Abstract
The Armed Forces Medical Examiner System (AFMES) is the only medicolegal death investigation system of the US federal government. Its origins can be traced to three dried tissue specimens placed on a shelf by a Civil War Surgeon General in 1862. The collections and the library of the Army Surgeon General spawned the Armed Forces Institute of Pathology (AFIP), the National Museum of Health and Medicine, the Walter Reed Army Institute of Research, and the National Library of Medicine. Pathologists of the Army Medical Museum performed the autopsies of assassinated Presidents Lincoln and Garfield and assisted with that of Kennedy. The now defunct AFIP created the first forensic pathology training program approved by the American Board of Pathology and then the AFMES. Col Ed Johnston, CAPT Charlie Stahl, and Col Dick Froede were the original pioneers of the AFMES.
Keywords: Armed Forces Medical Examiner System, forensic pathology history, military, Stahl, Froede
Introduction
The Founding Fathers intentionally drafted the U.S. constitution to reserve matters of the health, safety, morals, and general welfare—the so-called police powers—to the states rather than the federal government. Until 1965, after Presidents Lincoln, Garfield, McKinley, and Kennedy were assassinated; it was not a federal crime to shoot the President of the United States. Military physicians were involved in the autopsies of each of the assassinated presidents. The Armed Forces Medical Examiner System (AFMES) was established in the wake of the John Fitzgerald Kennedy (JFK) assassination. The following is the story of how that came to be.
American Military Medicine
In the late 1700s, medicine was only beginning to transition to its more modern form. Bloodletting, whether by incision or leeches, was still common practice, and probably responsible for the death of President Washington. Medical schools in Leiden, Edinburgh, London, and Paris now rivaled that of Padua. John Hunter was establishing surgery and William Smellie establishing obstetrics. Laënnec advanced auscultation by stethoscope and Auenbrugger chest percussion. Perhaps most significantly, Morgagni had published his De Sedibus, which established organ-based pathology over the humoral theory in 1761.
America was a backwater of medicine at the inception of its formation (1). The first medical school in the United States was established at the College of Philadelphia (later the University of Pennsylvania) by William Shippen Jr. and John Morgan in 1765 (2,3). Military medicine at that time was more definite as it often consisted of tourniquet use, removing bullets, and performing amputations—but without sterile procedures or anesthetics. Hygiene and public health measures would become more prominent in following decades.
U.S. military medicine began in 1775 when the Second Continental Congress established the Continental Army’s Hospital Department. Dr. Benjamin Church was appointed the first Director General of Hospitals and Chief Physician, but was later dismissed for treason (4). Morgan, then Shippen, succeeded Church as Director Generals of Hospitals of the Continental Army. A permanent and continuous medical department was not established until 1818 and physicians would not generally become military officers until 1947.
Dr. Joseph Lovell (1788-1836) became the first ranked medical director and thus first so-named Army Surgeon General in 1818 (5). He established the Library of the Surgeon General in 1836, when he acquired some books and journals for his office, which would eventuate in the National Library of Medicine.
The Army Medical Museum and the Surgeon General’s Library
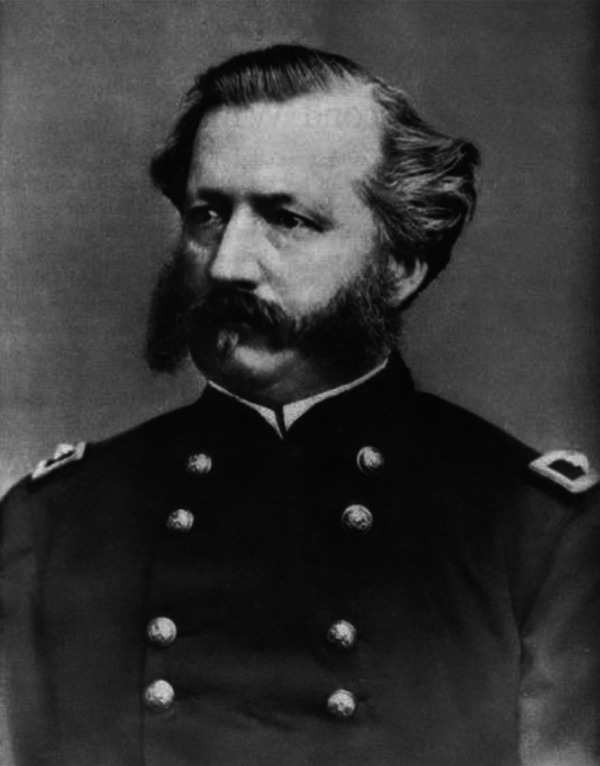
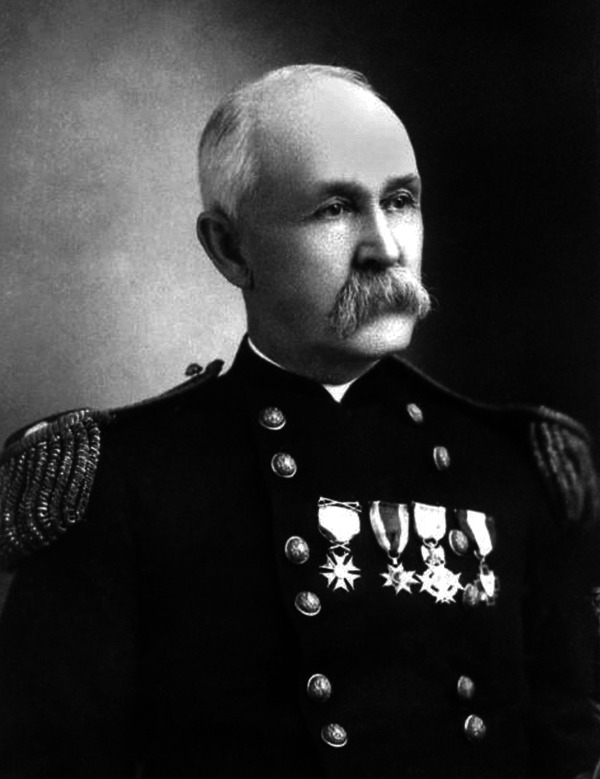
In 1862, 33-year-old Brigadier General William Alexander Hammond (1828-1900) (6,7) was appointed the 11th Surgeon General of the US Army by President Abraham Lincoln, over the advice of his Secretary of War, Edwin Stanton. Hammond had previously served in the Army in the West, but had rejoined with the outbreak of the war less than a year before his appointment. He had been recognized for his research by the American Medical Association in 1857. As he began, Congress issued a reorganization of the Medical Department of the Army. Hammond was a visionary and responsible for many accomplishments. He raised the qualifications for admission into the Medical Corps, increased the number of hospitals and succeeded in placing all general hospitals under his supervision. He promoted Major Jonathan Letterman (1824-1872) and supported his creation of an ambulance service. Particularly, Hammond was responsible for a new and vastly enlarged medical supply table and the provision of hospital clothing for patients. He would eventually write the first American textbook on neurology.

BG William A. Hammond (1828-1900)
As General Hammond took command, he was faced with the task of understanding the battlefield injuries and diseases that confronted the Army (8). He issued Circular No. 2, on May 21, 1862, to seek knowledge of the field conditions. He established a Registry of Sick and Wounded and later a Registry of Surgical Operations from military hospitals. Hammond ordered Assistant Surgeon Joseph Janvier Woodward (1833-1884) of the Army of the Potomac and Brigade Surgeon John Hill Brinton (1832-1907) of the Mississippi Volunteers to report for special duty. In his Circular No. 5, 1862, Hammond assigned Dr. Woodward to write the medical portion and Dr. Brinton to write the surgical portion of a medical history of the war.
Almost as an afterthought, the circular announced in its closing paragraph a proposed Army Medical Museum (AMM), which would eventuate in the Armed Forces Institute of Pathology (AFIP), now the National Museum of Health and Medicine (NMHM), and directed medical officers to diligently collect and forward:
all specimens of morbid anatomy, surgical, and medical, which may be regarded as valuable; together with projectiles and other foreign bodies removed, and such other matters as may prove of interest in the study of military medicine or surgery.
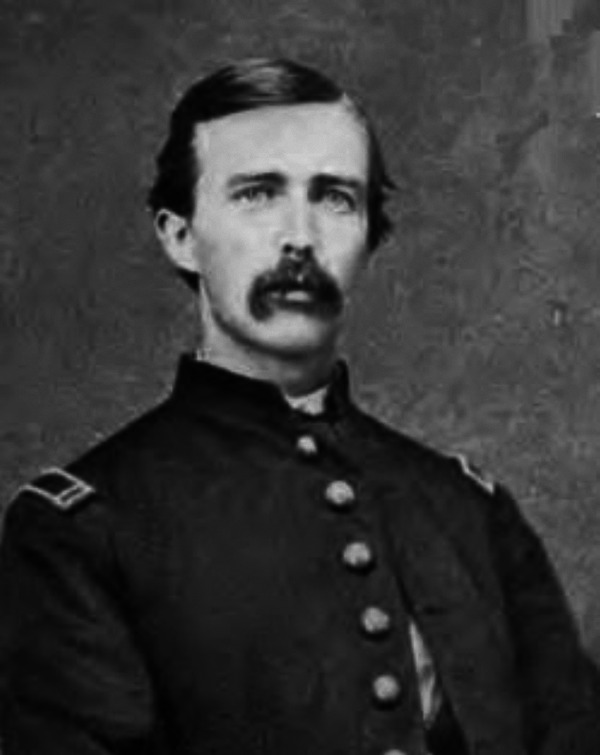
Major John Hill Brinton (1832-1907) (9), who was on General Ulysses Grant’s medical staff during his western campaign, was named the first curator of the museum. Brinton began a medical collection with three dry specimens and placed them on a shelf in his office. By 1863, over 1300 specimens had been collected. Of the nearly 1000 surgical specimens collected, all but a handful were of gunshot wounds. By 1865, the collection would grow to over 7600 specimens.

MAJ John H. Brinton (1832-1907)
Hammond, like his predecessor, clashed with the autocratic Secretary Stanton. Stanton eventually relieved General Hammond of duty, ordered him to New Orleans, Louisiana and placed Joseph K. Barnes in charge of the Surgeon General’s office. General Hammond demanded that he be restored to his office or be tried by court-martial. Hammond was court-martialed over his banning of mercury-laden calomel, but was acquitted. However, this finding was disapproved and a reconsideration directed which resulted in a verdict of guilty and dismissal from the Army in 1864. In 1878, at the height of his popularity, he campaigned for his vindication. By an act of Congress, he was restored to the Army with his full rank in 1879. His brief tenure of less than two years as the Army Surgeon General may have been the most impactful of any Surgeon General.
Brigadier General Joseph K. Barnes (1817-1883) became the acting Surgeon General and then succeeded Hammond as the Army Surgeon General in 1864. He would serve for 18 years and carried forth many of the initiatives that had begun with Hammond. He declared that “the Army Medical Museum continues to increase in value, and is already one of the most instructive pathological collections in the world.” It is significant that he described it as a pathological collection.
BG Joseph K. Barnes (1817-1883)
After Hammond’s dismissal, Major Brinton successfully overcame a push to scuttle the museum. In 1863, Brinton, Woodward, and two others proposed to establish a postgraduate medical school at the museum, but the proposal was quashed by Secretary Stanton; nonetheless it came to fruition 30 years later. Brinton was also controversially relieved of duty only one month after Hammond and reassigned.
Brinton’s assistant, Assistant Surgeon George Alexander Otis (1830-1881) (10,11) succeeded Brinton as curator of the museum in October 1864 and served until his death in 1881. Otis took over the surgical collections and photographic sections of the museum from Brinton, while Woodward continued his curation of the medical and microscopic sections—the focus of the medical section was on the statistical analysis of injuries and disease.
The final quarter of the 19th century was a blossoming of pathology (12). Rudolf Virchow had written his Cellular Pathology in 1858. Louis Pasteur and Robert Koch performed their studies that supported the germ theory at this time. The familiar hematoxylin and eosin stain was described by Wissowsky in 1876 (13,14). The first stain for microorganisms, the Ziehl-Nielsen stain was described in 1882 and 1883 (the Brown-Brenn’s Gram stain was not described until 1931). The microscope was the principal tool of this age. In keeping with this age, research strengths at the AMM were developed in microscopy, histochemistry, and photomicrography. From 1864, Woodward (15 -18) and his museum colleague, Edward Curtis (1838-1912) (19) perfected the technique of photomicrography, particularly through improvements of the objective lenses of microscopes, and Woodward pioneered use of aniline dyes for staining thin sections of tissues.
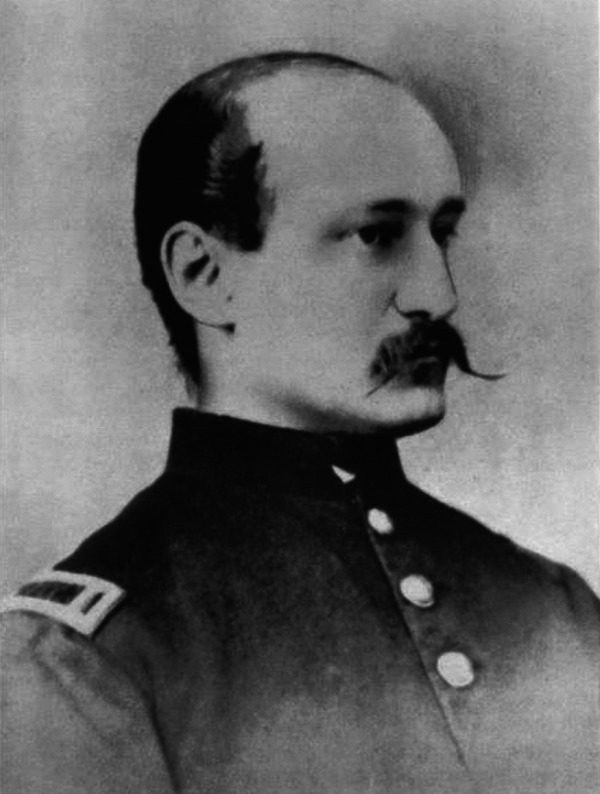
On April 15, 1865, Woodward and Curtis performed the autopsy of President Lincoln, who was shot the previous evening. They described the entrance wound, traced the bullet track through the left cerebral hemisphere into the white matter above the left corpus striatum, and noted that both orbital plates were fractured. On April 29, 1865, they performed the autopsy on John Wilkes Booth, which has remained controversial (20).
LTC Joseph J. Woodward (1833-1884)
At the conclusion of the war, Woodward and Otis began writing the Medical and Surgical History of the War of the Rebellion, which was eventually published in six volumes and 6000 pages from 1870 to 1883 (21,22). Otis died in 1881 and Major David Low Huntington (1834-1899) became the third curator of the museum and completed the remaining surgical volume; he was also placed in charge of the Surgeon General’s library. When Woodward died in 1884, Major Charles Smart was appointed his successor and completed the final volume of the medical section.
The collections grew enormously from the four years of Civil War activities. The museum began in a room of the Surgeon General’s office, then moved three times before settling into Ford’s Theatre in 1866 (which had been closed since the President’s assassination). The museum was opened to the public in 1867 and drew 6000 visitors by the end of the year.
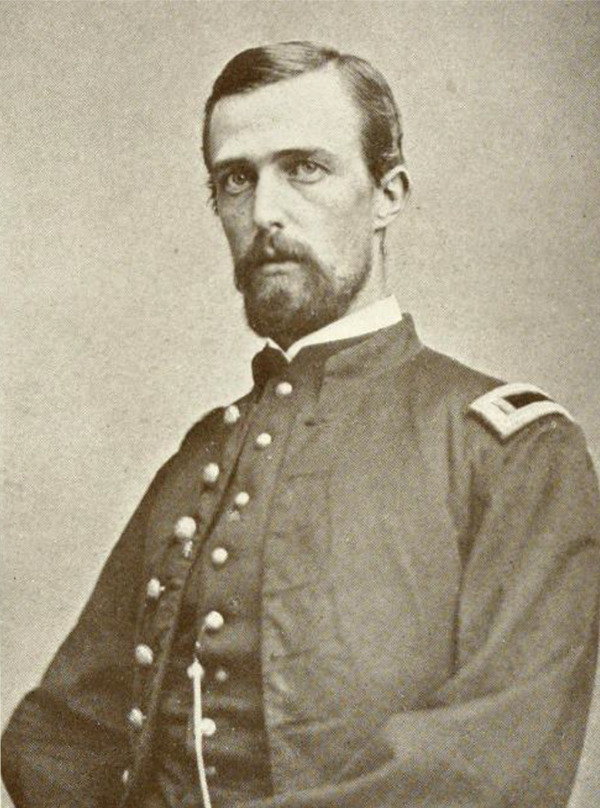
MAJ Edward Curtis (1838-1912)
Major John Shaw Billings (1838-1913) (23,24) was assigned the directorship of the Surgeon General’s Library in about 1867 and would continue his directorship to 1895. He succeeding building it into the largest medical book collection in America. When the card catalog system proved insufficient, Billings established the indexing system in 1879 that would become known as the Index Medicus.
LTC John S. Billings (1838-1913)
On September 20, 1881, Woodward and Dr. Daniel S. Lamb conducted the autopsy of President James A. Garfield, who died the previous evening. Lamb had worked at the museum starting 1865, became it’s pathologist in 1892, and remained in that position until his retirement in 1920. On July 2, 1881, Garfield had been shot twice, which included a grazing wound of the posterior left shoulder and a penetrating wound of the right lower back. Garfield died 80 days later from sepsis after repeated probings of the wound. They found the bullet lodged in the lumbar spine, fractures of the 11th and 12th ribs, multiple abscesses, right lower lobe pneumonia, and a ruptured splenic artery aneurysm. On June 30, 1882, Dr. Lamb performed the autopsy on Charles Guiteau, Garfield’s assassin.
In 1883, the AMM and the Surgeon General’s library were consolidated into one division and Major Billings was named curator and librarian. From November 1887 through February 1888, the museum moved onto the national mall into a new building designed by Adolph Cluss, affectionately called “Old Red Brick,” a site now occupied by the Hirschhorn Museum. During his tenure, Billings also headed the US Census Bureau’s division of Vital Statistics and supervised the 1880 and 1890 US Censuses. Prior to his departure from the Army, he designed the original buildings of the new Johns Hopkins Hospital which opened in 1889 and recruited the initial faculty, including William Welch and William Osler. He went on to become the first director of the New York Public Library.
In 1893, Brigadier General George Miller Sternberg (1838-1915) (25,26), known as the father of American bacteriology, became the 18th Surgeon General and would serve until 1902. Sternberg’s first act as Surgeon General was to establish a postgraduate Army Medical School (AMS), 30 years after it was first proposed. It is often considered to be the first school of public health and preventive medicine (although Johns Hopkins claims their 1916 School of Public Health should get this credit). The four-month school was to train physicians in the art of military medicine. The AMM staff were to serve as the lecturers. Then Captain Walter Reed (1851-1902) (27), the only military medical officer who had been trained by Dr. William Welch at Johns Hopkins, was brought in as the fifth curator of the AMM, which would function as the schoolhouse. Reed was appointed professor of bacteriology and clinical sanitary microscopy, and director of the pathological laboratory in the new AMS; he also served on the faculty of the National Medical College—later known as the George Washington University Medical School.
BG George M. Sternberg (1838-1915)
Reed would become Sternberg’s protégé in laboratory research and his field investigator of disease outbreaks. In 1899, Reed headed the Typhoid Fever Commission and, in 1900, the Yellow Fever Commission. Reed nor Sternberg believed Finlay’s mosquito theory, but Reed proved the mosquito vector when he was able to transmit the fever after the correct incubation period. Both Sternberg and Reed are thought of as infectious disease specialists, but they are more properly considered pathologists, their principal tool was the microscope, they performed extensive laboratory studies, and they studied disease. (They should be distinguished from another Reed-Sternberg pathology pair of the same period: the Reed-Sternberg cell of Hodgkin’s Lymphoma was described by Dorothy Reed Mendenhall in 1902 and Carl Sternberg in 1898.) Major William Cline Borden (1858-1934) served on the faculty with Reed and was the hospital commander at the Army General Hospital at the Washington Barracks (later Fort Leslie J. McNair). In 1902, when Major Reed developed appendicitis, Borden performed the appendectomy, but Reed developed peritonitis and died; this was Borden’s only such fatality and he was devastated.

MAJ Walter Reed (1851-1902)
In 1904, Major Borden proposed building a new hospital to replace the Army General Hospital at the Washington Barracks and colocating the AMM and AMS (then in the Old Red Brick building on the mall) in a single medical complex (28). He began to lobby congress the following year with partial success. The new Walter Reed General Hospital opened in 1909, with Borden as the first Commander. In 1910, the AMS moved out of the museum, but was not colocated with the hospital until 1923, when by order of General John J. Pershing, it was renamed the Walter Reed Army Institute of Research. In 1951, the entire complex was renamed the Walter Reed Army Medical Center (WRAMC). Later, in 1955, when the AFIP was colocated onto the base, Major Borden’s Dream was complete, except for the library, that in 1956 became the National Library of Medicine, was transferred to the US Public Health Service, and was located on the grounds of the National Institutes of Health (NIH) and the AMM, which did not move to the WRAMC campus until 1968.
AMM “Old Red Brick”, Washington Mall, Washington, D.C. (1887-1968)
The Armed Forces Institute of Pathology
At the dawn of the 20th century, pathology was struggling to define itself. Autopsies had been the primary tool to study disease through the centuries, but in recent decades the microbe hunters had stolen the limelight (29). Surgical pathology had not yet established itself as an essential part of medical practice (30). The discipline was facing the real threat of splintering into autopsy, bacteriology, immunology, toxicology, histology, and so on. The International Academy of Pathology was founded in 1906 (from a meeting at the AMM), the American Society of Clinical Pathology in 1928, and the College of American Pathologists (CAP) in 1949. The first pathology board examination of the American Board of Pathology (ABP) was given in 1936.
The AMM desired to make use of its collections, which grew huge through World Wars I and II (WWI and WWII) (31). One use involved medical illustrations, which educated military officers and enlisted personnel and helped bring down disease in WWI to levels lower than battlefield casualties for the first time. It was also instrumental in understanding the use of gas in warfare. Major George Russell Callender and then Colonel James Earle Ash promoted a registry movement in the 1920s that continued for decades. Civilian specimens began to be added to the military collections. In 1921, a collaboration between the museum and the American Academy of Ophthalmology and Otorhinolaryngology resulted in the first registry. In 1929, the Army Surgeon General declared that the museum was to collect and permanently preserve tissue pathology specimens, and use them for education, consultation, and research. The American Registry of Pathology (ARP) was formed in 1930.
The public exhibition functions of the museum took a backseat to research on the registry collections and the institution became an ivory tower of diagnostic surgical pathology. In 1947, the development of an Atlas of Tumor Pathology, based on the collections, was conceived and then sponsored by the National Research Council and the National Cancer Institute. The first fascicles of the series were sold by the ARP in 1949. Thereafter, the institute staff played a critical role in standardization of pathologic diagnosis of tumors and the development of the International Histological Classification of Tumors series of the World Health Organization (32).
In 1942, the solicitation for pathologic specimens became a military mandate and the pathology staff grew to 20 from three prior to the war. The growing collection of specimens required new space, but although Congress initially appropriated funds in 1919 and 1922, plans were shelved first during the great depression and then again for WWII. In 1946, due to the broadening research mission, the AMML was renamed the Army Institute of Pathology (AIP). In 1947, the museum functions were moved out of Old Red, across Independence Avenue into Chase Hall, where it remained until 1960. In 1949, the AIP became the central laboratory of pathology for all of the Armed Forces, as well as the Veteran’s Administration, and was renamed the AFIP. Plans were again drawn up for a new building. In June 1950, when North Korean communists crossed the 38th parallel into the Republic of Korea, the National Security Resources Board specified the new building to be a bomb-resistant structure.
In 1955, the AFIP moved into its new eight-story, 70, 000 square-foot, permanent home, building 54 on the Walter Reed campus. The formal opening included a dedication by President Dwight Eisenhower. The building was designed in 1951 to house the U.S. President in case of an atom bomb attack (33). The building had no windows and the walls were 8-ft thick concrete. The main entrance was a steel vault door and a helipad was located nearby. Nuclear bombs became more powerful and the building was obsolete before it was finished; another building of its design was never built again. At that time, it had four major departments, the Department of Pathology, ARP, Medical Illustration Service, and the Medical Museum. Although other functions moved into the new facility, the museum remained on the mall and open to the public, until 1960, when, after a few more moves, it physically rejoined the AFIP in 1971. In 1988, the institute’s medical museum was renamed the NMHM in recognition of the fact that since its founding in 1862, it had been the only federal museum in the country devoted exclusively to medicine. The library moved to the NIH in 1956.
Armed Forces Institute of Pathology Directors
| 1 | 1949-1950 | Brigadier General Raymond O. Dart, MC, USA |
| 2 | 1950-1955 | Brigadier General Elbert DeCoursey, MC, USA |
| 3 | 1955-1959 | Captain William M. Silliphant, MC, USN |
| 4 | 1959-1963 | Colonel Frank M. Townsend, MC, USAF |
| 5 | 1963-1967 | Brigadier General Joseph M. Blumberg, MC, USA |
| 6 | 1967-1971 | Captain Bruce H. Smith, MC, USN |
| 7 | 1971-1973 | Colonel Robert W. Morrissey, MC, USAF |
| 8 | 1973-1976 | Colonel James L. Hansen, MC, USA |
| 9 | 1976-1980 | Captain Elgin C. Cowart, MC, USN |
| 10 | 1980-1984 | Colonel William R. Cowan, MC, USAF |
| 11 | 1984-1987 | Colonel Robert R. McMeekin, Jr., MC (MD, JD), USA |
| 12 | 1987-1991 | Captain Robert Karnei, MC, USN |
| 13 | 1991-1995 | Captain Vernon W. Armbrustmacher, MC, USAF |
| 14 | 1995-1999 | Colonel Michael J. Dickerson, MC, USAF |
| 15 | 1999-2003 | Captain Glenn Wagner, MC, USN |
| 16 | 2003-2007 | Colonel Renata B. Greenspan, MC, USA |
| 17 | 2007-2011 | Dr. Florabel G. Mullick (civilian) |
AFIP Bdg 54, WRAMC Washington, D.C. 1955-2011
Forensic Pathology at the AFIP
Since its inception during the Civil War, the institute had significant material involving battlefield injuries and other trauma and accordingly had developed expertise in the pathology of trauma, however, with some exceptions, it was not a particular focus during its seminal years of development. In 1935, would ballistic studies (rifle bullets) were conducted by Col George R. Callender and Maj R. W. French of the AMM staff (34). Later studies were conducted at Camp Lejeune for sleeveless body armor, which eventuated in a 1951 joint Navy-Army mission to Korea led by Commander John S. Cowan, MC, USN, and Lieutenant Colonel Robert H. Holmes, MC, USA to assess the effectiveness in combat (35).
In 1877, Massachusetts first created a medical examiner position and New York City (NYC) created the first modern medical examiner office in 1918. Charles Norris (1867-1935) in NYC, George Burgess Magrath (1870-1938) in Boston, and William Scott Wadsworth (1868-1955) in Philadelphia were the first generation of American physicians employed full-time in medicolegal practice (36). Medical examiners were physicians of varying backgrounds and expertise with little or no training. By the 1920s, autopsy pathology was differentiated from other anatomic pathology areas by academic programs. The term forensic pathology was first coined in 1942 as more focused on medicolegal death investigation than legal medicine or medical jurisprudence (37).
George Burgess Magrath was the Suffolk County (Boston) Medical Examiner and Instructor of Legal Medicine at Harvard (38,39). Frances Glessner Lee (1878-1962) (40,41) and the Rockefeller Foundation funded Alan Richards Moritz (1899-1986) (42,43) to succeed McGrath and to establish a Department of Legal Medicine at the Harvard Medical School in 1937, the first such department in America. Moritz was succeeded by Richard Ford (1915-1970) (44,45) in 1949. Students came from Boston University, Tufts, and Harvard. Graduates included Lester Adelson (1914-2006), Russell Fisher (1916-1984), and Joseph Spelman (1919-1971). The program eventually closed in 1967, William J. Curran continued his lectureships (46).
The New York University Medical School (NYU), which was closely associated with the NYC Medical Examiner’s Office, established the NYU Department of Forensic Medicine in 1939. Dr. Charles Norris (47), the Chief Medical Examiner for NYC, was appointed the department head, Dr. Harrison Stanford Martland (1883-1954) (48), the Chief Medical Examiner for Newark, New Jersey, was an Associate Professor, and Alexander Oscar Gettler (1883-1968) was a Professor of Toxicology. Norris, prior to his becoming the first NYC Medical Examiner, had been the director of Bellevue Hospital’s pathology laboratory replacing Dr. William Henry Welch (1850-1934) after Welch left to become the first dean of the Johns Hopkins Medical School. Norris, as head of the NYU program would be succeeded by Martland (1883-1954) and then Dr. Milton Helpern (1902-1977). Students came from Cornell, Columbia, and Harvard. Graduates of the program included Milton Helpern, Charles P. Larson, and Michael Baden.
Later, after Dr. Moritz had returned to Cleveland in 1949 as the head of pathology for the Western Reserve University (WRU), in 1952, his protégé, Dr. Lester Adelson (49), as deputy to Coroner Dr. Samuel R. Gerber (MD, JD) (1898-1987), began a program of legal medicine at WRU.
Since 1953, the AFIP put on a postgraduate course in Forensic Pathology, designed primarily for pathology residents. Since 1959, the AFIP put on a Forensic Sciences Symposium every two to three years. Lectures were also conducted at the International Police Academy, for the Seminar on Homicide Investigation by Harvard Medical School, and at meetings of the American Academy of Forensic Sciences.
From the mid 1950s, the CAP, through Charles Phillip Larson (1910-1984) (50), and the American Medical Association (AMA), through Richard Ford, pressed the ABP for recognition of the subspecialty of forensic pathology (51). The ABP had recognized anatomic and clinical pathology in 1936, neuropathology in 1948, medical microbiology in 1950, chemical pathology in 1951, and hematopathology in 1955. The ABP recognized forensic pathology in 1956, Moritz was elected a trustee to the ABP in 1958, and the first board certification test was offered in 1959.
As the AFIP moved into its new home in 1955, the institution was organized into four divisions: 1) Department of Pathology, 2) the ARP, 3) Medical Illustration Services, and 4) the AMM.
A Forensic Pathology Registry was established through the sponsorship of the CAP in 1958 as a component of the ARP (52,53). The Division of Military Environmental Pathology was created in 1959 by the new Director, Colonel Frank M. Townsend, USAF, MC (1914-2001), who had a strong interest in aerospace and aviation pathology. The Division contained the Forensic Pathology, Aerospace Pathology, and Toxicology branches. Col Edward Harold Johnston, MC, USA (1924-2015), was the first Chief of the Military Environmental Pathology Division, as well as the Chief of the Forensic Pathology Branch, which was also staffed by Major Pierre Antoine Finck, MC, USA (1923-2018) (54) and Major Frank Wilson Kiel, MC (MD, JD), USA (1930-) (55). A Wound Ballistics Branch was added a few years later and was headed by Finck. Aviation Pathology, first headed by Captain Vernon Albert Stembridge, MC, USAF (1924-2000), involved investigations of aircraft mishap fatalities and would eventually be subsumed by the AFMES (56,57). In addition to an aerospace environment, an undersea environment was explored particularly with consultations with Captain Charles Wesley Shilling.
In 1962, the CAP sponsored the first forensic pathology residency program approved by the ABP and the AMA’s Committee on Medical Education and Hospitals at the AFIP, rather than in NYC, Boston, or Cleveland, as it was thought that the availability of pathologists in military installations would provide applicants for the forensic training (51, p. 82). Navy Commander Charles J. Stahl, III, MC, USN (1930-2016) (58 -60) was the first resident and completed the residency in 1963 (which included some training with Russell Fisher in Baltimore). In 1968-69, Major Richard Coe Froede, MC, USAF (1929-2011) (61,62) would also receive his forensic pathology training through this program.
In 1965, after a tour in Guam, Captain Stahl returned to head the Forensic Pathology Division of the AFIP, but by that time Finck and Kiel had re-stationed to Vietnam, and his only staff were a military police officer, a secretary, and a yeoman. Dr. Stahl became the Chief of the Division of Military Environmental Pathology in 1967. Brigadier General Joseph M. Blumberg, MC, USA (1909-1984) who was the AFIP Director from 1963 to 1967, later became board-certified in forensic pathology. The division was later renamed the Division of Forensic Sciences, and following a reorganization of the AFIP in 1974 was again renamed as the Department of Forensic Sciences. Lieutenant Colonel Froede succeeded Captain Stahl as the Chief of the Division of Forensic Pathology in 1968. By 1975, the Department had become the largest in the Institute, with not only the Forensic Pathology, Aerospace Pathology, Toxicology branches but also Accident Pathology, Underwater Pathology, Legal Medicine, and a group headed by Dr. Nelson Irey studying tissue reactions to drugs. Dr. Johnston, Stahl, and Froede established the AFIP as the center of forensic pathology for the military.
During this time, a Master’s program was established in conjunction with the George Washington University Department of Forensic Sciences for pathologists, investigators, and lawyers. This program produced significant leadership in the military for several years, including Roy Hazelwood who later helped establish the Federal Bureau of Investigation’s (FBI’s) Behavioral Sciences Unit.

COL Ed Johnston 1st AFIP FP Chief (1959-65)

CAPT Charlie Stahl, III 2nd AFIP FP Chief (1965-1974) 2nd AFME (1992-96) NAME Pres (1993-94)

Col Dick Froede 3rd AFIP FP Chief (1974-76) 1st AFME (1988-92) AAFS Pres (1989-90)
The Department of Forensic Pathology primarily reviewed military autopsy reports from the field as well as civilian consultations. The Vietnam War (1955-75) was an unconventional war compared to the WWI or Korea and the department saw deaths from punji sticks and fraggings. The only forensic pathologists in theater were Colonel Kiel, who commanded the 406th Army Medical Laboratory at Camp Zama, Japan, and Colonel Finck, who commanded the 9th Medical Laboratory in Saigon. Some Army pathologists later became forensic pathologists, particularly those involved with the Wound Data and Munitions Effectiveness Team.
Important cases during this time include the 1963 assassination of President John F. Kennedy, the 1963 Thresher submarine implosion, the 1968 assassination of Senator Robert F. Kennedy, the 1968 My Lai Massacre involving the court-martial of Lieutenant William Calley, the 1967 deaths of astronauts Grissom, White, and Chaffee during a prelaunch test inside the Apollo 1 command module, the 1977 crash of two commercial jets in Tenerife in the Canary Islands, the 1978 Jonestown mass suicide, the 1979 Jeffrey MacDonald case, the 1985 Gander, Newfoundland crash, and the 1986 Space Shuttle Challenger disaster. Among the various forensic pathologists who rotated through the AFIP forensic pathology unit were Tom Canfield, Don Reay, Ed Donoghue, and Vincent DiMaio.
Armed Forces Institute of Pathology Chiefs of Forensic Pathology
| 1 | 1959-1965 | Colonel Edward H. Johnston, MC, USA |
| 2 | 1965-1974 | Captain Charles J. Stahl, III, MC, USN |
| 3 | 1974-1976 | Colonel Richard Froede, MC, USA |
| 4 | 1976-1982 | Robert Thompson, MC, USN |
| 5 | 1982-1985 | Jerry Spencer, MC (MD, JD), USN |
| 6 | 1985-1988 | Charles Ruehle, MC, USAF |
The Assassination of JFK
On November 22, 1963, President John Fitzgerald Kennedy was assassinated in Dallas, Texas, by Lee Harvey Oswald, who was shot by Jack Ruby two days later. President Kennedy was pronounced dead in the Parkland Memorial Hospital emergency room at 1:00 pm, an hour and half after the shooting. Dr. Earl F. Rose (1926-2012), the Dallas County Medical Examiner, had jurisdiction of the body. At the time, the homicide of a sitting president was not a federal crime. Dr. Rose, whose office was across the hall from the Trauma Bay, strode over when he heard that the president had been pronounced dead. A Secret Service Agent and the President’s personal physician told him that there was not time to perform an autopsy. Dr. Rose objected and an intense argument ensued. After the body was placed in a casket and was rolled down the hallway with Mrs. Kennedy at the side, Dr. Rose and a local police officer attempted to block the door, but were pushed aside by Kennedy’s aides. Dr. Rose later stated that he had stepped aside to not further exacerbate the tension (51, pp. 96-97, 63). Dr. Rose did later perform the autopsy of Oswald. The body was taken to Air Force One waiting at Love Field, where President Lyndon B. Johnson was sworn in, before the aircraft left for Washington.
At the request of the widow, the body was taken to the Bethesda Naval Hospital, because President Kennedy had been a naval officer. The autopsy was conducted that night, from about 8:00 pm to midnight, by Commander James J. Humes, Commander J. Thornton Boswell, the Pathology Chief, and Lieutenant Colonel Pierre Finck, Chief of the Wound Ballistics at the AFIP. Commander Humes was the senior ranking officer. Neither Humes nor Boswell had ever performed a forensic autopsy; Finck was board certified in forensic pathology and had experience with forensic autopsies. The room was crowded by eight other physicians (none forensic pathologists), three Secret Service agents, two FBI agents, and more than a dozen others were present at various times during the autopsy.
The autopsy has been criticized (64). The pathologists were under pressure to do the autopsy quickly. Dr. Humes believed he was merely to recover the bullet (51, p. 99). Due to family concerns, the autopsy was limited to the head and chest; the neck organs were not removed. The clothes were not examined. There was no communication with the doctors at the hospital. The documentation was inadequate. The report does not include measurements. The subsequent brain examination has been questioned. Two death certificates were issued by others not in attendance and they were in conflict.
In large part as a response to the botched forensic autopsy, the President’s Warren Commission (1963-64), Ramsey Clark Panel (1968), Rockefeller Commission (1975), House Select Committee on Assassinations (1978-79), Assassinations Records Review Board (1992-98) investigated the death, but the controversy surrounding the death continues to this day.
The Assassination of Robert Francis Kennedy
On June 5, 1968, Senator Robert Francis Kennedy (RFK), while campaigning for President, was shot as he was shaking hands with a busboy in the kitchen of a Los Angeles hotel. A busboy, Sirhan Sirhan, fired eight times with a 22-caliber revolver. One bullet struck Kennedy’s armpit, one struck his back, the fatal shot struck him in the head behind his right ear, and another bullet merely perforated his coat; some shots hit bystanders—all of whom survived. He laid on the floor for 17 minutes, before the ambulance arrived. At the hospital, he was rushed into the operating room, where neurosurgeons cleaned his wound for four hours. Nonetheless, 12 hours after the surgery, he was pronounced dead in the early hours of June 6th.
There were several witnesses in the room and the gunman was wrestled to the ground. He was seen to approach RFK from the front. Some witnesses noted that RFK’s head was turned to the left at the time of the shooting. Nonetheless, the location of the wound in the back of the head gave rise to suspicions of a second gunman.
The Kennedy family objected to an autopsy, claiming that the cause of death was obvious, and pressed to remove the body to Washington, but that was not to happen. Dr. Thomas T. Noguchi, did not want a repeat of the problems with the JFK autopsy, and called the Director of the AFIP for assistance (51, pp. 103-106). The AFIP sent Commander Charles Stahl, III, Assistant Chief of the Military Environment Division and Chief of the Forensic Pathology Branch and Colonel Pierre Finck, Chief of the Wound Ballistics, and Dr. Kenneth Earle, Chief of the Neuropathology Division.
Dr. Noguchi with the three AFIP pathologists performed what has been described as “the perfect autopsy (65).” The autopsy reports on the Kennedys have been published as a “Study in Contrast (66).”
Legislative Reactions
The JFK assassination brought out the fact that it was not a federal crime to kill the president. In 1965, Congress passed legislation to make it so. 18 U.S.C. §1751 makes it a federal crime, punishable by death, to kill, kidnap, or assault the President, President-elect, Vice President, or other person in succession, or an attempt to do so. The law declares that the FBI will investigate and that the state and local investigations and prosecutions are suspended, but “assistance may be requested of any Federal, State, or local agency, including the Army, Navy, and Air Force, any statute, rule, or regulation to the contrary notwithstanding.” In 1971, after the RFK assassination, Congress extended the criminal law to cover other federal officials. 18 U.S.C. §351 covers congressional, cabinet, and Supreme Court Justices, as well as major Presidential and Vice-Presidential candidates in a manner similar to that of the President and Vice-President. Although not specifically in the law, it was presumed that the AFIP would be the lead for the medicolegal death investigations.
The Armed Forces Medical Examiner System
The notion of an Armed Forces Medical Examiner System (AFMES) surfaced in the early days of forensic pathology. In a letter dated December 22, 1950, to AFIP Director Elbert DeCoursey, Dick Ford recommended that the federal government should develop their own medicolegal death investigation system, particularly “adapting this state system to the Armed Forces.” The Director expressed his desire to create a Division of Legal Medicine (51, p. 82).
The notion resurfaced a decade later. Dr. Dick Froede, reflecting in an interview about his experiences at the AFIP, stated:
DR. FROEDE: It was at this time that Dr. Stahl and I, probably over a cup of coffee one morning, decided that maybe we ought to have a medical examiner system.…So the seed was planted then. And it took a long time before it finally reached fruition.
Q: Why did you feel that a medical-examiner’s office was necessary?
DR. FROEDE:…to legitimatize the office. The Department of Forensic Sciences that sounded great. But it was not like my colleagues outside, who were running coroner’s offices or medical-examiner’s offices.…And I think, in the long run, it was proven to be very valuable and very true (62, pp. 459-460).
The official history of the AFIP states: “In 1968, Stahl and Froede also came up with the initial idea for what is now the Armed Forces Medical Examiner System. This plan came to fruition 20 years later when Froede returned to AFIP as the first armed forces medical examiner, with the charge of establishing the medical examiner system as a separate entity within the institute (31, p. 131).”
Dr. Jerry Spencer, in his review of the history of the AFMES, provided more detail:
There had been discussions for years on how to convert the Division (later the Department) of Forensic Sciences into a Medical Examiner System. Captain Stahl and Colonel Froede first proposed an Armed Forces Medical Examiner System in 1973. At that time, the proposal did not obtain support from the Department of Defense (67).
Dr. James L. Luke writes about his first tenure at the AFIP as a Distinguished Scientist, immediately after his leaving the D.C. Medical Examiner’s office in 1983:
Reviewing case files submitted after the fact to the AFIP for consultation prompted discussions with Dr. Jerry Spencer, the Department of Forensic Sciences chairman, Dr. Mike Clark and others to find a better way. I ended up writing a memorandum to the Director, Dr. Robert McMeekin, with a narrative outline for establishing an Armed Forces Medical Examiner System. I had no further input in the process and learned sometime later that the medical examiner concept had been discussed in a paper published in 1973 in U.S. Navy Medicine by Drs. Charlie Stahl, Dick Froede and Jim Zimmerly (68). Dick Froede became the first Armed Forces Medical Examiner in 1988, almost two years after I had left the department (69).
The notion of had clearly been percolating within federal circles and the AFIP leadership. Dr. Froede was brought back to the AFIP as a Distinguished Scientist in 1987 to set up and establish the AFMES:
DR. FROEDE: Then one day I was in Dr. McMeekin’s office, and he said, “How would you like to come back?
…But when he said come here and be a Distinguished Scientist for a couple of years, do some research and things like that, I had no idea that I would ever end up as the Armed Forces Medical Examiner at that time.
…So I came here in 1987. And one of the first things they asked me to do was to take a look at the new medical-examiners’ reg. that they were trying to put through. And I found a lot of things in there that needed some change. I spent a good number of hours down at the Pentagon with an Army colonel there and with the lawyers, trying to get these changes. That bit of paper gave whoever was sitting in that job a lot of responsibility and very little authority. We tried to change as much as we could, but it was very difficult, because if we changed too much, it would have to make the round-robin again and it’d be another five years before you’d get started again. Nobody was willing to go through this. Let’s start it up, let’s see how it works, and then let’s work from there.
…It was coming from…the criminal-investigating people. They were fed up with the hospital pathologist who was allowed to do a case, or wasn’t allowed to do a case: “You can’t do an autopsy, you’ve got surgicals.” And it was also coming a little bit from the outside: “It’s about time you people shaped up and got a medical-examiner system in the military.” There had been several cases over the years before where everybody got upset about it. Congress got upset about it. And so Congress sort of mandated that this thing be set up. Now when they mandated, they didn’t pass a law. If they had passed a law, we’d be on our way home right now without any problems. But they didn’t, so it became just a reg. And with that, everybody would be sniping at it (62, pp. 463-465).
Despite these words, in late 1988, Dr. Froede explicitly and repeatedly told the author upon his arrival that the AFMES was created specifically to prevent another JFK-like debacle and not for any rationale based upon military need.
With the support of the ASD(HA) Enrique Mendez and the three Surgeons General, the AFMES was formally established on March 8, 1988, by Department of Defense Directive 6010.16 (70). Previously the AFIP was merely a consultation service, with base commanders inconsistently grappling with the 2500 noncombat deaths, but the AFMES now had true jurisdiction over specified deaths and a system to deal with them (71 -73). The AFMES remains the only federal medical examiner office in the United States.
The directive was followed in 1999 by the enactment of 10 U.S.C. §1471 Forensic pathology investigations into federal law (74). The statutory language was written by Captain Jerry Spencer, after the 1996 death of US Secretary of Commerce, Ronald H. Brown, from a plane crash in Croatia. Brown had been under investigation for corruption. A punched out circular defect in the skull, thought to be from bolt protruding from the fuselage resembled a gunshot wound. The death was followed by many government cover-up and conspiracy theories.
Dr. Froede began his tenure as the first Armed Forces Medical Examiner on the day after his 59th birthday, May 2, 1988. Initially the Office of the Armed Forces Medical Examiner (OAFME) was unfunded and the AFIP had to absorb the costs and began with a staff of four forensic pathologists, CAPT Glenn Wagner, COL Charles Springate, Col Donald Wright, and Col William Gormley.
The Division of Forensic Toxicology, headed by Michael T. Smith, was responsible for drug testing in the military worldwide. Major Victor W. Weedn established DNA identification capabilities that included the Armed Forces DNA Identification Laboratory and a repository of DNA specimens from all service members and DOD civilians in harm’s way (AFRSSIR).
Although the AFIP was in Washington, DC, autopsies were performed at the Dover Port Mortuary in Dover, Delaware, 100 miles away. Among the first priorities was to build-up the capabilities of the Dover facilities for the anticipated mass casualties of the looming first Persian Gulf War. Fortunately, there were only 294 deaths of US military members during that war; all were autopsied and identified.
Early efforts of the OAFME included the investigations of Colonel William Higgins in 1988, the USS Iowa explosion in 1989, Operation Just Cause (Panama) in 1989, the ferry accident of the USS Saratoga crew in 1990, the USS Cole bombing in 2000, and the 9/11 Pentagon and Somerset terrorist hijackings of 2001, Operation Enduring Freedom (Afghanistan) beginning in 2001, and Operation Iraqi Freedom (Iraq) beginning in 2003. In 1992, Dr. Froede named his mentor, Dr. Charles Stahl, to be his successor.
Disestablishment of the AFIP
Congress began planning for the reduction of military bases following the buildup of the Cold War as early as 1949 and hundreds of bases and facilities were closed. Recognizing that various politicians representing the jurisdictions of military bases would interfere with continued reductions, the Defense Base Realignment and Closure (BRAC) Act of 1990 established an independent nine-member BRAC commission to continue the military reductions. Rumors of a BRAC closure of the WRAMC began circulating in the early 1990s. In 2005, the BRAC Commission recommended to the President the realignment of WRAMC with relocation of its “military relevant functions” to the National Naval Medical Center, Bethesda, Maryland. The AFIP, which was located on WRAMC, was to be disestablished. President George W. Bush approved the recommendation and notified Congress of his decision. A political struggle for its survival ensued, but a resolution in the House of Representatives to disapprove the recommendation failed to pass. The pathology community mourned the fate of the AFIP (75 -78).
The AFIP was finally closed on September 15, 2011. The AFIP’s tissue repository, the largest in the world, which included 55 million glass slides, 31 million paraffin blocks, and more than 500 000 wet tissue samples, were given over to a newly created Joint Pathology Center in Fort Detrick’s Forest Glen Annex in Silver Spring, Maryland. The NMHM also moved to the Forest Glen Annex.
The AFMES was transitioned from the AFIP to the Medical Research and Material Command and physically moved to a temporary quarters in Rockville, Maryland, before its permanent move to the Dover AFB, Delaware. The Dover Port Mortuary was established in 1955 and was replaced by the Charles C. Carson Center for Mortuary Affairs in 2003. For the 2011 move, a new facility covering 117 000 square feet on two floors, and costing US$52 million was designed for the AFMES and its components. On August 31, 2015, the AFMES was transferred from U.S. Army Medical Research and Development Command to the Defense Health Agency, where it remains today.
Armed Forces Medical Examiners
| 1 | 1988-1992 | Richard Froede (USAF, ret.) |
| 2 | 1992-1996 | Charles J. Stahl, III (USN, ret.) |
| 3 | 1996-2001 | Jerry Spencer (USN, ret.) |
| 4 | 2001-2002 | Colonel Abubakr Marzouk, MC, USAF |
| 5 | 2002-2012 | Captain Craig Mallak, MC, USN |
| 6 | 2012-2016 | Colonel Ladd Tremaine, MC, USA |
| 7 | 2016- | Colonel Louis Finelli, MC, USA |
OAFME Dover AFB Dover, Delaware 2011-
Conclusion
The creation of a federal medical examiner system, the AFMES, in 1988, occurred long after state and local medicolegal death investigation systems were established. A need had always existed, but remained unrecognized. The foundation upon which the AFMES was established was incremental, accidental, and by force of personalities, but yet progressive and inevitable. Nonetheless, it took a fiasco, the botched autopsy of JFK, to finally trigger higher authorities to formally establish the AFMES. Since, its creation, the AFMES has clearly proven its worth.
Acknowledgments
The author thanks Adrianne Noe of the National Museum of Health and Medicine and her staff, especially Laura E. Cutter, for fact checking parts of this article and for input, as well as to COL Louis Finelli, MC, USA, CAPT Glen Wagner, MC, USN, ret., CDR Edward Donoghue, MC, USN, ret., CAPT Edward Reedy, MC, USN, ret, COL Thomas M. Canfield, USA, ret., and Dr. James Luke, for their review, input, and service.
Biography
Victor W. Weedn, MD, JD, George Washington University, Washington, DC, USA
Professor, Dept of Forensic Sciences
Footnotes
Disclosures & Declaration of Conflicts of Interest: The author has no conflicts of interest and no disclosures to make.
Financial Disclosure: The author has no financial disclosures to make.
References
- 1. Shyrock RH. Eighteenth century medicine in America. Proc Am Antiquarian Soc. 1950;59(2): 275–292. https://www.americanantiquarian.org/proceedings/44807198.pdf (accessed 24 July 2020). [Google Scholar]
- 2. Flexner A. Medical education in America: rethinking the training of American doctors. The Atlantic. June, 1910 https://www.theatlantic.com/magazine/archive/1910/06/medical-education-in-america/306088/ (accessed 24 July 2020).
- 3. The first American medical school: the formative years. Lancet. 2015;385(9981):1940–1941. doi:10.1016/S0140-6736(15)60950-3 [DOI] [PubMed] [Google Scholar]
- 4. Gillett MC. The Army Medical Department, 1775-1818. U.S. Army Center of Military History. U.S. Government Printing Office; 1981. https://history.amedd.army.mil/booksdocs/rev/gillett1/default.html (accessed 24 July 2020). [Google Scholar]
- 5. Craig SC. “Some System of the Nature We Have Here Proposed”: Joseph Lovell’s Remarks on the Sick Report, Northern Department, US Army, 1817 and the Rise of the Modern. US Army Medical Department, Borden Institute; 2015. https://www.cs.amedd.army.mil/FileDownloadpublic.aspx?docid=4924587d-a69d-49f2-954e-a0772d31cc2d (accessed 24 July 2020). [Google Scholar]
- 6. Henry RS. The Armed Forces Institute of Pathology: Its first century 1862-1962. Office of the Surgeon General, U.S. Government Printing Office; 1964. https://archive.org/details/TheArmedForcesInstituteOfPathology-ItsFirstCentury/page/n2 (accessed 24 July 2020). [Google Scholar]
- 7. William A. Hammond, Surgeons General website, Office of Medical History. U.S. Army Medical Department; Undated https://history.amedd.army.mil/surgeongenerals/W_Hammond.html (accessed 24 July 2020). [Google Scholar]
- 8. Devine S. Learning From the Wounded: The Civil War and the Rise of American Medical Science. UNC Press; 2014. http://www.civilwarmed.org/army-medical-museum/ (accessed 24 July 2020). [Google Scholar]
- 9. Brinton JH. Personal Memoirs of John H. Brinton: Civil War Surgeon, 1861-1865. Southern Illinois University Press; 1996. [Google Scholar]
- 10. Barnes JK. George alexander Otis. Edinb Med J. 1881;26(10):956–957. [Google Scholar]
- 11. Otis GA. Notes on the contributions of the Army Medical Museum, Feb. 7, 1878. Scientific and Historical Reports: Records of the Record and Pension Office, 1814-1919, File A, Entry 41, RG 94, NARA. Undated.
- 12. Long ER. A History of Pathology. Dover Publications, 1965. [Google Scholar]
- 13. Coleman R. The impact of histochemistry—a historical perspective. Acta Histochemica. 2000;102(1):5–14. doi:10.1078/0065-1281-00542 [DOI] [PubMed] [Google Scholar]
- 14. Riva MA, Manzoni M, Isimbaldi G, Cesana G, Pagni F. Histochemistry: historical development and current use in pathology. Biotechnic Histochemistry. 2014;89(2):81–90, doi:10.3109/10520295.2013.822559 [DOI] [PubMed] [Google Scholar]
- 15. Billings JS. Memoir of Joseph Janvier Woodward, 1833-1884. Nat Acad Sci. 1885:23:295–307. http://www.nasonline.org/publications/biographical-memoirs/memoir-pdfs/woodward-joseph-j.pdf. Biogr Mem Nat Acad 1886; 2:295-307 (accessed 24 July 2020). [Google Scholar]
- 16. Zimmerman LE. William Thomson and Joseph Janvier Woodward. History of Ophthalmology. Documenta Opthalmologica, 89 1995:39–43. Volume 7 doi:10.1007/978-94-011-0127-1_5 [DOI] [PubMed] [Google Scholar]
- 17. Woodward JJ. On the use of aniline in histological researches; with a method of investigating the histology of human intestine, and remarks on some of the points to be observed in the study of the diseased intestine in camp fevers and diarrhoeas. Am J Med Sci. 1865;49:106–118. https://babel.hathitrust.org/cgi/pt?id=uc1.c057905853&view=1up&seq=17&size=125 (accessed 24 July 2020). [Google Scholar]
- 18. Gage SH. Microscopy in America (1830-1945). Trans Am Micros Soc. 1964;83(4 supp):1–25. doi:10.2307/3224849; https://www.jstor.org/stable/3224849 [Google Scholar]
- 19. Echols M, Arbittier D. Edward Curtis, M.D., Arbittier museum of medical history. 2019. http://www.medicalantiques.com/civilwar/Medical_Authors_Faculty/Curtis_Edward.htm (accessed 24 July 2020).
- 20. Spiegel AD. Dr. John Frederick May and the identification of John Wilkes Booth’s body. J Community Health. 1998;23(5):383–405. https://link.springer.com/article/10.1023/A:1018702006867 (accessed 24 July 2020). [DOI] [PubMed] [Google Scholar]
- 21. The medical and surgical history of the war of the rebellion, 1861-65. Prepared under the direction of Surgeon General United States Army, Joseph K. Barnes. 6 volumes, U.S. Government Printing Office 1870–1888. https://archive.org/details/medicalsurgical32barnrich/page/n6
- 22. Rhoades ER. Photographic atlas of civil war injuries: photographs of surgical cases and specimens. Otis Historical Archives. JAMA. 1977;277(6):499 doi:10.1001/jama.1997.03540300067037 [Google Scholar]
- 23. Budreau LM. John Shaw Billings. In: Marble S, ed. Builders of Trust: Biographical Profiles from the Medical Corps Coin Borden Institute; 2011. https://www.cs.amedd.army.mil/borden/FileDownloadpublic.aspx?docid=beafb2f3-ac16-4711-a596-b3641388f535 (accessed 24 July 2020). [Google Scholar]
- 24. Millan W. Curriculum vitae optimum. Mary School Med Bull. 2014;99(3):16–17. [Google Scholar]
- 25. Craig SC. In the Interest of Truth: The Life and Science of Surgeon General George Miller Sternberg. Borden Institute; 2013. https://www.cs.amedd.army.mil/borden/FileDownloadpublic.aspx?docid=d5de0448-6e29-4083-828d-02ced2f538e4 (accessed 24 July 2020). [Google Scholar]
- 26. Prior RM. George Miller Sternberg. In: Marble S, ed. Builders of Trust: Biographical Profiles from the Medical Corps Coin Borden Institute; 2011. https://www.cs.amedd.army.mil/borden/FileDownloadpublic.aspx?docid=beafb2f3-ac16-4711-a596-b3641388f535 (accessed 24 July 2020). [Google Scholar]
- 27. Pierce JR. Walter Reed. In: Marble S, ed. Builders of Trust: Biographical Profiles from the Medical Corps Coin Borden Institute; 2011. https://www.cs.amedd.army.mil/borden/FileDownloadpublic.aspx?docid=beafb2f3-ac16-4711-a596-b3641388f535 (accessed 24 July 2020). [Google Scholar]
- 28. Standlee MW. Borden’s Dream: The Walter Reed Army Medical Center in Washington, D.C. The Borden Institute; 2009. https://www.cs.amedd.army.mil/borden/bookDetail.aspx?ID=518ebd44-f542-4bc3-a9b1-17027cd472ae&pageTitle=Borden's%20Dream:%20The%20Walter%20Reed%20Army%20Medical%20Center%20in%20Washington,%20DC (accessed 24 July 2020). [Google Scholar]
- 29. De Kruif PH. Microbe Hunters. Harcourt; 1926. [Google Scholar]
- 30. Johnson JA. Speaking for the dead: forensic scientists and American justice in the twentieth century [PhD dissertation]. Univ of Penn; 1992. . Proquest #9235156.
- 31. Stone P. Legacy of Excellence: The Armed Forces Institute of Pathology, 1862-2011. Borden Institute; 2011; p. 131 https://www.cs.amedd.army.mil/borden/bookDetail.aspx?ID=1229ffa5-9f33-412d-b476-1a52cb40f4a8&pageTitle=Legacy%20of%20Excellence:%20The%20Armed%20Forces%20Institute%20of%20Pathology,%201862-2011 (accessed 24 July 2020). [Google Scholar]
- 32. Sobin LH. The international histological classification of tumours. Bull World Health Org. 1981;59(6):813–819. [PMC free article] [PubMed] [Google Scholar]
- 33. Building a bombproof institute. The devil of history. May 26, 2015 https://devilofhistory.wordpress.com/2015/05/26/building-a-bombproof-institute/ (accessed 24 July 2020).
- 34. Callender GR, French RW. Wound ballistics: studies in the mechanism of wound production by rifle bullets. Military Surg. 1935;77(1):177–201. [Google Scholar]
- 35. Holmes RH, Enos WF, Beyer JC. Medical aspects of body armor used in Korea. JAMA. 1954;55(3):1477–1478. [DOI] [PubMed] [Google Scholar]
- 36. Johnson J. Coroners, corruption, and the politics of death: forensic pathology in the United States In: Clark MP, Crawford C, eds. Legal Medicine in History. Cambridge Univ Press; 1994. Chapter 11. [Google Scholar]
- 37. Moritz AR. Need of forensic pathology for academic sponsorship. Arch Path, 1942;33:382. [Google Scholar]
- 38. Tyre W. George Burgess Magrath: A Tribute. Glessner House; 2018. https://www.glessnerhouse.org/story-of-a-house/2018/12/11/george-burgess-magrath-a-tribute (accessed 24 July 2020). [Google Scholar]
- 39. George Burgess Magrath (1870-1938). Center for the history of medicine at Countway library. Undated https://collections.countway.harvard.edu/onview/exhibits/show/corpus-delicti/george-burgess-magrath (accessed 24 July 2020).
- 40. Miller LJ. Frances Glessner Lee: brief life of a forensic miniaturist: 1878-1962. Harvard magazine. Sept-Oct, 2005 https://harvardmagazine.com/2005/09/frances-glessner-lee-html (accessed 24 July 2020).
- 41. An Endowment for Legal Medicine. Center for the history of medicine at Countway library. Undated https://collections.countway.harvard.edu/onview/exhibits/show/corpus-delicti/endowment-for-legal-medicine (accessed 24 July 2020).
- 42. Carter JR. Alan Richards Moritz, MD, 1899-1986, Obituary. AJP;1987:March:401-2 http://archive.asip.org/journals/AJP/documents/in_memoriam/AlanRichardsMoritz.pdf (accessed 24 July 2020).
- 43. Adelson L. Alan Richards Moritz, M.D.: an appreciation. Am J For Med Pathol. 1981;2(4):297–298. https://journals.lww.com/amjforensicmedicine/Citation/1981/12000/Alan_Richards_Moritz,_M_D___An_appreciation_.2.aspx#pdf-link (accessed 24 July 2020). [DOI] [PubMed] [Google Scholar]
- 44. Richard Ford (1915-1970). Center for the history of medicine at Countway library. Undated. https://collections.countway.harvard.edu/onview/exhibits/show/corpus-delicti/richard-ford (accessed 24 July 2020).
- 45. Tedeschi LG, Richard Ford MD. In memoriam. Am J For Med Pathol. 1981;2(4):313–314. https://journals.lww.com/amjforensicmedicine/Citation/1981/12000/Richard_Ford,_M_D___In_memoriam.5.aspx (accessed 24 July 2020). [DOI] [PubMed] [Google Scholar]
- 46. In Memory of William J. Curran. Frances Glessner Lee Professor of Legal Medicine, Harvard University. Health Human Rights. 2014;2(2):5–8. https://cdn2.sph.harvard.edu/wp-content/uploads/sites/125/2014/03/3-Gostin.pdf (accessed 24 July 2020). [Google Scholar]
- 47. Eckert WG. Charles Norris (1868-1935) and Thomas A. Gonzales (1878-1956), New York’s pioneers. Am J For Med Pathol. 1987;8(4):350–353. doi:10.1097/00000433-198712000-00018 [DOI] [PubMed] [Google Scholar]
- 48. Eckert WG. Dr, Harrison Stanford Martland (1883-1954). Am J For Med Pathol. 1987;2(1):83–84. doi:10.1097/00000433-198103000-00014 [DOI] [PubMed] [Google Scholar]
- 49. Dolinak D, Balraj E. In memoriam: Lester Adelson, MD (1914-2006). Am J For Med Pathol. 2006;27(3):283–284. [Google Scholar]
- 50. McCallum JS. Crime Doctor: Dr. Charles P. Larson, World’s Foremost Medical-Detective, Reports from his Crime File. Writing Works, Inc; 1978. [Google Scholar]
- 51. Jentzen JM. Death Investigation in America: Coroners, Medical Examiners, and the Pursuit of Medical Certainty. Harvard Univ Press; 2009; p. 82, 96-97, 99, 103-106. [Google Scholar]
- 52. Silliphant WM. A central registry of forensic pathology. J For Sci. 1959;4:156–158. [Google Scholar]
- 53. Stahl CJ. The registry of forensic pathology. J Forensic Sci. 1968;13(2):151–162. [PubMed] [Google Scholar]
- 54. Pierre Antoine Finck. https://www.doximity.com/profiles/0480d54c-2a35-4720-a82a-854a4b715cb8 (accessed 24 July 2020).
- 55. Frank and Ruth Kiel: An inventory of their papers, 1566-2018 and undated, at the Southwest Collection/Special Collections Library. Texas Archival Resources Online; Texas Tech University. https://legacy.lib.utexas.edu/taro/ttusw/00448/tsw-00448.html (accessed 24 July 2020).
- 56. Townsend FM, Davidson WH. Experience of the Armed Forces Institute of Pathology in aircraft accident investigation, 1956-1960. Mil Med. 1961;126(5):335–339. [PubMed] [Google Scholar]
- 57. Hill IR. The historical background to aerospace pathology, Aviat Space Environ Med. 1982;53(1):1–5. [PubMed] [Google Scholar]
- 58. Stahl Charles J., III, M.D The History of the NAME, 2014. 4888-432625685 -1.pdf. 2014:585–591.https://www.thename.org/assets/docs/NAME_History_eBook_2014.pdf (accessed 24 July 2020).
- 59. Dr. Charles J. Stahl, Oral History Interview. June 15, 1994, by Charles Stuart Kennedy, AFIP https://archive.org/details/StahlCharles (accessed 24 July 2020).
- 60. Stahl Collection. 2012. Otis Historical Archives. OHA 315.5, 1951-2002. National Museum of Health & Medicine; https://www.health.mil/Reference-Center/Publications/2015/12/23/Stahl-Collection (accessed 24 July 2020). [Google Scholar]
- 61. Weedn VW. Richard Coe Froede, MD: an officer and a gentleman, in memoriam. Am J For Med Path. 2011;32(4):305–307. doi:10.1097/PAF.0b013e31822ed584 [DOI] [PubMed] [Google Scholar]
- 62. 00010: Froede, Richard. Interview by Charles Stuart Kennedy, 10/27/94. Otis Historical Archives, OHA 89, AFIP Oral History Collection, 1991-1994. National Museum of Health & Medicine; https://health.mil ‹ Reference-Center ‹ Publications ‹ 2015/12/18 ‹ AFIP. The History of the NAME, 2014. 4888-432625685 -1.pdf. pp. 443-470, 459-460, 463-465. https://www.thename.org/assets/docs/NAME_History_eBook_2014.pdf (accessed 24 July 2020). [Google Scholar]
- 63. Stafford N. Earl rose: pathologist prevented from performing autopsy on US President John f Kennedy. BMJ. 2012;345:e4768. doi:10.1136/bmj.e4768 [Google Scholar]
- 64. Simkin J. Pierre Antoine Finck, Spartacus Educational; September 1997, updated January 2020 https://spartacus-educational.com/JFKfinck.htm (accessed 24 July 2020).
- 65. Augenstein S. Case study: the assassination of RFK, and ‘The perfect autopsy’. June 19, 2018. Forensic magazine. https://www.forensicmag.com/news/2018/06/case-study-assassination-rfk-and-perfect-autopsy (accessed 24 July 2020).
- 66. Wecht CH. Postmortem protocols in official medical-legal investigation—a study in contrast (autopsy reports in the assassination deaths of President John F. Kennedy and Senator Robert F. Kennedy). Legal Medicine Annual. 1973:17–87. [Google Scholar]
- 67. Spencer J. The Armed Forces Medical Examiner System: A History. The History of the NAME, 2014. 4888-432625685 -1.pdf; 2014:108–117. https://www.thename.org/assets/docs/NAME_History_eBook_2014.pdf (accessed 24 July 2020).
- 68. Stahl CJ, Froede RC, Zimmerly JG. Forensic science at the Armed Forces Institute of Pathology: its role in military medicine. US Navy Med. 1973;61:20–27.4517573 [Google Scholar]
- 69. Luke JJL. The Armed Forces Medical Examiner System: A History. The History of the NAME, 2014 (4888-432625685 -1.pdf); 2014:356–357: https://www.thename.org/assets/docs/NAME_History_eBook_2014.pdf (accessed 24 July 2020).
- 70. Department of Defense Directive 6010.16, US Department of Defense, Mar 8, 1988. http://www.dtic.mil/dtic/tr/fulltext/u2/a272374.pdf (accessed 24 July 2020).
- 71. Clark MA, Ruehle CJ, Wright DG, Sohn SS, McMeekin RR. The Armed Forces Medical Examiner System: a change for the better. Aviat Space Environ Med. 1989;60(7 Pt 2):A1–3. [PubMed] [Google Scholar]
- 72. Shemonsky NK, Reiber KB, Williams LD, Froede RC. Jurisdiction on military installations. Mil Med. 1993;158(9):585–587. Am J Forensic Med Pathol. 1993;14(1):39-42. [PubMed] [Google Scholar]
- 73. Spencer JD. Medical examiner/coroner jurisdiction in cases involving federal interests. J For Sci. 1982;27(2):408–411. [PubMed] [Google Scholar]
- 74. Title 10 U.S.C. §1471, US Government Publishing Office; January 3, 2012. https://www.gpo.gov/fdsys/pkg/USCODE-2011-title10/pdf/USCODE-2011-title10-subtitleA-partII-chap75-subchapI-sec1471.pdf (accessed 24 July 2020).
- 75. Lee C. Pathologists Protest Defense Site’s Closure: Realignment will divvy up Functions of the Definitive Disease Clearinghouse. Washington Post. Feb. 4, 2007 https://www.washingtonpost.com/archive/politics/2007/02/04/pathologists-protest-defense-sites-closure-span-classbankheadrealignment-will-divvy-up-functions-of-the-definitive-disease-clearinghousespan/e4446cd4-47f0-484d-83f4-4a0d058620a4/ (accessed 24 July 2020).
- 76. Humphreys G, Ghent A. World laments loss of pathology service. Bull World Health Org. 2010;88(8):561–640. https://www.who.int/bulletin/volumes/88/8/10-010810/en/ (accessed 24 July 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lakhman K. ASCP Mourns Closure of the Armed Forces Institute of Pathology. Genomeweb; 2011. https://web.archive.org/web/20120317043253/http://www.genomeweb.com/blog/ascp-mourns-closure-armed-forces-institute-pathology (accessed 24 July 2020). [Google Scholar]
- 78. McCook A. Death of a pathology Centre: Shelved. Nature. 2011;476(7360):270–272. doi:10.1038/476270a [DOI] [PubMed] [Google Scholar]





