Abstract
Accessory bones in the region of the elbow are rare variants with high clinical significance as they may be confused with avulsion fractures. We investigated their prevalence and performed a statistical analysis to support their congenital origin. Their localization was mapped to show their exact site of occurrence. We evaluated anteroposterior and lateral X‐ray images of 2413 elbows in a Central European population from which a group of accessory bony structures was selected. Their character was evaluated, and accessory bones were identified. We used logistic regression to evaluate the potential relationship between the occurrence of accessory bones, the age of patients, and the occurrence of calcar olecrani. The prevalence of accessory bones of the elbow in the sample was 0.77%. Our results did not show a statistically significant relationship with the occurrence of calcar olecrani or with the age of patients. The most common type was os subepicondylare mediale (type V) in 0.46%, which was located distal to the medial epicondyle of the humerus, followed by os subepicondylare laterale (type III; 0.21%), situated laterally to the lateral epicondyle of the humerus. In comparison with previous reports, os sesamoideum mediale (type IV) was located more distally. Our data suggest that congenital accessory bones are a rare entity. Knowledge of their exact localization should be considered during diagnosis of avulsion fractures and other unclear diagnoses including accessory bony structures in the elbow region.
Keywords: accessory ossicles, elbow variability, sesamoid bones
Accessory bones in the region of the elbow are rare variants with high clinical significance as they may be confused with avulsion fractures. Their prevalence is less than 1%, with the most common localization slightly distal to the medial epicondyle of the humerus.

1. INTRODUCTION
Accessory bones in the region of the elbow joint are rare variants of the upper extremity skeletal system. Although they have been previously described in many case reports, to the best of our knowledge, there is no research concerning their prevalence.
Wood and Campbell (1994) classified seven distinct types of accessory bones based on a review of the literature and their own research. Three of these types, C, D and G, result from the failure of ossification centres to unite with the rest of the humeral condyle or the proximal end of the ulna. These include failure of the radial (type C), and ulnar (type D) apophyses of the humerus to unite with the medial and lateral epicondyle, respectively, and failure of the olecranon epiphysis to unite with the rest of the olecranon (type G), which is also referred to as a persistent epiphysis. Types D and F are sesamoid bones: type F is a sesamoid bone in the tendon of the brachialis muscle, and type D (also called patella cubiti) is a sesamoid bone in the tendon of the triceps brachii muscle. Types A and B are intra‐articular accessory bones. Type A is referred to as the os supratrochleare posterius and type B as the os supratrochleare anterius (Wood and Campbell, 1994). Both types A and B have been postulated to arise from separate ossification centres. Another theory is that os supratrochleare is as an accessory 'bone nucleus' of the olecranon (Obermann and Loose, 1983; Figure 1).
Figure 1.

Modified version of Wood and Campbell's classification: os supratrochleare anterius (I), in the older classification 'type A', os supratrochleare posterius (II), previously type B, os subepicondylare laterale (III), previously type C, os sesamoideum tricipitale (IV), previously types D and G, os subepicondylare mediale (V), previously type E, and os sesamoideum brachiale (VI), previously type F
To date, 35 cases of os supratrochleare posterius and three cases of os supratrochleare anterius have been described in the literature (Canamero et al., 2014). Eighteen cases of patella cubiti were presented in a literature review by Schwarz (1957), and later by Mittal et al. (2014). To the best of our knowledge, no case reports or prevalence studies describing the other sesamoid bones have been published, despite the fact that these bones are included in the classification mentioned above (Schwarz, 1957; Wood and Campbell, 1994).
The aim of the present study was to investigate the prevalence of the accessory bones of the elbow, to support their congenital origin by statistical analysis, and to show the precise localization of their occurrence as this has not been done before. Wood's classification has been modified according to these findings.
2. MATERIALS AND METHODS
We retrospectively evaluated anteroposterior and lateral X‐ray images of 2413 elbows taken at the Department of Radiology, Second Faculty of Medicine, Charles University and Motol University Hospital, in Prague, Czech Republic made between January 2013 and December 2017. All images were evaluated on a workstation with two monitors BARCO MDCG‐5221 (BARCO NV, Kortrijk, Belgium) with a resolution 2048×2560. We evaluated 1359 men with a mean (range) age of 40.57 (21–76) years and 1054 women with a mean (range) age of 43.68 (21–76) years. We excluded patients under the age of 21 years to ensure that growth plates were closed. Images with severe degenerative changes, dislocated or comminuted fractures, osteosynthesis material, total elbow arthroplasty, wrong positioning of the extremity or casting were excluded. This excluded 473 radiographs from further analysis. All images with accessory bony structures were saved and, according to their character, sorted into two groups: one consisting of images with pathological changes and the other with accessory bones.
Morphological features of a true accessory bone were defined as: (1) regular ovoid shape; (2) smooth margins; and (3) regular cortical to medullar ratio throughout the circumference. We used these criteria to differentiate accessory bones from avulsion fractures and degenerative changes. All of these criteria had to be fulfilled to consider an accessory bone candidate as a true accessory bone. All authors discussed images in the latter group and consulted with a specialist in skeletal radiology with 50 years of experience to re‐evaluate their character and find a consensus regarding origin to exclude all other possible causes mentioned in the previous literature (see below). A total of 101 radiographs considered as accessory bone candidates were excluded based on the above‐stated criteria. From these 101 accessory bone candidates, 15 were misclassified by a junior author and should not be present in the second group (seven were enostosis, four fractured calcar olecrani, two dislocated fractures and two synovial chondromatosis), 71 were mild degenerative changes and 15 were avulsion fractures. Afterwards they were sorted according to Wood‐Campbell's classification described above. Their localization is shown in Figure 2, and based on this, together with the existing literature, a slightly modified classification was proposed (Figure 1).
Figure 2.

Map of accessory bones found in our sample [Colour figure can be viewed at wileyonlinelibrary.com]
Under the assumption that the prevalence of accessory bones does not increase with age in the mature skeleton and that accessory bone candidates were more likely to be degenerative changes than congenital bones when calcar olecrani were present, we tested the relationship between the occurrence of accessory bones and the age of patients and the presence of calcar olecrani to check that we had not misclassified any degenerative changes as accessory bones.
The occurrence of accessory bones and the occurrence of calcar olecrani are binary variables and age is a positive integer variable. The inference was made using logistic regression with the occurrence of accessory bones as a dependent variable. Logistic regression was used to model the relationship of logged odds using the following linear model:
where x 1 and x 2 are the independent variables (in our case patient's age and the occurrence of calcar olecrani) and is the estimated probability of the occurrence of accessory bones.
Python statistical library statsmodels, version 0.8.0, was used for the analysis (Seabold and Perktold, 2010) and the pandas library for data manipulation (McKinney, 2010).
3. RESULTS
We identified 17 true accessory bones in 15 patients (0.77%). The summary of the prevalence of the accessory bones in the examined sample is shown in Table 1, where the number of patients who had at least one accessory bone of the given type is shown. Two patients had more than one accessory bone; thus, the number of patients with bones of a given type does not add up to the number of patients with accessory bones. The location of the accessory bones is shown in Figure 2. Our map of accessory bones shows that os sesamoideum mediale (type IV) was previously described in a significantly more proximal position. The medial epicondyle of the humerus is depicted in its normal form as it was not separated from the rest of the humerus in any of the radiographs. Type VI is slightly smaller and type IV was moved to the place of Wood's type D. We did not find any bone in the place of Wood's type G nor was it found in the available literature.
Table 1.
Prevalence of individual accessory bones type in the examined patients (N = 1940)
| Type | Patients, n (%) |
|---|---|
| I | 0 (0) |
| II | 1 (0.05) |
| III | 4 (0.21) |
| IV | 1 (0.05) |
| V | 9 (0.46) |
| VI | 2 (0.10) |
| Any | 15 (0.77) |
Note that the total number of observed types does not add up to the number of patients with any accessory bone as there was a patient with multiple accessory bones.
The results of the logistic regression, using age and the occurrence of calcar olecrani as independent variables, are shown in Table 2. The reported positive relationship between age and the occurrence of accessory bones was not statistically significant (P = 0.059). The relationship between the occurrence of accessory bones and the occurrence of the calcar olecrani was also found to be non‐significant (P = 0.209). The age distribution of the patients with and without accessory bones is depicted in Figure 3. The distribution of patients with accessory bones and the calcar olecrani is shown in Table 3, while the age distribution of patients with and without accessory bones is shown in Table 4. The results of the statistical analysis of the potential relationship are consistent with our expectations, and thus, we believe that the accessory bones identified were congenital bones and not the result of degenerative changes.
Table 2.
The relationship between the occurrence of accessory bones, age and the occurrence of the calcar olecrani
| Coefficient | SE | P | 95% CI | ||
|---|---|---|---|---|---|
| Age | 0.0318 | 0.017 | 0.059 | −0.001 | 0.065 |
| Calcar olecrani | 0.6932 | 0.551 | 0.209 | −0.388 | 1.774 |
Abbreviation: CI, confidence interval.
Results are from the logistic regression where the independent variables were age and occurrence of the calcar olecrani. The table shows the estimated coefficients and their estimated standard error with a 95% confidence interval. 'Age' denotes the coefficient for the variable describing the patient's age, and 'Calcar olecrani' denotes the coefficient of the variable describing the occurrence of the calcar olecrani. The coefficient β0 is not reported.
Figure 3.
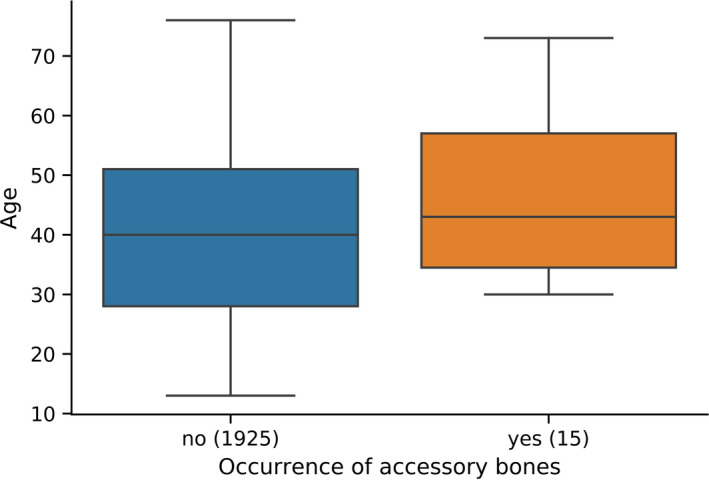
Age of patients vs. occurrence of accessory bones [Colour figure can be viewed at wileyonlinelibrary.com]
Table 3.
Occurrence of accessory bones and calcar olecrani (N = 1940)
| Without accessory bones | With accessory bones | |
|---|---|---|
| With calcar olecrani, n | 379 | 5 |
| Without calcar olecrani, n | 1546 | 10 |
Table 4.
Occurrence of accessory bones in individual age groups
| Age band | With accessory bones, n | Total number of patients |
|---|---|---|
| 21–30 years | 1 | 604 |
| 30–40 years | 5 | 407 |
| 40–50 years | 3 | 430 |
| 50–60 years | 3 | 276 |
| 60–70 years | 1 | 134 |
| 70–80 years | 2 | 89 |
| Total | 15 | 1940 |
4. DISCUSSION
The prevalence of the accessory bones was found to be 0.77%. Our results are consistent with the elbow accessory bone classification published by Wood and Campbell (1994). The occurrence of accessory bones is not statistically significantly tied to the age of patients.
Our results correspond to those observed by Bell (1975) who reported 12% (six cases) of the loose bodies in the elbow as being idiopathic, which could be accessory bones of congenital origin. We identified 12.71% (15 cases) of accessory bones from a total of 118 loose bodies.
Our sample may be biased as it consists of radiographs performed to investigate elbow pathology. Due to the rarity of elbow accessory bones and the gap in the literature on this topic, we believe that a study on an even larger sample would be useful to evaluate the prevalence of all types of the accessory bones and to more precisely evaluate their relationship to patient age.
Wood and Campbell's classification states that Type C and Type E are apophyses that failed to unite with the humerus. In our opinion, this statement is incorrect as no part of the distal humerus was missing in the cases of Type C and E bones that we identified. Therefore, we believe that these two types are sesamoid bones. Computed tomography reports of accessory bones would be helpful to show the exact location of these bones.
We created a modified version of Wood's classification based on our findings (Figure 1). Confusion still exists between Wood's types D and G. No previous study has proven that they should be considered as two separate entities. We decided to fuse those two entities into one category as no difference between them is described in the previous literature. Greek numbers are used in our modified classification to prevent confusion but until the issue of patella cubiti is solved this classification cannot be considered final. We find the term 'os sesamoideum tricipitale' more appropriate than patella cubiti as the latter term should be used to describe the shape made by the articular surface of the patella, which should be used only in cases when the bone is intra‐articular and presents as olecranon separated from the proximal ulna. We propose the term 'os subepicondylare laterale' for Type III, which was also previously referred to as paratrochlear bone (Schwarz, 1957). For types V and VI, we propose the terms 'os subepicondylare mediale' and 'os sesamoideum brachiale', respectively. The term accessory coronoid was also used in the literature for the os sesamoideum brachiale (Schwarz, 1957).
Knowledge of accessory bones is essential when formulating differential diagnoses for elbow pathology. Particular attention should be given to os supratrochleare posterius and os supratrochleare anterius as most of the cases described in the literature caused symptoms such as the limitation of elbow extension and pain and were therefore surgically removed (Wood and Campbell, 1994). Symptoms probably occur due to fracture of accessory bone caused by direct movement of the ulna during forced elbow extension (Obermann and Loose, 1983). Many conditions were reported to be confused with the accessory bones such as avulsion fractures, aseptic necrosis, osteochondritis dissecans, persistent epiphysis, calcific bursitis, synovial chondromatosis and loose bodies owing to the trauma or osteoarthrosis (Bell, 1975; Gudmundsen and Ostensen, 1987). Nevertheless, we did not find any cases except avulsion fractures and degenerative changes that could be misclassified as accessory bones. We were able to differentiate these two pathologies from accessory bones using our criteria outlined in the methods (Figure 4).
Figure 4.

Accessory bone vs. degeneration. The accessory bone (on the left) has typical ovoid shape, smooth margin and cortex ratio. The degenerative elbow (on the right) has typical multiple, quite irregular shape and size calcifications, located around the joint, especially in the epicondylar area
Conflicts of interest
None declared.
Acknowledgements
We thank Miloslav Roček for the kind access to the radiographic images, Jan Šprindrich for consultations and advice, Kateřina Kuncová and Vojtěch Janeček for all the illustrations used in this article, Sheri Doyle and Adam Whitley for language corrections and to all anonymous reviewers for their help with the final version of the manuscript.
This research did not receive any financial support. The data that support the findings of this study are available from the corresponding author on reasonable request.
Vo.K. designed the study, collected the main data and wrote the main part of the manuscript, Vl.K. performed all the statistics, helped with analysis of the collected data and wrote a significant part of the manuscript. V.C collected a significant part of the data, reviewed the manuscript and helped analyze the data. M.P helped analyze all images as well as wrote the radiological part of manuscript and reviewed the whole text. D.K supervised the study, edited the manuscript and helped to design the study.
Kunc V, Kunc V, Černý V, Polovinčák M, Kachlík D. Accessory bones of the elbow: Prevalence, localization and modified classification. J. Anat. 2020;237:618–622. 10.1111/joa.13233
References
- Bell, M.S. (1975) Loose bodies in the elbow. British Journal of Surgery, 62(11), 921–924. 10.1002/bjs.1800621116 [DOI] [PubMed] [Google Scholar]
- Canamero, B. , Ángeles, M. , Giraldo, S. , Alberto, W. , Rivera, G. , Ignacio J., et al (2014) Os supratrochleare dorsale del codo. Acta Rheuma, 10.3823/1304 [DOI] [Google Scholar]
- Gudmundsen, T.E. and Ostensen, H. (1987) Accessory ossicles in the elbow. Acta Orthop Scan, 10.3109/17453678709146457 [DOI] [PubMed] [Google Scholar]
- McKinney W. (2010) Data structures for statistical computing in python. Proc Python Science Conf. [Google Scholar]
- Mittal, R. , Sampath Kumar, V. and Gupta, T. (2014) Patella cubiti: A case report and literature review. Archives of Orthopaedic and Trauma Surgery, 134(4), 467–471. 10.1007/s00402-014-1926-7 [DOI] [PubMed] [Google Scholar]
- Obermann, W.R. and Loose, H.W. (1983) The os supratrochleare dorsale: A normal variant that may cause symptoms. AJR Am J Roentegnol, 141(1), 123–127. 10.2214/ajr.141.1.123 [DOI] [PubMed] [Google Scholar]
- Seabold, S. and Perktold, J. (2010) Statmodels: Econometric and statistical modeling with Python. Proc Python Science Conf. [Google Scholar]
- Schwarz, G.S. (1957) Bilateral antecubital ossicles (fabellae cubiti) and other rare accessory bones of the elbow. Radiology, 69(5), 730–734. 10.1148/69.5.730 [DOI] [PubMed] [Google Scholar]
- Wood, V.E. and Campbell, G.S. (1994) The supratrochleare dorsale accessory ossicle in the elbow. Journal of Shoulder and Elbow Surgery, 3(6), 395–398. 10.1016/S1058-2746(09)80026-8 [DOI] [PubMed] [Google Scholar]


