Abstract
Background:
Large and massive rotator cuff repairs constitute a true challenge for arthroscopic shoulder surgeons. Retear rates as high as 20% have been reported after arthroscopic double-row and suture-bridge techniques used for these tears.
Hypothesis:
A modified triple-row repair will provide satisfactory clinical results with lower risk for retear.
Study Design:
Case series; Level of evidence, 4.
Methods:
Between March 2016 and August 2017, a total of 52 patients with large and massive rotator cuff tears received a modified triple-row cuff repair. A middle repositioning anchor was inserted between the medial and the lateral rows. The middle anchor sutures were loaded to lateral knotless anchors in a star-shaped configuration. Functional evaluation was performed using the American Shoulder and Elbow Surgeons score, University of California, Los Angeles score, Constant-Murley score, and Simple Shoulder Test. Subjective evaluation was carried out using a visual analog scale for pain and a subjective shoulder value score. Health-related as well as disease-specific quality-of-life scores were also used. Retear rates were assessed by means of musculoskeletal ultrasonography. Patients were evaluated for a minimum of 24 months.
Results:
This study included 34 female and 18 male patients with a mean age of 57.17 ± 6.7 years. There were 35 patients (67.3%) with large tears and 17 patients (32.7%) with massive tears. Significant improvement from preoperative values was seen in all functional and subjective scores (P < .001). The mean forward flexion was 163° ± 9.7°, and the mean lateral abduction was 159.4° ± 9.4°. All patients had excellent scores on the general health-related and disease-specific quality-of-life scales. No retears were reported at the end of the follow-up period.
Conclusion:
The star-shaped, modified triple-row cuff repair is a valid and effective solution for surgical management of large and massive rotator cuff tears, providing excellent results and low risk for retears.
Keywords: large and massive cuff tear, triple row, rotator cuff tear, star cuff repair
Rotator cuff tears are a common cause of shoulder pain and disability. Debate continues regarding the ideal surgical management of large and massive rotator cuff tears. Many surgeons favor simple debridement and decompression, whereas others favor open repairs. However, the majority of these tears are now treated with arthroscopic repair and decompression. The controversy is especially intense regarding the optimal repair strategy for these tears. Despite the improved biomechanical performance of the newer repair techniques, rates of recurrent tearing as high as 20% are commonly reported.12,32
Retears are more likely with large tears as well as those with a high degree of tendon retraction, short tendons, and severe fatty degeneration. The initial tear size is reported to be the most significant factor that affects tendon healing. The relative risk of retear increases 2.29 times with every 1-cm increase in tear size.3,24
The double-row and suture-bridge repair techniques were thought to have smaller retear rates. These techniques provide better biomechanical properties compared with single-row techniques in terms of mechanical strength, gap formation, footprint coverage, and tendon-to-bone contact, which theoretically lead to improved healing response.5,7 Despite these advantages, some studies demonstrated significantly high rates of cuff retears after double-row and suture-bridge techniques.9,20,33,36 Trantalis et al33 postulated that the medial cuff failure that was found only with double-row and suture-bridge techniques may be due to the increased tension exerted on medial anchors during insertion and suture tightening.
Although some strategies have been proposed to decrease medial row failure with large and massive tears,18,23 the main problem remains, in that adequate restoration and tension-free repair of the cuff with sufficient footprint coverage are often not guaranteed, regardless of the repair technique.22
An additional reduction anchor to relieve tension on the medial row and to increase the footprint contact has been introduced as a promising strategy to prevent cuff retear in large and highly retracted tears. This triple-row technique, with the central middle anchor tied first, allows tension-free knotting of the medial row with better footprint coverage as well as higher contact pressure. The possibility of tendon mobilization with the grasper to its native footprint was described as a tension-free repair by Ostrander et al.25,26
In the present study, a modification of the originally described triple-row technique is proposed, in which the middle repositioning central anchor sutures are linked to the lateral knotless anchors to produce more tension-free repair and more tendon compression. As well, from a biomechanical point of view, the more interconnection that exists between anchors, the less likely a tension mismatch during humeral rotation will occur.28 To our knowledge, no published data are available in the literature presenting such a technique or evaluating the clinical results of linking both the double-row with the suture-bridge techniques in a single construct.
The aim of this study was to evaluate the clinical outcomes and retear rates after an arthroscopic star-shaped, modified triple-row technique for large and massive tears. The hypothesis of this study was that the modified triple-row technique will lead to satisfactory early clinical results with low retear rates.
Methods
This study was a prospective case series with approval received from the local university ethical committee.
Patient Selection
From March 2016 to August 2017, a total of 52 patients with full-thickness large and massive tears were admitted to our institution. They all received an arthroscopic modified triple-row cuff repair technique performed by the same surgeon (M.G.M.) and were considered for inclusion in this study.
The inclusion criteria were patients with large and massive tears on magnetic resonance imaging (MRI) with high-grade tendon retraction that was either Patte30 grade II, with retraction to the articular surface of the head of the humerus, or Patte grade III, with retraction to the glenoid margin. Patients with subscapularis tears more than grade I according to Lafosse et al,19 as well as patients with previous shoulder surgery, rotator cuff arthropathy, frozen shoulder, severe fatty degeneration of the cuff (Goutallier grade >III), and/or irreparable cuff tears, were excluded from the study. Irreparable tears were identified as fatty degeneration with Goutallier grade >III, decreased acromiohumeral distance <6 mm, loss of the tendon length with retraction beyond the glenoid, and/or poor quality of tendon tissue during arthroscopy.
All patients were evaluated preoperatively both clinically and radiologically. In all patients, MRI scans showed a large or massive cuff tear with tendon retraction beyond the footprint (Figure 1).
Figure 1.
Massive rotator cuff tear with tendon retraction grade II according to Patte.30
Surgical Technique
Surgery was performed arthroscopically with the patient in a semisetting position under general anesthesia with an interscalene block. An examination under anesthesia was performed first to ensure free passive range of motion (ROM).
Routine shoulder arthroscopy was performed through the standard posterior portal. Any intra-articular pathology was evaluated, after which cuff inspection was done from within the joint before switching to the subacromial space. An anterolateral portal was created using a needle under direct arthroscopic visualization directed toward the center of the tear (Figure 2). Footprint preparation using a 5.5-mm bur through the anterolateral portal then followed. A biceps tenotomy or intra-articular tenodesis was performed according to the age of the patient; tenotomy was preferred in patients older than 60 years. An anterior portal through the rotator interval was established if subscapularis debridement was attempted. Mobilization of retracted and scarred tendon was applied through use of a soft tissue liberator, arthroscopic shaver, and/or radiofrequency ablation device.
Figure 2.

Massive tear of supraspinatus and infraspinatus viewed from lateral portal.
A routine shoulder subacromial decompression was conducted if needed. Any lateral impingement was decompressed from the posterior portal to decrease retear risk. The medial row anchors were placed first. Two titanium double-loaded, 5-mm anchors (AllThread Ti; Zimmer Biomet) were placed just lateral to the articular cartilage 1 cm apart. Then, all strands of both medial anchors were passed independently through the cuff to have 4 mattress sutures after the sutures were tied.
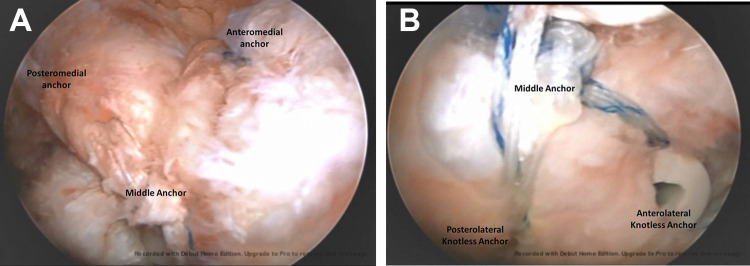
Before the sutures were tied, a repositioning central titanium “middle row” double-loaded anchor was placed (AllThread Ti) at the edge of the footprint. One limb of each color of the suture threads was passed through the cuff in a simple fashion to anatomically reduce the cuff to its footprint. These 2 simple sutures were tied first to adjust the tension of the tendon before the medial row was tied. This allowed tension-free knotting of the medial row anchors. After the medial row was tied, 1 strand from each mattress suture was cut, leaving 4 strands from the medial row and 2 strands from the middle row. Finally, a lateral row with 2 polyether-ether-ketone (PEEK) 5.5-mm knotless anchors (Quattro Link; Cayenne Medical Inc) was placed lateral to the greater tuberosity. Each knotless anchor was loaded with 3 strands: 2 strands from the medial row (1 strand from the anterior anchor and 1 strand from the posterior anchor) and 1 strand from the middle row. This allowed more cuff compression and less gap formation (Figure 3).
Figure 3.
Modified triple-row cuff repair viewed from lateral portal. (A) Medial part of the repair; (B) lateral part of the repair.
After the repair was finished, the arthroscope was shifted to the lateral portal to assess adequate compression of the cuff under a star-shaped repair with no dog-ear formation (Figure 4). Then the arthroscope was switched intra-articularly to evaluate the adequacy of the repair from inside.
Figure 4.
(A) Modified linked triple-row technique where the sutures of the middle anchor (green strands) are loaded to the lateral knotless anchors. (B) Star-shaped repair of modified linked triple-row technique.
Postoperative Management
After surgery, all of the patients were immobilized in a broad arm sling for 6 weeks. Passive ROM was allowed from the first day after surgery, and active-assisted ROM was permitted 3 weeks later. This early rehabilitation was possible because of the highly secured repair. Active ROM was allowed after 6 weeks under the supervision of a specialized physiotherapist, and physical work was encouraged 4 months after surgery.
At follow-up, patients were assessed as follows:
Shoulder function was assessed with the American Shoulder and Elbow Surgeons (ASES) score,31 the University of California, Los Angeles (UCLA) shoulder score,35 the Constant-Murley score (CMS),11 and the Simple Shoulder Test (SST).13
Subjective patient assessments were obtained through use of the subjective shoulder value (SSV) (0%-100%, where 100% = normal) and a visual analog scale (VAS) for pain (0-10, where 10 = maximum pain).
Health-related quality of life was assessed using the 12-Item Short Form Health Survey (SF-12)34 and Rotator Cuff Specific Quality of Life Score (RCQOL).15
Cuff integrity was evaluated radiographically by use of ultrasonography with a special musculoskeletal probe (Aplio 500 with 14-MHz musculoskeletal transducer; Toshiba Medical System) by an independent radiologist at least 24 months after surgery. MRI (Magnetom Sempra, with Syngo MR E11 Healthineers scanner and 1.5-T Tim coil; Siemens Healthcare) was conducted in 6 patients who had concerns about shoulder pain and discomfort shortly after surgery (Figure 5).
Figure 5.
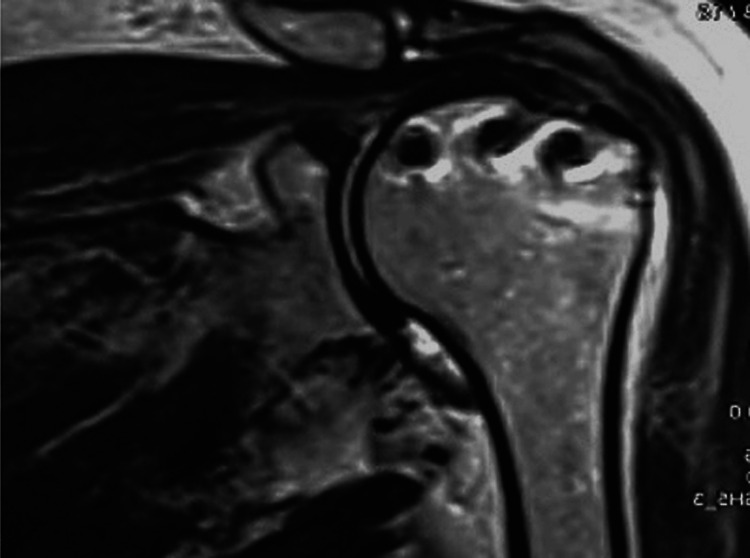
Postoperative magnetic resonance imaging scan shows adequate cuff healing after the star-shaped triple-row technique.
Statistical Analysis
Statistical analysis was conducted by use of IBM SPSS Version 25.0 (SPSS Inc). The Kolmogorov-Smirnov test was used to test the normality of data. An independent t test was performed to compare any 2 independent groups. Paired t test was used to compare preoperative and postoperative values, and the chi-square test was applied to compare qualitative data. The level of significance was set at P < .05.
Results
Between March 2016 and August 2017, a total of 52 patients with full-thickness large and massive tears underwent an arthroscopic star-shaped, modified triple-row rotator cuff repair. The study included 34 female and 18 male patients. The mean follow-up was 25.17 ± 1.8 months (range, 24-30 months). The mean age at the time of surgery was 57.17 ± 6.7 years. Patients’ demographic data are provided in Table 1.
Table 1.
Patient Demographic Data (N = 52 Patients)a
| Variable | Mean ± SD or n (%) |
|---|---|
| Age, y | 57.17 ± 6.7 (41-67) |
| Duration of symptoms, mo | 11.4 ± 3.2 (5-18) |
| Sex | |
| Male | 18 (34.6) |
| Female | 34 (65.4) |
| Side affected | |
| Right | 33 (63.5) |
| Left | 19 (36.5) |
| Dominant side affected | |
| Dominant | 26 (50) |
| Nondominant | 26 (50) |
| Type of tear | |
| Traumatic | 8 (15.4) |
| Degenerative | 44 (84.6) |
| Smoking status | |
| Smoker | 10 (19.2) |
| Nonsmoker | 42 (80.7) |
| Occupation | |
| Housewife | 19 (36.5) |
| Sedentary office worker | 22 (42.3) |
| Manual worker | 11 (21.2) |
| Tear size | |
| Large (3-5 cm on MRI) | 35 (67.3) |
| Massive (>5 cm on MRI) | 17 (32.7) |
| Tendons affected | |
| SS | 20 (38.5) |
| SS+IS | 26 (50) |
| SS+IS+GI subscapularis | 6 (11.5) |
| Tear retraction | |
| Patte grade II | 33 (63.5) |
| Patte grade III | 19 (36.5) |
| Tendon degeneration | |
| Goutallier grade II | 40 (76.9) |
| Goutallier grade III | 12 (23.1) |
| Concomitant procedures | |
| Subacromial decompression | 36 (69.2) |
| Biceps tenotomy | 28 (53.8) |
| Biceps tenodesis | 24 (46.1) |
aGI, grade I; IS, infraspinatus; MRI, magnetic resonance imaging; SS, supraspinatus.
Regarding the patients’ functional evaluation, a significant improvement was seen in both objective and subjective scores from the preoperative point to the end of the follow-up (Table 2).
Table 2.
Preoperative Versus Postoperative Functional and Subjective Assessmentsa
| Preoperative | Postoperative | Difference (95% CI) | t | P Value | |
|---|---|---|---|---|---|
| Functional assessment | |||||
| ASES | 24.6 ± 1.9 | 93.5 ± 1.6 | 68.9 (68.1-69.5) | 198.5 | <.001b |
| CMS | 29.2 ± 2.5 | 90.2 ± 1.4 | 61.0 (60.2-61.7) | 170.8 | <.001b |
| SST | 18.4 ± 7.6 | 84.6 ± 6.0 | 66.2 (64.1-68.2) | 63.7 | <.001b |
| UCLA | 6.2 ± 1.91 | 33 ± 1.6 | 26.7 (25.9-27.5) | 69.3 | <.001b |
| Subjective assessment | |||||
| VAS | 6.8 ± 0.89 | 0.9 ± 0.7 | 5.9 (5.5-6.2) | 37.2 | <.001b |
| SSV | 28.1 ± 7.4 | 90.3 ± 4.0 | 62.3 (59.7-64.8) | 49.6 | <.001b |
aASES, American Shoulder and Elbow Surgeons score; CMS, Constant-Murley score; SST, Simple Shoulder Test; SSV, subjective shoulder value; UCLA, University of California, Los Angeles score; VAS, visual analog scale.
bStatistically significant difference between pre- and postoperative values (P < .05)
As for the active ROM at the end of follow-up, the mean forward flexion was 163° ± 9.7°, lateral abduction was 159.4° ± 9.4°, and external rotation was 71.7° ± 7.5°. Regarding internal rotation, 10 patients (19.2%) achieved internal rotation to the waist, 29 patients (55.8%) to the T12 level, and 13 patients (25%) to interscapular level T7. ROM improved significantly from preoperative values for forward flexion, abduction, and external and internal rotation (P < .001 for all) (Table 3).
Table 3.
Preoperative Versus Postoperative Active Range of Motiona
| Preoperative | Postoperative | Difference (95% CI) | t | P | |
|---|---|---|---|---|---|
| Forward flexion, deg | 81.7 ± 13.9 (50-100) | 163 ± 9.7 (150-180) | 82.1 (76.9-87.2) | 31.8 | <.001b |
| Abduction, deg | 66.3 ± 13.4 (50-90) | 159.4 ± 9.4 (150-170) | 93.1 (88.0-98.1) | 36.8 | <.001b |
| External rotation. deg | 40.1 ± 9.9 (20-60) | 71.7 ± 7.5 (60-80) | 31.5 (28.1-34.9) | 18.7 | <.001b |
| Internal rotation, n (%) | T12: 11 (21.2) Waist: 41 (78.8) |
T7: 13 (25) T12: 29 (55.8) Waist: 10 (19.2) |
χ2 = 17.42 | <.001b |
aPreoperative and postoperative data are reported as mean ± SD (range) unless otherwise indicated.
bStatistically significant difference between pre- and postoperative values (P < .05).
Evaluating the quality-of-life outcomes at the end of the follow-up, we noted a significant improvement in the general health-related and disease-specific quality-of-life scores. The mean SF-12 physical score was 53.5 ± 1.8 (range, 51.1-55.3) and the mean SF-12 mental score was 53.8 ± 3.9 (range, 48.7-57.5). The mean RCQOL score was 87.4 ± 3.6 (range, 82.7-92.4). No retears were noted at the end of the follow-up, either clinically or radiologically during a specialized ultrasound probe examination by a professional musculoskeletal radiologist.
Subgroup analysis by cause of tear, amount of retraction, tendon degeneration, and tear size showed no significant differences in any functional, subjective, ROM, or quality-of-life scores (Tables 4 and 5).
Table 4.
Difference in Outcomes According to Tear Type and Tear Retractiona
| Type of Tear | Tear Retraction | |||||||
|---|---|---|---|---|---|---|---|---|
| Traumatic | Degenerative | t | P | Patte Grade II | Patte Grade III | t | P | |
| Functional assessment | ||||||||
| ASES | 93.5 ± 1.3 | 93.5 ± 1.7 | 0.07 | .94 | 93.4 ± 1.6 | 93.6 ± 1.7 | –0.04 | .76 |
| CMS | 90.1 ± 1.6 | 90.2 ± 1.3 | 0.22 | .82 | 90.3 ± 1.5 | 90.1 ± 1.3 | 0.47 | .63 |
| SST | 84.3 ± 6.9 | 84.6 ± 5.9 | 0.11 | .9 | 84.5 ± 6.6 | 84.6 ± 5.0 | –0.02 | .98 |
| UCLA | 32.8 ± 2.1 | 33 ± 1.4 | 0.28 | .78 | 32.8 ± 1.6 | 33.2 ± 1.4 | –0.85 | .39 |
| Subjective assessment | ||||||||
| VAS | 1.1 ± 0.8 | 0.9 ± 0.7 | 0.77 | .44 | 0.8 ± 0.7 | 1.1 ± 0.7 | –1.23 | .22 |
| SSV | 91.2 ± 3.5 | 90.2 ± 4.1 | 0.65 | .51 | 91.0 ± 4.0 | 89.2 ± 3.8 | 1.6 | .11 |
| Range of motion, deg | ||||||||
| Forward flexion | 158.7 ± 9.9 | 164.7 ± 9.5 | 1.63 | .1 | 164.5 ± 9.7 | 162.6 ± 9.4 | 0.67 | .5 |
| Abduction | 158.71 ± 9.9 | 159.5 ± 9.3 | 0.21 | .82 | 157.8 ± 8.9 | 162.1 ± 9.7 | –1.58 | .11 |
| External rotation | 72.5 ± 8.8 | 71.5 ± 7.4 | 0.3 | .75 | 71.8 ± 7.2 | 71.5 ± 8.3 | 0.1 | .91 |
| Quality of life | ||||||||
| SF-12 PCS | 54.4 ± 1.3 | 53.3 ± 1.9 | 1.75 | .12 | 53.4 ± 1.9 | 53.5 ± 1.9 | –0.21 | .83 |
| SF-12 MCS | 52.3 ± 4 | 54 ± 3.8 | 1.11 | .27 | 53.7 ± 4.0 | 53.9 ± 3.8 | –0.24 | .81 |
| RCQOL | 86.6 ± 4.1 | 87.5 ± 3.6 | 0.65 | .51 | 87.4 ± 3.7 | 87.3 ± 3.6 | 0.13 | .89 |
aASES, American Shoulder and Elbow Surgeons score; CMS, Constant-Murley score; MCS, Mental Component Summary; PCS, Physical Component Summary; RCQOL, Rotator Cuff Specific Quality of Life Score; SF-12, 12-Item Short Form Health Survey; SST, Simple Shoulder Test; SSV, subjective shoulder value; UCLA, University of California, Los Angeles score; VAS, visual analog scale.
Table 5.
Difference in Outcomes According to Tendon Degeneration and Tear Sizea
| Tendon Degeneration | Tear Size | |||||||
|---|---|---|---|---|---|---|---|---|
| Goutallier Grade II | Goutallier Grade III | t | P | Large | Massive | t | P | |
| Functional assessment | ||||||||
| ASES | 93.4 ± 1.8 | 94 ± 0.9 | –1.3 | .19 | 93.6 ± 1.8 | 93.3 ± 1.3 | 0.73 | .46 |
| CMS | 90.1 ± 1.3 | 90.5 ± 1.5 | –0.74 | .46 | 90.3 ± 1.4 | 90.0 ± 1.3 | 0.81 | .42 |
| SST | 83.9 ± 6.0 | 86.8 ± 5.5 | –1.44 | .15 | 84.2 ± 6.6 | 85.2 ± 4.7 | –0.55 | .58 |
| UCLA | 32.9 ± 1.6 | 33.2 ± 1.1 | –0.57 | .56 | 32.8 ± 1.7 | 33.3 ± 1.1 | –1.07 | .28 |
| Subjective assessment | ||||||||
| VAS | 0.8 ± 0.68 | 1.1 ± 0.83 | 1.22 | .22 | 0.8 ± 0.71 | 1 ± 0.74 | 0.8 | .42 |
| SSV | 90.1 ± 4 | 91.2 ± 4.3 | –0.83 | .4 | 91.0 ± 3.9 | 89.1 ± 4.0 | 1.59 | .11 |
| Range of motion, deg | ||||||||
| Forward flexion | 162.7 ± 8.7 | 167.5 ± 12.1 | –1.5 | .14 | 164.5 ± 9.5 | 162.3 ± 10.3 | 0.76 | .45 |
| Abduction | 158.7 ± 9.1 | 161.6 ± 10.2 | –0.94 | .35 | 158 ± 9 | 162.3 ± 9.7 | –1.59 | .11 |
| External rotation | 72 ± 7.5 | 70.8 ± 7.9 | 0.46 | .64 | 71.7 ± 7.4 | 71.7 ± 8.0 | –0.22 | .98 |
| Quality of life | ||||||||
| SF-12 PCS | 53.7 ± 1.8 | 52.8 ± 2 | 1.41 | .16 | 53.4 ± 1.9 | 53.5 ± 1.6 | –0.38 | 07 |
| SF-12 MCS | 53.4 ± 4 | 55.0 ± 3.2 | –1.3 | .19 | 53.6 ± 4.0 | 54.0 ± 3.7 | –0.34 | .73 |
| RCQOL | 87.3 ± 3.6 | 87.7 ± 3.7 | 0.37 | .71 | 87.4 ± 3.7 | 87.4 ± 3.4 | 0.69 | .94 |
aASES, American Shoulder and Elbow Surgeons score; CMS, Constant-Murley score; MCS, Mental Component Summary; PCS, Physical Component Summary; RCQOL, Rotator Cuff Specific Quality of Life Score; SF-12, 12-Item Short Form Health Survey; SST, Simple Shoulder Test; SSV, subjective shoulder value; UCLA, University of California, Los Angeles score; VAS, visual analog scale.
Discussion
Large and massive rotator cuff tears are a notable challenge for arthroscopic shoulder surgeons. Not only is it difficult to mobilize scarred retracted tendons, but it is also hard to achieve a tension-free repair. The management of large and massive retracted cuff tears continues to evolve as techniques for treatment improve. Nowadays, full arthroscopic repair (using advanced repair techniques such as double row and suture bridge) as well as allograft reconstruction is commonly used.2
The results of the present study confirm the reliability of the star-shaped, modified triple-row technique as a solution for large and massive tears, with no reported retears over a 24-month follow-up. The clinical outcomes improved significantly from preoperative values in all functional scores (ASES, CMS, SST, UCLA) and subjective scores (SSV and VAS). Moreover, the general health-related (SF-12) and disease-specific (RCQOL) quality-of-life scores were excellent at the end of the follow-up, which is challenging with large and massive tears. Additionally, the tightly secured repair allowed for an accelerated rehabilitation program, with active assisted ROM that started 3 weeks postoperatively. This may explain the final improvement on the subjective and quality-of-life scores. After comparing the patients with large tears versus massive tears, we found no significant differences in any functional, subjective, ROM, or quality-of-life scores between the groups.
Many studies have shown the biomechanical superiority of double-row and suture-bridge techniques over single-row repairs. These techniques have better mechanical strength, footprint coverage, less gap formation, and more tendon-to-bone compression, which may enhance healing.1,6,16,21,27,28 However, the price for this better biomechanical behavior may be a disturbed biological response.10 Excessive contact pressure may reduce blood flow to the rotator cuff tendon. This stress concentration may explain the increased risk of retear around the medial anchors that has been reported during the past decade with the double-row and suture-bridge techniques.8 Kim et al17 and Hein et al14 reported the retear rate after the suture-bridge technique to be around 42% in large and massive tears. The main source of these retears was medial cuff failure. A large amount of tension exerted on the medial row during suture tightening was postulated by Trantalis et al33 as the main cause of this retear.
Such tension can be decreased through a meticulous release of the scarred retracted tendon followed by tying the medial sutures over a well-reduced tendon without overtension. This is attainable by placing a repositioning or reduction anchor before tying the medial row. A recent study by Park et al29 found that repair tension was the most important factor for the integrity of rotator cuff repair.
In 2012, Ostrander and McKinney25 introduced the concept of triple-row cuff repair as a modification of transosseous-equivalent repair. They found that this technique anatomically reduced the lateral part of the cuff without causing an overtensioned or bunched cuff medially. This third row of fixation placed independently between the medial and lateral rows improved the contact area by anatomically reducing the cuff before the medial row was tied. The position of this anchor is very critical; thus, it should be placed at the site that restores the anatomic features and in a position midway between the medial and the anticipated lateral row anchors. Replicating the anatomic features can maximize the contact area and contact pressure without deleterious impact on the biological parameters. The main advantage of the triple-row technique is a tension-free knotting of the medial anchors. The potential for tension-free repair was confirmed by tendon mobilization with the grasper to the native footprint. With the standard suture-bridge technique, the medial anchors are tied first. This generates compression at the anchor sites only, which strangulates the tendon medially and may lead to medial cuff failure.25,26
The modified star-shaped, triple-row technique proposed in this study has many theoretical advantages compared with the double-row and the suture-bridge techniques. The double-row technique restores the footprint anatomically but without an efficient contact pressure.10 The suture-bridge repair solves this problem by linking the sutures of the medial row to the lateral aspect of the greater tuberosity. Although it has a double-row configuration however, it functions as a single-row repair in that the whole construct fails in the case of medial row failure. Therefore, by linking these 2 techniques in the modified triple-row technique proposed in this study, a triple effect can be achieved. First, an anatomic restoration of the footprint that resembles the double-row repair. Second, a better contact pressure and tendon compression that are similar to the suture-bridge technique. Third, a “tension-free” repair that is a unique feature of the triple-row construct.
Furthermore, in the original triple-row technique, once the medial anchor fails, the construct will depend on the middle anchor as if it were a single-row repair. With the modification presented in this study, unlike the original triple-row technique, the middle anchor is linked and loaded to the lateral row. This may give the construct more stability and superior performance.
A paucity of data are available regarding the clinical outcomes of triple-row cuff repair. The only clinical data on the originally described triple-row technique were recently published by Buckup et al.4 In that study, 81 patients with large and massive tears were assessed after a mean of 36.2 months after triple-row repair. The overall retear rate was 4.9% (4/81). The clinical outcome was good to excellent (ASES score, 94 ± 11; SSV, 92 ± 12; UCLA score, 33 ± 5; CMS, 90 ± 9). Unlike our study, Buckup et al applied the original triple-row technique with unlinked construct. Moreover, they did not use the health-related or the disease-specific quality-of-life scores to assess patient satisfaction after the repair.
Our study has some limitations. An additional anchor entails relatively more time and cost and poses a challenge in suture management, which necessitates a steep learning curve. Additional anchors could influence infection rates and may compromise the bone of the greater tuberosity, although neither of these problems were seen in this study or in other studies of the triple-row technique. The short follow-up of 24 months in the present study is another drawback; hence, further studies with longer follow-up period and larger number of patients may be needed. Moreover, this was a prospective therapeutic case series study with low evidence power and without a control group.
Additional limitations include the following: only 6 patients were submitted to postoperative MRI; only repairable cuff tears were included with anatomic tendon mobilization to the footprint; patients with high-grade Goutallier fatty infiltration were excluded from the study; some patients underwent additional procedures (biceps procedures, subacromial decompression); all procedures were performed by just 1 experienced surgeon; and most of the patients were low demand regarding activities of daily living.
Conclusion
The star-shaped, modified triple-row technique described in this study may represent a valid and effective solution for surgical management of large and massive rotator cuff tears, providing very low complication rates and excellent outcomes over 2-year follow-up. The technique appears to pose a low risk for retears. A randomized controlled trial of triple-row versus suture-bridge techniques is needed to compare retear rates and clinical outcomes.
Footnotes
Final revision submitted March 30, 2020; accepted April 21, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Alexandria University (ref No. 00012098).
References
- 1. Baums MH, Spahn G, Buchhorn GH, Schultz W, Hofmann L, Klinger H-M. Biomechanical and magnetic resonance imaging evaluation of a single-and double-row rotator cuff repair in an in vivo sheep model. Arthroscopy. 2012;28(6):769–777. [DOI] [PubMed] [Google Scholar]
- 2. Bittar ES. Arthroscopic management of massive rotator cuff tears. Arthroscopy. 2002;18(9):104–106. [DOI] [PubMed] [Google Scholar]
- 3. Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87(6):1229–1240. [DOI] [PubMed] [Google Scholar]
- 4. Buckup J, Smolen D, Hess F, Sternberg C, Leuzinger J. The arthroscopic triple-row modified suture bridge technique for rotator cuff repair: functional outcome and repair integrity. J Shoulder Elbow Surg. 2020;29(2):308–315. [DOI] [PubMed] [Google Scholar]
- 5. Burkhart SS. Reconciling the paradox of rotator cuff repair versus debridement: a unified biomechanical rationale for the treatment of rotator cuff tears. Arthroscopy. 1994;10(1):4–19. [DOI] [PubMed] [Google Scholar]
- 6. Burkhart SS, Adams CR, Burkhart SS, Schoolfield JD. A biomechanical comparison of 2 techniques of footprint reconstruction for rotator cuff repair: the SwiveLock-FiberChain construct versus standard double-row repair. Arthroscopy. 2009;25(3):274–281. [DOI] [PubMed] [Google Scholar]
- 7. Chen M, Xu W, Dong Q, Huang Q, Xie Z, Mao Y. Outcomes of single-row versus double-row arthroscopic rotator cuff repair: a systematic review and meta-analysis of current evidence. Arthroscopy. 2013;29(8):1437–1449. [DOI] [PubMed] [Google Scholar]
- 8. Cho NS, Lee BG, Rhee YG. Arthroscopic rotator cuff repair using a suture bridge technique: is the repair integrity actually maintained? Am J Sports Med. 2011;39(10):2108–2016. [DOI] [PubMed] [Google Scholar]
- 9. Cho NS, Yi JW, Lee BG, Rhee YG. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med. 2010;38(4):664–671. [DOI] [PubMed] [Google Scholar]
- 10. Christoforetti JJ, Krupp RJ, Singleton SB, Kissenberth MJ, Cook C, Hawkins RJ. Arthroscopic suture bridge transosseus equivalent fixation of rotator cuff tendon preserves intratendinous blood flow at the time of initial fixation. J Shoulder Elbow Surg. 2012;21(4):523–530. [DOI] [PubMed] [Google Scholar]
- 11. Constant C, Murley A. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 12. Duquin TR, Buyea C, Bisson LJ. Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med. 2010;38(4):835–841. [DOI] [PubMed] [Google Scholar]
- 13. Godfrey J, Hamman R, Lowenstein S, Briggs K, Kocher M. Reliability, validity, and responsiveness of the simple shoulder test: psychometric properties by age and injury type. J Shoulder Elbow Surg. 2007;16(3):260–267. [DOI] [PubMed] [Google Scholar]
- 14. Hein J, Reilly JM, Chae J, Maerz T, Anderson K. Retear rates after arthroscopic single-row, double-row, and suture bridge rotator cuff repair at a minimum of 1 year of imaging follow-up: a systematic review. Arthroscopy. 2015;31(11):2274–2281. [DOI] [PubMed] [Google Scholar]
- 15. Hollinshead RM, Mohtadi NG, Guchte RAV, Wadey VM. Two 6-year follow-up studies of large and massive rotator cuff tears: comparison of outcome measures. J Shoulder Elbow Surg. 2000;9(5):373–379. [DOI] [PubMed] [Google Scholar]
- 16. Kim DH, ElAttrache NS, Tibone JE, et al. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med. 2006;34(3):407–414. [DOI] [PubMed] [Google Scholar]
- 17. Kim JR, Cho YS, Ryu KJ, Kim JH. Clinical and radiographic outcomes after arthroscopic repair of massive rotator cuff tears using a suture bridge technique: assessment of repair integrity on magnetic resonance imaging. Am J Sports Med. 2012;40(4):786–793. [DOI] [PubMed] [Google Scholar]
- 18. Kim KC, Shin HD, Cha SM, Park JY. Comparisons of retear patterns for 3 arthroscopic rotator cuff repair methods. Am J Sports Med. 2014;42(3):558–565. [DOI] [PubMed] [Google Scholar]
- 19. Lafosse L, Lanz U, Saintmard B, Campens C. Arthroscopic repair of subscapularis tear: surgical technique and results. Orthop Traumatol Surg Res. 2010;96(suppl 8):S99–S108. [DOI] [PubMed] [Google Scholar]
- 20. Lee KW, Seo DW, Bae KW, Choy WS. Clinical and radiological evaluation after arthroscopic rotator cuff repair using suture bridge technique. Clin Orthop Surg. 2013;5(4):306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mazzocca AD, Millett PJ, Guanche CA, Santangelo SA, Arciero RA. Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med. 2005;33(12):1861–1868. [DOI] [PubMed] [Google Scholar]
- 22. Mihata T, Watanabe C, Fukunishi K, et al. Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med. 2011;39(10):2091–2098. [DOI] [PubMed] [Google Scholar]
- 23. Neyton L, Godenèche A, Nové-Josserand L, Carrillon Y, Cléchet J, Hardy MB. Arthroscopic suture-bridge repair for small to medium size supraspinatus tear: healing rate and retear pattern. Arthroscopy. 2013;29(1):10–17. [DOI] [PubMed] [Google Scholar]
- 24. Nho SJ, Brown BS, Lyman S, Adler RS, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elbow Surg. 2009;18(1):13–20. [DOI] [PubMed] [Google Scholar]
- 25. Ostrander RV III, McKinney BI. Evaluation of footprint contact area and pressure using a triple-row modification of the suture-bridge technique for rotator cuff repair. J Shoulder Elbow Surg. 2012;21(10):1406–1412. [DOI] [PubMed] [Google Scholar]
- 26. Ostrander RV III, Smith J, Saper M. Triple-row modification of the suture-bridge technique for arthroscopic rotator cuff repair. Arthrosc Tech. 2016;5(5):e1007–e1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun B-J, Lee TQ. Part I: footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16(4):461–468. [DOI] [PubMed] [Google Scholar]
- 28. Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun B-J, Lee TQ. Part II: biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16(4):469–476. [DOI] [PubMed] [Google Scholar]
- 29. Park S-G, Shim B-J, Seok H-G. How much will high tension adversely affect rotator cuff repair integrity? Arthroscopy. 2019;35(11):2992–3000. [DOI] [PubMed] [Google Scholar]
- 30. Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;254:81–86. [PubMed] [Google Scholar]
- 31. Richards RR, An K-N, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg.1994;3(6):347–352. [DOI] [PubMed] [Google Scholar]
- 32. Rousseau T, Roussignol X, Bertiaux S, Duparc F, Dujardin F, Courage O. Arthroscopic repair of large and massive rotator cuff tears using the side-to-side suture technique: mid-term clinical and anatomic evaluation. Orthop Traumatol Surg Res. 2012;98(4):S1–S8. [DOI] [PubMed] [Google Scholar]
- 33. Trantalis JN, Boorman RS, Pletsch K, Lo IK. Medial rotator cuff failure after arthroscopic double-row rotator cuff repair. Arthroscopy. 2008;24(6):727–731. [DOI] [PubMed] [Google Scholar]
- 34. Ware JE, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. [DOI] [PubMed] [Google Scholar]
- 35. Wright RW, Baumgarten KM. Shoulder outcomes measures. J Am Acad Orthop Surg. 2010;18(7):436–444. [DOI] [PubMed] [Google Scholar]
- 36. Yamakado K, Katsuo S-i, Mizuno K, Arakawa H, Hayashi S. Medial-row failure after arthroscopic double-row rotator cuff repair. Arthroscopy. 2010;26(3):430–435. [DOI] [PubMed] [Google Scholar]