., Sarker S., Hunter A., Gidwani S. Is it safe to restart elective day-case surgery? Lessons learned from upper limb ambulatory trauma during the COVID-19 pandemic. J Clin Orthop Trauma. 2020 doi: 10.1016/j.jcot.2020.07.023. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]