Abstract
Background:
The coronavirus disease-19 has been labeled a pandemic by World Health Organization. By virtue of its highly contagious attribution, this virus has spread across over the world and the numbers are still rapidly increasing. Increasing numbers of confirmed cases and mortality rates of coronavirus disease 2019 are occurring in several countries. The aim of this systematic review was to summarize clinical presentations of this newly emerging coronavirus disease.
Methods:
A systematic review of published articles was conducted using databases such as PubMed, Scopus, and Google Scholar. A search was conducted on 18 to 25 April 2020. Search terms included “novel coronavirus,” “2019 novel coronavirus,” “Coronavirus disease 2019,” “COVID-19,” “severe acute respiratory syndrome coronavirus 2.” The studies published in the English language and their full texts available were included. The eligible study designs were cross-sectional, case-control, cohort, and case series.
Results:
Thirty (30) studies which contain 4829 participants were included in this review. From included studies, the age of infected patients were found in range 0.25 to 94 years. The main clinical symptoms of COVID-19 patients were fever (77.6%), cough (64.8%), fatigue (27.2%), dyspnea (21.2%) and sputum production (18.0%).
Conclusion:
This systematic review identified that fever, cough, fatigue, and dyspnea were the most common reported clinical features of coronavirus disease 19. Understanding of the clinical spectrum and impact of this novel disease is important for all individuals, especially for healthcare workers to manage and prevent it.
Keywords: Coronavirus disease 19, COVID-19, clinical presentation, systematic review
Background
Coronavirus disease 19 (COVID-19) is a respiratory virus which is occurred by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 Toward the end of December 2019, it was identified with human-to-human transmission and severe human infection, originating in Wuhan, China. The virus has been labeled a pandemic by World Health Organization (WHO) since March, 2020.2 By virtue of its highly contagious attribution, this novel coronavirus has spread across over the world and the numbers are still rapidly increasing.3 As of 25 April 2020, more than 3 million laboratory-confirmed cases have been documented and several death cases reported globally. Almost all countries in world have identified confirmed cases of COVID-19.4
Increasing numbers of confirmed cases and mortality rates of coronavirus disease 2019 are occurring in several countries.5 United States (U.S) is a country with the highest coronavirus cases. U.S has also witnessed the highest number of deaths due to COVID-19 in the world. Coronavirus continues to be severe in Italy and Spain, making it the most-affected countries in Europe.4 It is identified that about 15% of COVID-19 patients have severe illness and 5% have critical illness. The mortality rate due the virus ranges from 0.25% to 3.0%. The mortality rates are much greater for susceptible populations, such as older people and those having underlying disorders.6
Elderly patients are susceptible to severe coronavirus disease 2019 outcomes as a consequence of their age and, in some cases, underlying health conditions.7 Studies from China have indicated that elderly patients, particularly those with chronic comorbidities, are at increased risk for severe illness and death. Even though the majority of COVID-19 cases in China were mild (81%), elderly people above 60 years deaths were approximately 80%.8 A study from US reported that 80% of deaths due to COVID-19 were aged ⩾65 years with the greatest percentage of severe outcomes amid people aged ⩾85 years.9 Although elderly and those with underlying disorders appear to be more vulnerable to becoming severely ill with the virus, people of all ages can be infected by the virus.2
The ongoing COVID-2019 outbreak brought a significant threat to global public health and created a global health crisis.10 The outbreak of coronavirus disease 19 not only resulted great public concern, but also brought about huge psychological disturbance, particularly for health care workers. A study identified that more than one third of healthcare professionals standing frontline to handle the outbreak during its peak in China had insomnia. The healthcare professionals who suffered from insomnia were also more likely to feel depressed, anxious, and have stress-based trauma.11
It is confirmed that COVID-19 is spread by human-to-human transmission via droplets or direct contact, and infection has been estimated to have mean incubation period of 6.4 days.12 COVID-19 may cause disease ranging from asymptomatic to fatal disease.13 Recent evidence suggests that even someone who is non-symptomatic can spread COVID-19 with high efficiency, and conventional measures of protection, such as face masks, provide insufficient protection. A patient undergoing surgery in a hospital in Wuhan infected 14 health-care workers while asymptomatic.14
The signs and symptoms of COVID-19 were extensively explained in WHO-China joint report on COVID-19. Symptoms are non-specific and the presentation of disease can range from asymptomatic to severe pneumonia and death. It was reported that fever, dry cough, fatigue, sputum production and shortness of breath were the most common symptoms.15 Severe damage on the lung tissue can result in acute respiratory distress syndrome (ARDS) which is the major contributor to intensive care unit care and mortality from COVID-19, especially in those older than 60 years, with history of smoking, and underlying disorders.16
COVID-19 is newly emerged and rapidly growing infectious disease outbreak which is challenging global community because of the limited amount of data available about the disease. As the spread virus is ongoing, the number of people infected with the virus will be increased and health workers need to understand these to minimize the impact of COVID-19 infection. Although the number of people infected by the virus is increasing through the world, no enough attention has been given to summarizing the clinical presentations of the virus. This review was aimed to summarize clinical presentations of COVID-19 which will help healthcare providers and public health policy makers in their efforts to treat patients and contain the current outbreak. Moreover, it will help to strengthen the knowledge of any reader about the clinical features of the disease.
Methods
Search strategy and database
The aim of this review was to summarize the clinical presentation of COVID-19 based on available literatures. This systematic review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.17 A systematic review of published literature was undertaken to identify studies that included clinical features of COVID-19.
The data bases such as PubMed, Scopus and Google scholar were employed to identify all relevant articles published on the theme of this review. A search was conducted for primary articles published in English language. A search was conducted on 18 to 25 April 2020 using the search MeSH “novel coronavirus,” “2019 novel coronavirus,” “2019-nCoV,” “Coronavirus disease 2019,” “COVID-19,” “severe acute respiratory syndrome coronavirus 2” and “SARS-CoV-2.” All studies identified during the database search were assessed for relevance to the review based on the information provided in the title and abstract. The full texts of eligible articles were then downloaded for further screening and final inclusion.
Among the 30 research articles included in this review, 23 articles were cross-sectionals, 4 articles were case series and 3 studies were retrospective cohorts. The studies included in this review were conducted in 9 different countries. These were China, US, Italy, Bolivia, Japan, German, Belgium, France, and Spain. However, the majority of studies were obtained from China as largest proportions of available articles were published by Chinese scholars.
Eligibility criteria and study selection
The studies published in the English language and their full texts available were included. Studies were included if they were published in peer-reviewed journals. The eligible study designs were cross-sectional, case-control, cohort, and case series. Studies were excluded on any 1 of the following conditions: the full article was not available, outcomes were not well-defined, a duplicate citation, review articles and the studies did not report to COVID-19 signs and symptoms. After duplicated removed, the title and abstract were used to screen the results of the initial search. The full texts of relevant articles were assessed for inclusion and exclusion criteria.
Data collection process and data items
Data extracted from eligible studies onto a standardized data abstraction sheet. The studies were extracted using author, publication year, country, study design, sample size, patient demographics such as age and sex, and clinical presentations. Two reviewers performed the data extraction and 1 reviewer assessed the accuracy of the extracted data.
Methodology quality assessment
The Agency for Healthcare Research and Quality (AHRQ) was used to assess the quality of included studies. It was done by 2 reviewers. These criteria included 11 items, including subjects’ selection, research quality control and data processing. Each question has “yes,” “no” or “unclear” and “not applicable” alternative responses in which 1 them is answer.18
Results
Search results
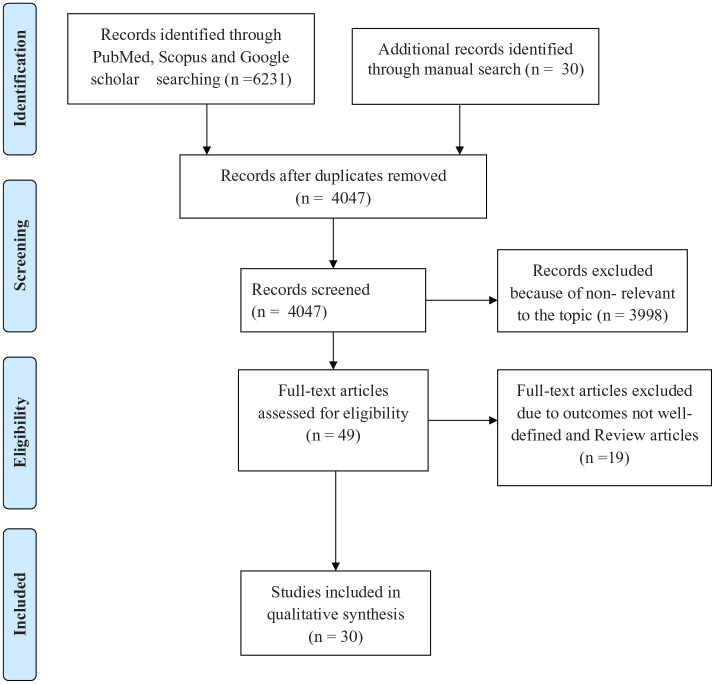
About 6261 studies were retrieved using search strategy. After removal of duplicates and irrelevant articles, about 49 articles obtained. Full texts of these 49 articles were accessed and 30 articles were accepted and considered for final review (Figure 1).
Figure 1.
PRISMA flow chart for study selection.
Inclusion criteria were primary articles published in English language and their full texts were available. The eligible study designs were cross-sectional, case-control, cohort, and case series. The study was excluded when outcomes were not well-defined, and did not report to COVID-19 signs and symptoms.
Characteristics of included studies
A total of 4829 study participants were included in this systematic review. The smallest age of in this study was 0.25 year and the oldest age was 94 years.
A study conducted in North Hospital of Changsha first Hospital in China reported that 18.6% of patients were severely ill. It was identified that one-fifth of total patients were had with at least 1 comorbid and advanced age is a high-risk factor for severe illness.19 Another study in China identified that 32% cases were over 60 years. It was also found that more patients in older group were diagnosed as severe.20 A Study from Wuhan, China reported that 33.3% of 102 patients infected with the virus in the hospital setting. This study identified that younger patients and health care workers were more likely to survived.21 The characteristics of the included studies are shown in Table 1.
Table 1.
The characteristics and demographic data of the included studies.
| Author | Year | Country | Study design | Sample size | Age (range in years) | Sex (male, %) |
|---|---|---|---|---|---|---|
| Zheng et al19 | 2020 | China | Cross sectional | 161 | 33.5-57 | 49.7 |
| Li et al22 | 2020 | China | Cross sectional | 131 | 20-90 | 48 |
| Cheng et al23 | 2020 | China | Cross sectional | 11 | 35-65 | 72.7 |
| Lian et al20 | 2020 | China | Cross sectional | 788 | 0.25-94 | 51.6 |
| Cao et al21 | 2020 | China | Cohort | 102 | 37-67 | 52.0 |
| Zhang et al24 | 2020 | China | Cross sectional | 17 | 23-74 | 47.1 |
| Wan et al25 | 2020 | China | Case series | 135 | 36-55 | 53.3 |
| Li et al26 | 2020 | China | Cross sectional | 25 | 29-66 | 48 |
| Yang et al27 | 2020 | China | Cohort | 149 | 32-59 | 54.4 |
| Li et al28 | 2020 | China | Cross sectional | 83 | 31-66 | 53 |
| Guan et al29 | 2020 | China | Cross sectional | 1099 | 35-58 | 58.2 |
| Goyal et al30 | 2020 | US | Case series | 393 | 18-75 | 60.6 |
| Giacomelli et al31 | 2020 | Italy | Cross sectional | 59 | 50-74 | 67.8 |
| Song et al32 | 2020 | China | Cross sectional | 51 | 33-65 | 49 |
| Escalera-Antezana et al33 | 2020 | Bolivia | Cross sectional | 12 | 25-43 | 50 |
| Huang et al34 | 2020 | China | Cross sectional | 41 | 41-58 | 73 |
| Wang et al35 | 2020 | China | Cross sectional | 69 | 35-62 | 46 |
| Tabata et al36 | 2020 | Japan | Cross sectional | 104 | 25-93 | 51·9 |
| Zhao et al3 | 2020 | China | Cohort | 77 | 1-94 | 44.2 |
| Chen et al37 | 2020 | China | Cross sectional | 99 | 21-82 | 68 |
| Chen et al38 | 2020 | China | Cross sectional | 29 | 26-79 | 72.4 |
| Wang et al39 | 2020 | China | Cross sectional | 138 | 42-68 | 54.3 |
| Liu et al40 | 2020 | China | Cross sectional | 137 | 20-83 | 44.5 |
| Liu et al41 | 2020 | China | Case series | 24 | 12-84 | 33.3 |
| Yang et al42 | 2020 | China | Cross sectional | 52 | 33.6-85.8 | 67.3 |
| Luers et al43 | 2020 | German | Cross sectional | 72 | 21-87 | 56.9 |
| Zou et al44 | 2020 | China | Cross sectional | 81 | 50-68.5 | 46.9 |
| Lechien et al45 | 2020 | Belgium* | Cross sectional | 417 | 19-77 | 36.9 |
| Mao et al46 | 2020 | China | Case series | 214 | 37-68 | 40.7 |
| Yan et al47 | 2020 | US | Cross sectional | 59 | 18-79 | 49.2 |
-Included other 3 countries: France, Spain and Italy.
By summarizing the clinical presentation of COVID-19, we found that the main clinical symptoms of COVID-19 patients were fever (77.6%), cough (64.8%), fatigue (27.2%), and dyspnea (21.2%). Less commonly reported symptoms include headache or dizziness (15.2%), diarrhea (11.8%), and nausea and vomiting (5.9%). Some studies reported olfactory disorders and gustatory disorders which counted 10.1% and 10%, respectively. Symptoms like hemoptysis, chills, fear of cold, chest pain/tightness, anorexia, confusion, and rhinitis were rarely reported clinical features of COVID-19 (Tables 2 and 3).
Table 2.
Clinical features of coronavirus from the included studies, 2020.
| Author | n | Fever | Cough | Dyspnea | Sore throat | Fatigue | Muscle ache /Arthralgia | Headache/dizziness | Diarrhea | Nausea and vomiting | Sputum production | Olfactory disorders | Gustatory disorders | Others |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Zheng et al19 | 161 | 122 (75.8) | 101 (62.7) | 23 (14.3) | – | 64 (39.8) | 18 (11.2) | 12 (7.5) | 17 (10.6) | 6 (3.7) | – | – | – | – |
| Li et al22 | 131 | 85 (65) | 85 (65) | 5 (4) | – | 13 (10) | 2 (2) | – | 1 (1) | – | – | – | – | – |
| Cheng et al23 | 11 | 8 (72.7) | 7 (63.6) | 1 (9.1) | 1 (9.1) | – | 3 (27.3) | – | 1 (9.1) | – | 3 (27.3) | – | – | – |
| Lian et al20 | 788 | 636 (80.7) | 506 (64.2) | 37 (4.7) | 111 (14.1) | 139 (17.6) | 91 (11.5) | 75 (9.5) | – | – | 265 (33.6) | – | – | 47 (5.9), 15 (1.9) |
| Cao et al21 | 102 | 83 (81.4) | 50 (49) | – | – | 56 (54.9) | 35 (34.3) | – | 11 (10.8) | – | – | – | – | – |
| Zhang et al24 | 17 | 12 (70.6) | 9 (52.9) | 1 (5.9) | 1 (5.9) | 6 (35.3) | 7 (41.2) | 4 (23.5) | – | – | 7 (41.2) | – | – | 5 (29.4) |
| Wan et al25 | 135 | 120 (88.9) | 102 (76.5) | 18 (13.3) | 24 (17.7) | 44 (32.5) | – | – | 18 (13.3) | – | 12 (8.8) | – | – | 14 (10.3), 12 (8.8) |
| Li et al26 | 25 | 24 (96) | 17 (68) | 20 (80) | – | 17 (68) | – | – | 5 (20) | – | – | – | – | – |
| Yang et al27 | 149 | 114 (76.5) | 87 (58.4) | 2 (1.34) | 21 (14.1) | – | 5 (3.36) | 13 (8.7) | 11 (7.4) | 2 (1.34) | 48 (32.2) | – | – | 21 (14.1), 16 (10.7) |
| Li et al28 | 83 | 72 (86.7) | 65 (78.3) | 9 (10.8) | 6 (7.2) | – | 15 (18.1) | 9 (10.8) | 7 (8.4) | – | 15 (18.1) | – | – | 5 (6) |
| Guan et al29 | 1099 | 966 (87.9) | 744 (67.7) | 204 (18.6) | 153 (13.9) | 419 (38.1) | 163 (14.8) | 150 (13.6) | 41 (3.7) | 55 (5.0) | 367 (33.4) | – | – | 125 (11.4), 53 (4.8) |
| Goyal et al30 | 393 | 303 (77.1) | 312 (79.4) | 222 (56.5) | – | – | 94 (23.9) | – | 93 (23.7) | 75 (19.1) | – | – | – | – |
| Giacomelli et al31 | 59 | 43 (72.8) | 22 (37.3) | 15 (25.4) | 1 (1.7) | – | 3 (5.1) | 2 (3.4) | – | – | – | 14 (23.7) | 17 (28.8) | – |
Others: hemoptysis, chills, fear of cold, chest pain/tightness, anorexia, nasal obstruction, nasal congestion.
Table 3.
Common patterns and distribution on clinical manifestation of patients with COVID-19.
| Clinical manifestation | No. of number of studies | No. of cases/total no. of patients | % |
|---|---|---|---|
| Fever | 30 | 3748/4829 | 77.6 |
| Cough | 29 | 3130/4829 | 64.8 |
| Dyspnea | 25 | 1026/4829 | 21.2 |
| Sore throat | 19 | 696/4829 | 14.4 |
| Fatigue | 22 | 1314/4829 | 27.2 |
| Muscle ache /Arthralgia | 20 | 866/4829 | 17.9 |
| Headache/dizziness | 23 | 736/4829 | 15.2 |
| Diarrhea | 23 | 569/4829 | 11.8 |
| Nausea and vomiting | 13 | 285/4829 | 5.9 |
| Sputum production | 17 | 867/4829 | 18.0 |
| Olfactory disorders | 6 | 486/4829 | 10.1 |
| Gustatory disorders | 6 | 484/4829 | 10.0 |
| Others | 12 | 802/4829 | 16.6 |
Others: hemoptysis, chills, fear of cold, chest pain/tightness, anorexia, confusion and rhinitis.
Table 2.
Clinical features of coronavirus from the included studies, 2020 (continued).
| Author | n | Signs and symptoms (%) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fever | Cough | Dyspnea | Sore throat | Fatigue | Muscle ache /Arthralgia | Headache/dizziness | Diarrhea | Nausea & vomiting | Sputum production | Olfactory disorders | Gustatory disorders | Others | ||
| Song et al32 | 51 | 49 (96) | 24 (47) | 7 (14) | 3 (6) | 16 (31) | – | 8 (16) | 5 (10) | 3 (6) | 2 (4) | – | – | 9 (18) |
| Escalera-Antezana et al33 | 12 | 9 (75) | 9 (75) | – | 5 (41.7) | 4 (33.3) | 5 (41.7) | – | 2 (16.7) | 1 (8.3) | – | – | – | |
| Huang et al34 | 41 | 40 (98) | 31 (76) | 22 (55) | – | 18 (44) | – | 3 (8) | – | – | 11 (28) | – | – | 2 (5) |
| Wang et al35 | 69 | 60 (87) | 38 (55) | 20 (29) | 6 (9) | 29 (42) | 21 (30) | 15 (21.7) | 10 (14) | 3 (4) | 20 (29) | – | – | 14 (20), 7 (10) |
| Tabata et al36 | 104 | 39 (37·5) | 50 (48·1) | 22 (21·2) | 11 (10·6) | 24 (23·1) | – | 20 (19·2) | 11 (10·6) | – | 24 (23·1) | – | – | – |
| Zhao et al3 | 77 | 66 (85.7) | 49 (63.6) | 16 (20.8) | 5 (6.5) | 21 (27.3) | 9 (11.7) | 10 (13) | 1 (1.3) | 6 (7.8) | 8 (10.4) | – | – | 9 (11.7) |
| Chen et al37 | 99 | 82 (83) | 81 (82) | 31 (31) | 5 (5) | – | 11 (11) | 8 (8) | 2 (2) | 1 (1) | – | – | – | 9 (9) |
| Chen et al38 | 29 | 28 (96.6) | 21 (72.4) | 17 (58.6) | – | 12 (41.4) | – | 2 (6.9) | 4 (13.8) | – | 21 (72.4) | – | – | – |
| Wang et al39 | 138 | 136 (98.6) | 82 (59.4) | 43 (31.2) | 24 (17.4) | 96 (69.6) | 48 (34.8) | 22 (15.9) | 14 (10.1) | 19 (13.8) | 37 (26.8) | – | – | 55 (39.9) |
| Kui et al40 | 137 | 112 (81.8) | 66 (48.2) | 26 (19.0) | – | 44 (32.1) | – | 13 (9.5) | 11 (8.0) | – | 6 (4.4) | – | – | 7 (5.1) |
| Liu et al41 | 24 | 19 (79.2) | 6 (25.0) | 2 (8.3) | – | 6 (25.0) | – | 4 (16.7) | – | – | – | – | – | – |
| Yang et al42 | 52 | 51 (98.1) | 40 (76.9) | 33 (63.5) | – | 18 (34.6) | 7 (13.5) | 3 (5.8) | – | 2 (3.8) | 3 (5.8) | – | – | 1 (1.9) |
Others: anorexia, chest tightness/pain, confusion, hemoptysis.
Table 2.
Clinical features of coronavirus from the included studies, 2020 (continued).
| Author | n | Signs and symptoms (%) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fever | Cough | Dyspnea | Sore throat | Fatigue | Muscle ache /Arthralgia | Headache/dizziness | Diarrhea | Nausea & vomiting | Sputum production | Olfactory disorders | Gustatory disorders | Others | ||
| Luers et al43 | 72 | 36 (50) | 54 (75) | – | 45 (62.5) | – | 51 (70.8) | 56 (77.8) | 22 (30.6) | – | – | 53 (73.6) | 50 (69.4) | 40 (55.6) |
| Zou et al44 | 81 | 59 (72.8) | – | – | – | 30 (37) | – | 12 (14.8) | – | – | – | 11 (13.6) | 21 (25.9) | 22 (27.2) |
| Lechien et al45 | 417 | 201 (48.2) | 326 (78.2) | 198 (47.5) | 224 (53.7) | 190 (45.6) | 241 (57.8) | 192 (46.0) | 213 (51.1) | 96 (23.0) | – | 357 (85.6) | 342 (88.8) | 218 (52.3) |
| Mao et al46 | 214 | 132 (61.7) | 107 (50) | – | 31 (14.5) | – | – | 64 (29.9) | 41 (19.2) | – | – | 11 (5.1) | 12 (5.6) | 68 (31.8) |
| Yan et al47 | 59 | 41 (69.5) | 39 (66.1) | 32 (54.2) | 19 (32.2) | 48 (81.4) | 37 (62.7) | 39 (66.1) | 28 (47.5) | 16 (27.1) | 18 (30.5) | 40 (67.8) | 42 (71.2) | 28 (47.5) |
Others: Rhinitis, chest pain, Anorexia and nasal obstruction.
Discussion
COVID-19 has already reached almost all countries around the world, sending billions of people into lockdown as health services struggle to contain it. Over the last 4 months, more than 3 millions laboratory-confirmed cases have been documented globally.4 The outbreak of this virus is an unprecedented disaster which affects the world including developed countries like U.S, China, and Italy in all aspects, especially health, social and economic.48
Even though COVID-19 presents with fever associated with cough, and dyspnea, the clinical presentations of COVID-19 are not specific which is difficult to differentiate it from other viral respiratory infections. Its clinical spectrum varies from asymptomatic to clinical conditions characterized by severe respiratory failure that necessitates mechanical ventilation and support in an intensive care unit. The virus may cause systemic manifestations in terms of sepsis and multiple organ dysfunction syndromes.49,50
A sufficient understanding of the characteristics of the coronavirus disease 19 is essential to effectively management the disease. It is also important to implement necessary measures in a timely manner. Even though we have some basic understanding of the clinical manifestations of coronavirus, our understanding is inadequate. This is due to inconsistencies reports still exist in the findings of many available literatures, and the sample sizes in of most of these literatures were too small for a dependable summary to be drawn.51 This systematic review combined data from 30 studies in order to bring a more reliable summary of the signs and symptoms of patients infected with coronavirus disease 19.
In this systematic review, we tried to summarize clinical presentation of COVID-19 confirmed cases. We found 4829 cases from 30 articles to summarize the major clinical manifestations of COVID-19. The most commonly observed symptoms were fever and cough. Fever was identified in 3748 cases (77.6%) which reported by all studies included in this review and its range was 42.3% to 98.6%. Cough was the second most common reported symptom in this review which presented in 3130 cases (64.8%) and its value varied from 25.0% to 82.0%.3,19-47 Fatigue was the third most common symptoms which experienced by 1314 cases (27.2%) (Tables 2 and 3). This finding was consistent with a systematic review and meta-analysis conducted by Rodriguez-Morales et al52 in which they reported fever and cough were the most frequently symptoms experienced by patients infected by coronavirus disease 19. They found fever in 88.7% 8, cough in 57.6% and fatigue in 29.4%. Our review was also in line with another systematic review and meta-analysis performed by Sun et al53 They reported that fever occurred in 89.8% of cases, cough in 72.2% and fatigue in 42.5%. This systematic review was also found similar results with a systematic review done by Lovato et al54 which reported that fever (85.6%), cough (68.7%), and fatigue (39.4%) were the most common symptoms of COVID-19.
Our review identified that gastrointestinal symptoms such as diarrhea, nausea and vomiting were minor clinical features of COVID-19. Some studies reported that patients also experienced olfactory disorders and gustatory disorders. Symptoms like hemoptysis, chills, fear of cold, chest pain/tightness, anorexia, confusion and rhinitis were rarely reported by some studies. Even though the virus is highly contagious, about 80% of infected people have mild symptoms or no symptoms.55 Therefore, healthcare workers have to understand these to minimize the impact COVID-19 on population, health systems, and economic risks and implement protective measures which enable to contain the disease.
One of the limitations of this review was language restriction. Only articles published in English language were considered. The second limitation was only available data from published articles were collected. Data from unpublished papers were not included. The other limitation could be exclusion of articles with no full texts as it can reduce sample size.
Conclusion
Clinical presentations of COVID-19 patients were mostly heterogeneous. Therefore, it is difficult to differentiate the virus from other respiratory infectious diseases based on the symptoms alone. This systematic review identified that fever, cough, fatigue, and dyspnea were the most common reported clinical features of coronavirus disease 19. Although symptoms such as hemoptysis, chills, fear of cold, chest pain/tightness, anorexia, confusion, and rhinitis were expressed by few people, they should not be ignored. Understanding of the clinical spectrum and impact of this novel disease is important for all individuals, especially for healthcare workers to manage and prevent it.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ contributions: TSH designed, arranged and supervised this study as the corresponding author. FB and TA participated in study design, searching articles, extracting, analysis, and/ or interpretation of data. TSH drafted the manuscript and all authors revised it. All authors have read and approved the final manuscript.
Availability of data and materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
ORCID iD: Tadesse Sheleme  https://orcid.org/0000-0002-4527-1571
https://orcid.org/0000-0002-4527-1571
References
- 1. CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) – United States. MMWR Morb Mortal Wkly Rep. 2020;69:343-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Coronavirus disease, 2020. https://www.who.int. Accessed April 18, 2020.
- 3. Zhao W, Yu S, Zha X, et al. Clinical characteristics and durations of hospitalized patients with COVID-19 in Beijing: a retrospective cohort study. MedRxiv. 2020. [Google Scholar]
- 4. COVID-19. Coronavirus pandemic, April 19, 2020. https://www.worldometers.info/coronavirus/. Accessed April 19, 2020.
- 5. Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:811-818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020; 382:2049-2055. [DOI] [PubMed] [Google Scholar]
- 7. Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing Facility King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Surveillances V. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly. 2020;2:113-122. [PMC free article] [PubMed] [Google Scholar]
- 9. COVID C, Team R. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lin Q, Zhao S, Gao D, Lou Y, Yang S, Musa SS, et al. A conceptual model for the coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China with individual reaction and governmental action. Int J Infect Dis. 2020;93:211-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang C, Yang L, Liu S, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. 2020;11:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020;55:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kannan S, Ali PSS, Sheeza A, Hemalatha K. COVID-19 (Novel Coronavirus 2019)–recent trends. Eur Rev Med Pharmacol Sci. 2020;24:2006-2011. [DOI] [PubMed] [Google Scholar]
- 14. Chang D, Xu H, Rebaza A, Sharma L, Dela Cruz CS. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir Med. 2020;8:e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Report of the WHO-China joint mission on coronavirus disease 2019. (COVID-19), 2020. https://www.who.int/docs/default-source/coronaviruse/whochina-joint-mission-on-covid-19-final-report.pdf. Accessed February 20, 2020.
- 16. Kakodkar P, Kaka N, Baig M. A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19). Cureus. 2020;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moher D, Liberati A, Tetzlaff J, Altman DG. Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Agency for Healthcare Research and Quality (AHRQ) checklist to assess quality of the included studies. 2013 https://www.ncbi.nlm.nih.gov/books/NBK35156/. Accessed April 27, 2020.
- 19. Zheng F, Tang W, Li H, Huang Y, Xie Y, Zhou Z. Clinical characteristics of 161 cases of corona virus disease 2019 (COVID-19) in Changsha. Eur Rev Med Pharmacol Sci. 2020;24:3404–10. [DOI] [PubMed] [Google Scholar]
- 20. Lian J, Jin X, Hao S, et al. Analysis of epidemiological and cinical features in older patients with corona virus disease 2019 (COVID-19) out of Wuhan. Clin Infect Dis. 2020;71:740–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cao J, Tu W-J, Cheng W, et al. Clinical features and short-term outcomes of 102 patients with corona virus disease 2019 in Wuhan, China [published online ahead of print April 2, 2020]. Clin Infect Dis. doi: 10.1093/cid/ciaa243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Li X, Zeng W, Li X, et al. CT imaging changes of corona virus disease 2019 (COVID-19): a multi-center study in Southwest China. J Transl Med. 2020;18:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cheng Z, Lu Y, Cao Q, et al. Clinical features and chest CT manifestations of coronavirus disease 2019 (COVID-19) in a single-center study in Shanghai, China. Am J Roentgenol. 2020:1-6. [DOI] [PubMed] [Google Scholar]
- 24. Zhang S, Li H, Huang S, You W, Sun H. High-resolution CT features of 17 cases of Corona Virus Disease 2019 in Sichuan province, China. Eur Respir J. 2020;55:2000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wan S, Xiang Y, Fang W, Zheng Y, Li B, Hu Y, et al. Clinical features and treatment of COVID-19 patients in Northeast Chongqing. J Med Virol. 2020;92:797-806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Li Y-K, Peng S, Li L-Q, et al. Clinical and transmission characteristics of Covid-19—A retrospective study of 25 cases from a single thoracic surgery department. Curr Med Sci. 2020:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yang W, Cao Q, Qin L, et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020;80:388-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Li K, Wu J, Wu F, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Investig Radiol. 2020;55:327-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Guan W-j, Ni Z-y, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv. 2020. [Google Scholar]
- 30. Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of covid-19 in New York City. N Engl J Med. 2020;382:2372-2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Giacomelli A, Pezzati L, Conti F, et al. Self-reported olfactory and taste disorders in patients with severe acute respiratory coronavirus 2 infection: a cross-sectional study. Clin Infect Dis. 2020; 71:889-890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Song F, Shi N, Shan F, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:210-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Escalera-Antezana JP, Lizon-Ferrufino NF, Maldonado-Alanoca A, et al. Clinical features of cases and a cluster of Coronavirus Disease 2019 (COVID-19) in Bolivia imported from Italy and Spain. Travel Med Infect Dis. 2020;35:101653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395:497-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wang Z, Yang B, Li Q, Wen L, Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2020;71:769-777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tabata S, Imai K, Kawano S, Ikeda M, Kodama T, Miyoshi K, et al. The clinical characteristics of COVID-19: a retrospective analysis of 104 patients from the outbreak on board the Diamond Princess cruise ship in Japan. medRxiv. 2020;18:v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chen L, Liu H, Liu W, et al. Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:E005-E. [DOI] [PubMed] [Google Scholar]
- 39. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Liu K, Fang Y-Y, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J. 2020;133:1025-1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Liu YSL, Zhang D, Tang S, et al. The epidemiological and clinical characteristics of 2019 novel coronavirus infection in Changsha, China. China. (2/10/2020). Available at SSRN: http://dx.doi.org./10.2139/ssrn.3537093 [Google Scholar]
- 42. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Luers JC, Rokohl AC, Loreck N, et al. Olfactory and gustatory dysfunction in Coronavirus disease 19 (COVID-19) [published online ahead of print May 1, 2020]. Clin Infect Dis. doi: 10.1093/cid/ciaa525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zou L, Yu T, Zhang Y, Dai L, Zhang Z. Olfactory and gustatory dysfunctions in patients with COVID-19 in Wuhan, China. Infect Dis. 2020. [Google Scholar]
- 45. Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020;277:2251-2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Yan CH, Faraji F, Prajapati DP, Boone CE, DeConde AS, eds. Association of chemosensory dysfunction and Covid-19 in patients presenting with influenza-like symptoms. Int Forum Allergy Rhinol. 2020;10:806-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Di Gennaro F, Pizzol D, Marotta C, et al. Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review. Int J Environ Res Public Health. 2020;17:2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lupia T, Scabini S, Pinna SM, Di Perri G, De Rosa FG, Corcione S. 2019-novel coronavirus outbreak: A new challenge. J Global Antimicrob Resist. 2020; 22-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Yang Y, Peng F, Wang R, Guan K, Jiang T, Xu G, et al. The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J Autoimmunity. 2020:102434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Tan SC. Clinical and epidemiological characteristics of Coronavirus Disease 2019 (COVID-19) patients. medRxiv. 2020. [Google Scholar]
- 52. Rodriguez-Morales AJ, Cardona-Ospina JA, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020:101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sun P, Qie S, Liu Z, Ren J, Xi JJ. Clinical characteristics of 50466 patients with 2019-nCoV infection. medRxiv. 2020. [Google Scholar]
- 54. Lovato A, de Filippis C. Clinical presentation of COVID-19: a systematic review focusing on upper airway symptoms. Ear Nose Throat J. 2020:0145561320920762. [DOI] [PubMed] [Google Scholar]
- 55. Organization WH. Coronavirus disease 2019 (COVID-19): situation report, 70. 2020. www.apps.who.in. Accessed April 28, 2020.