Abstract
Objectives
Art therapy has been widely used in clinical settings and has shown preliminary success in military trauma. This case study describes a mask‐making art therapy directive facilitated by a board‐certified art therapist as an adjunct to group posttraumatic stress disorder (PTSD) treatment in a military‐intensive outpatient program.
Methods
Described are clinical outcome measures, linguistic analysis of a personal journal, evaluation of this service‐member's artwork, and experiences in the program.
Results
Mask‐making, as a trauma‐focused group‐art therapy directive, expanded the understanding of treatment progress reflected in journal notes, mask imagery, and by a change in linguistic indices of trauma processing, despite an overall increase in PTSD symptoms as he confronted his traumatic experiences. He reported improvement in coping and successfully returned to full military duty following treatment.
Conclusions
This case study suggests that art therapy and written narrative, combined with standardized self‐report assessments, may more accurately indicate improvement in overall PTSD treatment.
Keywords: art therapy, LIWC, military, posttraumatic stress disorder, trauma
During and following World Wars I and II, practitioners in the United States and abroad acknowledged the therapeutic value of the creative expression for convalescing soldiers and veterans psychologically traumatized by war (Howie, 2017). Although many names have been given to describe symptoms attributed to combat and non‐combat‐related trauma experiences, such as shell shock, cardiorespiratory neuroses, battle exhaustion, traumatic neurosis, and combat fatigue, by 1980, the constellation of symptoms—intrusive re‐experiencing, avoidance, numbing, and hypervigilance, was termed posttraumatic stress disorder (Crocq & Crocq, 2000; Ramirez, 2016). The body of literature reflects that the creative art therapies, including art therapy, dance/movement therapy, drama therapy, and music therapy, as well as expressive writing, provide a pathway to reduce functional and psychological impairment related to posttraumatic stress disorder (PTSD) through the process of expression, containment and externalization of emotions, meaning‐making, and integration of fragmented memories (Campbell, Decker, Kruk, & Deaver, 2016; Decker, Deaver, Abbey, Campbell, & Turpin, 2018; Jones, Walker, Drass, & Kaimal, 2018; Kaimal, Walker, Herres, French, & DeGraba, 2018; Ramirez, 2016). Furthermore, nonverbal creative expression in the context of therapy facilitates the reintegration of sensory with verbal memories more effectively than verbalization alone. Lobban and Murphy (2017) proposed that art therapy may bypass avoidant coping strategies which frequently stall recovery when using recommended first‐line trauma‐focused verbal therapies such as cognitive behavioral therapy, cognitive processing therapy (CPT), prolonged exposure, and eye movement and desensitization reprocessing.
Mask‐making, as an art therapy directive, is a widely used technique for exploring difficult emotions and self‐perceptions (Howie, 2017; Jones et al., 2018; Walker, Kaimal, Gonzaga, Myers‐Coffman, & DeGraba, 2017). Among indigenous tribal communities, such as the Alaskan Yup'ik people, masks are created to explore and share healing stories of human experience (Kawagley, 1990). These masks frequently portray peace, harmony, anger, remorse, the power of intuition, and the emergence of inner wisdom from the unconscious mind. Walker, Kaimal, Koffman, and DeGraba (2016) suggest similar intent when introducing mask‐making to service members struggling with PTSD‐related fear, confused identity, and existential questions associated with combat and other experienced traumas. Mask‐making occurs during group‐art therapy scheduled the first week of a 4‐week intensive outpatient program at the National Intrepid Center of Excellence (NICoE) in Bethesda, MD, a multidisciplinary treatment program for TBI and PTSD (Walker et al., 2016). Mask‐making, in a group‐art therapy setting, fostered a safe environment for military service members with similar trauma‐related experiences to create and share imagery and stories. An outside analysis of the resultant masks suggested references to physical and psychological suffering, relationship to self and others, and connection to all beings based on patient descriptions of completed mask imagery and the mask‐making process (Walker et al., 2017). Lobban (2017) compared mask themes created by veterans with chronic PTSD diagnoses at the beginning and at the end of 12 group‐art therapy sessions spread over a 5–9‐month time period. Participants interpreted the mask concept using a variety of art materials and techniques, such as natural materials, clay, and drawing media, rather than using a mask form. Using direct observation of art‐making, image analysis, self‐report measures, verbal communication, and written reflections of two veterans who had completed the series, Lobban (2017) discovered evidence of change, including reduction of avoidant coping behavior, recognition of cognitive distortion about self‐concepts, and increased emotional tolerance.
Lobban (2017) further posited that art therapy seemed to improve PSTD symptoms by circumventing avoidant and other protective defense behaviors, allowing for the exploration of emotions and reprocessing of traumatic memories with cognitive restructuring. This may explain the rationale for the inclusion of art therapy within group‐CPT for military PTSD populations enrolled in intensive outpatient programs (Hoyt et al., 2018; Zalta et al., 2018). CPT was developed for the treatment of PTSD and is a preferred evidence‐based treatment for military populations (Gallagher & Resick, 2012; Lenz, Bruijn, Serman, & Bailey, 2014). The intended outcome for CPT seems to align with Lobban's (2017) findings using art therapy for PTSD in regard to the restructuring of cognitive distortion and the trauma narrative through verbal and imaginal review of the traumatic incident, resulting in restoration of hope and personal sense of agency (Gallagher & Resick, 2012; Resick, 2001). It is interesting to note that secondary symptoms related to PTSD, including guilt, shame, social disconnection, and negative health perceptions (Lenz et al., 2014), have been commonly represented in mask imagery and associated narratives (Walker et al., 2017).
Participant reports and psychometric measures suggest decreased anxiety and improved overall resilience (Kaimal et al., 2018; Walker et al., 2017). Campbell et al. (2016) cited positive participant satisfaction scores following a combination of CPT with a trauma‐focused individual art therapy protocol over CPT alone, reporting participant feedback to include improved trauma processing with decreased avoidance and distressing sensory responses and improved insight. Decker et al. (2018) reported similar findings in a randomized study of military service members receiving CPT with adjunctive art therapy during individual treatment, utilizing a multidirective, visual trauma narrative approach compared to individuals receiving CPT and supportive psychotherapy. Statistically significant improvements in the reduction of PTSD symptoms and depression were noted and participants rated art therapy as more beneficial than CPT. The current study sought to add to the current literature by focusing on a group therapy intervention with a single art directive, integrated into intensive outpatient treatment utilizing CPT.
Whereas art therapy appears to be a valuable therapeutic adjunct to trauma‐focused therapies within many clinical populations, including military service members and veterans with PTSD, empirical evidence to support the efficacy of art therapy for PTSD is limited and complex (Baker, Metcalf, Varker, & O'Donnell, 2018). Variability in modes of intervention approaches, methods, and theoretical framework differences cause research challenges in regard to measuring change directly related to art therapy for PTSD treatment (Foundation for Arts & Healing, 2011). Baker et al. (2018) suggest a need for well‐designed scalable trials to more clearly connect art therapy to mechanisms of change, perhaps through collaboration with an interdisciplinary team of researchers. This case study presents an example of art therapy and psychology cotreatment for PTSD, using a single art therapy directive over the course of a group intensive outpatient trauma program.
Over the past 20 years, there have been several iterations of intensive outpatient programs (IOP) that have addressed military‐related posttraumatic stress disorder (e.g., Engel, Roy, Kayanan & Ursano, 1998; Lande, Williams, Francis, Gragnani, & Morin, 2011). Intensive outpatient programs are typically a higher level of care than outpatient treatment with patients attending several group or individual sessions per week (Timko, Sempel, & Moos, 2003). In the military setting, an IOP may be preferable to inpatient treatment or long‐term outpatient treatment as a means to limit lost training time (Lande & Pourzand, 2016). The intent of the current case study is to illustrate the utilization of a trauma‐focused art‐based intervention to augment intensive outpatient treatment for posttraumatic stress disorder. The current study examines clinical data, personal journal notes, mask sketches, and the completed mask of an Active Duty service‐member while participating in a 6‐week, PTSD track within a group‐based intensive outpatient treatment program.
1. METHOD
1.1. Patient background
Chief Echo (patient pseudonym) was a 47‐year‐old, married, heterosexual man currently on active duty in the Navy and holding the rank of Senior Chief Petty Officer, a high‐ranking, enlisted officer. Throughout his 23 years of service, Chief Echo had experienced several traumatic events during approximately 80 months of total combat‐related deployments. This military experience notwithstanding, the majority of traumatic life events and PTSD symptoms endorsed by Chief Echo were due to a significant history of physical and emotional abuse during his upbringing in an orphanage. Chief Echo originally presented for outpatient treatment approximately 10 months before enrollment in the current intensive outpatient treatment program, receiving intermittent care for trauma‐related symptoms with a diagnosis of unspecified trauma disorder. However, Chief Echo desired care in a dedicated setting that would allow him to focus on recovery. As a result, Chief Echo was referred to the intensive outpatient program at Madigan Army Medical Center.
1.2. Treatment setting
Chief Echo enrolled in two sequential courses of intensive outpatient group‐based treatment (see Hoyt et al., 2018 for a complete description of this program). First, he was enrolled in a 4‐week Skills and Resiliency Treatment Program (SRT; 5 days/week, at least 3 hr of intervention daily) focused on increasing coping skills and overall emotion regulation. These 4 weeks initially emphasized his own goals to “reduce anger in communicating with other people” and “learn how to deal with [his] stress” on a daily basis. Furthermore, this initial skills‐based program was intended to increase distress tolerance so that Chief Echo could better engage in PTSD treatment, the second component of his enrollment in the intensive outpatient program (Hoyt, Rielage, & Williams, 2012). After completing the SRT track, he had a break in care for 2 weeks before returning to the PTSD track of the intensive outpatient program. This intervention was a closed‐cohort, 6‐week treatment program (5 days/week, at least 3 hr of intervention daily) primarily utilizing group‐based trauma therapy led by a psychologist and social worker with significant formal training in Cognitive Processing Therapy (e.g., Resick et al., 2015). As part of the PTSD track, Chief Echo also participated in a weekly 90‐min group‐art therapy intervention within the program, led by a board‐certified art therapist. Given Chief Echo's geographic separation from his family for the duration of these programs, he was housed in a private room at the wounded warrior barracks.
1.3. Art therapy intervention
A 90‐min mask‐making group‐art therapy directive was provided each Friday during the first 4 weeks of the intensive outpatient program PTSD track and concluded with group verbal processing during Week 5. The mask‐making theme provided a secure structure to safely begin the creative process while maintaining an open‐ended, nondirective approach for exploring personal concepts and stories (Lobban, 2017). There were no content or theme restrictions. Each participant was offered one papier‐mâché mask form at the first art therapy session along with paint, air‐dry clay, and a variety of collage materials. Participants were instructed to use any portion of the mask, outside and inside surfaces, and encouraged to add materials of personal importance to the mask in addition to media provided, if desired. Additional mask forms were available upon request. Participants were informed that the mask project would progress over several weeks, culminating with group narrative‐processing of the art‐making experience and applied meaning at the final art therapy session. Masks were stored in the meeting room throughout the duration of the treatment program. Following the art therapy group‐processing session during Week 5 of the PTSD track, Chief Echo revealed to the art therapist that he had been keeping personal journal notes, including embedded sketches of his mask throughout the trauma groups. Sketches were drawn in the journal from memory both following an art therapy session and in advance of future sessions with written descriptions of visual elements.
1.4. Measures
Throughout his enrollment in the intensive outpatient program, Chief Echo completed the following symptom measures and other assessments of current functioning (see Table 1).
Table 1.
Psychological test scores during the skills and resiliency track, PTSD track, and at 1‐month follow‐up
| BASIS‐24 | PCL‐5 | PHQ‐9 | |
|---|---|---|---|
| Intake to SRT | 0.84 | – | – |
| Week 1 of SRT | 1.06 | 19 | – |
| Week 4 of SRT | 1.42 | 16 | – |
| Week 5 of SRT | 1.85 | 21 | – |
| Week 6 of SRT | 1.80 | – | 15 |
| Week 7 of SRT | 1.10 | – | 11 |
| Week 1 of PTSDT | 1.44 | 16 | 10 |
| Week 2 of PTSDT | 1.92 | 42 | 17 |
| Week 3 of PTSDT | 1.34 | 31 | 13 |
| Week 6 of PTSDT | 1.64 | 49 | 17 |
| Follow‐up Post PTSDT | – | 29 | 17 |
Note: Dashes indicate when specific test data was not collected.
Abbreviations: BASIS‐24, Behavior and Symptom Identification Scale‐24 Overall Score; PCL‐5, PTSD Checklist for DSM‐5; PHQ‐9, Patient Health Questionnaire‐9; PTSDT, posttraumatic stress disorder track; SRT, skills and resiliency track.
1.4.1. PTSD symptoms
PTSD symptoms were measured using the PTSD Checklist for DSM‐5 (PCL‐5; Blevins, Weathers, Davis, Witte, & Domino, 2015). The PCL‐5 is a 20‐item self‐report measure that indexes PTSD symptom severity based on DSM‐5 criteria, with each item rated on a 0–4 scale ranging from “Not at all” to “Extremely.” Total scores on the PCL‐5 range from 0 to 80, and psychometric validation in service‐member samples recommended a clinical cutoff score of 33 (Wortmann et al., 2016). Previous studies on this measure have shown good internal consistency, test–retest reliability, and convergent validity with other measures of PTSD symptoms (Blevins et al., 2015). Chief Echo completed the PCL‐5 eight times during his 10‐week treatment at the intensive outpatient program.
1.4.2. General distress
General distress was measured using the Behavior and Symptom Identification Scale (BASIS‐24; Eisen, Normand, Belanger, Spiro, & Esch, 2004). The BASIS‐24 is a 24‐item self‐report scale indexing overall distress (e.g., “During the past week, how much difficulty have you had coping with problems in your life?”). Each item is rated on a scale from 0 (not stressful or frequent) to 4 (highly stressful or frequent); average item scores provide an index of general distress. Previous studies have demonstrated that the BASIS‐24 has good internal consistency, test–retest reliability, and convergent validity with other measures of global mental health (Eisen, Gerena, Ranganathan, Esch, & Idiculla, 2006). Chief Echo completed the BASIS‐24 weekly during his 10‐week treatment at the intensive outpatient program.
1.4.3. Depression
Co‐morbid symptoms of depression were measured using the Patient Health Questionnaire (PHQ‐9; Kroenke, Spitzer, & Williams, 2001). The PHQ‐9 is 9‐item scale indexing symptoms of depression on a scale of 0 (not at all) to 3 (nearly every day). PHQ‐9 total scores range from 0 to 27; PHQ scores greater than 10 are indicative of major depression (Kroenke et al., 2001). Previous studies on the measure in service members have shown good psychometric properties (e.g., Reger, Gahm, Swanson, & Duma, 2009). Chief Echo completed the PHQ‐9 seven times during his 10‐week treatment at the intensive outpatient program.
1.4.4. Narrative analysis
Chief Echo's trauma narratives and self‐directed journal activities completed during the PTSD track of the intensive outpatient program were analyzed using the Linguistic Inquiry and Word Count (LIWC 2015) software (Pennebaker, Boyd, Jordan, & Blackburn, 2015). This software examines the occurrence of various words in text samples and can measure a variety of cognitive and affective processes through language use. The LIWC software has been utilized in a number of previous studies as a measure of processing associated with traumatic events (Hoyt & Yeater, 2011), including within military samples (Hoyt & Pasupathi, 2008). For the current case study, the Analytical thinking, Clout, Authenticity, Tone, I‐words, Positive emotion, Negative emotion, and Insight categories in the LIWC software were used to measure cognitive and affective changes in Chief Echo's writing throughout the treatment program. These categories were chosen based on previous literature related to linguistic processing following a traumatic event (e.g., Tani, Peterson, & Smorti, 2016).
2. RESULTS
2.1. PTSD symptoms
At initial intake to the intensive outpatient program, Chief Echo endorsed minimal symptoms of PTSD on the PCL‐5, with a total score of 19 that was well below the clinical cutoff of 33 (Wortmann et al., 2016). He endorsed only moderate symptoms in the areas of self‐blame, anhedonia, difficulty experiencing positive emotions, irritability, hypervigilance, and difficulty concentrating. Regarding the subjective description of his traumatic events, he reported frequent thoughts about bombs and explosions, including ruminating on whether explosive devices may be hidden in common areas. This low‐level endorsement of PTSD symptoms continued until the beginning of the PTSD track, with scores ranging from 16 to 21 on the PCL‐5. Following the first week of the PTSD group, Chief Echo endorsed significantly higher symptoms of PTSD in the clinical range, with a score of 42 on the PCL‐5. One hypothesis for this perceived spike in PTSD symptoms is that the group engagement provided the first opportunity to confront his history of both military and childhood traumatic events, as well as greater awareness of his own symptoms. By the midpoint of the group, his score on the PCL‐5 had decreased to 31, below the clinical range. However, at program discharge, his score had again increased to 49. This included a significant endorsement of emotional and physical responses related to traumatic memories, strong negative emotions, anhedonia, and insomnia. Other patients from this program have shown similar increases in symptoms at discharge, often due to anxiety about returning to full duty. Approximately 1 month following discharge from the intensive outpatient program, Chief Echo reported a score of 29 on the PCL‐5. This suggested that he had been able to generalize what he had learned in the treatment program to his daily military duties. Note that he reported significantly higher symptoms of PTSD following program completion than at intake.
2.2. Overall distress
Mirroring his endorsement of symptoms on the PCL‐5, Chief Echo similarly endorsed minimal distress on the BASIS‐24 at program intake, with a score of 0.8. By the midpoint of the SRT track, he indicated an increase in distress to a BASIS‐24 score of 1.8, with prominent feelings of depression, racing thoughts, mood swings, and a loss of self‐confidence. Overall distress similarly peaked at the midpoint of the PTSD track, with a total BASIS‐24 score of 1.9 and prominent endorsement of difficulty concentrating, ongoing depression, feeling nervous, racing thoughts, mood swings, and feeling short‐tempered. By the end of the PTSD track, the total BASIS‐24 score had decreased slightly to 1.6.
2.3. Depression
Chief Echo's endorsement of depression symptoms was consistent throughout the treatment program, with scores on the PHQ‐9 ranging from 10 to 17. This included a prominent endorsement of appetite changes, insomnia, fatigue, and anhedonia. Indeed his score at intake (PHQ = 15) was very similar to his score at program completion (PHQ = 17). Regarding Chief Echo's risk of suicide, during program intake, he endorsed a history of three episodes of suicide behavior during the past year, including suicidal thoughts with intent and a suicide plan, but no occurrences during the past 3 months. Chief Echo subsequently denied any suicidal ideation or behaviors at all 10 subsequent screenings administered during enrollment in the intensive outpatient program.
2.4. Art therapy
Although the interpretation of artwork by the art therapist is typically secondary to the client's description and meaning, art therapists are trained to view created images from imaginal and symbolic perspectives including content, structure, process, and how art media is applied to generate metaphorical language and meaning (Abbenante & Wix, 2016). The following subjective interpretation of Chief Echo's artwork is informed by the expertise of a board‐certified art therapist, based on direct work with Chief Echo in facilitating the art therapy group.
2.4.1. Week 1
Chief Echo embedded a sketch of his mask (see Figure 1) in his personal journal following art therapy at the end of the first week of the PTSD group. In his written notes, he recalled paint color choices and placement, textures, and the clockwise direction in which he applied media to the mask. There was no explanation about color symbolism, only that the upper right color was described as “silver” and “gunmetal gray.” Assuming he worked in the clockwise direction as he described, metallic colors suggest a need for self‐protection, as if wearing armor. Color choice transitioned to orange on the right lower quarter of the mask, including jagged orange marks layered over the gray color. The remaining half was completely painted bright red, with the placement of a “horn on the head” created from air‐dry clay. Chief Echo wrote that he intended to paint the horn black. The mask portrayed a split representation, with half of the mask that seems to represent a devilish scheme. The dark blue lip suggested emotional variability from one half which appears as a neutral or concealed expression, to a slight smile on the other half, supported by Chief Echo's co‐occurring journal entry in which he describes conflicted emotions. On the inner portion of the mask, the eye area was covered with steel wool. The top one‐third of the inside area of the mask was painted the same shade of blue as was used on the lip area. It is reasonable to assume Chief Echo was expressing a need to establish safety (Herman, 1997) by concealing and revealing only what felt comfortable in the moment.
Figure 1.

Mask design progression from patient journal
2.4.2. Week 2
Following the second art therapy session, Chief Echo added two sketches to his personal journal depicting the exterior and interior views of the mask. He wrote that he “enjoyed updating the mask,” with additional comments to suggest active engagement in creative and cognitive processing outside of the therapeutic group setting. Chief Echo defined the red color as “devil red” assigning symbolic value or meaning to color choice. A small dowel and wire object were added below the mask nose, which he associated in his writing to a childhood memory from a time prior to entry into the orphanage. Chief Echo spread white glue across the mask exterior which, when dried, created the appearance of what he described as “peeling skin,” a metaphor indicating a sloughing process was occurring (see Figure 2). Concurrent journal entries revealed increased interest and participation in social engagement activities.
Figure 2.
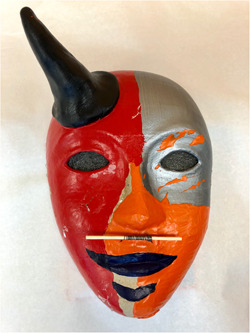
Exterior view of completed mask [Color figure can be viewed at wileyonlinelibrary.com]
2.4.3. Week 3
Chief Echo created another sketch outside of group‐art therapy and described in his journal decisions to transition from painting the mask form to creating objects within the interior of the mask. The inside of the mask (see Figure 3) became a container to symbolically represent more vulnerable aspects of his identity and emotions related to present experiences and past trauma‐related psychological injury. Chief Echo glued a small cotton ball at the highest point of the mask interior over blue paint described in his journal as “sky blue” representing “tranquility and peace within,” something he longed for. He spelled out the words “buried treasure and memories” in the lowermost area of the sketch over an unpainted mask area, possibly parts of his trauma and identity he wished to avoid. Over the top of this area, Chief Echo described his intention to create TNT barrels, including plans to use clay and collage materials to create fuses as a visual representation of his experience with emotional triggers (“paying respect to my emotional hot buttons” and what “sets me into explosive mood swings”). He identified the steel wool, which had been placed inside the mask in the first week of art therapy, as “thoughts” and spelled out “Problem Child” using letter beads strung on the wire attached to the steel wool. It is plausible that Chief Echo used visual symbols to engage in reprocessing memories and attempt to reintegrate traumatic events (Herman, 1997). Chief Echo created another drawing in his journal between the third and fourth art therapy sessions. His writing focused on his emotional response to a fellow group member's story and artwork. Chief Echo's sketch featured a rendering of his exterior facing mask attached to a display on a “small mirrored turntable,” and his text indicated he was interested in ways he could share the mask with others, a “conversation piece” as described in his journal. He wrote about conversations he had with his spouse, “…talking about my mask for a while. I've been explaining it for a long while.” He seemed interested in revealing parts of himself and his trauma in an effort to connect with others (Herman, 1997).
Figure 3.

Interior view of completed mask [Color figure can be viewed at wileyonlinelibrary.com]
2.4.4. Week 4
Before the art therapy session Chief Echo created a sketch of the created components within his mask, surrounded by a detailed written description of the intended meaning. He wrote about having a greater awareness of his moods and related past trauma to new insight and meaning. He labeled the drawing details and explained their meaning:
Army Figurine: “comms guy,” likely a reference to military service
Mirror: reflection to those “looking inside my head”
String of letter beads, spelled words “wait,” “feel,” “terror,” “cruelty,” and “hate:” “words that are clear in my mind”
Stickers of words “Fearless, Strong:” perhaps indicating a willingness to take a risk and recognition of personal strength and resilience “in my deep foundation”
Monster leg: may represent trauma “under my conflicted reasoning soul, I have Godzilla lurking there”
Fuses attached to TNT barrels: may represent mood swings from tranquil to explosive
Unattached fuses: a self‐described change in meaning from original intent as emotional triggers to “nerve bundles…fed by past experiences and some overt tragedy and some horror”
Chief Echo drew sketches of a tiny journal, a microphone, microscope, and magnifying glass noting that he intended to add more symbols to the mask before the final art therapy session during Week 5. He wrote in his journal about a “great conversation” with the art therapist, which involved verbal reflections about his mask and feeling positive regard toward the art therapist, confirming a therapeutic relationship had been established. He also disclosed a need for belongingness and acceptance in his journal and described attempts to connect to others through conversation, social gatherings, and personal letters. Chief Echo inscribed the pages of his tiny journal which was attached to the center area of the mask interior over the steel wool representative of his “thoughts,” acknowledging the importance of self‐expression through journal writing.
2.5. Narrative analysis
Over the course of the 6‐week IOP PTSD track and for a period of 1 month after completion of the IOP, Chief Echo wrote multiple entries in his personal journal. These journal entries were transcribed and then analyzed using the LIWC program. Tables 2 and 3 present data representing selected LIWC findings that pertain to psychotherapy processes for each week and for the follow‐up period of time. Ample word counts were obtained for weekly and follow‐up data ranging from 1,090 to 3,798 words for each segment analyzed.
Table 2.
LIWC summary language variable results during the PTSD track
| Segment analyzed | Analytical thinking | Clout | Authenticity | Tone |
|---|---|---|---|---|
| Week 1 | 57.65 | 51.76 | 53.40 | 26.81 |
| Week 2 | 61.46 | 26.90 | 78.51 | 52.75 |
| Week 3 | 53.28 | 54.91 | 51.65 | 38.91 |
| Week 4 | 57.44 | 38.52 | 51.62 | 35.98 |
| Week 5 | 51.84 | 30.74 | 67.07 | 17.62 |
| Week 6 | 53.53 | 65.69 | 41.01 | 30.41 |
| Follow‐up post PTSDT | 55.44 | 50.00 | 57.85 | 18.66 |
Note: Summary variable data above are composite scores that range from 0 to 100 with higher scores representing a higher level of the dimension measured.
Abbreviations: LIWC, linguistic inquiry and word count; PTSDT, posttraumatic stress disorder track.
Table 3.
LIWC linguistic, psychological, and cognitive process variable results during the PTSD track
| Segment analyzed | I‐words | Positive emotion | Negative emotion | Insight |
|---|---|---|---|---|
| Week 1 | 6.42 | 2.01 | 1.95 | 1.51 |
| Week 2 | 8.83 | 3.01 | 1.57 | 1.30 |
| Week 3 | 7.08 | 3.05 | 2.32 | 1.24 |
| Week 4 | 7.45 | 2.91 | 2.33 | 2.27 |
| Week 5 | 9.19 | 1.72 | 2.28 | 2.08 |
| Week 6 | 7.16 | 2.48 | 2.20 | 2.02 |
| Follow‐up post PTSDT | 6.92 | 1.62 | 2.10 | 1.44 |
Note: Values entered in this table represent the percentage of total words that fall into each category in the LIWC dictionary.
Abbreviations: LIWC, linguistic inquiry and word count; PTSDT, posttraumatic stress disorder track.
Analytical thinking reflects a person's use of logical or formal language use of communication versus a more informal or narrative approach (Pennebaker, Chung, Frazee, Lavergne, & Beaver, 2014). This patient's writing reflects a balance between the two throughout the duration of the PTSD track and thereafter. Changes are shown however the dimension of clout (an indicator of presenting with confidence and a sense of certainty) decreased during the same Week 5 of the PTSD track that saw a significant increase in written language that manifests authenticity (showing greater genuineness and personal contemplation) of communication. In terms of psychotherapy change processes, this patient may be experiencing potential psychological insights as reflected in his journal writing and possibly revealing a sense of vulnerability. This notion is further underscored with his general emotional tone (low scores associated with negative emotions) being fairly negative which may be a clinical marker for emotional pain associated with these psychological insights. By Week 6, a reversal of clout and authenticity is seen with increased confidence and certainty reflected in his writings though perhaps less personal. This latter finding may be common to those completing an episode of psychotherapy where closure and leaving on a more upbeat emotional note, as shown in the increased emotional tone score, may be characteristic.
Of the many personal pronouns that have gained attention in Pennebaker's research, the first‐person pronoun, or “I,” holds significant psychological value. Those who experience psychological or physical distress tend to focus attention inward, and this is often associated with greater usage of the first‐person pronoun (Rude, Gortner, & Pennebaker, 2004). The use of this I‐talk, as noted by Tackman et al. (2019), is associated with a proneness towards general distress. Chief Echo demonstrated an increased use of I‐talk as well as his lowest usage of positive emotion words during his writings at Week 5. These findings also occur within the context of generally increased usage of words that are associated with psychological insight which appears to be more common during the second half of this patient's participation in the PTSD track. This is also consistent with the findings discussed above regarding possible increased depth of creative self‐reflection and contemplation at this stage of the intensive outpatient program. There is also a trend toward Chief Echo's writing having slightly more negative emotional content approximately 3 weeks into the PTSD group and this may be consistent with the nature of trauma‐based therapy in which stressful memories are processed through primarily cognitive‐behavioral strategies.
3. DISCUSSION
This case review of Chief Echo's clinical assessments, personal journal notes with sketches, and the completed mask provided compelling insight into his cognitive and creative processes during the group intensive outpatient trauma treatment program, and structure for understanding the inter‐relatedness of visual and narrative data with linguistic analysis and self‐report measure scores. Self‐report measures provided a clinical context, whereas linguistic and mask analysis focused on Chief Echo's organically written narrative of his experience.
In contrast to previous studies which relied on clinical notes, interviews and coding methods to understand a patient's experience in trauma therapy, this case highlights data directly provided by Chief Echo through disclosure of personal journal notes and sketches to the art therapist at the conclusion of the final art therapy session. His unredacted written and visual narrative proved valuable for understanding his response to trauma treatment, most notably during Week 5 of the PTSD track. It appeared that Chief Echo was able to bypass avoidant behavior as his mask‐making effort progressed from attention to the self‐protective exterior mask portion during the first two art therapy sessions to extensive focus on symbols and words contained within the mask interior; representations of traumatic memories and associated emotionality (Lobban, 2017; Wise & Nash, 2013). From a constructivist art therapy perspective, it seemed that Chief Echo engaged in trialing a range of creative interpretation and meaning of mask imagery during and between art therapy sessions as evidenced by corresponding notes (Matto, 1998). This sustained level of originative thinking through visual art and writing combined with CPT facilitated objective observation of thoughts and feelings, the construction of adaptive expressions, and references to surviving behaviors which may have contributed to an improved sense of meaning and control and arguably improved resilience (Norman, 2000). Indeed, metaphor use in art therapy may reduce the emotional effect of traumatic memories, allowing safe distance for deeper exploration (Wise & Nash, 2013). Bruner (1990) similarly posited that symbolic and metaphoric activities provide a means to organize experience and frame structure for negotiating and internalizing self‐concepts thus forming a more authentic narrative. The reconstruction process shapes one's experiential reality by moving from a sense of victimhood to personal agency through the achievement of internal and external coherence, livability, and adequacy (Bruner, 1990). Chief Echo employed mask imagery to create a metaphoric visual narrative, both internalized and externalized, integrated in such a way that he was able to more effectively verbalize insight about his trauma experience to his spouse, the trauma therapists, and fellow group members (Jones, Drass, & Kaimal, 2019).
Interestingly, there appeared to be some incongruence of Chief Echo's recovery progress between self‐reporting through journal notes and observation, and the results of the psychological self‐report data. Although Chief Echo reported an overall increase in PTSD symptoms, he subjectively reported significant improvement in functioning and ability to cope with these symptoms, and successfully returned to duty following treatment. Indeed, symptom reporting, in this case, may not have been the best index of recovery for Chief Echo. According to Meichenbaum (2017) treatment outcomes often may be due to other factors such as the therapeutic alliance and deliberate practice of cognitive processing skills as well as ownership of one's narrative. Active engagement in group‐art therapy within manualized trauma treatment enabled Chief Echo to practice cognitive processing in a creative nonverbal form, and empower him to take ownership of his personal narrative, as reflected in his journal notes (Decker et al., 2018). The impact of multiple sources of data, such as the inclusion of nonverbal strategies (e.g., art therapy and written narratives) with standardized self‐report measures, may have more potential as a method to more accurately monitor overall improvement in clinical care (Pedersen, 2016). Better recognition of an individual's experience can improve the therapeutic alliance, reshape treatment goals through the shared interpretation of motivation to change, and guide longitudinal care decisions (Jones et al., 2019).
A unique feature of this case study is the use of mask‐making as a singular art directive for the duration of the trauma program. Although mask‐making has been included as part of multidirective trauma‐focused art therapy programs (Decker et al., 2018; Jones et al., 2019), there are no known examples of mask‐making as an exclusive art therapy directive within a PTSD track of an intensive outpatient program. The progressive mask‐making concept has been embedded within the Madigan Army Medical Center IOP PTSD track program since 2017 and grew out of a collaboration between psychotherapists facilitating the IOP PTSD track and the art therapist. Chief Echo, as with other trauma track group participants, was allotted more than 6 hr total time to complete his mask during the IOP before the final group‐art therapy verbal processing session. Talwar (2007) postulated that improved PTSD functioning using creative therapies requires the integration of cognitive, emotional, and physiological memory. It appears that progressive mask‐making allows sufficient time for the integration process to occur, particularly when combined with a manualized trauma curriculum. In fact, in a systematic review of the effectiveness of art therapy in trauma treatment (Schouten, de Niet, Knipscheer, Kleber, & Hutschemaekers, 2015) and a randomized controlled study (Decker et al., 2018) found that decrease of trauma symptom severity was greatest among those in which art therapy was used in combination with psychotherapy. This suggests that further research is needed on the integration of art therapy into group trauma‐focused treatment.
Several limitations of the current case study suggest directions for future research. As a case study, Chief Echo's experience may not generalize to other patients engaged in similar tasks. Although outcomes from this specific IOP with an art therapy component have shown positive results in previous research (Hoyt et al., 2018), more specific research is needed on the therapeutic value of trauma‐focused art tasks, such as those described herein. Furthermore, the inconsistency between self‐report symptom measures and other indices of trauma recovery in the current case suggested that additional research is needed relating to reconciling the therapeutic value of narrative and art therapy interventions with reported clinical symptomatology. The current study also was limited by some inconsistency in the program collecting outcome measures, due to both technical and administrative limitations at the time. Future work in this area may need to collect more systematic outcomes in a larger cohort to better demonstrate effectiveness. It also is important to note that Chief Echo has practiced personal journal writing for many years, most of which has not been shared publicly. Thus, it is unclear to what degree treatment outcomes may have been driven by this therapeutic engagement in writing versus the art therapy directive. Willing disclosure of his lived experience during mask‐making and trauma processing highlights the potential therapeutic value of expressive writing activities and consideration for inclusion in trauma group programs (Nazarian & Smyth, 2013). Although the regular practice of personal journal writing is variable among military service members, a meta‐analysis of the efficacy of therapeutic writing methods, nonetheless, implicates further research for use as a therapeutic tool for cognitive restructuring during trauma treatment and in conjunction with creative art therapies (van Emmerik, Reijntjes, & Kamphuis, 2013).
Overall results from the current case study suggest that a trauma‐focused art therapy directive may be a beneficial adjunct treatment to existing intensive outpatient programs for service members with PTSD. By leveraging expressive techniques, patients in such programs may be able to overcome avoidance symptoms, better engage in the treatment, and ultimately utilize these techniques to better process traumatic events.
ACKNOWLEDGMENTS
Creative Forces®: NEA Military Healing Arts Network is an initiative of the National Endowment for the Arts (NEA) in partnership with the U.S. Departments of Defense and Veterans Affairs and the state and local arts agencies. Administrative support for the initiative is provided by Americans for the Arts. This initiative serves the special needs of military patients and veterans who have been diagnosed with traumatic brain injury and psychological health conditions, as well as their families and caregivers. The program places creative arts therapies at the core of patient‐centered care at 11 clinical sites throughout the country, including Madigan Army Medical Center at Joint Base Lewis‐McChord, plus a telehealth program, and increases access to community arts activities to promote health, wellness, and quality of life for military service members, veterans, and their families and caregivers. The views expressed in this article are those of the authors and do not reflect the official policy of the U.S. Department of the Army, U.S. Department of Defense, or the U.S. Government. The investigators have adhered to the policies for the protection of human subjects as prescribed in 45 CFR 46.
Maltz B, Hoyt T, Uomoto J, Herodes M. A case analysis of service‐member trauma processing related to art therapy within a military‐intensive outpatient program. J Clin Psychol. 2020;76:1575–1590. 10.1002/jclp.22929
REFERENCES
- Abbenante, J. , & Wix, L. (2016). Archetypal art therapy In Gussak D. E. & Rosal M. L. (Eds.), The Wiley handbook of art therapy (pp. 37–46). Chichester, UK: John Wiley & Sons. [Google Scholar]
- Baker, F. , Metcalf, O. , Varker, T. , & O'Donnell, M. (2018). A systematic review of the efficacy of creative arts therapies in the treatment of adults with PTSD. Psychological Trauma: Theory, Research Practice and Policy, 10, 643–651. 10.1037/tra0000353 [DOI] [PubMed] [Google Scholar]
- Blevins, C. A. , Weathers, F. W. , Davis, M. T. , Witte, T. K. , & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM‐5 (PCL‐5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Bruner, J. (1990). Acts of meaning. Cambridge, MA: Harvard University Press. [Google Scholar]
- Campbell, M. , Decker, K. P. , Kruk, K. , & Deaver, S. P. (2016). Art therapy and cognitive processing therapy for combat‐related PTSD: A randomized controlled trial. Art Therapy: Journal of the American Art Therapy Association, 33, 169–177. 10.1080/07421656.2016.1226643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crocq, M. A. , & Crocq, L. (2000). From shell shock and war neurosis to posttraumatic stress disorder: A history of psychotraumatology. Dialogues in Clinical Neuroscience, 2, 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker, K. P. , Deaver, S. P. , Abbey, V. , Campbell, M. , & Turpin, C. (2018). Quantitatively improved treatment outcomes for combat‐associated PTSD with adjunctive art therapy: Randomized controlled trial. Art Therapy, 35, 184–194. 10.1080/07421656.2018.1540822 [DOI] [Google Scholar]
- Eisen, S. V. , Gerena, M. , Ranganathan, G. , Esch, D. , & Idiculla, T. (2006). Reliability and validity of the BASIS‐24 mental health survey for Whites, African‐Americans, and Latinos. The Journal of Behavioral Health Services & Research, 33, 304–323. 10.1007/s11414-006-9025-3 [DOI] [PubMed] [Google Scholar]
- Eisen, S. V. , Normand, S. L. T. , Belanger, A. J. , Spiro, A., III , & Esch, D. (2004). The revised Behavior and Symptom Identification Scale (BASIS‐R): Reliability and validity. Medical Care, 42, 1230–1241. 10.1097/00005650-200412000-00010 [DOI] [PubMed] [Google Scholar]
- van Emmerik, A. A. P. , Reijntjes, A. , & Kamphuis, J. H. (2013). Writing therapy for posttraumatic stress: A meta‐analysis. Psychotherapy and Psychosomatics, 82, 82–88. 10.1159/000343131 [DOI] [PubMed] [Google Scholar]
- Engel, C. C. , Roy, M. , Kayanan, D. , & Ursano, R. (1998). Multidisciplinary treatment of persistent symptoms after Gulf war service. Military Medicine, 163, 202–208. [PubMed] [Google Scholar]
- Foundation for Arts & Healing (2011). Creative, artistic and expressive therapies for PTSD. Brookline, MA: Smyth, J. [Google Scholar]
- Gallagher, M. , & Resick, P. (2012). Mechanisms of change in cognitive processing therapy and prolonged exposure therapy for PTSD: Preliminary evidence for the differential effects of hopelessness and habituation. Cognitive Therapy Research, 36, 750–755. 10.1007/s10608-011-9423-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman, J. L. (1997). Trauma and recovery. New York, NY: Basic Books. [Google Scholar]
- Howie, P. (2017). Art therapy with military populations: History, innovation and application. Abingdon, UK: Routledge. [Google Scholar]
- Hoyt, T. , Barry, D. M. , Kwon, S. J. , Capron, C. , De Guzman, N. , Gilligan, J. , & Edwards‐Stewart, A. (2018). Preliminary evaluation of treatment outcomes at a military intensive outpatient program. Psychological services, 15, 510–519. 10.1037/ser0000190 [DOI] [PubMed] [Google Scholar]
- Hoyt, T. , & Pasupathi, M. (2008). Blogging about trauma: Linguistic markers of apparent recovery. Electronic Journal of Applied Psychology, 4, 56–62. 10.7790/ejap.v4i2.106 [DOI] [Google Scholar]
- Hoyt, T. , Rielage, J. K. , & Williams, L. F. (2012). Military sexual trauma in men: Exploring treatment principles. Traumatology, 18, 29–40. 10.1177/1534765611430724 [DOI] [Google Scholar]
- Hoyt, T. , & Yeater, E. A. (2011). The effects of negative emotion and expressive writing on posttraumatic stress symptoms. Journal of Social and Clinical Psychology, 30, 549–569. 10.1521/jscp.2011.30.6.549 [DOI] [Google Scholar]
- Jones, J. , Drass, J. , & Kaimal, G. (2019). Art therapy for military service members with post‐traumatic stress and traumatic brain injury: Three case reports highlighting trajectories of treatment and recovery. The Arts in Psychotherapy, 63, 18–30. 10.1016/j.aip2019.04.004 [DOI] [Google Scholar]
- Jones, J. , Walker, M. S. , Drass, J. M. , & Kaimal, G. (2018). Art therapy interventions for active duty military service members with post‐traumatic stress disorder and traumatic brain injury. International Journal of Art Therapy, 23, 70–85. 10.1080/17454832.2017.1388263 [DOI] [Google Scholar]
- Kaimal, G. , Walker, M. S. , Herres, J. , French, L. M. , & DeGraba, T. J. (2018). Observational study of associations between visual imagery and measures of depression, anxiety and posttraumatic stress among active duty military service members with traumatic brain injury at the Walter Reed National Military Center. BMJ Open Access, 8, e021448 10.1136/bmjopen-2017-021448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawagley, O. (1990). Yup'ik ways of knowing. Canadian Journal of Native Education, 17, 5–17. [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. (2001). The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lande, R. G. , & Pourzand, M. (2016). Components and characteristics of a psychiatric partial hospital military program. Military Medicine, 181, 213–218. 10.7205/MILMED-D-14-00716 [DOI] [PubMed] [Google Scholar]
- Lande, R. G. , Williams, L. B. , Francis, J. , Gragnani, C. , & Morin, M. (2011). Characteristics and effectiveness of an intensive military outpatient treatment program for PTSD. Journal of Aggression, Maltreatment & Trauma, 20, 530–538. 10.1080/10926771.2011.588149 [DOI] [Google Scholar]
- Lenz, S. , Bruijn, B. , Serman, N. , & Bailey, L. (2014). Effectiveness of cognitive processing therapy for treating posttraumatic stress disorder. Journal of Mental Health Counseling, 36, 360–376. [Google Scholar]
- Lobban, J. (2017). Bypassing the sentinel In Lobban J. (Ed.), Art therapy with military veterans: Trauma and the image (pp. 152–166). Abingdon, UK: Routledge. [Google Scholar]
- Lobban, J. , & Murphy, D. (2017). Using art therapy to overcome avoidance in veterans with chronic posttraumatic stress disorder. International Journal of Art Therapy, 23, 99–114. 10.1080/17454832.2017.1397036 [DOI] [Google Scholar]
- Matto, H. C. (1998). Cognitive‐constructivist art therapy model: A pragmatic approach for social work practice. Families in Society: The Journal of Contemporary Social Services, 79, 631–640. 10.1606/1044-3894.866 [DOI] [Google Scholar]
- Meichenbaum, D. (2017). A constructive narrative perspective on trauma and resilience: The role of cognitive and affective processes In Gold S. (Ed.), APA Handbook of Trauma Psychology (pp. 429–442). Washington, DC: American Psychological Association. [Google Scholar]
- Nazarian, D. , & Smyth, J. M. (2013). An experimental test of instructional manipulations in expressive writing interventions: Examining processes of change. Journal of Social & Clinical Psychology, 32, 71–96. 10.1521/jscp.2013.32.1.71 [DOI] [Google Scholar]
- Norman, J. (2000). Constructive narrative in arresting the impact of post‐traumatic stress disorder. Clinical Social Work Journal, 28, 303–319. 10.1023/A:1005135802159 [DOI] [Google Scholar]
- Pedersen, A. (2016). The role of patient narratives in healthcare innovation: Supporting translation and meaning making. Journal of health organization and management, 30, 244–257. 10.1108/JHOM-01-2015-0007 [DOI] [PubMed] [Google Scholar]
- Pennebaker, J. W. , Boyd, R. L. , Jordan, K. , & Blackburn, K. (2015). The development and psychometric properties of LIWC2015. Austin, TX: University of Texas at Austin. [Google Scholar]
- Pennebaker, J. W. , Chung, C. K. , Frazee, J. , Lavergne, G. M. , & Beaver, D. I. (2014). When small words foretell academic success: The case of college admissions essays. PLOS One, 9, e115844 10.1371/journal.pone.0115844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez, J. (2016). A review of art therapy among military service members and veterans with posttraumatic stress disorder. Journal of Military and Veteran Health, 24, 40–50. [Google Scholar]
- Reger, M. A. , Gahm, G. A. , Swanson, R. D. , & Duma, S. J. (2009). Association between number of deployments to Iraq and mental health screening outcomes in US army soldiers. The Journal of Clinical Psychiatry, 70, 1266–1272. 10.4088/JCP.08m04361 [DOI] [PubMed] [Google Scholar]
- Resick, P. A. (2001). Cognitive therapy for posttraumatic stress disorder. Journal of Cognitive Psychotherapy, 5, 321–329. [Google Scholar]
- Resick, P. A. , Wachen, J. S. , Mintz, J. , Young‐McCaughan, S. , Roache, J. D. , Borah, A. M. , … Peterson, A. L. (2015). A randomized clinical trial of group cognitive processing therapy compared with group present‐centered therapy for PTSD among active duty military personnel. Journal of Consulting and Clinical Psychology, 83, 1058–1068. 10.1037/ccp0000016 [DOI] [PubMed] [Google Scholar]
- Rude, S. S. , Gortner, E. M. , & Pennebaker, J. W. (2004). Language use of depressed and depression‐vulnerable college students. Cognition and Emotion, 18, 1121–1133. 10.1080/02699930441000030 [DOI] [Google Scholar]
- Schouten, K. A. , de Niet, G. J. , Knipscheer, J. W. , Kleber, R. J. , & Hutschemaekers, G. J. M. (2015). The effectiveness of art therapy in the treatment of traumatized adults: A systematic review on art therapy and trauma. Trauma, Violence & Abuse, 16, 220–228. 10.1177/1524838014555032 [DOI] [PubMed] [Google Scholar]
- Tackman, A. M. , Sbarra, D. A. , Carey, A. L. , Donnellan, M. B. , Horn, A. B. , Holtzman, N. S. , … Mehl, M. R. (2019). Depression, negative emotionality, and self‐referential language: A multi‐lab, multi‐measure, and multi‐language‐task research synthesis. Journal of Personality and Social Psychology, 116, 817–834. 10.1037/pspp0000187. [DOI] [PubMed] [Google Scholar]
- Talwar, S. (2007). Accessing traumatic memory through art making: An art therapy trauma protocol. The Arts in Psychotherapy, 34, 22–35. 10.1016/j.aip.2006.09.001 [DOI] [Google Scholar]
- Tani, F. , Peterson, C. , & Smorti, M. (2016). The words of violence: Autobiographical narratives of abused women. Journal of Family Violence, 31, 885–896. 10.1007/s10896-016-9824-0 [DOI] [Google Scholar]
- Timko, C. , Sempel, J. M. , & Moos, R. H. (2003). Models of standard and intensive outpatient care in substance abuse and psychiatric treatment. Administration and Policy in Mental Health, 30, 417–436. 10.1023/A:1024693614501 [DOI] [PubMed] [Google Scholar]
- Walker, M. S. , Kaimal, G. , Gonzaga, A. M. L. , Myers‐Coffman, K. A. , & DeGraba, T. J. (2017). Active‐duty military service members’ visual representations of PTSD and TBI in masks. International Journal of Qualitative Studies in Health and Well‐being, 12, 1267317 10.1080/17482631.2016.1267317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker, M. S. , Kaimal, G. , Koffman, R. , & DeGraba, T. J. (2016). Art therapy for PTSD and TBI: A senior active duty military service member's therapeutic journey. The Arts in Psychotherapy, 49, 10–18. 10.1016/j.aip.2016.05.015 [DOI] [Google Scholar]
- Wise, S. , & Nash, E. (2013). Metaphor as heroic mediator: Imagination, creative arts therapy and group process as agents of healing with veterans In Scurfield R. M. & Platoni K. (Eds.), Healing War Trauma: a Handbook of Creative Approaches (pp. 123–138). New York, NY: Routledge. [Google Scholar]
- Wortmann, J. H. , Jordan, A. H. , Weathers, F. W. , Resick, P. A. , Dondanville, K. A. , Hall‐Clark, B. , … Litz, B. T. (2016). Psychometric analysis of the PTSD Checklist‐5 (PCL‐5) among treatment‐seeking military service members. Psychological Assessment, 28, 1392–1403. 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]
- Zalta, A. , Held, P. , Smith, D. L. , Klassen, B. J. , Lofgreen, A. M. , Normand, P. S. , … Karnik, N. S. (2018). Evaluating patterns and predictors of symptom change during a three‐week intensive outpatient treatment for veterans with PTSD. BMC Psychiatry, 18, 242 10.1186/s12888-018-1816-6 [DOI] [PMC free article] [PubMed] [Google Scholar]


