Summary
Organ transplantation saves and transforms lives. Failure to secure consent for organ retrieval is widely regarded as the single most important obstacle to transplantation. A soft opt‐out system of consent for deceased organ donation was introduced into Wales in December 2015, whilst England maintained the existing opt‐in system. Cumulative data on consent rates in Wales were compared with those in England, using a two‐sided sequential procedure that was powered to detect an absolute difference in consent rates between England and Wales of 10%. Supplementary risk‐adjusted logistic regression analysis examined whether any difference in consent rates between the two nations could be attributed to variations in factors known to influence UK consent rates. Between 1 January 2016 and 31 December 2018, 8192 families of eligible donors in England and 474 in Wales were approached regarding organ donation, with overall consent rates of 65% and 68%, respectively. There was a steady upward trend in the proportion of families consenting to donation after brain death in Wales as compared with England and after 33 months, this reached statistical significance. No evidence of any change in the donation after circulatory death consent rate was observed. Risk‐adjusted logistic regression analysis revealed that by the end of the study period the probability of consent to organ donation in Wales was higher than in England (OR [95%CI] 2.1 [1.26–3.41]). The introduction of a soft opt‐out system of consent in Wales significantly increased organ donation consent though the impact was not immediate.
Keywords: organ donation, presumed consent, public policy, transplantation
Introduction
Organ transplantation saves and transforms lives, and economic analysis suggests it saves the NHS hundreds of millions of pounds each year 1. Access to solid organ transplantation is determined by donor and donor organ availability, and whilst the identification and referral of potential deceased donors often restricts organ availability, failure to secure consent for organ retrieval is regarded widely as the single most important obstacle to transplantation 1.
The legal frameworks for consent for deceased organ donation fall into two major categories: opt‐in, where expressed consent is required from the patient or their relatives; and opt‐out, where consent is presumed in the absence of a statement made by the patient in their lifetime to the contrary. Most of the studies exploring models of organ donation consent have been retrospective and observational, usually involving either a direct comparison between different jurisdictions or, less commonly, ‘before and after’ studies of the impact of switching from opt‐in to an opt‐out system of consent within a given country 2, 3, 4, 5, 6, 7.
The UK is made up of four major nations: England (population 56.0 million); Scotland (population 5.4 million); Wales (population 3.1 million); and Northern Ireland (population 1.9 million) 8. Although responsibility for healthcare is devolved to each nation to organise and deliver, organ donation is delivered nationally by NHS Blood and Transplant as single UK‐wide service. This organisation is responsible for all key elements of the donation pathway in the UK, namely: donor identification and referral; family approach for consent; and organ retrieval.
An opt‐out system of consent was introduced into Wales in December 2015, whereas the rest of the UK maintained the opt‐in system 9. The new legislation in Wales allowed for consent to be deemed to have been given if the patient had not otherwise expressed their decision (e.g. a recorded or verbally expressed positive or negative decision to donate) or were not in an excepted group (under 18, lacked prior capacity, non‐resident of Wales). Under the current opt‐in system operational within the rest of the UK, consent is requested of the family in such circumstances. Whilst the legislative change in Wales provides a legal basis for deeming (presuming) consent, the family are still asked to support the deemed consent, a system known as soft opt‐out. As in England, there is no legal right to veto an expressed positive decision to donate; however, in practical terms this can still happen. The same is true of overriding a deemed consent in Wales, where opposition from a family will stop donation proceeding.
The methodology of our study was designed to take advantage of the unique opportunity to prospectively compare consent rates for deceased donation in Wales with those in England, in order to investigate the impact of the change in legislation.
Methods
The majority of data analysed in this study are from the UK Potential Donor Audit, a continuous national audit of all patients aged ≤ 80 years who die within an intensive care unit or emergency department in a UK hospital 10. The consent rate is the proportion of families of eligible donors approached for formal organ donation discussion where consent for donation was ascertained. The UK Organ Donor Register (ODR) is active across all four UK nations and due to the legislation change in Wales this was modified in 2015 to allow expression of either an opt‐in or opt‐out organ donation decision. If there is no known prior donation decision, only in Wales could the consent be deemed legal. To avoid bias in favour of the Welsh opt‐out system, where awareness of the option to opt‐out was much higher, individuals who had opted‐out of organ donation using the ODR were also included in the consent rate calculation even if their families were only approached to inform them of the opt‐out decision. Data on trends in donor numbers in England and Wales following the introduction of opt‐out into Wales were extracted from the UK transplant registry which records all donors and transplants.
Separate analyses were carried out for the two types of deceased organ donation practised in the UK: donation after the diagnosis of death using neurological criteria (donation after brain death (DBD)); and controlled donation after circulatory death (DCD). The baseline consent rates were taken to be the combined consent rates for England and Wales between 1 April 2014 and 31 March 2015 and were 67% for DBD and 53% for DCD. Underlying DBD and DCD consent rates between the two nations were assumed to be the same before the change in legislation. Before deemed consent commenced in Wales, a decision was made to only compare Wales with England, as Scotland had publicly announced plans to explore moving to an opt‐out system, and this may have impacted on consent rates.
Analyses were performed using a two‐sided sequential procedure 11, 12, designed to have 90% power to detect an absolute difference in consent rates between England and Wales of 10%, with significance at the 5% level. With a standard fixed sample test of two proportions we would expect to wait 5 years before completing sample recruitment. For this reason, a sequential study design was used so that data could be legitimately reviewed on a regular basis. By using O'Brien and Fleming boundaries, more stringent significance levels were utilised in the earlier assessments 13. This study design would also account for the fact that the number of eligible deceased donors in England was approximately 20 times that of Wales. Expected sample sizes were such that the duration of the study would be around 3 years (12 quarters) if there was a true difference in consent rates. Using this sequential study design, cumulative data on consent rates in Wales were compared with those in England, and the quarterly results were shared over the life of the study with the Welsh government and interested stakeholders.
Once unadjusted sequential analyses were complete, retrospective risk‐adjusted logistic regression analysis was conducted 14, to further examine the impact of opt‐out on consent rates once the effect of other factors known to influence UK consent rates had been taken into account 15. At the end of each quarter, the significance of the difference in the cumulative proportions was evaluated using a z‐statistic for comparing the two proportions 11. The quarterly values of the z‐statistic were plotted against the number of eligible donors whose families were approached regarding organ donation. Boundary lines were constructed in such a way that should a point cross the upper boundary, the study would conclude that the Welsh consent rate had significantly increased relative to the English consent rate, whereas crossing the lower boundary would indicate that the Welsh consent had significantly reduced. If the study continued until a point crossed the vertical dotted line (after complete sample recruitment), the study would conclude that there was no significant difference between the two consent rates. All analyses were carried out using SAS Enterprise Guide 7.1 (SAS Institute, Cary, NC, USA).
Results
Between 1 January 2016 and 31 December 2018, 8192 families of eligible donors in England and 474 in Wales were approached regarding organ donation, with overall consent rates of 65% and 68%, respectively. Individual quarterly consent rates for DCD and DBD donation are shown in Table 1. There was considerable variation in the quarterly consent rates in Wales, which can be attributed to the much smaller number of potential donors in Wales compared with England. Nevertheless, it can be seen that quarterly DBD consent rates in Wales were generally higher than in England. In contrast, whilst DCD consent rates in Wales were initially much lower, they gradually increased and eventually were higher than in England. English DCD consent rates remained relatively static throughout.
Table 1.
Quarterly rates of organ donation after diagnosis of death using neurological criteria (donation after brain death) and controlled donation after circulatory death for England and Wales from 1 January 2016 to 31 December 2018. Values are number and proportion
| Year | Quarter | Donation after brain death | Donation after circulatory death | ||||||
|---|---|---|---|---|---|---|---|---|---|
| England | Wales | England | Wales | ||||||
| Approaches | Consent rate | Approaches | Consent rate | Approaches | Consent rate | Approaches | Consent rate | ||
| 2016 | 1 | 255 | 67.8% | 12 | 83.3% | 416 | 63.9% | 27 | 44.4% |
| 2 | 283 | 65.7% | 8 | 75.0% | 392 | 59.9% | 18 | 55.6% | |
| 3 | 267 | 62.2% | 14 | 78.6% | 351 | 57.8% | 31 | 45.2% | |
| 4 | 299 | 70.6% | 12 | 75.0% | 394 | 58.9% | 26 | 46.2% | |
| 2017 | 1 | 279 | 71.7% | 17 | 82.4% | 406 | 59.1% | 28 | 64.3% |
| 2 | 298 | 68.8% | 12 | 83.3% | 403 | 61.3% | 15 | 46.7% | |
| 3 | 299 | 76.9% | 15 | 73.3% | 368 | 54.6% | 20 | 55.0% | |
| 4 | 323 | 71.2% | 21 | 90.5% | 397 | 63.5% | 29 | 65.5% | |
| 2018 | 1 | 358 | 70.7% | 20 | 65.0% | 400 | 65.0% | 33 | 60.6% |
| 2 | 322 | 72.0% | 13 | 76.9% | 388 | 61.1% | 23 | 87.0% | |
| 3 | 307 | 73.3% | 16 | 93.8% | 319 | 60.2% | 26 | 69.2% | |
| 4 | 309 | 71.5% | 21 | 85.7% | 359 | 62.7% | 17 | 76.5% | |
The corresponding sequential charts for DBD and DCD donors with quarterly values of the z‐statistic plotted against number of families approached are shown in Fig. 1. As the quarterly monitoring progressed, a steady upward trend was observed in the sequential chart (Fig. 1a) showing an improving DBD consent rate in Wales relative to England. In quarter 11, the plotted point crossed the upper boundary concluding the DBD study and providing statistical evidence of a significant increase in the DBD consent rate in Wales compared with England. Data for quarter 12 continued the improving trend and an additional test was well within the boundary, verifying our findings. The sequential chart provided no evidence of a similar trend in DCD consent rates (Fig 1b). Although an improving DCD trend can be observed in the latter quarters (and Table 1 gives the appearance of dramatic improvement in the last three quarters) the study concluded with the plotted points for DCD consent crossing the dotted line at the end of sample recruitment. This unadjusted analysis shows that there was no evidence of any statistical change in the DCD consent rate in Wales, relative to England, since the introduction of the opt‐out system in Wales.
Figure 1.
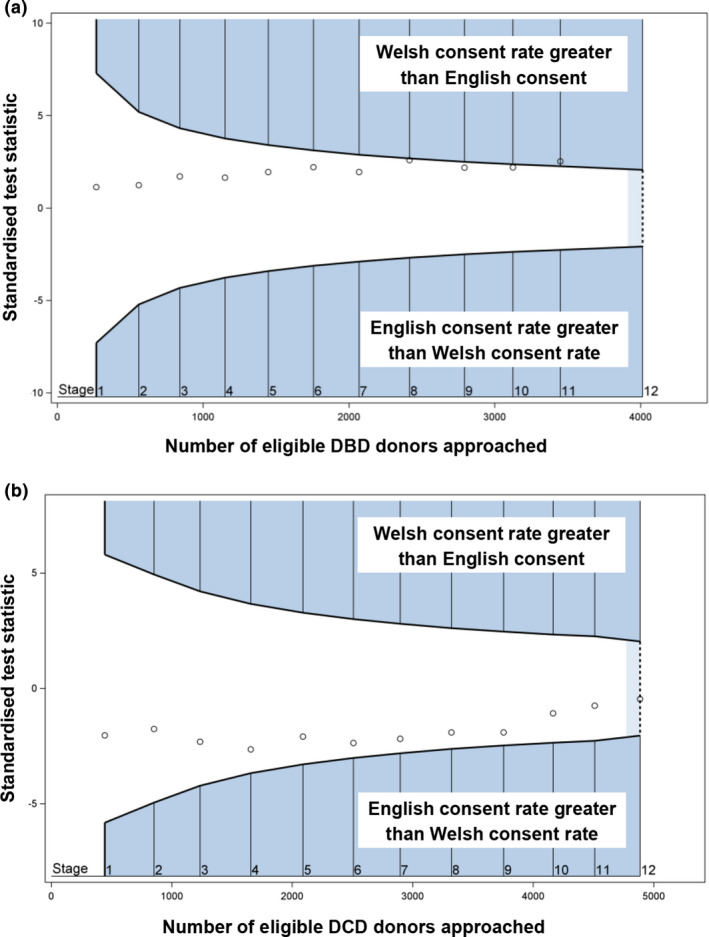
Quarterly consent rates for organ donation after diagnosis of death using (a) neurological criteria (donation after brain death (DBD) and (b) controlled donation after circulatory death (DCD) for England and Wales from 1 January 2016 to 31 December 2018. Small circles, quarterly z‐statistic comparing consent rates. Blue boundary lines: crossing the boundary lines into the blue shaded areas indicates that the Welsh consent rate is significantly different relative to the English consent rate. Vertical dotted line: crossing the vertical dotted line indicates complete sample recruitment and that there is no significant difference between the two consent rates.
Multivariable logistic regression analysis was carried out to explore further the impact of the opt‐out system in Wales. The model considered both DBD and DCD consent together by adjusting for how the type of donation influenced the likelihood of consent. It also took into account other factors that had previously been identified to influence consent rates in the UK, namely: patient's prior decision; patient's ethnicity; pre‐mention of donation; and if a specialist nurse for organ donation was involved in the family approach 15. Finally, the effect of donation nation was considered as a marker for the impact of opt‐out and year of donation included to account for changes over time.
An interaction term indicated that the influence of opt‐out on consent over time (combined DBD and DCD) became highly significant. In the first calendar year following opt‐out, the chance of consent in Wales was significantly lower than England (OR [95%CI] 0.40 [0.28–0.71]). In the second‐year, consent was equally likely in the two nations (OR [95%CI] 1.00 [0.63–1.60]), and in the third year the chance of ascertaining consent in Wales was double that seen in England (OR [95%CI] 2.1 [1.26–3.41]).
Our study noted a higher proportion of Welsh patients had expressed a prior positive decision to be an organ donor (Table 2). In patients who had not expressed any prior donation decision, either by registering on the ODR or verbally telling their family and therefore deemed consent would apply in Wales, we observed an increasing chance of ascertaining consent in Wales when compared with England. In 2018, having adjusted for the same factors used in our original model, the chance of consent in Wales for this cohort was almost three times higher than in England (OR [95%CI] 2.8 [1.58–5.03]).
Table 2.
Prior decision by patients regarding organ donation in England and Wales. Values are number (proportion)
| England | Wales | |
|---|---|---|
| n = 7814a | n = 417a | |
| Opt‐in (on organ donor register) | 2555 (33%) | 166 (40%) |
| Opt‐in (verbally expressed) | 298 (4%) | 47 (11%) |
| Opt‐out (on organ donor register) | 207 (3%) | 42 (10%) |
| Unknown | 4754 (61%) | 162 (39%) |
435 cases were excluded in the multivariable logistic regression dataset due to unknown ethnicity and missing organ status.
Although this analysis focused on the impact of opt‐out on consent rates, higher rates of consent should be expected to result in increased donor numbers. Both English and Welsh donor numbers have increased since the new legislation was introduced in Wales (Table 3). However, Wales achieved 28.9 donors per million population in 2018, which is indicative of an improving national trend and one which is occurring at a greater rate than England.
Table 3.
Annual deceased donation rates per million population (pmp)* by nation of donating hospital
| Year | England | Wales | ||
|---|---|---|---|---|
| Donations; n | Donation rate; pmp | Donations; n | Donation rate; pmp | |
| 2015 | 1110 | 20.0 | 56 | 18.0 |
| 2016 | 1164 | 21.0 | 57 | 18.3 |
| 2017 | 1268 | 22.8 | 77 | 24.8 |
| 2018 | 1350 | 24.3 | 90 | 28.9 |
*Donors per million population are provided as an indication of donation rates. Population figures for the nation of donor hospital are an approximation based on mid‐2016 estimates from the Office of National Statistics 2011 census figures (England, Isle of Man and Channel Islands 55.51 million and Wales 3.11 million) and do not account for patients who become a donor in a nation which differed from their nation of residence.
During the study period there were 186 (8% of all ODR opt‐in approaches; 58 DBD, 128 DCD) family overrides of ODR opt‐in in England compared with 16 (10%; 4 DBD, 12 DCD) in Wales. Family override of deemed consent in Wales occurred on 31 occasions (26% of all deemed approaches; 9 DBD, 22 DCD). Theoretically, if the family can provide evidence to support that the potential donor had changed their mind and the registered opt‐out was not the last known decision, the registered opt‐out could be overridden. This never occurred during the study period.
Discussion
We have been able to provide prospective evidence of a positive impact of opt‐out legislation on consent rates for organ donation in Wales. By the end of the study period, the chance of consent in Wales was double that seen in England and almost three times higher in patients who had made no prior donation decision in life. Pleasingly, there was also a greater increase in the number of donors per million population in Wales compared with England; however, the study was not powered to examine this outcome and this finding should be interpreted with caution.
Our study is unable to differentiate whether the improvement in consent rate in Wales can be attributable to legislation change alone or was associated with a number of other interventions introduced as part of opt‐out implementation. Wales implemented deemed consent 2 years after the legislation was passed in 2013. These years allowed an extensive media promotion campaign by the Welsh government informing the Welsh public that the law around organ donation was changing and they had to make a decision: either to opt‐in, opt‐out or have their consent deemed. The Welsh government committed £2 million (€2.2 million, US$ 2.42 million) over 2 years to the campaign achieving 74% population awareness of the legislative change before implementation 16. Our analysis identified a higher proportion of Welsh residents who had expressed a prior positive decision (either registration on the ODR or being expressed verbally to family) to be an organ donor.
The experience of the NHS Blood and Transplant's team of specialist nurses in organ donation who cover Wales, was that a period of adjustment (with an increase in training needs) was required for healthcare staff to become fully accustomed to the change in style and language of the family approach under the new legislation. We propose that it was familiarity with the legislation, training and growing confidence in the healthcare professionals who approached families regarding donation in Wales, as well as high public awareness, that led to the observed increase in consent rates. It was not possible for our study to determine whether the same improvement could have been achieved without the impetus of legislation change. What is clear is that the Welsh government's decision to move to an opt‐out system may be regarded somewhat as a leap of faith. At the time of the legislation international evidence of benefit was inconclusive 2, 3 and UK expert opinion had expressed reservations 17, 18, 19, 20.
Our sequential analysis identified a significant increase in terms of the Welsh DBD consent rates relative to the rate in England. This evidence was not replicated in the same quarterly DCD consent rate monitoring. We speculate that DCD was less influenced by the legislation change than DBD due to differing family experiences of the two types of donation 21, 22, 23.
The supplementary multivariable logistic regression analysis provided additional evidence of a significant difference in combined DBD and DCD consent rates between the two nations over and above the effect of previous published key influential factors. Our analysis showed that there was a delay of 2 years from the introduction of the opt‐out policy before the difference in consent rates became apparent for combined DBD and DCD donation in Wales. This finding was supported by an earlier study which showed no difference in consent rates for organ donation between Wales and the rest of the UK in the first 18 months following implementation of the new legislation 24.
A key limitation in our analysis was that the sequential analysis assumed the underlying Welsh and England consent rates were similar before opt‐out and that the impact would be immediate. We only compared Wales to England and did not include Scotland or Northern Ireland but as their population numbers are relatively small compared with England, we do not believe this would have impacted upon our findings.
The Welsh example has been observed closely by other nations. In 2019, both England and Scotland passed legislation to introduce deemed consent and deemed authorisation respectively. While in Nova Scotia and the Netherlands, authorities have also introduced opt‐out legislation. We would urge all countries contemplating a change to their consent legislation, or another major initiative to increase organ donation numbers, to consider and design before implementation how they will assess the impact of any changes.
The introduction of an opt‐out policy for organ donation in Wales provided a unique opportunity to compare consent rates for deceased donation in Wales with England prospectively. We observed that organ donation consent rates in Wales significantly increased in comparison with England, although the impact was not immediate and took several years to take effect. Our study and the experience from Wales provides evidence to inform and support opt‐out initiatives world‐wide which, if replicated, could increase consent rates and consequently improve the number of organs available for transplant.
Acknowledgement
No external funding or competing interests declared.
Contributor Information
P. Walton, @PhilW_It_n.
D. Gardiner, Email: dale.gardiner@nhsbt.nhs.uk, @dalecgardiner.
References
- 1. A Collaborative UK strategy . Taking Organ Transplantation to 2020: a detailed strategy. 2013. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/4240/nhsbt_organ_donor_strategy_long.pdf (accessed 08/03/2020).
- 2. Rithalia A, McDaid C, Suekarran S, Myers L, Sowden A. Impact of presumed consent for organ donation on donation rates: a systematic review. British Medical Journal 2009; 338: a3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Palmer M. Welsh Government: Opt‐out systems of organ donation: International evidence review. 2012. https://gov.wales/sites/default/files/statistics-and-research/2018-12/121203optoutorgandonationen.pdf (accessed 08/03/2020).
- 4. Niven J, Chalmers N. Scottish Government: Opt out organ donation: a rapid evidence review. 2018. https://pdfs.semanticscholar.org/1139/797025e9f121ab37d9e3296fa02f4505cee4.pdf (accessed 08/03/2020).
- 5. Shepherd L, O'Carrol RE, Ferguson E. An international comparison of deceased and living organ donation/transplant rates in opt‐in and opt‐out systems: a panel study. BMC Medicine 2014; 12: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Glazier A. Success of opt‐in organ donation policy in the United States. Journal of the American Medical Association 2019; 322: 719–20. [DOI] [PubMed] [Google Scholar]
- 7. Ahmad MU, Hanna A, Mohamed AZ, et al. A systematic review of opt‐out versus opt‐in consent on deceased organ donation and transplantation (2006–2016). World Journal of Surgery 2019; 43: 3161–71. [DOI] [PubMed] [Google Scholar]
- 8. Office for National Statistics . Population estimates for the UK, England and Wales, Scotland and Northern Ireland: mid‐2018. 2018. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland. Mid‐2016 estimate (accessed 08/03/2020).
- 9. National Assembly for Wales . Human Transplantation (Wales) Act. 2013. https://www.legislation.gov.uk/anaw/2013/5/data.pdf (accessed 08/03/2020).
- 10. NHS Blood and Transplant . Bristol: organ donation and transplantation clinical; c2009‐2019 [cited 2019 Jan 14]. The Potential Donor Audit Report. 2019. https://www.odt.nhs.uk/statistics-and-reports/potential-donor-audit-report (accessed 08/03/2020).
- 11. Jennison C, Turnbull BW. Group Sequential Methods with Applications to Clinical Trials. London: Chapman and Hall/CRC, 2000. [Google Scholar]
- 12. Whitehead J. The Design and Analysis of Sequential Clinical Trials, 2nd edn. Chichester: John Wiley & Sons, 1997. [Google Scholar]
- 13. O'Brien PC, Fleming TR. A multiple testing procedure for clinical trials. Biometrics 1979; 35: 549–56. [PubMed] [Google Scholar]
- 14. Collett D. Modelling Binary Data, 2nd edn. London: Chapman & Hall/CRC, 2002. [Google Scholar]
- 15. Hulme W, Allen J, Manara AR, Murphy PG, Gardiner D, Poppitt E. Factors influencing the family consent rate for organ donation in the UK. Anaesthesia 2016; 71: 1053–63. [DOI] [PubMed] [Google Scholar]
- 16. Welsh Government . Update to survey of public attitudes to organ donation: key figures from wave 10. 2015. https://gov.wales/sites/default/files/statistics-and-research/2019-04/public-attitudes-organ-donation-wave-10-key-figures.pdf (accessed 08/03/2020).
- 17. Organ Donation Taskforce . The potential impact of an opt out system for organ donation in the UK. 2008. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/4250/thepotentialimpactofanoptoutsystemfororgandonationintheuk.pdf (accessed 08/03/2020).
- 18. Fabre J, Murphy P, Matesanz R. Presumed consent: a distraction in the quest for increasing rates of organ donation. British Medical Journal 2010; 341: c4973. [DOI] [PubMed] [Google Scholar]
- 19. Rudge CJ, Buggins E. How to increase organ donation: does opting out have a role? Transplantation 2012; 93: 141–4. [DOI] [PubMed] [Google Scholar]
- 20. Simpson P. Consultation on the human transplantation (Wales) bill: written evidence from the UK Donor Ethics Committee (UKDEC). 2013. http://senedd.assembly.wales/documents/s13676/HSC4-04-13%20p5%20Paper%205%20-%20UKDEC.pdf (accessed 08/03/2020).
- 21. Manara AR, Murphy PG, O'Callaghan G. Donation after circulatory death. British Journal of Anaesthesia 2012; 108(Suppl. 1): i108–21. [DOI] [PubMed] [Google Scholar]
- 22. Taylor LJ, Buffington A, Scalea JR, et al. Harms of unsuccessful donation after circulatory death: An exploratory study. American Journal of Transplantation 2018; 18: 402–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Prescott J, Gardiner D, Hogg L, Harvey D. How the mode of organ donation affects family behaviour at the time of organ donation. Journal of the Intensive Care Society 2018; 20: 204–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Noyes J, McLaughlin L, Morgan K, et al. Short‐term impact of introducing a soft opt‐out organ donation system in Wales: before and after study. British Medical Journal Open 2019; 9: e025159. [DOI] [PMC free article] [PubMed] [Google Scholar]


