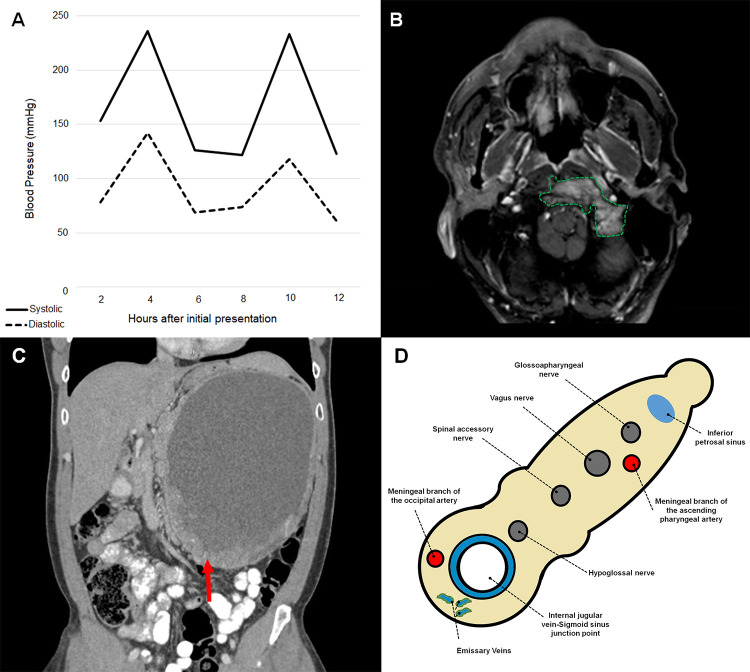
A 51-year-old man developed progressive dysarthria. Hours after presenting, he experienced paroxysmal diaphoresis and blood pressure fluctuations (Figure 1A). Examination showed weak cough, hoarseness, flaccid dysarthria, weak left shoulder shrug, and left tongue deviation. Our findings of lower cranial neuropathies prompted brainstem and neck imaging, revealing contrast-enhancing mass in the jugular foramen (Figure 1B). His dysautonomia compelled neuroendocrine studies, which showed elevated chromagranin A (7047 ng/mL; normal <93), epinephrine (3334 µg; normal <21), and norepinephrine (1117 µg; normal 15-80). Abdominal imaging indicated a large retroperitoneal mass (Figure 1C), confirmed as a pheochromocytoma (pheo) on biopsy.
Figure 1.
A, Line plots of blood pressure fluctuations during the first 12 hours after initial presentation. B, Axial T1-weighted magnetic resonance image of the neck with contrast demonstrating avidly enhancing mass (outlined) within the left jugular foramen, extending medially and eroding the left aspect of the clivus. C, Coronal computed tomography of the abdomen showing large retroperitoneal soft tissue mass (arrow), likely the primary tumor, displacing loops of bowel inferiorly and medially. D, Cross-sectional schematic representation of structures passing through the jugular foramen.
Malignant pheo is rare, accounting for 8% to 13% of catecholamine-secreting tumors; this is classically described as the “10% rule.”1 There are sparse reports of neuraxis involvement.2,3 Diagnostic challenges arise, given that hyperadrenergic spells (ie, diaphoresis, tachycardia, hypertension) are nonspecific, and abdominal tumor burden can remain asymptomatic for years—as seen in our patient.4,5 Local tissue invasion is often the only clue.4,6 In our case, cranial nerve 9 to 12 involvement offered localizing value to the jugular foramen (Figure 1D), eponymously known as the Collet-Sicard syndrome (CSS).7,8 The differential diagnosis for CSS is broad, including tumor (eg, glomus jugulare, meningioma, schwannoma), trauma (vertebral fracture), inflammatory disorders (sarcoid, systemic lupus), infection (varicella zoster), and vascular phenomena (carotid aneurysm, venous thrombosis).8,9 Here, malignant pheo represented a possible unifying diagnosis between CSS and hyperadrenergic spells. This concern prompted neuroendocrine studies. Given that ∼95% of malignant pheo’s are intra-abdominal in origin, elevated catecholamines should further compel abdominal imaging for both prognostication and treatment guidance.10
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Jordan Y. Amar, MD, MSc  https://orcid.org/0000-0002-2455-6543
https://orcid.org/0000-0002-2455-6543
References
- 1. Jimenez P, Tatsui C, Jessop A, Thosani S, et al. Treatment for malignant pheochromocytomas and paragangliomas: 5 years of progress. Curr Oncol Rep. 2017;19(12):83. [DOI] [PubMed] [Google Scholar]
- 2. Boettcher LB, Abou-Al-Shaar H, Ravindra VM, et al. Intracranial epidural metastases of adrenal pheochromocytoma: a rare entity. World Neurosurg. 2018;114:235–240. [DOI] [PubMed] [Google Scholar]
- 3. Liu S, Song A, Zhou X, et al. Malignant pheochromocytoma with multiple vertebral metastases causing acute incomplete paralysis during pregnancy: Literature review with one case report. Medicine (Baltimore). 2017;96(44):e8535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bravo EL. Evolving concepts in the pathophysiology, diagnosis, and treatment of pheochromocytoma. Endocr Rev. 1994;15(3):356–368. [DOI] [PubMed] [Google Scholar]
- 5. Baguet JP, Hammer L, Mazzuco TL, et al. Circumstances of discovery of phaeochromocytoma: a retrospective study of 41 consecutive patients. Eur J Endocrinol. 2004;150(5):681–686. [DOI] [PubMed] [Google Scholar]
- 6. Hamidi O, Young WF, Jr, Iñiguez-Ariza NM, et al. Malignant pheochromocytoma and paraganglioma: 272 patients over 55 years. J Clin Endocrinol Metab. 2017;102(9):3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Collet FJ. Sur un nouveau syndrome paralytique pharyngo-larynge par blessure de guerre (hemiplegie glosso-laryngo-scapulo-pharyngee). Lyon Med. 1915;124:121–129. [Google Scholar]
- 8. Prashant R, Franks A. Collet-Sicard syndrome—a report and review. Lancet Oncol. 2003;4(6):376–377. [DOI] [PubMed] [Google Scholar]
- 9. Neo S, Lee KE. Collet-Sicard syndrome: a rare but important presentation of internal jugular vein thrombosis. Pract Neurol. 2017;17(1):63–65. [DOI] [PubMed] [Google Scholar]
- 10. Mei L, Khurana A, Al-Juhaishi T, et al. Prognostic factors of malignant pheochromocytoma and paraganglioma: a combined SEER and TCGA databases review. Horm Metab Res. 2019;51(7):451–457. [DOI] [PubMed] [Google Scholar]