Abstract
Macular hemorrhage can occur spontaneously and repeatedly without choroidal neovascularization or other known lesions associated with myopia. We report a case of repeated myopic macular hemorrhage following fish oil supplementation. A 32-year-old male was referred with newly acquired paracentral scotoma in the left eye. Serial retinal imaging, including fundus photography, fluorescein angiography, and spectral-domain optical coherence tomography were performed. Fundus photography and fluorescein angiography showed a subtle red-colored lesion nasal to the fovea. Optical coherence tomography showed a dome shaped elevation in the ellipsoid zone and interdigitation zone in the left eye. No known ocular risk factors for macular hemorrhage, such as choroidal neovascularization, lacquer cracks, Fuch’s spot or choroid thinning or keratoconus were observed. After 2 months without any treatment, the left eye lesion disappeared. However 2 weeks later, another newly developed red-colored lesion close to the left fovea was observed. At that moment, the detailed medical history revealed that the patient had been regularly taking a high dose of commercially available fish oil supplement beginning one month before the first macular hemorrhage. After discontinuation of the fish oil, the second left hemorrhage resolved gradually over the following 8 weeks. No recurrent hemorrhages have been detected at the 12 months follow-up visits. Our observations suggest that the relative value of nutritional supplementation with high doses of fish oil should be cautioned in patients with repetitive retinal hemorrhage.
Keywords: Fish oil, macular, hemorrhage, choroidal neovascularization, anti-VEGF
Introduction
Choroidal neovascularization (CNV), chorioretinal thinning, and lacquer crack1,2 are often associated with macular hemorrhage in high myopia. As some patients sometimes spontaneously recover without any therapeutical intervention such as anti-vascular endothelial growth factor (VEGF) treatment or photodynamic therapy (PDT)3 clinicians often choose observation before initiating anti-VEGF treatment or PDT.3 Seldom are nutritional factors like “fish oil” considered as potential confounding factors, though fish oil with eicosapentaenoic acid (EPA) has previously been reported to increase bleeding time in animal studies where rats have been administered fish oil supplement.4–6 Here, we report a case of highly myopic patient with repeated macular hemorrhage that seems to be associated with prolonged use of high dose “fish oil,” Cessation of fish oil supplementation was associated with complete clinical recovery.
Case
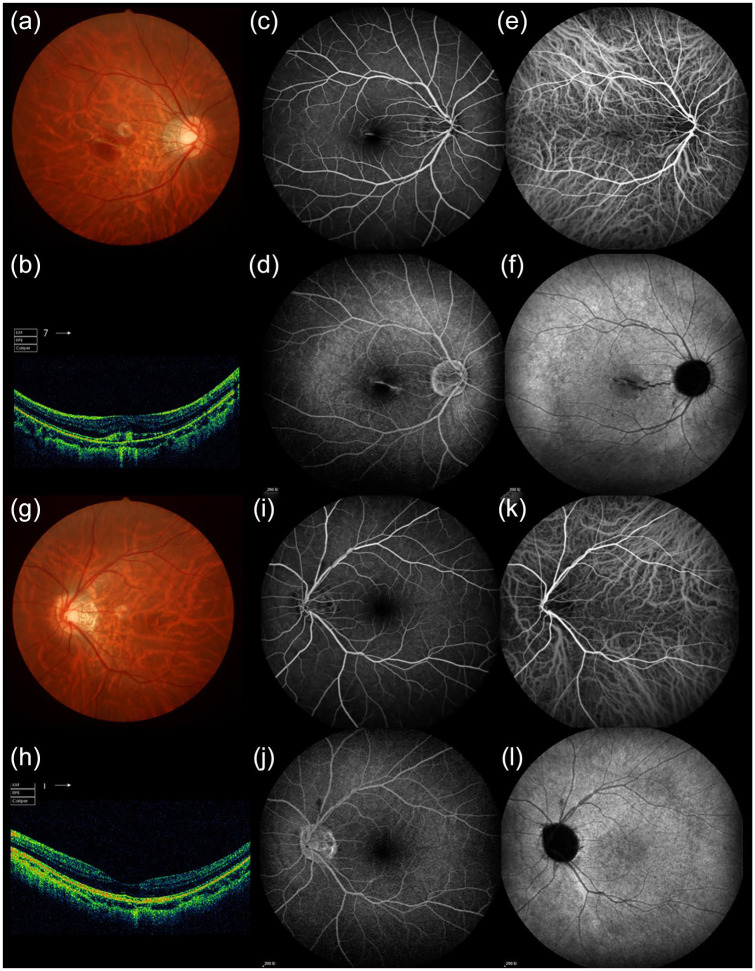
A 32-year-old Chinese man with high myopia {-10.5D right eye (RE) and -9.75D left eye (LE)} was referred to our clinic for anti-VEGF intravitreal injection treatment for a paracentral scotoma in the left eye (LE) with no visible evidence of CNV (Figure 1(g)–(l)) in December 2012. Eight months earlier, (April 2012) he had presented with a paracentral scotoma in the right eye (RE), which was diagnosed as CNV (Figure 1(a)–(f)) confirmed by fluorescein angiography (FA) and indocyanine green angiography (ICGA). PDT combined with anti-VEGF intravitreal injection (Ranibizumab) was administered to the RE. One month later, the CNV in the right eye became inactive though the structural changes remained. Visual acuity through the RE also improved from 6/8 to 6/6 and has remained stable.
Figure 1.
Right eye showed central hemorrhage in the color photograph (a), which is due to CNV leakage in FFA (c, d) and ICGA (e, f). FFA and ICGA was recorded simultaneously at the early phase (c, e) and the late phase (d, f). OCT showed discontinuity of RPE layer and subretinal high reflectivity which is consistent with CNV (b). Left eye showed normal structure in the color photograph (g), OCT (h), FFA (i, k) and ICGA (j, l), which is eight months prior to the first presentation in LE.
When the patient represented in December 2012, he reported difficulties in reading through the LE that was supported by imaging of a paracentral scotoma in the LE. Fundus photography revealed a subtle red-colored lesion nasal to the left fovea (Figure 2(c)). Spectral-domain optical coherence tomography (SD-OCT)(Topcon Corporation, Tokyo, Japan) revealed a dome shaped elevation in the ellipsoid zone (EZ) and interdigitation zone (IZ) nasal to the fovea (Figure 2(d)) of the LE, without choroid thinning. Neither autofluorescence (AF) imaging or FA (Figure 2(a)–(b)) revealed any CNV. No other risk factors such as choriod thinning or lacquer cracks were observable. In December 2012, this patient was referred for anti-VEGF treatment for the LE. Close observation showed was no evidence of CNV. Multifocal electroretinogram (mfERG) (EDI, San Mateo, CA) showed reduced N and P wave amplitude in the nasal parafoveal area (Figure 3(a) and (b)), which is consistent with the hemorrhage lesion in SD-OCT. Three weeks later, mfERG showed slight recovery in amplitude in the nasal parafoveal area (Figure 3(c) and (d)). Eight weeks after the first LE hemorrhage (Jan.2013), the left paracentral scotoma and the dome-shaped elevation observed on OCT had dissipated. However, a second paracentral scotoma closer to the left fovea developed within the next 2 weeks (February 2013). A new dot-like lesion was also observed in the fundus photography (Figure 2(e)) and new dome shaped elevation in the ellipsoid zone and IZ nasal to the fovea was showed by SD-OCT (Figure 2(f)).
Figure 2.
FFA showed a small hypofluorescence lesion during the early phase (a) nasal to the fovea (white arrow) This was maintained to the late phase without change (b) when the paracentral scotoma first appeared in the left eye (December 2012). Fundus color photography showed a small red-colored lesion, nasal to the fovea (white arrow)(c). Spectral-domain optical coherence tomography (SD-OCT) demonstrated a dome-shaped elevation in the ellipsoid zone (EZ) and interdigitation zone (IZ) nasal to the fovea (whit arrow)(e). Ten weeks later, just 2 weeks after recovery of initial hemorrhage, a new retinal hemorrhage occurred in his left eye (double white arrow)(e), located temporal to the previous one (white arrow). SD-OCT showed a dome-shaped elevation in the retinal photoreceptor layer similar to the previous one (white arrow)(f). Fundus color photography and SD-OCT showed a left retinal hemorrhage which was absorbed and did not reoccur during follow-up 2 months (g, h) and 12 months (i, j) after cessation of high dose fish oil.
Figure 3.
When paracentral scotoma first appeared in the left eye in Dec.2012, multifocal electroretinogram (mfERG) showed reduced N and P wave in the nasal parafoveal area either in wave traces (a) or 3D plots (b), which is consistent with the hemorrhage lesion in OCT. Three weeks later, mfERG showed slight recovery in the nasal parafoveal area in wave traces (c) and 3D plots (d).
When directly questioned, the patient reported regularly taking two capsules of fish oil nutritional supplement, as two 1000 mg capsules. The total dose was 1000 mg Omega-3, and 400 mg docosahexaenoic (DHA), 600 mg EPA. The nutritional supplementation program had been initiated by the patient himself, one month before the first macular hemorrhage in the left eye, and was still continuing at the time of the second left macular hemorrhage. Examination of intergrades of fish oil with different brands suggests the patient had taken a high dose (A2 as shown in the Table 1). Immediate discontinuation of the supplement was recommended, and the second hemorrhage resolved gradually over the next 8 weeks. No further hemorrhages have been observed in the following months. Figure 3(g)–(h) show the results 2 months later and Figure 3(i) and (j), show photos at 6, and 12 months post-cessation of the fish oil supplementation. Screening blood tests were performed twice: once ranibizumab injection for RE (April, 2012) and 1 month after the discontinuation of the fish oil supplement (March, 2013). The blood platelet level (PLT) was normal (268 × 109/L) at the first test, but had dramatically decreased to only half (129 × 109/L) of the normal level (300 × 109/L), at the time of the second assessment by which time fish oil capsules had been discontinued for 1 month. Three months after the discontinuation of the fish oil supplement, the patient’s PLT level had returned to previous normal level as 279 × 109/L.
Table 1.
Intergrades of Fish oil with different brands.
| A | B | C | D | E | F | G | |||
|---|---|---|---|---|---|---|---|---|---|
| A1 | A2 (High pure) | A3 (Super pure) | |||||||
| Fish oil | 1200 mg | 1000 mg | 1360 mg | 1200 mg | 1000 mg | ||||
| Total Omega-3 fatty acid | 360 mg | 500 mg | 950 mg | 360 mg | 300 mg | ||||
| DHA | 265–300 mg | 182 mg | 120 mg | 100 mg | 120 mg | ⩾110 | |||
| EPA | 170–200 mg | 129 mg | 180 mg | 160 mg | 180 mg | ⩾170 | |||
| Fat | 1200 mg | 1000 mg | 1500 mg | 1000 mg | |||||
| Cholesterol | 10 mg | 10 mg | ⩽5 mg | 10 mg | |||||
| Vitamin E | 20 mg | 1 mg | |||||||
DHA: docosahexaenoic; EPA: eicosapentaenoic acid.
Discussion
This case reports a possible association between macular hemorrhage without CNV and fish oil nutrition supplement and highlights the need for physician’s awareness of such potential associations possibly resulting in retinal dysfunction and loss of vision. Although several recent papers have suggested potential risk factors associated with subretinal hemorrhages in myopic eyes,1,2 there is little definitive understanding of the biological etiology of retinal hemorrhages. Indeed in the left eye of this patient, there was no sign of trauma, keratoconus, or corneal surgery which have all previously been associated with retinal bleeding.7 OCT and fundus fluorescein angiography (FFA) imaging did not show any visible sign of CNV, choroid thinning, or lacquer cracks indicating the need for exhaustive medical histories to exclude personal environmental factors such as nutritional supplements. Association between fish oil, and especially EPA and increased bleeding time in animals and humans has been known for considerable time.6,8–11
EPA was first reported to increase bleeding in animals in 1989.4 In the 1990s, there were several studies suggesting fish oil affected the anticoagulation status of coronary artery integrity particularly after coronary surgery.9–11 More recently, young rats fed fish oil supplement for only 1 week, have been shown to be at greater risk of hemorrhagic stroke following middle cerebral artery occlusion than those fed normal diet.6 Duodenum ulcer bleeding has also been reported in a 60-year-old amateur athlete taking omega three supplement for a year.8 A recent clinical trial evaluated the effects of icosapent ethyl in 8179 patients with cardiovascular risk and showed that icosapent ethyl significantly decreased the risk of ischemic events, while also associated with serious bleeding events.12
Conclusion
In conclusion, our clinical observations suggest that in this case, after exclusion of other reported risk factors related to macular hemorrhage in high myopia, repeated macular hemorrhage without apparent CNV may be associated with the excessive intake of fish oil. Thus, in future patients with repetitive retinal hemorrhage should be investigated for and cautioned against taking high dosages of fish oil, especially before selecting invasive treatments such as anti-VEGF intravitreal injection.
Acknowledgments
The authors are grateful to Yi Wang for his insightful comments, Chen Sun and Minfang Zhang for their great technical support.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Chongqing Social and livelihood science innovation grant (cstc2017shmsA130100), National Basic Research Program of China (2018YFA0107301), and National Nature Science Foundation of China (81974138). This study was supported by grants from National Hospital Organization Network Research Fund (H30-NHO-Sensory Organs-03).
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Yan-Ling Long  https://orcid.org/0000-0003-3442-3311
https://orcid.org/0000-0003-3442-3311
References
- 1. Asai T, Ikuno Y, Nishida K. Macular microstructures and prognostic factors in myopic subretinal hemorrhages. Invest Ophthalmol Vis Sci 2014; 55(1): 226–232. [DOI] [PubMed] [Google Scholar]
- 2. Kang HM, Koh HJ. Ocular risk factors for recurrence of myopic choroidal neovascularization: long-term follow-up study. Retina 2013; 33(8): 1613–1622. [DOI] [PubMed] [Google Scholar]
- 3. Yoon JU, Byun YJ, Koh HJ. Intravitreal anti-VEGF versus photodynamic therapy with verteporfin for treatment of myopic choroidal neovascularization. Retina 2010; 30(3): 418–424. [DOI] [PubMed] [Google Scholar]
- 4. Juan H, Sametz W. Fish oil diet rich in eicosapentaenoic acid increases bleeding time in the rat by interaction with sympathetic transmitters. Agents Actions 1989; 28(1–2): 130–136. [DOI] [PubMed] [Google Scholar]
- 5. Clarke J, Herzberg G, Peeling J, et al. Dietary supplementation of omega-3 polyunsaturated fatty acids worsens forelimb motor function after intracerebral hemorrhage in rats. Exp Neurol 2005; 191(1): 119–127. [DOI] [PubMed] [Google Scholar]
- 6. Pascoe MC, Howells DW, Crewther DP, et al. Fish oil diet associated with acute reperfusion related hemorrhage, and with reduced stroke-related sickness behaviors and motor impairment. Front Neurol 2014; 5: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Oh JY, Yu HG. Keratoconus associated with choroidal neovascularization: a case report. J Med Case Report 2010; 4(1): 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Detopoulou P, Papamikos V. Gastrointestinal bleeding after high intake of omega-3 fatty acids, cortisone and antibiotic therapy: a case study. Int J Sport Nutr Exerc Metab 2014; 24(3): 253–257. [DOI] [PubMed] [Google Scholar]
- 9. Eritsland J, Arnesen H, Gronseth K, et al. Effect of dietary supplementation with n-3 fatty acids on coronary artery bypass graft patency. Am J Cardiol 1996; 77(1): 31–36. [DOI] [PubMed] [Google Scholar]
- 10. Leaf A, Jorgensen MB, Jacobs AK, et al. Do fish oils prevent restenosis after coronary angioplasty. Circulation 1994; 90(5): 2248–2257. [DOI] [PubMed] [Google Scholar]
- 11. Bender NK, Kraynak MA, Chiquette E, et al. Effects of marine fish oils on the anticoagulation status of patients receiving chronic warfarin therapy. J Thromb Thrombolysis 1998; 5(3): 257–261. [DOI] [PubMed] [Google Scholar]
- 12. Bhatt DL, Steg PG, Miller M, et al. Risk reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J Med 2019; 380(1): 11–22. [DOI] [PubMed] [Google Scholar]