Key Points
Question
Do adverse pregnancy outcomes represent independent risk factors for atherosclerotic cardiovascular disease in women?
Findings
In this cohort study including 46 805 Women’s Health Initiative participants, hypertensive disorders of pregnancy and low birth weight were independently associated with atherosclerotic cardiovascular disease after adjustment for standard risk factors and other adverse pregnancy outcomes.
Meaning
Adverse pregnancy outcomes are sex-specific risk factors for atherosclerotic cardiovascular disease in women.
This study evaluates whether adverse pregnancy outcomes are associated with increased atherosclerotic cardiovascular disease risk independently of traditional risk factors.
Abstract
Importance
Atherosclerotic cardiovascular disease (ASCVD) may have unique risk factors in women. Most women have a history of pregnancy; common adverse pregnancy outcomes (APOs) appear to be associated with ASCVD, but prior studies have limitations.
Objective
To assess whether APOs are associated with increased ASCVD risk independently of traditional risk factors.
Design, Setting, and Participants
The APO history among participants in the Women’s Health Initiative, a large multiethnic cohort of postmenopausal women, was assessed. The associations of 5 self-reported APOs (gestational diabetes, hypertensive disorders of pregnancy, low birth weight [ie, birth weight less than 2.49 kg], high birth weight [ie, birth weight greater than 4.08 kg], and preterm delivery by 3 weeks or more) with ASCVD were analyzed, adjusting for traditional ASCVD risk factors. Data were collected and analyzed in 2017.
Exposures
APOs (gestational diabetes, hypertensive disorders of pregnancy, low birth weight, high birth weight, and preterm delivery).
Main Outcomes and Measures
Adjudicated ASCVD.
Results
A total of 48 113 Women’s Health Initiative participants responded to the survey; the median (interquartile range) age at time of enrollment was 60.0 (55.0-64.0) years. A total of 13 482 participants (28.8%) reported 1 or more APOs. Atherosclerotic cardiovascular disease was more frequent in women who reported an APO compared with those without APOs (1028 of 13 482 [7.6%] vs 1758 of 30 522 [5.8%]). Each APO, analyzed separately, was significantly associated with ASCVD, and gestational diabetes, hypertensive disorders of pregnancy, low birth weight, and preterm delivery remained significant after adjustment for traditional ASCVD risk factors. When all APOs were analyzed together, hypertensive disorders of pregnancy (odds ratio, 1.27; 95% CI, 1.15-1.40) and low birth weight (odds ratio, 1.12; 95% CI, 1.00-1.26) remained independently associated with ASCVD. All findings were materially unchanged by additional adjustment for parity, body mass index, and socioeconomic factors.
Conclusions and Relevance
In this large multiethnic cohort of women, hypertensive disorders of pregnancy and low birth weight were independently associated with ASCVD after adjustment for risk factors and other APOs.
Introduction
Cardiovascular disease is the leading cause of death among women in the US,1 and identification of sex-specific risk factors could enhance cardiovascular risk assessment and prevention. Pregnancy is an exposure unique to women: 85% of women give birth at least once in their lives, and up to 30% may experience an adverse pregnancy outcome (APO).2,3 The associations of APOs, such as gestational diabetes, hypertensive disorders of pregnancy, preterm delivery, and low birth weight, with atherosclerotic cardiovascular disease (ASCVD) later in life have only recently been examined.
Gestational diabetes, hypertensive disorders of pregnancy, preterm delivery, and low birth weight have each been associated with subsequent development of ASCVD risk factors as well as with an increased incidence of clinically apparent ASCVD.2,4,5,6,7,8,9,10,11,12 Consequently, the American Heart Association recommends that taking a history of APOs be part of ASCVD risk evaluation,13 and the 2018 cholesterol treatment guidelines suggest that hypertensive disorders of pregnancy, preeclampsia, gestational diabetes, small-for-gestational-age infants, and preterm deliveries be considered risk enhancers when discussing initiation of statins for primary prevention of ASCVD in women.14 The European Society of Cardiology 2016 guidelines on cardiovascular disease prevention state that it is not clear whether APOs represent risk factors themselves or if they predispose women by their association with other ASCVD risk factors.15
The associations between APOs (including hypertensive disorders of pregnancy, gestational diabetes, small-for-gestational-age infants, and preterm deliveries) and ASCVD risk are supported by several lines of evidence, yet there are limitations and gaps in this evidence. For example, most prior studies of these APOs have not adjusted for all established ASCVD risk factors, many were not prospective or lacked long-term follow-up, and few have been conducted in multiethnic cohorts. Furthermore, most studies have only examined the association of a single APO with ASCVD risk, even though several APOs may occur in the same woman. We sought to overcome several of these limitations by examining data from the Women’s Health Initiative (WHI), a large multiethnic cohort study with rigorous, prospective follow-up and adjudicated ASCVD outcomes.
Methods
Study Population
The WHI is a longitudinal cohort study, consisting of 3 randomized clinical trials (of hormone therapy, dietary changes, and calcium/vitamin D supplementation) and an observational study.16 Women were enrolled between 1994 and 1998 and have been followed up prospectively.17 At entry, WHI participants were aged 50 to 79 years, postmenopausal, and represented ethnically diverse populations.17 Race and ethnicity were self-reported by the participants. Extensive baseline data were collected at an in-person visit, including the participant’s reproductive history, but no data on APOs were collected at study entry.17 This study was approved by the University of California, San Francisco, institutional review board, and all participants gave written informed consent to participate in WHI and its extension study.
APO Questionnaire
In 2017, a questionnaire surveyed participants’ history of APOs (in 1 or more pregnancies) and asked about their dental health, memory, and changes in mental functioning (eAppendix in the Supplement). The survey was sent to all surviving WHI enrollees who were still participating in the study and included 6 questions on APOs during any pregnancy, with possible responses of no, yes, and don’t know. The APOs surveyed were gestational diabetes, gestational hypertension, preeclampsia, low birth weight (ie, birth weight less than 2.49 kg), high birth weight (ie, birth weight greater than 4.08 kg), and preterm delivery by 3 weeks or more (preterm delivery). More than 1 APO may have occurred in the same woman but not necessarily during the same pregnancy.
Outcomes
The primary study outcome was ASCVD, defined as either myocardial infarction, stroke, peripheral artery disease, or coronary revascularization. These outcomes were prospectively ascertained between study entry and the time of the 2017 survey and were adjudicated using standard criteria.18
Covariates
We analyzed baseline characteristics from the data collected at enrollment into the WHI. The ASCVD risk factors included hyperlipidemia (defined as use of cholesterol-lowering drugs), hypertension (including use of antihypertensive drugs), diabetes (not pregnancy related and self-reported), and smoking status. Data on income, highest education level attained, and self-reported ethnicity were also recorded at study entry.
Statistical Analyses
Women were eligible for this study if they had a history of pregnancy that lasted for more than 6 months and were alive and still participating in the WHI in 2017 when the survey was performed. Women were excluded if, at baseline, they reported previous stroke, myocardial infarction, or coronary revascularization procedure. Nonresponders were defined as eligible WHI participants who did not answer the survey.
We assessed differences between responders and nonresponders using counts and percentages for categorical variables and medians and interquartile ranges for continuous variables. We also compared the characteristics of women who reported an APO with those who did not, by counts and percentages for categorical variables and medians and interquartile ranges for continuous variables. In the primary analysis, we used multinomial logistic regression to assess the association between each APO and ASCVD; in this model, each APO was coded using 3 categories (yes, no, or don’t know), and the responses yes and don’t know were compared with the reference category (no) for their association with ASCVD. In secondary analyses, we tested whether results were changed by using 2 alternative model specifications, in which the don’t know responses were (1) treated as missing (ie, omitted from the model) and (2) combined with the yes responses. For simplicity, we present the results of the primary analysis in the main article and the results of the 2 sensitivity analyses in the eAppendix in the Supplement because the findings were similar.
For each APO, we first used a univariate model and then adjusted for the traditional ASCVD risk factors (age, hyperlipidemia, hypertension, diabetes, and smoking). Finally, we assessed the joint associations of each APO with ASCVD in a multivariable model that simultaneously adjusted for all APOs and risk factors. We tested each model for interaction by race/ethnicity. A 2-sided P value less than .05 was considered statistically significant.
All statistical analyses were conducted using RStudio 1.1.456 by RStudio (R version 3.5.1; The R Foundation). Data retrieval was done using SAS Enterprise version 9.4 (SAS Institute).
Results
Survey Responders
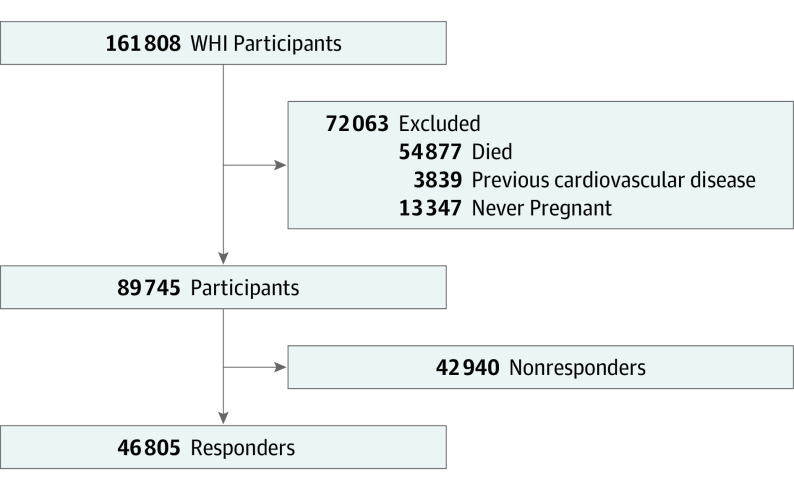
Of the 161 808 women enrolled in the WHI, 71 661 were still being followed up in 2017 and were mailed a survey about APOs. A total of 46 805 eligible study participants (65.3%) responded and answered questions on APOs (Figure 1). The median (interquartile range) age at the time of enrollment was 60 (55.0-64.0) years. Responders were younger and had less hypertension, diabetes, and hyperlipidemia than eligible nonresponders (Table 1). Responders were also more likely than nonresponders to be White, college educated, and have higher incomes (Table 1). Atherosclerotic cardiovascular disease was more frequent in women who reported an APO compared with those without APOs (1028 of 13, 482 [7.6%] vs 1758 of 30, 522 [5.8%]).
Figure 1. Flow Diagram for the Selection of the Study Participants From the Women’s Health Initiative (WHI).
Table 1. Baseline Characteristics of Survey Responders and Nonresponders.
| Variable | No. (%) | P value | ||
|---|---|---|---|---|
| Nonresponders (n = 42 940) | Responders (n = 46 805) | Total (N = 89 745) | ||
| Age at enrollment, median (IQR), y | 62.0 (56.0-67.0) | 60.0 (55.0-64.0) | 61.0 (56.0-66.0) | <.001 |
| Hypertension | 13 625 (31.9) | 11 537 (24.7) | 25 162 (28.2) | <.001 |
| Diabetes | 2144 (5.0) | 1186 (2.5) | 3330 (3.7) | <.001 |
| Smoking | 19 966 (46.9) | 22 124 (47.5) | 42 090 (47.2) | .06 |
| Hyperlipidemia | 5371 (13.3) | 4513 (10.2) | 9884 (11.7) | <.001 |
| Race/ethnicity | ||||
| White | 31 273 (74.1) | 41 667 (90.0) | 72 940 (82.4) | <.001 |
| Black | 5853 (13.9) | 2402 (5.2) | 8255 (9.3) | |
| Hispanic | 3198 (7.6) | 1113 (2.4) | 4311 (4.9) | |
| Other | 1873 (4.4) | 1136 (2.5) | 3009 (3.4) | |
| Education | ||||
| High school or less | 11 324 (26.6) | 7811 (16.8) | 19 135 (21.5) | <.001 |
| Some college or more | 26 341 (61.9) | 34 852 (74.9) | 61 193 (68.7) | |
| Other | 4881 (11.5) | 3845 (8.3) | 8726 (9.8) | |
| Income, $ | ||||
| <20 000 | 7251 (18.4) | 3460 (7.8) | 10 711 (12.7) | <.001 |
| 20 000-74 000 | 25 462 (64.6) | 28 745 (64.5) | 54 207 (64.5) | |
| ≥75 000 | 6730 (17.1) | 12 365 (27.7) | 19 095 (22.7) | |
| BMI, median (IQR) | 27.4 (24.2-31.6) | 26.2 (23.4-30.0) | 26.8 (23.7-30.8) | <.001 |
| Parity | ||||
| No term pregnanciesa | 1420 (3.3) | 531 (1.1) | 1951 (2.2) | <.001 |
| 1 | 4391 (10.3) | 4384 (9.4) | 8775 (9.8) | |
| 2 | 11 884 (27.9) | 14 244 (30.6) | 26 128 (29.3) | |
| 3 | 11 005 (25.8) | 13 347 (28.6) | 24 352 (27.3) | |
| 4 | 6949 (16.3) | 7779 (16.7) | 14 728 (16.5) | |
| ≥5 | 7001 (16.4) | 6327 (13.6) | 13 328 (14.9) | |
| Breastfeeding | 22 874 (53.8) | 27 616 (59.3) | 50 490 (56.7) | <.001 |
| ASCVD | 2982 (6.9) | 3053 (6.5) | 6035 (6.7) | .01 |
| Age at ASCVD, median (IQR), y | 72.4 (67.0-77.4) | 71.7 (66.8-76.9) | 72.1 (66.9-77.1) | .09 |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range.
Women with no term pregnancies had to be pregnant for at least 6 months to be eligible.
APOs
Adverse pregnancy outcomes were reported by 13 482 women (28.8%). A single APO occurred in 8726 women, and 2 or more APOs were reported by 4756 women (eFigure 1 in the Supplement). The single most common APO was preterm delivery, which was reported by 6790 women (14.5%), followed by low birth weight, which was reported by 5773 women (12.3%) (eTable 1 in the Supplement). The most common combination of APOs was preterm delivery and low birth weight, with 3719 women (7.9%) reporting having had both conditions. Because many women reported both gestational hypertension (n = 1506) and/or preeclampsia (n = 2065), in subsequent analyses, we combined these responses into the single category of hypertensive disorders of pregnancy.
Baseline characteristics of women at entry into the WHI differed by the presence and type of APO (Table 2). Hypertension at entry in the WHI was significantly more prevalent among women who reported a prior hypertensive disorder of pregnancy (1457 of 2936 [49.6%]) than women reporting other APOs (low: 1782 of 6790 [26.2%]; high: 332 of 959 [34.6%]) or no APOs (6551 of 30 522 [21.5%]). Diabetes at entry into the WHI was significantly more prevalent among women who reported prior gestational diabetes (145 of 959 [15.1%]) compared with women reporting other APOs (low: 202 of 6790 [3.0%]; high: 158 of 2691 [5.9%]) or no APOs (556 of 30 522 [1.8%]). Other ASCVD risk factors, including age, hyperlipidemia, and smoking at study entry, were generally similar in women with different APOs. Baseline characteristics according to the survey responses yes, don’t know, and no for each APO are detailed in the eAppendix and eTable 2 in the Supplement.
Table 2. Baseline Characteristics According to Adverse Pregnancy Outcome (APO) Statusa.
| Characteristic | No. (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| No APOs (n = 30 522)b | Uncertain APO status (n = 2801)b | ≥1 APO (n = 13 482)b | Gestational diabetes (n = 959) | Low birth weight (n = 5773) | High birth weight (n = 2691) | Preterm delivery (n = 6790) | Hypertensive disorders of pregnancy (n = 2936) | |
| Age at enrollment, median (IQR), y | 60.0 (55.0-64.0) | 63.0 (57.0-67.0) | 60.0 (55.0-64.0) | 58.0 (54.0-61.0) | 60.0 (56.0-64.0) | 60.0 (56.0-65.0) | 60.0 (55.0-64.0) | 59.0 (55.0-64.0) |
| Hypertension | 6551 (21.5) | 1840 (65.9) | 4036 (30.0) | 332 (34.6) | 1603 (27.9) | 714 (26.7) | 1782 (26.3) | 1457 (49.8) |
| Diabetes | 556 (1.8) | 100 (3.6) | 530 (3.9) | 145 (15.1) | 177 (3.1) | 158 (5.9) | 202 (3.0) | 143 (4.9) |
| Smoking | 14 260 (46.9) | 1299 (46.7) | 6565 (48.9) | 422 (44.3) | 3075 (53.5) | 1143 (42.6) | 3417 (50.5) | 1366 (46.8) |
| Hyperlipidemia | 2718 (9.4) | 341 (12.9) | 1454 (11.4) | 106 (11.7) | 593 (10.8) | 278 (11.0) | 706 (11.0) | 394 (14.1) |
| Race/ethnicity | ||||||||
| Black | 1414 (4.7) | 218 (7.9) | 770 (5.8) | 73 (7.7) | 401 (7.0) | 99 (3.7) | 349 (5.2) | 227 (7.8) |
| Hispanic | 689 (2.3) | 84 (3.1) | 340 (2.5) | 37 (3.9) | 137 (2.4) | 72 (2.7) | 161 (2.4) | 77 (2.7) |
| White | 27 420 (90.7) | 2318 (84.4) | 11 929 (89.4) | 793 (83.9) | 5008 (87.7) | 2472 (92.8) | 6058 (90.2) | 2537 (87.3) |
| Other | 703 (2.3) | 128 (4.7) | 305 (2.3) | 42 (4.4) | 166 (2.9) | 22 (0.8) | 148 (2.2) | 64 (2.2) |
| Education | ||||||||
| High school and less | 4863 (16.0) | 572 (20.5) | 2376 (17.7) | 160 (16.8) | 1024 (17.9) | 560 (20.9) | 1122 (16.6) | 562 (19.2) |
| Some college and more | 23 027 (75.9) | 1967 (70.6) | 9858 (73.6) | 706 (73.9) | 4194 (73.2) | 1879 (70.2) | 5061 (75.0) | 2089 (71.5) |
| Other | 2430 (8.0) | 247 (8.9) | 1168 (8.7) | 89 (9.3) | 515 (9.0) | 239 (8.9) | 569 (8.4) | 269 (9.2) |
| Income, $ | ||||||||
| <20 000 | 2062 (7.1) | 332 (12.7) | 1066 (8.3) | 86 (9.3) | 452 (8.2) | 270 (10.4) | 491 (7.6) | 241 (8.5) |
| 20 000-74 000 | 18 496 (63.6) | 1773 (67.8) | 8476 (65.8) | 585 (63.4) | 3616 (65.6) | 1714 (66.0) | 4199 (64.9) | 1943 (68.7) |
| ≥75 000 | 8508 (29.3) | 509 (19.5) | 3348 (26.0) | 252 (27.3) | 1448 (26.3) | 612 (23.6) | 1775 (27.5) | 645 (22.8) |
| BMI, median (IQR) | 25.9 (23.2-29.6) | 26.8 (23.9-30.9) | 26.7 (23.8-30.8) | 28.2 (24.6-32.3) | 26.0 (23.2-29.8) | 28.1 (25.0-32.3) | 26.1 (23.3-30.0) | 28.2 (24.7-32.5) |
| Parity | ||||||||
| No term pregnanciesc | 372 (1.2) | 60 (2.1) | 99 (0.7) | 1 (0.1) | 37 (0.6) | 5 (0.2) | 84 (1.2) | 5 (0.2) |
| 1 | 3194 (10.5) | 310 (11.1) | 880 (6.5) | 59 (6.2) | 380 (6.6) | 68 (2.5) | 442 (6.5) | 267 (9.1) |
| 2 | 10 123 (33.2) | 818 (29.2) | 3303 (24.5) | 253 (26.4) | 1309 (22.7) | 462 (17.2) | 1632 (24.0) | 779 (26.5) |
| 3 | 8721 (28.6) | 771 (27.5) | 3855 (28.6) | 298 (31.1) | 1621 (28.1) | 765 (28.4) | 1947 (28.7) | 860 (29.3) |
| 4 | 4699 (15.4) | 448 (16.0) | 2632 (19.5) | 169 (17.6) | 1156 (20.0) | 619 (23.0) | 1338 (19.7) | 539 (18.4) |
| ≥5 | 3283 (10.8) | 376 (13.4) | 2668 (19.8) | 175 (18.2) | 1253 (21.7) | 758 (28.2) | 1328 (19.6) | 479 (16.3) |
| Breastfeeding | 18 194 (59.6) | 1651 (58.9) | 7771 (57.6) | 604 (63.0) | 3056 (52.9) | 1770 (65.8) | 3802 (56.0) | 1643 (56.0) |
| ASCVD | 1758 (5.8) | 266 (9.5) | 1028 (7.6) | 86 (9.0) | 458 (7.9) | 202 (7.5) | 513 (7.6) | 273 (9.3) |
| Age at ASCVD, median (IQR), y | 71.9 (66.9-76.9) | 73.6 (69.1-80.1) | 70.8 (66.3-75.7) | 69.5 (63.5-74.4) | 70.7 (66.0-75.9) | 72.4 (67.8-76.3) | 70.6 (65.6-76.0) | 69.6 (64.7-74.9) |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range.
The number of women with any APO does not equal the sum of yes responses to each APO, since some women had more than 1 APO. Data in columns for the individual APOs refer to women who answered yes; baseline characteristics of those who responded don’t know are summarized for each APO in eTable 2 in the Supplement.
Women who answered no to all APO questions are included in the No APO column; women who answered yes to 1 or more APO are included in the Any APO column; and women who answered don’t know to at least 1 APO without answering yes to any APO are included in the Uncertain APO Status column.
Women with no term pregnancies needed to be pregnant for at least 6 months to be eligible.
A total of 1028 of 13 482 women with an APO (7.6%) had developed ASCVD between entry into WHI and the time of the survey compared with 1758 of 30 522 women without an APO (5.8%) (Table 2; eFigure 2 in the Supplement). The mean (SD) age at onset of ASCVD was lower among women with a history of an APO than those without (70.8 years; IQR, 66.3-75.7 years vs 71.9 years; IQR, 66.9-76.9 years).
APOs and ASCVD
The associations of the responses yes and don’t know for each APO with ASCVD were similar in the multinomial logistic model, which separately compared the yes and don’t know responses with the reference category (no); for simplicity, we present the odds ratios (ORs) for the yes responses in the article and present the ORs for the don’t know responses in eFigure 3 in the Supplement. The ORs for the yes responses in the multinomial model were also similar to the ORs for yes responses in 2 alternative models of the association of APOs with ASCVD, including a binary logistic model in which don’t know responses were treated as missing data and a binary logistic model in which don’t know and yes responses were combined into a single category and compared with no responses (eTable 3 in the Supplement).
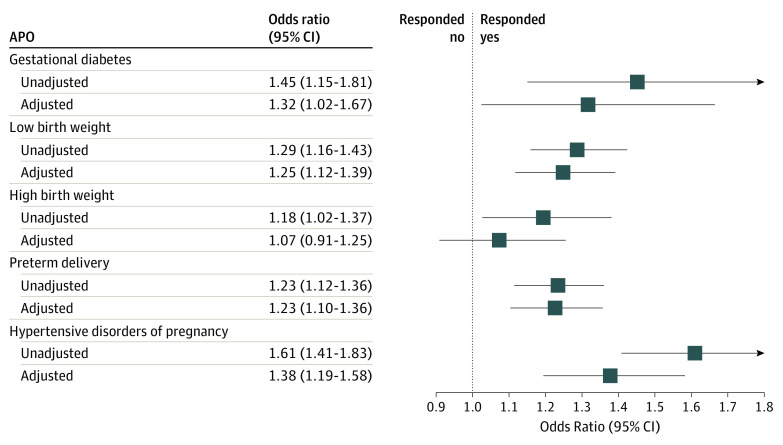
Each of the 5 APOs was significantly associated with ASCVD in a univariate model (Figure 2). After adjustment for traditional ASCVD risk factors, all APOs remained statistically significantly associated with ASCVD, with the exception of high birth weight (Figure 2). The associations of low birth weight and preterm delivery with ASCVD were largely unchanged by adjustment for traditional risk factors, while the associations of other APOs with ASCVD were attenuated by roughly half after adjustment for traditional risk factors, although they remained significant (Figure 2). The association of hypertensive disorders of pregnancy with ASCVD was primarily attenuated by adjustment for subsequent development of hypertension, while the association of gestational diabetes with ASCVD was primarily attenuated by adjustment for subsequent development of diabetes (eFigure 4 in the Supplement).
Figure 2. Association of Individual Adverse Pregnancy Outcomes (APOs) With Atherosclerotic Cardiovascular Disease (ASCVD).
Each line displays the odds ratio and its 95% CI from the comparison of yes and no responses based on a multinomial logistic model. For each APO, the top line shows the odds ratio for the APO from an unadjusted model and the bottom line shows the odds ratio for the APO from a model that adjusted for all traditional ASCVD risk factors, including age, hyperlipidemia, hypertension, diabetes, and smoking.
Multiple APOs
When all 5 APOs were tested jointly for their association with ASCVD in a model that adjusted for traditional risk factors, only hypertensive disorders of pregnancy and low birth weight were independently associated with ASCVD. Hypertensive disorders of pregnancy had an adjusted OR of 1.34 (95% CI, 1.15 to 1.54), and low birth weight had an adjusted OR of 1.18 (95% CI, 1.03 to 1.35) (Figure 3).
Figure 3. Association of Multiple Adverse Pregnancy Outcomes (APOs) With Atherosclerotic Cardiovascular Disease (ASCVD).
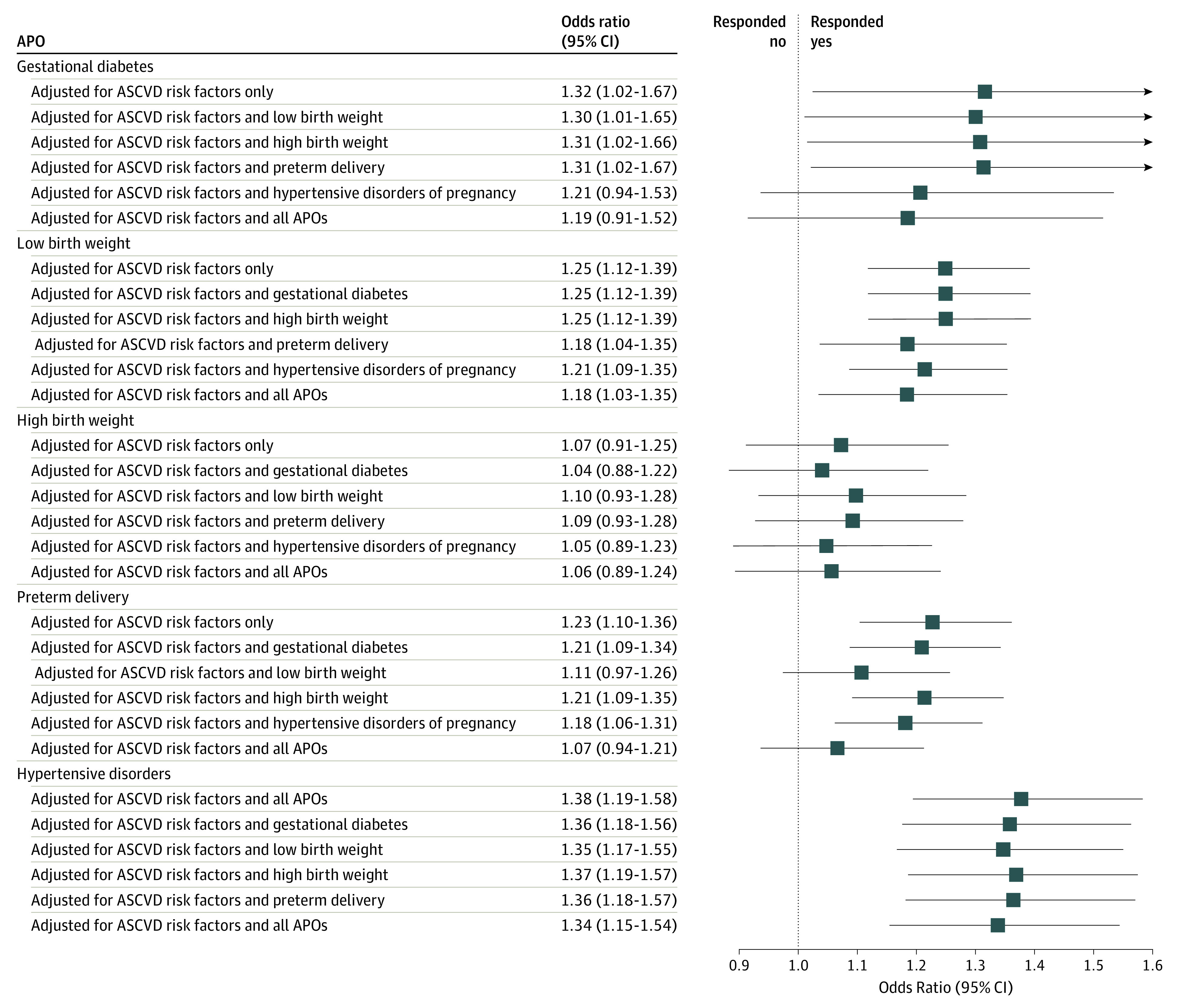
Each line displays the odds ratio and it 95% CI from the comparison of yes and no responses based on a multinomial logistic regression model. For each APO, the top line shows the odds ratio adjusted for traditional ASCVD risk factors, including age, hyperlipidemia, hypertension, diabetes, and smoking, but for no other APOs. The next 4 lines show the odds ratio adjusted for the traditional ASCVD risk factors plus an additional APO. The bottom line shows the odds ratio for the APO adjusted for the traditional ASCVD risk factors plus all other 4 APOs.
Additional Adjustments and Effect Modification
All results were not materially changed after additional adjustment for race/ethnicity, income, education, body mass index, breastfeeding, and parity (eFigure 5 in the Supplement). There was no statistically significant effect modification by race/ethnicity of any of the associations between APOs and ASCVD (eFigure 5 in the Supplement). Results from all analyses were virtually unchanged when multiple imputation of missing baseline data was used.
Discussion
In this large, multiethnic cohort of women, gestational diabetes, hypertensive disorders of pregnancy, preterm delivery, and low birth weight were significantly associated with ASCVD, even after adjustment for traditional ASCVD risk factors. When all 5 APOs were assessed together in a single model (which also adjusted for ASCVD risk factors), hypertensive disorders of pregnancy and low birth weight were each independently associated with ASCVD. All of the associations between individual APOs and ASCVD remained significant after further adjustment for race/ethnicity and socioeconomic status, without evidence of effect modification by race/ethnicity. Our study supports guideline recommendations that clinicians should consider a history of pregnancy-associated disorders when assessing ASCVD risk in older women.19,20 Indeed, our results suggest that hypertensive disorders of pregnancy and low birth weight are the most important APOs to consider as potential ASCVD risk enhancers.
The association between pregnancy outcomes and women’s cardiovascular health has become a focus of research interest and might identify unique mechanisms of ASCVD development in women. Previous studies have been inconsistent in demonstrating whether specific individual APOs add to risk prediction. A 2019 study21 reported that adding preeclampsia, gestational hypertension, preterm delivery, and small for gestational age to risk prediction models modestly increased risk discrimination for ASCVD events and added to information provided by traditional risk factors. Adverse pregnancy outcomes, which have been termed a positive stress test, are associated with late-onset ASCVD, but it is not clear whether these associations are independent of established ASCVD risk factors because hypertensive disorders of pregnancy and gestational diabetes are antecedents of diabetes and hypertension.22,23,24
Prior studies have not found significant associations between high birth weight (or large for gestational age) and later maternal cardiovascular disease.25,26 Low birth weight and small for gestational age are common metrics of the health of a pregnancy, and each has been associated with cardiovascular disease in prior studies.2 Infants may be small for gestational age because of poor implantation of the placenta into the uterus or from vascular insufficiency of the maternal uterine artery, leading to inadequate levels of oxygen and nutrients to the fetus. Low birth weight is defined as the weight of an infant at birth, regardless of gestational age, and may be owing to premature birth. Genetic factors and maternal nutrition may also affect fetal size.
Our study confirms that traditional ASCVD risk factors are more common in women who have had the APOs we studied but also that APOs remain significantly associated with ASCVD even after adjusting for these risk factors. Our study extends prior work by evaluating the joint associations of several APOs with ASCVD, while most prior studies have assessed only single APOs. Because a woman can have more than 1 APO (eFigure 1 in the Supplement), it has been uncertain whether some of the specific APOs that we studied are more closely associated with ASCVD risk, particularly because hypertensive disorders of pregnancy, low birth weight, and preterm delivery may share the same underlying pathophysiology.2,22,27 Our finding that hypertensive disorders of pregnancy and low birth weight were independently associated with ASCVD suggests that these APOs merit particular scrutiny in future epidemiologic and mechanistic studies.
Hypertensive disorders of pregnancy have been found to be associated with late ASCVD in meta-analyses.6,8,9 Low birth weight was not significantly associated with ASCVD in a 2019 meta-analysis of cohort studies,8 but we found a strong independent association between low birth weight and ASCVD, which is plausible because low birth weight, preterm birth, and hypertensive disorders of pregnancy may all arise from placental dysfunction.2,22,27,28,29,30 Preterm delivery has also been found to be associated with ASCVD in a 2018 meta-analysis,10 and while our study confirms this association, it was no longer significant after adjustment for low birth weight because these APOs commonly occur in the same pregnancy and share pathophysiologic mechanisms. Hypertensive disorders of pregnancy and low birth weight remained independently associated with ASCVD when adjusting for a full APO history, confirming the results of previous studies.6,7,8,9
Prior meta-analyses8 have demonstrated an association between gestational diabetes and ASCVD, which we confirmed in this study. However, this association was attenuated by adjustment for subsequent development of diabetes and was not independent of other APOs. It is important to note that the definition of gestational diabetes has evolved over the past 50 years, and with the advent of oral glucose tolerance testing in the 1970s and more aggressive care for gestational diabetes, the accuracy of the diagnosis of gestational diabetes has improved, and more recent studies will be less subject to exposure misclassification.29
It is unclear whether APOs are associated with ASCVD because they are involved in novel pathophysiologic processes or whether their association with ASCVD serves as an indicator of longer-term and more severe underlying cardiometabolic risk, either by heralding earlier development of diabetes, hypertension, and metabolic syndrome or by serving as a stress test for preexisting metabolic risk.22 Prior studies suggest that APOs remain associated with ASCVD even after adjustment for traditional risk factors, but they could still be serving as markers for more severe metabolic abnormalities. Novel pathophysiologic pathways might connect APOs with late ASCVD, and this possibility will be important to assess in future studies.
Limitations
This study has limitations. This study was based on 46 805 WHI participants who had survived to 2017 and were able to respond to our survey about APOs, which may have introduced survival bias into the estimated strengths of association. However, it is most likely that the women at highest risk of ASCVD would have died prior to the survey, which would have biased our findings toward the null and might account for the lower ORs in our study than reported by prior studies.8
We relied on self-reported APOs, and while women’s ability to recall APOs has been validated in short-term studies,30 it has not been studied over the longer intervals in this study. Study participants’ recall of birth weight and early delivery seemed to be more confident than their recall of gestational diabetes or hypertensive disorders of pregnancy. It is possible that recall bias may have affected our results. It would have been ideal for us to have obtained objective information from medical records about APOs in the study participants; however, the fragmented health care system in the US and the lack of longitudinal, searchable records going back 4 to 5 decades makes retrieval of objective records on APOs infeasible. To the extent that self-reported APOs are uncertain, the likely bias in our results would be toward the null.
This study did not include as many minority women as the entire WHI because of their higher mortality and lower response rates to the survey. Nevertheless, we had a sufficient sample of nonwhite women to document the consistency of the associations between APOs and ASCVD by race/ethnicity. We had data on body mass index only at the time of enrollment, not prior to pregnancy, and we lacked data on gestational weight gain and hence could not assess their effects on ASCVD risk.
Additionally, we assessed the birth weight and preterm delivery in categories and not as continuous variables. It would have been ideal to test associations of measured birth weight and gestational age at delivery as well as continuous measurements of glucose tolerance and blood pressure with the development of ASCVD.
Conclusions
One or more APOs occurred in roughly one-third of women in this large multiethnic cohort study and were independently associated with late ASCVD. Hypertensive disorders of pregnancy and low birth weight were noteworthy because their associations with ASCVD were independent of both traditional cardiac risk factors and preterm delivery and gestational diabetes; consequently, hypertensive disorders of pregnancy and low birth weight may be particularly important risk enhancers to consider when performing ASCVD risk stratification in older women. Further research is needed to understand the potential mechanisms that might link hypertensive disorders of pregnancy and low birth weight with late ASCVD.
eAppendix. WHI survey of adverse pregnancy outcomes.
eTable 1. Distribution of adverse pregnancy outcomes.
eTable 2. Baseline characteristics for each APO by response (yes, don’t know, and no).
eTable 3. Primary and secondary analyses of the association of APOs with ASCVD.
eFigure 1. Overlap between the different adverse pregnancy outcomes (APOs).
eFigure 2. Prevalence of ASCVD by APO response (yes, don’t know, and no).
eFigure 3. Associations between don’t know responses to APO survey items and ASCVD.
eFigure 4. Associations between APOs and ASCVD adjusted for individual traditional risk factors.
eFigure 5. Associations between APOs and ASCVD, with additional adjustment for race/ethnicity, education, income, parity, breastfeeding, and body mass index.
References
- 1.Xu J, Murphy SL, Kochanek KD, Bastian B, Arias E. Deaths: final data for 2016 (National Vital Statistics Reports volume 67, number 5). Natl Vital Stat Reports. 2018;67(6):1-76. [PubMed] [Google Scholar]
- 2.Rich-Edwards JW, Fraser A, Lawlor DA, Catov JM. Pregnancy characteristics and women’s future cardiovascular health: an underused opportunity to improve women’s health? Epidemiol Rev. 2014;36(1):57-70. doi: 10.1093/epirev/mxt006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martinez G, Daniels K, Chandra A. Fertility of men and women aged 15-44 years in the United States: National Survey of Family Growth, 2006-2010. Natl Health Stat Report. 2012;51(51):1-28. [PubMed] [Google Scholar]
- 4.Hutcheon JA, Lisonkova S, Joseph KS. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol. 2011;25(4):391-403. doi: 10.1016/j.bpobgyn.2011.01.006 [DOI] [PubMed] [Google Scholar]
- 5.Bertoni AG, Burke GL, Owusu JA, et al. . Inflammation and the incidence of type 2 diabetes: the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care. 2010;33(4):804-810. doi: 10.2337/dc09-1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974-977. doi: 10.1136/bmj.39335.385301.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fraser A, Nelson SM, Macdonald-Wallis C, et al. . Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the Avon Longitudinal Study of Parents and Children. Circulation. 2012;125(11):1367-1380. doi: 10.1161/CIRCULATIONAHA.111.044784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grandi SM, Filion KB, Yoon S, et al. . Cardiovascular disease-related morbidity and mortality in women with a history of pregnancy complications. Circulation. 2019;139(8):1069-1079. doi: 10.1161/CIRCULATIONAHA.118.036748 [DOI] [PubMed] [Google Scholar]
- 9.Wu P, Haththotuwa R, Kwok CS, et al. . Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2017;10(2):1-9. doi: 10.1161/CIRCOUTCOMES.116.003497 [DOI] [PubMed] [Google Scholar]
- 10.Wu P, Gulati M, Kwok CS, et al. . Preterm delivery and future risk of maternal cardiovascular disease: a systematic review and meta-analysis. J Am Heart Assoc. 2018;7(2):e007809. doi: 10.1161/JAHA.117.007809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haas DM, Parker CB, Marsh DJ, et al. ; NHLBI nuMoM2b Heart Health Study . Association of adverse pregnancy outcomes with hypertension 2 to 7 years postpartum. J Am Heart Assoc. 2019;8(19):e013092. doi: 10.1161/JAHA.119.013092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haas DM, Ehrenthal DB, Koch MA, et al. ; National Heart, Lung, and Blood Institute nuMoM2b Heart Health Study Network . Pregnancy as a window to future cardiovascular health: design and implementation of the nuMoM2b heart health study. Am J Epidemiol. 2016;183(6):519-530. doi: 10.1093/aje/kwv309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mosca L, Benjamin EJ, Berra K, et al. ; American Heart Association . Effectiveness-based guidelines for the prevention of cardiovascular disease in women, 2011 update: a guideline from the American Heart Association. J Am Coll Cardiol. 2011;57(12):1404-1423. doi: 10.1016/j.jacc.2011.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grundy SM, Stone NJ, Bailey AL, et al. . 2018 AHA/ACC/aacvpr/aapa/abc/acpm/ada/ags/apha/aspc/nla/pcna guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):e285-e350. doi: 10.1016/j.jacc.2018.11.003 [DOI] [PubMed] [Google Scholar]
- 15.Piepoli MF, Hoes AW, Agewall S, et al. ; ESC Scientific Document Group . 2016 European guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315-2381. doi: 10.1093/eurheartj/ehw106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The Women’s Health Initiative Study Group Design of the Women’s Health Initiative clinical trial and observational study. Control Clin Trials. 1998;19(1):61-109. doi: 10.1016/S0197-2456(97)00078-0 [DOI] [PubMed] [Google Scholar]
- 17.Hays J, Hunt JR, Hubbell FA, et al. . The Women’s Health Initiative recruitment methods and results. Ann Epidemiol. 2003;13(9)(suppl):S18-S77. doi: 10.1016/S1047-2797(03)00042-5 [DOI] [PubMed] [Google Scholar]
- 18.Curb JD, McTiernan A, Heckbert SR, et al. ; WHI Morbidity and Mortality Committee . Outcomes ascertainment and adjudication methods in the Women’s Health Initiative. Ann Epidemiol. 2003;13(9)(suppl):S122-S128. doi: 10.1016/S1047-2797(03)00048-6 [DOI] [PubMed] [Google Scholar]
- 19.Brown HL, Warner JJ, Gianos E, et al. ; American Heart Association and the American College of Obstetricians and Gynecologists . Promoting risk identification and reduction of cardiovascular disease in women through collaboration with obstetricians and gynecologists: a Presidential Advisory From the American Heart Association and the American College of Obstetricians and Gynecologists. Circulation. 2018;137(24):e843-e852. doi: 10.1161/CIR.0000000000000582 [DOI] [PubMed] [Google Scholar]
- 20.Arnett DK, Blumenthal RS, Albert MA, et al. . 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. doi: 10.1161/CIR.0000000000000678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Markovitz AR, Stuart JJ, Horn J, et al. . Does pregnancy complication history improve cardiovascular disease risk prediction? findings from the HUNT study in Norway. Eur Heart J. 2019;40(14):1113-1120. doi: 10.1093/eurheartj/ehy863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siddiqui N, Hladunewich M. Understanding the link between the placenta and future cardiovascular disease. Trends Cardiovasc Med. 2011;21(7):188-193. doi: 10.1016/j.tcm.2012.05.008 [DOI] [PubMed] [Google Scholar]
- 23.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25(10):1862-1868. doi: 10.2337/diacare.25.10.1862 [DOI] [PubMed] [Google Scholar]
- 24.Ahmed R, Dunford J, Mehran R, Robson S, Kunadian V. Pre-eclampsia and future cardiovascular risk among women: a review. J Am Coll Cardiol. 2014;63(18):1815-1822. doi: 10.1016/j.jacc.2014.02.529 [DOI] [PubMed] [Google Scholar]
- 25.Li C-Y, Chen H-F, Sung F-C, et al. . Offspring birth weight and parental cardiovascular mortality. Int J Epidemiol. 2010;39(4):1082-1090. doi: 10.1093/ije/dyq045 [DOI] [PubMed] [Google Scholar]
- 26.Bonamy AK, Parikh NI, Cnattingius S, Ludvigsson JF, Ingelsson E. Birth characteristics and subsequent risks of maternal cardiovascular disease: effects of gestational age and fetal growth. Circulation. 2011;124(25):2839-2846. doi: 10.1161/CIRCULATIONAHA.111.034884 [DOI] [PubMed] [Google Scholar]
- 27.Romero R, Kusanovic JP, Chaiworapongsa T, Hassan SS. Placental bed disorders in preterm labor, preterm PROM, spontaneous abortion and abruptio placentae. Best Pract Res Clin Obstet Gynaecol. 2011;25(3):313-327. doi: 10.1016/j.bpobgyn.2011.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Valdiviezo C, Garovic VD, Ouyang P. Preeclampsia and hypertensive disease in pregnancy: their contributions to cardiovascular risk. Clin Cardiol. 2012;35(3):160-165. doi: 10.1002/clc.21965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol. 1982;144(7):768-773. doi: 10.1016/0002-9378(82)90349-0 [DOI] [PubMed] [Google Scholar]
- 30.Carter EB, Stuart JJ, Farland LV, et al. . Pregnancy complications as markers for subsequent maternal cardiovascular disease: validation of a maternal recall questionnaire. J Womens Health (Larchmt). 2015;24(9):702-712. doi: 10.1089/jwh.2014.4953 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. WHI survey of adverse pregnancy outcomes.
eTable 1. Distribution of adverse pregnancy outcomes.
eTable 2. Baseline characteristics for each APO by response (yes, don’t know, and no).
eTable 3. Primary and secondary analyses of the association of APOs with ASCVD.
eFigure 1. Overlap between the different adverse pregnancy outcomes (APOs).
eFigure 2. Prevalence of ASCVD by APO response (yes, don’t know, and no).
eFigure 3. Associations between don’t know responses to APO survey items and ASCVD.
eFigure 4. Associations between APOs and ASCVD adjusted for individual traditional risk factors.
eFigure 5. Associations between APOs and ASCVD, with additional adjustment for race/ethnicity, education, income, parity, breastfeeding, and body mass index.