Abstract
The median artery has been considered as an embryonic structure, which normally regresses around the 8th week of gestation. However, various prevalences have been reported in adults since the 18th century. Furthermore, in a study by Henneberg and George (1995; Am J Phys Anthropol 96, 329–334), has suggested that increasing prevalence of the median artery during the 20th century was a ‘possible secular trend’. The present study, conducted nearly a quarter of a century later, is a continuation of that study. A total of 26 median arteries were found in 78 upper limbs obtained from Australians aged 51 to 101 years, who died in the period 2015–2016, a prevalence rate of 33.3%. Analysis of the literature showed that the presence of the median artery has been significantly increasing (p = .001) over time, from approximately 10% in people born in the mid‐1880s to approximately 30% by the end of the 20th century. The significance of the prevalence increased to a p value <.0001, when the results of the present study and other studies conducted by our research team were combined. After removal of the studies that were possibly biased, because of their specific focus on the evolutionary aspects of the median artery, the significance remained at p = .018. The present study provides an example of microevolutionary changes in the internal anatomy of the human body. Second‐order polynomial regression of the median artery's prevalence on dates of birth shows that it is now present in 35% of people and predicts that people born 80 years from now will all carry a median artery if the trend continues. When the median artery prevalence reaches 50% or more, it should not be considered as a variant, but as a ‘normal’ human structure.
Keywords: anatomical variation, median artery, microevolution, secular trend
Median artery accompanied the median nerve and completed the superficial palmar arch laterally.

1. INTRODUCTION
The median artery of the human forearm has been described as a foetal vessel that supplies the hand and regresses with the development of the radial and ulnar arteries (Jones and Ming, 1988). The regression of the median artery commences at approximately the eighth week of intrauterine life (Aragão et al., 2017). However, the median artery persists in a considerable number of foetuses of gestation ages 13–38 weeks (Aragão et al., 2017), in newborns and infants (Kopuz et al., 1995; George and Henneberg 1996) and in adults (Henneberg and George, 1992a, 1992b; Rodriguez‐Baeza et al., 1995; Kopuz and Gulman 1997; Rodriguez‐Niedenfuhr et al., 1999; Lindley and Kleinert, 2003; D’Costa et al., 2006; Claassen et al., 2008; Natsis et al., 2009; Nayak et al., 2010; Eid et al., 2011).
Two main phenotypes of persistent median artery, palmar and forearm have been described. They supply the forearm and the hand, or the forearm only, respectively. Commencement of the persistent median arteries occurs variably from the common interosseous artery, the anterior interosseous artery, the caudal angle between the common interosseous and ulnar arteries, and the ulnar artery (Rodriguez‐Niedenfuhr et al., 1999; Claassen et al., 2008; Aragão et al., 2017; Cheruiyot et al., 2017). The median artery lies alongside the median nerve on its medial or lateral side (Cheruiyot et al., 2017) in the proximal third of the forearm, and in the distal part it is located between the anterior surface of the median nerve and the deep surface of the flexor digitorum superficialis muscle. The arrangement of the median artery in the proximal part of the forearm varies. The artery runs either anterior or posterior to the anterior interosseous nerve and, in some cases, pierces the median nerve in a posterior to anterior direction or a radial to ulnar direction (Rodriguez‐Niedenfuhr et al., 1999; Claassen et al., 2008; Cheruiyot et al., 2017). Substantial variations in the arrangement of the median artery were seen in the distal third of the forearm. The median artery entered the palm in some cases and completed the superficial palmar arch or directly formed some of the common digital arteries 1–3 (Rodriguez‐Niedenfuhr et al., 1999; Claassen et al., 2008; Cheruiyot et al., 2017). This pattern of median artery arrangement has been referred to as the palmar phenotype of the median artery (Rodriguez‐Niedenfuhr et al., 1999; Cheruiyot et al., 2017). In others, the median artery terminated in the distal forearm and did not reach the wrist. This pattern of median artery arrangement has been referred to as the antebrachial phenotype (Rodriguez‐Niedenfuhr et al., 1999; Cheruiyot et al., 2017).
In the palmar phenotype, the median artery emerges between the tendon of flexor carpi radialis and the tendon of flexor digitorum superficialis to the middle finger, passes through the carpal tunnel deep to the flexor retinaculum and enters the palm (Rodriguez‐Niedenfuhr et al., 1999; Classen et al., 2008). In some cases, the median artery joins the superficial branch of the ulnar artery and forms the superficial palmar arch (Rodriguez‐Niedenfuhr et al., 1999; Claassen et al., 2008; Cheruiyot et al., 2017), while in others, the median artery terminates by forming some of the one to three common digital arteries (Rodriguez‐Niedenfuhr et al., 1999; Cheruiyot et al., 2017). In the antebrachial phenotype, the median artery terminates in the proximal third of the forearm within the median nerve sheath or the distal third of the forearm within the flexor tendon sheath or in the median nerve sheath (Rodriguez‐Niedenfuhr et al., 1999).
The median artery, when present, passes through the carpal tunnel, thus it can compress the median nerve, causing carpal tunnel syndrome (Olave et al., 1997; Natsis et al., 2009). Furthermore, space limitations in the carpal tunnel could cause thrombosis, aneurysm, calcification or traumatic rupture of the artery (Natsis et al., 2009; Potu et al., 2011). In addition, harvesting the ulnar or radial arteries could damage persistent median arteries. This could lead to ischaemia of the hand, if the artery contributes significantly to the blood supply of the hand (Cheruiyot et al., 2017). A persistent median artery is usually considered a disadvantage when complications arise due to its presence. However, in rare instances, it could also be advantageous as it can act as an ‘emergency vessel’ because, if damage to the radial or ulnar arteries occurs, it can still supply blood to the hand (Argawal et al., 2013).
The aim of the present study was to investigate the prevalence of persistent median arteries in postnatal humans over the last 250 years and to test the hypothesis that a secular trend of increase in its prevalence has occurred. The focus of this study was not to analyse the prevalence of the occurrence of the median artery in relation to ethnicity, geographic origin or variations by sex, but to identify the global trends in its occurrence.
2. MATERIALS AND METHODS
2.1. Australian sample
The current sample comprised a total of 78 upper limbs dissected at two different Australian Universities. Upper limbs from 20 whole cadavers (17 females, three males = 40 limbs) were dissected at the University of Adelaide, Medical School by J.K. and M.H. These cadavers were donated to the University of Adelaide for medical teaching and research. The donations were made by members of the local community of Australians of European descent. This satisfied the conditions of the National Health and Medical Research Council (2007) Statement on Ethical Conduct in Human Research (Australian). Thirty‐two embalmed, prosected upper limbs (15 females, 17 males) and prosected upper limbs of three whole cadavers (one female and two male) used for medical teaching at the University of Sydney were observed by T.L. All investigations involving cadavers at the University of Sydney were conducted in accordance with the NSW Anatomy Act, 1977. These cadavers were also donated by Australians of European descent. Thus, a total of 23 whole cadavers (46 upper limbs) and 32 single upper limbs were included in the present study (N = 78).
The mean (range) age of the deceased individuals was 80 (51–101) years, which corresponded to birth decades from the 1910s to 1960s. All upper limbs were studied according to the same criteria. A median artery, exposed by dissection, was considered present if it was a sizeable vessel that supplied blood to the forearm or the hand beyond the median nerve. The present study aimed to investigate the presence or absence of persistent median arteries, not details of their course, size or variation as has been discussed in other studies (Rodriguez‐Niedenfuhr et al., 1999; Bilge et al., 2006; Joshi et al., 2014; Cheruiyot et al., 2017). An example of a median artery from the present study is shown in Fig. 1.
Figure 1.
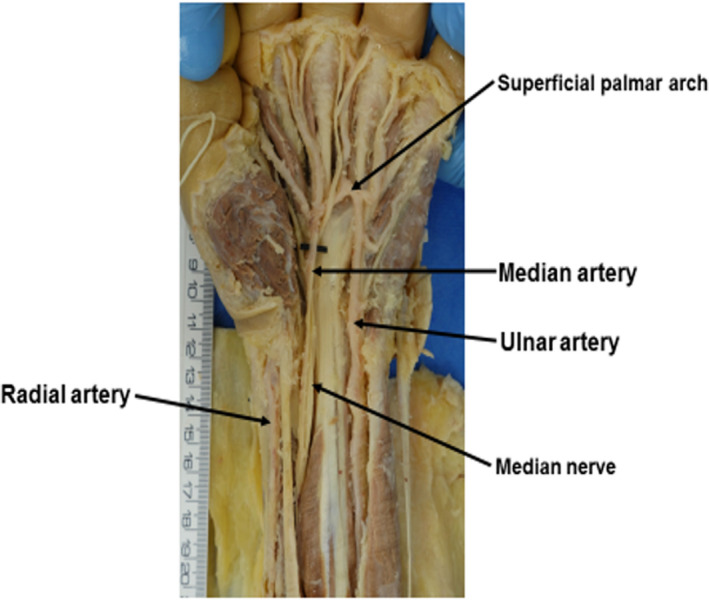
Median artery and superficial palmar arch (anterior dissection of the left lower forearm, wrist and hand) – Median artery accompanied the median nerve and completed the superficial palmar arch laterally. Note, the radial artery did not contributed to the superficial palmar arch [Colour figure can be viewed at wileyonlinelibrary.com]
The prevalence rate of persistent median arteries in the forearms of the present study, together with those published by a number of authors over the last two centuries (Table 2) were analysed. The aim of the analysis was to investigate the secular trend in the occurrence of median arteries in human forearms. Biases towards increasing the prevalence rates of persistent median arteries and the inaccuracies that could occur in the identification of the persistent median arteries were minimized, using the methods described below.
2.1.1. Data sources
A comprehensive literature review was conducted to ensure publications that fitted the inclusion criteria were found. The following search strategies were used: a computer search of the literature and cross referencing of papers cited from relevant articles.
The Google Scholar search for literature using the term ‘persistent median artery’ yielded over 284 000 results in various languages. This search was then limited by refining the search terms based on the inclusion criteria. The following search terms were used in various combinations: persistent median artery; dissection; cadavers; prevalence; secular trend; meta‐analysis; arterial supply of the hand; anatomical variations; and persistent median artery prevalence rate.
In some cases, the original articles could not be sourced after exhaustive literature searches. In these cases, multiple other sources reporting the prevalence rates of the unsourced paper were used. It was a condition that at least two other papers needed to have reported the prevalence rate in order for it to be considered reliable.
2.1.2. Exclusions
Prevalences of median arteries of the forearm that have been reported from patients selected for carpal tunnel syndrome corrections (e.g. Barfred et al., 1985; Lisanti et al., 1995) were excluded; persistent median artery has been suggested to cause pain in carpal tunnel syndrome (Barfred et al., 1985; Lisanti et al., 1995), thus selection of patients for treatment of this condition could have increased the prevalence. The presence of median arteries reported from studies using angiographic techniques was also excluded as angiography produces a different visibility of smaller arteries, which could also lead to bias. Angiographic studies were also excluded because the aim of the present study was to capture a broad timeline of reported cases, and angiographic techniques were developed after the earliest cases included in this study; these cases were therefore excluded to reduce the bias.
2.1.3. Grouping
The available data on prevalence rates of persistent median arteries of the forearm (i.e. other than those excluded) were considered in three sets. In all three sets, if a study reported different prevalences based on the age of participants, the prevalence for each age group was analysed separately, because the sets differed with regard to date of birth which was used to study the time trend (secular trend). This explains why there are more prevalence rates than there are papers which report them. The inclusion criteria for each set were as follows:
Set 1 included prevalences of persistent median arteries of the forearms obtained from the present study and all published articles, except for those excluded above. Set 1 is composed of 62 prevalences.
Set 2 included the prevalences of persistent median arteries of the forearms presented in set 1, after excluding those obtained from foetuses (Aragão et al., 2017), and from studies that were limited only to hands (Tandler, 1896; Jaschtschinski, 1897; Barbosa Sueiro, 1916; Smanio, 1941; Weathersby, 1954; Coleman & Anson 1961; Kenesi et al., 1967; Chalmers, 1978; Braun et al., 1979; Ebner & Hammer 1988; Jelicic 1988; Olave et al., 1997; Gellman et al., 2001; Fazan et al., 2004; Barbe et al., 2005; Loukas et al., 2005; Bilge et al., 2006; Agarwal et al., 2014; Joshi et al., 2014; i.e. the palmar phenotype). The median arteries observed in foetuses have not completed their development, thus they could not be considered as persistent arteries. Furthermore, median arteries in studies limited only to the hands could only show palmar type prevalences. Set 2 was composed of 42 prevalences.
Studies which involved author M.H. (including the present study) could have the potential for bias towards the investigation of a secular trend. Therefore, in the Set 3 analysis, all prevalences of persistent median arteries of forearms obtained from the present study and papers co‐authored by M.H. (Henneberg and George, 1992a, 1992b, 1995; George & Henneberg, 1996) were excluded. This set comprised 45 prevalences obtained from publications.
All analyses were conducted to study the relationship between dates of birth of individuals studied and the prevalence of the median artery to test the hypothesis that the prevalence of this embryonic variant in postnatal life is undergoing microevolution (Henneberg & George, 1995), i.e. an increase in frequency between generations. The birth dates were reconstructed from age of studied cadavers reported by authors of each paper and dates of publication of each paper.
The age at death of participants was not always given in the literature. If publications did not contain information regarding the age of participants or their date of birth, then the estimated average age of cadaveric specimens at the date of published studies was subtracted from the date of publication to arrive at the date of birth.
Regressions of prevalences of the median artery on dates of birth were explored in data selected in the sets. The significance of coefficients of correlation was tested. A chi‐squared test was used to examine whether there were any significant differences in the prevalence of the persistent median artery between sexes, left and right limbs and its occurence either bilaterally or unilaterally (when whole specimens were available). Significance levels of p = .05 or lower were accepted (Fig. 1).
3. RESULTS
In the present sample, when the data were analysed by single limbs (N = 78), statistically significant differences were not observed between males and females (χ2 = 0.570, p = .450) or left and right limbs (χ2 = 0.451, p = .502). When both limbs of the same cadaver were present, statistically significant differences were not observed (χ2 = 0.451, p = .502) between bilateral or unilateral occurrences (N = 23). The frequency of the occurrence of median arteries in each group is presented in Table 1. The data were pooled and analysed as a whole, as there were no statistically significant differences between sexes or lateralities.
Table 1.
Frequency of median artery by, sex and antimere in the sample studied by the authors
| Upper limbs | Sex | Side | Occurrence | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Right | Left | Unilateral | Bilateral | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| With the artery | 18 | 35.3 | 8 | 29.6 | 11 | 29.7 | 15 | 36.6 | 7 | 30.4 | 5 | 21.7 |
| Without the artery | 33 | 64.7 | 19 | 70.4 | 26 | 70.3 | 26 | 63.4 | 16 | 69.6 | 18 | 78.3 |
| Total | 51 | 100.0 | 27 | 100.0 | 37 | 100.0 | 41 | 100.0 | 23 | 100.0 | 23 | 100.0 |
Twenty‐six median arteries were observed in the 78 upper limbs investigated, giving a total prevalence rate of 33.3% per 100 limbs. The prevalence in those born before 1940 (31.5%) was lower than in those born after 1940 (38.1%), but this difference was not significant (χ2 = 0.293, p = .588); however, those born after 1940 showed a greater prevalence (Table 1).
The prevalence calculated from the present study was compared with those in the published literature (Table 2). Data reported in the total of 47 published papers, as well as the findings from the present study were included in the Set 1 analysis. A total of 62 separate prevalences were reported, when age cohorts were considered separately. The range of prevalence in the first set was 0%–81.2%, while the calculated year of birth ranged from 1846 to 1997. There was a significant increase (p < .0001) in the prevalences of median arteries of forearms on average during this time from approximately 10% in 1846 to over 30% in 1997 (Fig. 2).
Table 2.
Prevalences of the median artery by direct anatomical observations reported in publications
| Author (year) | Prevalence, % |
|---|---|
| Adachi (1928) | 8.00 |
| Agarwal et al. (2014) | 11.53 a |
| Aragão et al. (2017) | 81.25 b |
| Aung & Than (2009) | 60.00 |
| Barbe et al. (2005) | 2.50 a |
| Barbosa Sueiro (1916) | 12.00 a |
| Bilge et al. (2006) | 8.00 a |
| Braun et al. (1979) | 8.00 a |
| Chalmers (1978) | 4.39 a |
| Cheruiyot et al. (2017) | 59.68 |
| Claassen et al. (2008) | 7.40 |
| Coleman & Anson (1961) | 9.90 a |
| D’Costa et al. (2006) | 15.80 |
| Ebner & Hammer (1988) | 5.4 a |
| Eid et al. (2011) | 4.00 |
| Fazan et al. (2004) | 11.00 a |
| Gellman et al. (2001) | 15.56 a |
| George and Henneberg 1996 | 44.20 c |
| Gray (1945) | 1.10 |
| Henneberg & George (1992a) | 27.10 c |
| Henneberg & George (1992b) | 27.40 c |
| Henneberg & George (1995) | 31.60 c |
| Jaschtschinski (1897) | 12.00 a |
| Jaschtschinski (1897) | 3.96 a |
| Jelicic et al. (1988) | 2.00 a |
| Joshi et al. (2014) | 4.00 a |
| Keen (1961) | 9.50 |
| Kenesi et al. (1967) | 3.00 a |
| Kodama (2000) | 8.2 |
| Kopuz et al. (1995) | 12.50 |
| Kopuz et al. (1995) | 0.00 |
| Kopuz & Gulman (1997) | 20.00 |
| Libersa et al. (1982) | 16.00 |
| Loukas et al. (2005) | 21.10 a |
| Lucas et al. 2020 (current study) | 33.33 c |
| Mansor et al. (1999) | 31.82 c |
| McCormack et al. (1953) | 4.43 |
| Misra (1955) | 8.33 |
| Natsis et al. (2009) | 2.78 |
| Nayak et al. (2010) | 15.40 |
| Olave et al. (1997) | 23.00 a |
| Patnaik & Paul (2016) | 6.00 |
| Pecket et al. (1973) | 30.00 |
| Potu et al. (2011) | 8.00 |
| Rodriguez‐Niedenführ et al. (1999) | 12.00 |
| Rodriguez‐Baeza et al. (1995) | 3.44 |
| Singla et al. (2012) | 6.67 |
| Smanio (1941) | 20.00 a |
| Srivastava & Pande (1990) | 1.50 |
| Tandler (1896) | 16.88 a |
| Weathersby (1954) | 10.00 a |
Where the same author is referenced twice, the data were split into two distinct groups, such as children and adults; the prevalence for children is presented first. For additional information regarding the samples of these studies, please refer to the original publications.
Studies that only used the hand or carpal tunnel to describe the prevalence of the median artery.
Data that were only collected on foetuses.
Studies that involved M.H.
Figure 2.

Prevalence of the median artery over time (year of birth), set 1 (N = 62)
In the analysis of Set 2, 19 published papers were removed (data indicated by superscript 'a' in Table 2) because they only contained data on one type of median artery (palmar phenotype). Additionally one study was removed because it was conducted on foetuses alone (indicated by superscript 'b' in Table 2). A total of 42 separate prevalences were included in the Set 2 analysis, after age cohorts were separated (Fig. 3). The range of prevalence was 0%–60%, while the calculated year of birth ranged from 1878 to 1997. Despite a large number of papers being removed, the prevalences of the median arteries continued to increase over time, from approximately 10% in 1878 to 30% in 1997, as in the previous analysis, and the increase was significant (p = .018).
Figure 3.

Prevalence of the median artery over time (year of birth), set 2 (N = 42)
A total of 43 separate studies were included in Set 3, with a total of 45 separate prevalences after age cohorts were reported separately (Fig. 4). All studies that involved M.H., including present study were removed (data indicated by superscript 'c' in Table 2), because of the potential for corroborative reasoning to lead to bias. The prevalences ranged from 0% to 81.2%, while the calculated year of birth ranged from 1846 to 1997, which was the same as in Set 2, respectively. Many of the papers that involved M.H. reported birth cohorts separately, which increased the sample size for the analysis of Set 1 (N = 62 separate prevalences). In spite of the decrease in sample size, by almost one‐third (i.e.17 prevalences), the secular trend for the presence of the median arteries in the forearms still significantly increased over time (p = .001), from approximately 10% in 1846 to 30% in 1997. This was similar to findings in previous analyses.
Figure 4.

Prevalence of the median artery over time (year of birth), set 3 (N = 45)
4. DISCUSSION
The findings of the present study indicate that the prevalence of the persistent median artery in postnatal life approximately tripled over the last 125 years (Fig. 2). The significance and the validity of this finding was robustly tested by eliminating biases that could have influenced the analyses. The data from research co‐authored by M.H. were removed from one analysis (Set 3) to eliminate the bias towards a secular trend, and the significance of the trend of increase remained at p = .001, while the increase remained from approximately 10% to 30% during the period of observation (Fig. 4). The significance of the secular trend of prevalences of persistent median arteries in the forearms increasing by tenfold was robust (p < .0001) when the results of the present study and those published by M.H. and his co‐authors were pooled (Fig. 2). Furthermore, when the data from studies that only reported median arteries in foetuses or in hands which could have increased the biases towards a secular trend were removed, the significance remained at p = .018 (Fig. 3). The findings of the present study are therefore valid.
The prevalences of the persistent median arteries in forearms could vary among people according to the geographical location of the population studied. Prevalences have varied between 1.5% and 60% (Aung and Than, 2009; Natsis et al., 2009; Cheruiyot et al., 2017). The present study used an Australian sample of European origin. These results were comparable to those reported in black South Africans, their white counterparts and Malaysians of similar birth years; all these groups had a prevalence of approximately 30% (Henneberg and George, 1992a, 1992b; George and Henneberg, 1996; Mansoor et al., 1999) These findings where consistent data collection methods were used, did not show differences between groups based on geographic or ethnic origin. Therefore, it is likely that different prevalences reported for coeval samples from different geographic locations may be a result of differences in research methods.
The reduction in prevalences of persistence of median arteries from 81.3% in foetuses (gestation age of 13–38 weeks; Aragão et al., 2017) to 44.2% in neonates (George & Henneberg, 1996) may indicate that the process of regression of the median artery continues from the 8th week of gestation to the end of the neonatal period. Aragão et al. (2017) are in agreement with this view. The mechanism for the regression of the median artery is initiated and regulated by specific genes. Persistence of the median artery into adulthood indicates the failure of the expression of these genes. Increasing the prevalence over the last 125 years means a true evolutionary process of the change in gene pools. Retention of the palmar type phenotypes of the median artery may be the result of the failure of the regression process to commence. This could have resulted from alteration of or damage to genes by mutations. Alternatively, the mother could have been subjected to an environmental insult such as an infection before the initiation of the regression process. This could have stopped the commencement of the regression process of the median artery. Furthermore, as suggested by Rodriguez‐Niedenfuhr et al. (1999), the regression process of the median artery could progress from the palm towards the elbow. Thus, a health insult (e.g. an infection) to the mother or the neonate during the process, could stop the regression leaving the forearm type phenotype of the median artery. Prevalences of 76% and 73% of the forearm type phenotype compared to 20% and 27% of the palmar type phenotype in the adults (Rodriguez‐Niedenfuhr et al., 1999) and foetuses (Aragão et al., 2017), respectively, may favour the health insult theory. The reason for the acceptance of the health insult theory is that the chances of the mother or the neonate facing an infection are greater than those of genes undergoing mutations to generate two separate phenotypes, unless gene expressions vary among individuals. Healthcare for pregnant women has improved globally over the last 125 years, thus the trend for the occurrence of persistent median arteries in forearms of adults for maternal health reasons should reduce, not increase as seen in the present study. The observed increase therefore in the prevalence of persistent median arteries in adult forearms of people in many countries may be a trend associated with the evolutionary process.
Similar to the increase in the prevalence of persistent median arteries of the forearms, the prevalence of other anatomical features such as spina bifida occulta (Henneberg & Henneberg 1999; Solomon et al., 2009; Lee et al., 2010), tarsal coalitions (Solomon et al., 2003) and fabella (Berthaume et al., 2019) has increased over the last 2–3 centuries. Evidence indicates that changes in the natural selection pressures acting on these specific anatomical features could have caused microevolutionary processes, leading to the observed increases in prevalence rates (Henneberg and Henneberg 1999; Solomon et al., 2009; Lee et al., 2010; Rühli and Henneberg, 2013; Berthaume et al., 2019).
In the sample collected by the authors of the present study, the prevalence of the persistence of the median artery in the forearms of people born before 1940 was not significantly different from that of people born after 1940. However, the 38.1% prevalence of the persistent median artery in forearms of people born after 1940 was comparable to that reported by Henneberg and George (1995) for the same period. The small size of the sample could be the reason for the lack of significance, but in these days of dwindling studies of cadavers it is difficult to obtain observations on large sample size.
The tripling in the prevalence of the median artery over the last 150‐year period of investigation (p < .0001; Fig. 2), if extrapolated using the same regression line, could predict that the median artery will be present in 100% of individuals born in the year 2100 and later. That is approximately 250 years from the beginning of the artery's first reported incidence as a ‘variant’. This prediction to become true, the mutation/natural selection pressures that caused the microevolution over the last 150 years (i.e. from 1846 to 1997), should continue to act on humans at least for the next 103 years (i.e. from 1997 to 2100). It is unlikely that such a continuation will occur without modifications. However, it is likely that increases in the prevalence of persistent median arteries of the forearm will continue. When this prevalence rate reaches 50% or more (Kumaratilake and Saniotis, 2018), persistent median arteries of the forearms will be considered as normal structures of the forearm and the hand. The question to ask is whether the mutation/natural selection pressures acted in causing the trend that occurred during the 150 years of this study or whether the health insults to the mother and the foetus were changing during this period, or both.
Limitations of the present study include the fact that the number of whole cadavers that were available for the study was not adequate. In addition, our search of the literature may have missed some publications not listed in Google Scholar. Finally, the definitions of 'persistent median artery' may have differed somewhat among the various published studies included in the present study.
Conflicts of interest
None declared.
Author contributions
All authors contributed equally to this research. M.H. and J.K. collected the data from the University of Adelaide. T.L. collected the data from Sydney University. T.L. collected the literature data for the analyses. All authors analysed the data. T.L. wrote the original draft and M.H. and J.K. edited all drafts.
Acknowledgements
The authors would like to thank Miss Laura O'Loughlin for her input in the pilot study for this research. The authors would also like to thank Mr Marcus Robinson of the University of Sydney for access to prosected specimens, Dr Arthur Saniotis for assistance with dissections and variation recordings and Mr Tavik Morgenstern for photographing all specimens.
Lucas T, Kumaratilake J, Henneberg M. Recently increased prevalence of the human median artery of the forearm: A microevolutionary change. J. Anat. 2020;237:623–631. 10.1111/joa.13224
REFERENCES
- Adachi, B. (1928) Das Arteriensystem der Japaner. Kyoto, Japan: Maruzen, 1, 285–356. [Google Scholar]
- Agarwal, K.K. , Saxena, A. , Soni, S. and Das, A.R. (2013) Persistent median artery: A sign of primitive arterial pattern. OA Case Reports, 15, 128. [Google Scholar]
- Agarwal, P. , Gupta, S. , Yadav, P. and Sharma, D. (2014) Cadaveric study of anatomical variations of the median nerve and persistent median artery at the wrist. Indian Journal of Plastic Surgery, 47, 95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aragão, J.A. , da Silva, A.C. , Anunciação, C.B. and Reis, F.P. (2017) Median artery of the forearm in human foetuses in northeastern Brazil: anatomical study and review of the literature. Anatomical Science International, 92, 107–111. [DOI] [PubMed] [Google Scholar]
- Aung, H.H. and Than, T.A.M. (2009) Incidence of persistent median artery of the forearm in Myanmar adults. Acta Anatomica Nippon, 84, 202. [Google Scholar]
- Barbe, M. , Bradfield, J. , Donathan, M. and Elmaleh, J.E.D. (2005) Coexistence of multiple anomalies in the carpal tunnel. Clinical Anatomy, 18, 251–259. [DOI] [PubMed] [Google Scholar]
- Barbosa Sueiro, M.B. (1916) Arcadas arteriais palmares. Archives of Anatomy and Anthropology, 2, 389–414. [Google Scholar]
- Barfred, T. , Højlund, A.P. and Bertheussen, K. (1985) Median artery in carpal tunnel syndrome. The Journal of Hand Surgery, 10, 864–867. [DOI] [PubMed] [Google Scholar]
- Berthaume, M.A. , Federico, E.D. and Bull, A.M.J. (2019) Fabella prevalence rate increases over 150 years, and rates of other sesamoid bones remain constant: a systematic review. Journal of Anatomy, 235, 67–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilge, O. , Pinar, Y. , Özer, M. and Govsa, F. (2006) A morphometric study on the superficial palmer arch of the hand. Surgical and Radiologic Anatomy, 28, 343–350. [DOI] [PubMed] [Google Scholar]
- Braun, J.B. , Werner, J.E. , Borrelly, J. , Foucher, G. , Merle, M. and Michon, J. (1979) Quelques notions d’anatomie artérielle de la main et leurs applications chirurgicales. Annales de Chirurgie, 33, 701–706. [PubMed] [Google Scholar]
- Chalmers, J. (1978) Unusual cases of peripheral nerve compression. The Hand, 10, 168–175. [DOI] [PubMed] [Google Scholar]
- Cheruiyot, I. , Bundi, B. , Munguti, J. , Olabu, B. , Ngure, B. and Ogeng’o, J. (2017) Prevalence and anatomical patterns of the median artery among adult black Kenyans. Anatomy Journal of Africa, 6, 1015–1023. [Google Scholar]
- Claassen, H. , Schmitt, O. and Wree, A. (2008) Large patent median arteries and their relation to the superficial palmer arch with respect to history, size consideration and clinic consequences. Surgical and Radiologic Anatomy, 30, 57–63. [DOI] [PubMed] [Google Scholar]
- Coleman, S.S. and Anson, B.J. (1961) Arterial patterns in the hand based upon a study of 650 specimens. Surgery, Gynecology & Obstetrics, 113, 409–424. [PubMed] [Google Scholar]
- D’Costa, S. , Narayana, K. , Narayan, P. , Nayak, S.R. and Madhan, S.J. (2006) Occurrence and fate of palmar type of median artery. ANZ Journal of Surgery, 76, 484–487. [DOI] [PubMed] [Google Scholar]
- Ebner, I. and Hammer, H. (1988) Aspekte der arteriellen Gefässbezie‐hungen im Hohlhandbereich. Acta Anatomica, 131, 297–304. [PubMed] [Google Scholar]
- Eid, N. , Ito, Y. , Shibata, M.A. and Otsuki, Y. (2011) Persistent median artery cadaveric study and review of the literature. Clinical Anatomy, 24, 627–633. [DOI] [PubMed] [Google Scholar]
- Fazan, V.P. , Borges, C.T. , Da Silva, J.H. , Caetano, A.G. and Filho, O.A. (2004) Superficial palmer arch: an arterial diameter study. Journal of Anatomy, 204, 307–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gellman, H. , Botte, M.J. , Shankwiler, J. and Gelberman, R.H. (2001) Arterial patterns of the deep and superficial palmer arches. Clinical Orthopaedics and Related Research, 383, 41–46. [DOI] [PubMed] [Google Scholar]
- George, B.J. and Henneberg, M. (1996) High frequency of the median artery of the forearm in South African newborns and infants. South African Medical Journal, 86, 175–176. [PubMed] [Google Scholar]
- Gray, D.J. (1945) Some variations appearing in the dissecting room. Stanford Medical Bulletin, 3, 120–127. [Google Scholar]
- Henneberg, M. and George, B.J. (1992a) High incidence of the median artery of the forearm in a sample of recent south African Cadavers. Journal of Anatomy, 180, 185–188. [PMC free article] [PubMed] [Google Scholar]
- Henneberg, M. and George, B.J. (1992b) A further study of the high incidence of the median artery of the forearm in S Afr . Journal of Anatomy, 181, 151–154. [PMC free article] [PubMed] [Google Scholar]
- Henneberg, M. and George, B.J. (1995) Possible secular trend in the incidence of an anatomical variant: Median artery of the forearm. American Journal of Physical Anthropology, 96, 329–334. [DOI] [PubMed] [Google Scholar]
- Henneberg, R.J. and Henneberg, M. (1999) Variation in the closure of the sacral canal in the skeletal sample from Pompeii, Italy, 79 AD. Perspective Human Biology, 4, 177–188. [Google Scholar]
- Jaschtschinski, S.N. (1897) Morphologie und topographie des arcus volaris sublimis und profundus. Anatomische Hefte, 7, 163–188. [Google Scholar]
- Jelicic, N. , Gajicin, S. and Zbrodowski, A. (1988) Arcus palmaris superficialis. Acta Anatomica, 132, 187–190. [PubMed] [Google Scholar]
- Jones, N.F. and Ming, N.L. (1988) Persistent Median Artery as a cause of pronator syndrome. The Journal of Hand Surgery, 13, 728–732. [DOI] [PubMed] [Google Scholar]
- Joshi, S.B. , Vatsalaswamy, P. and Bahetee, B.H. (2014) Variation in formation of superficial palmar arches with clinical implications. Journal of Clinical and Diagnostic Research, 8, 6–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keen, J.A. (1961) A study of the arterial variations in the limbs, with special reference to symmetry of vascular patterns. The American Journal of Anatomy, 108, 245–261. [DOI] [PubMed] [Google Scholar]
- Kenesi, C. , Alexandre, J.H. and Aaron, C. (1967) Les arteres de la main. Archives D'anatomie et de Cytologie Pathologiques, 15, 99–102. [PubMed] [Google Scholar]
- Kodama, K. (2000) Arteries of the upper limb Sato T. and Akita K. (Ed). Tokyo, Japan: University of Tokyo Press, 220–237. [Google Scholar]
- Kopuz, C. , Gulman, B. and Baris, S. (1995) Persistent median artery: an anatomical study in neonatal and adult cadavers. Acta Anatomica Nippon, 70, 577–580. [PubMed] [Google Scholar]
- Kopuz, C. and Gulman, B. (1997) A further morphological study of the persistent median artery in neonatal cadavers. Surgical and Radiologic Anatomy, 19, 403–406. [DOI] [PubMed] [Google Scholar]
- Kumaratilake, J.S. and Saniotis, A. (2018) Integral segmental bi‐lateral renal arteries and unilateral renal veins in a cadaver: A new classification. International Journal of Anatomical Variations, 11, 26–31. [Google Scholar]
- Lee, Y.C. , Solomon, L.B. , Rühli, F.J. , Schiess, R. , Öhrström, L. , Sullivan, T. , Alkadhi, H. and Henneberg, M. (2010) Confirmation of microevolutionary increase in spina bifida occulta among Swiss birth cohorts. European Spine Journal, 20, 776–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libersa, C.I. , Francke, J.P. and Mauppin, J.M. (1982) The arterial supply to the palm of the hand (arteriae palmae manus). Anatomia Clinica, 4, 33–45. [Google Scholar]
- Lindley, S.G. and Kleinert, J.M. (2003) Prevalence of anatomic variations encountered in elective carpal tunnel release . The Journal of Hand Surgery, 28, 849–855. [DOI] [PubMed] [Google Scholar]
- Lisanti, M. , Rosati, M. and Pardi, A. (1995). Persistent median artery in carpal tunnel syndrome. Acta Orthopaedica Belgica, 61, 315–318. [PubMed] [Google Scholar]
- Loukas, M. , Holdman, D. and Holdman, S. (2005) Anatomical variations of the superficial and deep palmar arches. Folia Morphologiica, 64, 78–83. [PubMed] [Google Scholar]
- Mansor, O. , Kassim, Z. and Henneberg, M. (1999) The incidence of the median artery in the forearms of Malaysians. Perspective Human Biology, 4, 223–228. [Google Scholar]
- McCormack, T.J. , Cauldwel, E.W. and Anson, B.J. (1953) Brachial and antebrachial arterial patterns. Surgery, Gynecology & Obstetrics, 96, 43–54. [PubMed] [Google Scholar]
- Misra, B.D. (1955) The arteria mediana. Journal of the Anatomical Society of India, 4, 48. [Google Scholar]
- National Health and Medical Research Council . (2007). The National Statement on Ethical Conduct in Human Research. http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/e72.pdf [Google Scholar]
- Natsis, K. , Iordache, G. , Gigis, I. , Kyriazidou, A. , Lazaridis, N. , Noussios, G. and Paraskevas, G. (2009) Persistent median artery in the carpal tunnel: Anatomy, embryology, clinical significance, and review of the literature. Folia Morphologiica, 68, 193–200. [PubMed] [Google Scholar]
- Nayak, S.R. , Krishnamurthy, A. , Kumar, S.M. , Prabhu, L.V. , Potu, B.K. , D'Costa, S. and Ranade, A.V. (2010) Palmar type of median artery as a source of superficial palmar arch: A cadaveric study with its clinical significance. Hand (New York, N.Y.), 5, 31–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olave, E. , Prates, J.C. , Gabrielli, C. and Pardi, P. (1997) Median artery and superficial palmar branch of the radial artery in the carpal tunnel. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery, 31, 13–16. [DOI] [PubMed] [Google Scholar]
- Patnaik, M. and Paul, S. (2016) Persistent median artery of the forearm and palm: A cadaver study into its origin, course, fate and clinical significance. Italian Journal of Anatomy and Embryology, 121, 88–95. [PubMed] [Google Scholar]
- Pecket, P. , Gloobe, H. and Nathan, H. (1973) Variations in the arteries of the median nerve with special consideration on the ischemic factor in the carpal tunnel syndrome (CTS). Clinical Orthopaedics and Related Research, 97, 144–147. [PubMed] [Google Scholar]
- Potu, B.K. , Ray, B. , Pai, S.R. , Bhat, K.M. , Pulakunta, T. , Sarda, R. and Mishra, S. (2011) A Preliminary survey of the median artery in human cadavers of South Indian Origin. Bratislava Medical Journal, 112, 292–295. [PubMed] [Google Scholar]
- Rodriguez‐Niedenführ, M. , Sanudo, J.R. , Vázquez, T. , Nearn, L. , Logan, B. and Parkin, I. (1999) Median artery revisited. Journal of Anatomy, 195, 57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez‐Baeza, A. , Nebot, J. , Ferreira, B. , Reina, F. , Pérez, J. , Sañudo, J.R. and Roig, M. (1995) An anatomical study and ontogenic explanation of 23 cases with variations in the main pattern of the human brachio‐antebrachial arteries. Journal of Anatomy, 187, 73–479. [PMC free article] [PubMed] [Google Scholar]
- Rühli, F.J. and Henneberg, M. (2013) New perspectives on evolutionary medicine: The relevance of microevolution for human health and disease. BMC Medicine, 11, 115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla, R.K. , Kaur, N. and Dhiraj, G.S. (2012) Prevalence of the persistent median artery. Journal of Clinical and Diagnostic Research, 6, 1454–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smanio, T. (1941) Observacoes sobre a constituiqlo e a topografia da arcada arterial palmar superficial em negros brasileiros. Folia Clinica et Biologica, 3, 83–91. [Google Scholar]
- Solomon, L.B. , Rühli, F. and Lee, Y.C. (2009) Secular trend in the opening of the sacral canal: An Australian Study. Spine, 34, 244–248. [DOI] [PubMed] [Google Scholar]
- Solomon, L.B. , Rühli, F.J. , Taylor, J. , Ferris, L. , Pope, R. and Henneberg, M. (2003) A dissection and computer tomograph study of tarsal coalitions in 100 cadaver feet. Journal of Orthopaedic Research, 21, 352–358. [DOI] [PubMed] [Google Scholar]
- Srivastava, S.K. and Pande, B.S. (1990) Anomalous pattern of median artery in the forearm of Indians. Acta Anatomica, 138, 193–194. [DOI] [PubMed] [Google Scholar]
- Tandler, J. (1896) Zur Anatomie der Arterien der Hand. Anatomische Hefte, 7, 263–282. [Google Scholar]
- Weathersby, H.T. (1954) The volar arterial arches. Anatomical Record, 118, 365–366. [Google Scholar]


