Abstract
Introduction
Adults with limb amputation and other physical disabilities are less likely to participate in physical activity than adults in the general population and have elevated risk of heart disease and stroke. Swimming is a physical activity often recommended for persons with limb amputation. However, a standard economical swim prosthesis that facilitates easy transition from land to water does not exist.
Objective
The objectives were (1) to measure ease of first‐time use and likability of a novel U.S. Food and Drug Administration (FDA)–cleared 510(k) three‐dimensional (3D) printed device, the “FIN,” in a recreational pool; and (2) to determine differences in time to complete basic swim tasks using the novel 3D printed amphibious lower limb prosthesis or a standard Swim Ankle prosthesis. Our hypotheses were the following: (1) that the novel 3D printed amphibious lower limb prosthesis would be easy and likeable upon first use; and (2) that basic swim tasks would take comparable time to complete with either device.
Setting
Academic medical center and community pool in New York.
Participants
Participants were (N = 10) English‐speaking adults with a transtibial amputation who self‐identified to swim comfortably in a recreational setting.
Interventions
Participants completed tasks typical of recreational swimming while wearing the novel 3D printed amphibious lower limb prosthesis or a Swim Ankle.
Main Outcome Measurements
Participants performed a series of recreational swim tasks at self‐selected speeds: entering/exiting pool, walking, swimming, and treading water, and completed a survey to assess the primary outcomes: likability, ease of use, and adverse events (feasibility).
Results
Participants found the novel 3D printed amphibious lower limb prosthesis more likable compared to the Swim Ankle and easy to use. Time to exit the pool was significantly reduced with the novel 3D printed amphibious lower limb prosthesis, while time to complete a 25‐m lap was comparable. Participants did not show significant changes in vital signs when using either prosthesis.
Conclusions
The novel 3D printed amphibious lower limb prosthesis was likable and easy to use upon first use. This study supports conducting a larger clinical trial to determine if the data are broadly reproducible.
Introduction
In 2005, 1.6 million persons were living in the United States with limb loss, and there are ~185 000 limb amputations annually.1, 2 By 2050, the number of persons living with limb loss is anticipated to more than double.1 Upper and lower limb amputations secondary to dysvascular disease account for the majority (54%) of cases, and of these over two‐thirds have a comorbid diagnosis of diabetes. Limb loss secondary to trauma accounts for an additional 45% of the prevalent cases and cancer for the remaining cases (<2%).1
Limb amputation impacts many aspects of life, including employment, psychosocial health, community integration, and physical activity. As in any population, reduced physical activity can lead to increased risk of coronary heart disease and stroke. Conversely, benefits of physical activity include elevated mood and emotional health.3, 4 Adults with mobility‐related disabilities such as lower limb amputation are less likely to participate in physical activity relative to the general population and are more likely to be obese, elevating their risk of heart disease and stroke.5, 6, 7
In the general population, physical limitations, lack of confidence, embarrassment, and constructs of the social environment may act as obstacles to physical activity.3, 4 In a U.S. study (2001‐2005), 43.8% of individuals with a disability and 32.8% of individuals without a disability were inactive, demonstrating that persons with disabilities lead more sedentary lifestyles than those without.6, 7 Known barriers to participation in physical activity for persons with lower limb amputations include lack of transportation, inaccessible fitness facilities, income, and discriminatory societal attitudes.5, 8 Individuals with lower limb prostheses were significantly more likely than people with upper limb prostheses to experience challenges in the physical environment, sports and physical recreation, as well as restrictions in their community life and employment.9 Nearly three of four individuals with a major limb amputation experienced difficulties due to the emotional effects of their disability, and 36% felt that their dignity was compromised because of it.
As demonstrated in other populations living with physical challenges, the probability of participating in physical activity, exercise, and sport after an amputation was higher in those who did so prior to amputation.4, 5, 10 Swimming and fishing are common activities after limb amputation, as a prosthesis is not required for participation or functional independence.4, 11 Self‐worth, self‐efficacy, and overall health can be improved with the reinforcement of physical activity after limb amputation.4, 12 Unfortunately, a standardized and economical prosthesis for swimming and water activities does not exist.
Currently, the ankle foot, or fixed angle foot, is an available swim prosthesis that makes a 90° angle with the floor (Figure 1F); thus, it cannot be used when walking over ground and is difficult to use to transition into and out of the water, as required to enter or exit a pool or natural body of water. Aside from such design limitations, cost may be an additional barrier to swimming for individuals with lower limb amputation. In the 1980s, the cost of a prosthesis for swimming was estimated to range from $2500 to $10 000.13 A recent meta‐analysis acknowledged that economic costs of transtibial prosthetics, estimated to be within a lifetime range of $0.5 to $1.8 million for an individual, are challenging given the different etiologies, multiple intervention options, variations in labor costs, and lack of available data restricted to the prosthesis itself (not including costs of surgical and associated care).14 A recent analysis of prosthetic costs for Veterans of Vietnam, Operation Iraqi Freedom, and Operation Enduring Freedom estimated that a waterproof prosthesis for transfemoral limb loss cost $19 649, using Medicare costs in 2005.15 Modifications to a prosthesis for swimming may increase the price; a swim foot/ankle may range from $1500 to 3000 and additional customizations will add labor and material costs from the prosthetic provider.
Figure 1.

Examples of the novel 3D printed amphibious lower limb prosthesis and its use: (A) The novel 3‐D printed amphibious lower limb prosthesis can be used with standard socket and easily assembled. (B) A participant can use the novel 3D printed amphibious lower limb prosthesis for walking over ground or (C) when exiting the pool via a ramp. (D) Donning and doffing the novel 3D printed amphibious lower limb prosthesis is easy and is used with a participant's own standard socket. (E) Each novel device is printed specifically for the user. (F) The Rampro Swim Ankle: The ankle locks into the walking or swimming position as needed (image downloaded from www.rampro.net).
In 2017, Northwell Health created novel three‐dimensional (3D) printed amphibious lower limb prosthesis to be used for swimming, called the “FIN” (Figure 1A‐E). In 2018, the FIN received U.S. Food and Drug Administration (FDA) clearance as a (510 k) prosthetic and orthotic accessory, Class I device. The novel 3D printed amphibious lower limb prosthesis is printed at a lower cost than traditional swim prosthetics, has a nonslip sole that is optimized for use on wet surfaces, and has a flexible ankle hinge that fits over an individual's typical socket. It is printed using nylon enhanced by carbon fiber and contains conically shaped holes with the goal of creating drag and propulsion through the water. As with other prosthetic devices, the novel 3D printed amphibious lower limb prosthesis was designed to be specific to each user (eg, the number of holes within each prosthesis can be changed for each individual), while keeping the cost within a range of $2500 to $15 000, depending on additional customizations that the user may desire. The cost of a single novel 3D printed amphibious lower limb prosthesis used in this study was $2500. The novel 3D printed amphibious lower limb prosthesis can be used on both wet and dry land, facilitating improved transitions between swimming and other activities of daily living without requiring the user to switch prostheses. The novel 3D printed amphibious lower limb prosthesis overall design allows for an individual to don a single prosthetic leg to travel to a water‐activity destination and to enter and exit a water environment without any additional prosthetic adjustments. Together, these design features should make the novel 3D printed amphibious lower limb prosthesis easier to use, likable, and more affordable than traditional swim prostheses.
Previously, the prototype was used by two individuals and was well‐liked for its ease of use and lack of adverse events common in this population, such as triggering skin breakdown or irritation. In preparation for greater availability of the prosthesis to the general public, here we conducted a pilot clinical study in an indoor pool environment to obtain data from adults with lower limb amputations on use of the novel 3D printed amphibious lower limb prosthesis and compare their experiences with it to those with a typical ankle foot swim prosthesis.
The primary objective of this pilot clinical study was to test if the novel 3D printed amphibious lower limb prosthesis was easy to use and well‐liked by users (N = 10) upon first encounter in a recreational pool setting. The secondary objective was to determine if there were any major differences in the time needed to complete basic tasks associated with recreational swimming, including getting into and out of a pool, swimming a short distance, and treading water. Our primary hypothesis was that participants would find the novel 3D printed amphibious lower limb prosthesis easy to use on initial encounter in a recreational swim setting. Our secondary hypothesis was that basic swim tasks would take comparable time to complete with novel 3D printed amphibious lower limb prosthesis and with the standard Swim Ankle.
Methods
This prospective study was performed in an academic medical center in accordance with ethical standards and with approval from the local institutional review board. Prior to initiating study participation, individuals were informed that their involvement in this study was entirely voluntary and that their honest feedback and input were sought regarding their experiences using the novel 3D printed amphibious lower limb prosthesis. The participants were informed that there would be no negative consequences of any kind if they declined to participate or if they preferred the Swim Ankle over the novel 3D printed amphibious lower limb prosthesis in any way. Inclusion criteria were the following: age of 18 to 85 years, male or female, history of below the knee amputation, able to enter and exit the pool unassisted, self‐identified to be able to swim comfortably in a recreational setting, and English speaking. Exclusion criteria were the following: clinically significant wounds on the residual limb identified by a physiatrist board certified in physical medicine and rehabilitation on the day of the pool study visit. Participants who met exclusion criteria were alerted to seek follow‐up care from their primary physician, with the opportunity to participate at another study visit once the wound resolved. This was a pilot study with a sample size of convenience. Active time for each participant consisted of three visits for prosthetic fittings, followed by a single 3‐hour pool study visit. Multiple pool days were offered to accommodate participants’ schedules.
In a public community Olympic size pool, each participant was asked to complete a series of tasks that are typical of recreational swimming with the standard Swim Ankle and with the novel 3D printed amphibious lower limb prosthesis (Figure 1). Participants were instructed that they could decline to perform any of the tasks and were advised to swim at a comfortable pace, as opposed to a competitive one. Trial times were recorded for each task to indicate ease of performance (Figure 2).
Figure 2.
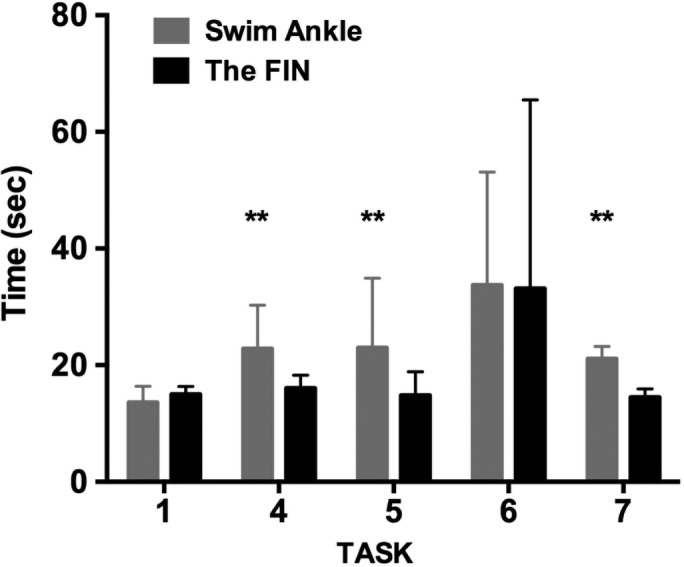
Time to Complete Each Task Using the novel 3‐D printed amphibious lower limb prosthesis or Swim Ankle: Task 1: Entering pool via ramp; Task 4: Exiting pool via ladder, P = .008; Task 5: Entering pool via ladder, P = .008; Task 6: swim lap (25 m); Task 7: Exiting pool via ramp, P = .004. Bars show median and error bars show interquartile ranges (sec). Stars indicate P value ranges: ** = .001 to .01. Note: Tasks 2 and 3 were not timed, so data are not shown.
The primary endpoint was the general ease of use and likability of the novel 3D printed amphibious lower limb prosthesis after its first use in completing tasks representative of recreational swimming, indicated by objective outcomes such as time to complete each task and changes in vital signs. Potential ease of use and likability were measured in a survey completed by participants (see Table 1, Figure 4). The secondary endpoint was efficiency of use, as indicated by the following: (1) timed tests at self‐selected speeds for entering and exiting pool; (2) performing recreational tasks in a pool (walking, swimming); and (3) ability to tread water for 60 seconds. Descriptive statistics are provided to compare use of the novel 3D printed amphibious lower limb prosthesis and the Swim Ankle.
Table 1.
Participant survey
| Question | Percentage of participants with the indicated response | |||||
|---|---|---|---|---|---|---|
| How would you rate the weight of the FIN prosthesis? | Too heavy | Heavy | Appropriate 80% | Light 20% | Too Light | N/A |
| How would you rate the weight of the Swim Ankle prosthesis? | Too heavy 20% | Heavy 30% | Appropriate 30% | Light 10% | Too Light | N/A 10% |
| How does the weight of the FIN affect your ability to swim? | Major Hindrance | Minor Hindrance | No Effect 10% | Minor Improvement 90% | Major Improvement | N/A |
| How does the weight of the Swim Ankle affect your ability to swim? | Major Hindrance 30% | Minor Hindrance | No Effect 40% | Minor Improvement 3 0% | Major Improvement | N/A |
| Please rate your comfort while using the FIN to swim: | Very Uncomfortable 10% | Uncomfortable | Neutral | Comfortable 20% | Very Comfortable 70% | N/A |
| Please rate your comfort while using the Swim Ankle to swim: | Very Uncomfortable 10% | Uncomfortable 20% | Neutral 30% | Comfortable 20% | Very Comfortable 20% | N/A |
| Please rate your comfort while swimming with no prosthesis (only your residual limb): | Very Uncomfortable 10% | Uncomfortable 30% | Neutral 20% | Comfortable 20% | Very Comfortable 10% | N/A 10% |
| Please rate your comfort while standing in the pool using the FIN: | Very Uncomfortable | Uncomfortable | Neutral 10% | Comfortable 10% | Very Comfortable 80% | N/A |
| Please rate your comfort while standing in the pool using the Swim Ankle: | Very Uncomfortable | Uncomfortable 20% | Neutral 20% | Comfortable 40% | Very Comfortable 10% | N/A 10% |
| Please rate your comfort while standing in the pool with no prosthesis (only with your residual limb): | Very Uncomfortable 20% | Uncomfortable 30% | Neutral 30% | Comfortable 20% | Very Comfortable | N/A |
| Please rate how much energy it took to use the FIN to complete a lap in the pool: | A great deal of energy | Quite a bit of energy 10% | Some energy 50% | Very little energy 30% | No energy at all 10% | N/A |
| Please rate how much energy it took to use the Swim Ankle to complete a lap in the pool: | A great deal of energy 10% | Quite a bit of energy 40% | Some energy 20% | Very little energy 30% | No energy at all | N/A |
| Please rate how much energy it took to complete a lap in the pool with no prosthesis (only your residual limb): | A great deal of energy 40% | Quite a bit of energy 40% | Some energy 10% | Very little energy | No energy at all | N/A 10% |
| Please rate how much energy it took to use the FIN to tread water: | A great deal of energy | Quite a bit of energy | Some energy 40% | Very little energy 60% | No energy at all | N/A |
| Please rate how much energy it took to use the Swim Ankle to tread water: | A great deal of energy | Quite a bit of energy 30% | Some energy 40% | Very little energy 30% | No energy at all | N/A |
| Please rate how much energy it took to tread water with no prosthesis (only your residual limb): | A great deal of energy 30% | Quite a bit of energy 30% | Some energy 20% | Very little energy 20% | No energy at all | N/A |
| Please rate your balance coming out of the pool using the ladder with the FIN being wet: | Poor | Fair | Good 20% | Very good 20% | Excellent 60% | N/A |
| Please rate your balance coming out of the pool using the ladder with the Swim Ankle being wet: | Poor | Fair 30% | Good 30% | Very good 20% | Excellent 20% | N/A |
| Please rate your balance coming out of the pool using the ramp with the FIN being wet: | Poor | Fair | Good 20% | Very good 40% | Excellent 40% | N/A |
| Please rate your balance coming out of the pool using the ramp with the Swim Ankle being wet: | Poor | Fair 30% | Good 40% | Very good 20% | Excellent 10% | N/A |
| How would you rate your quality of swimming while using the FIN? | Poor | Fair | Good 10% | Very good 40% | Excellent 50% | N/A |
| How would you rate your quality of swimming while using the Swim Ankle? | Poor | Fair 30% | Good 30% | Very good 30% | Excellent 10% | N/A |
| How would you rate your quality of swimming with no prosthesis (only with your residual limb)? | Poor 30% | Fair 40% | Good 20% | Very good 10% | Excellent | N/A |
| Did you feel any pain while swimming with the FIN? | A great deal of pain | Quite a bit of pain | Some pain | A little pain | No pain at all 100% | N/A |
| Did you feel any pain while swimming with the Swim Ankle? | A great deal of pain | Quite a bit of pain 10% | Some pain | A little pain 10% | No pain at all 80% | N/A |
| Did you feel any pain while swimming with no prosthesis (only with your residual limb)? | A great deal of pain | Quite a bit of pain | Some pain | A little pain | No pain at all 100% | N/A |
| How would you rate your ability to transition from standing/walking to swimming with the FIN? | Very Difficult | Difficult | Neutral 10% | Easy 30% | Very easy 60% | N/A |
| How would you rate your ability to transition from standing/walking to swimming with the Swim Ankle? | Very Difficult | Difficult 30% | Neutral 20% | Easy 20% | Very easy 30% | N/A |
| How would you rate your ability to transition from swimming to standing/walking with the FIN? | Very Difficult | Difficult | Neutral 10% | Easy 30% | Very easy 60% | N/A |
| How would you rate your ability to transition from swimming to standing/walking with the Swim Ankle? | Very Difficult | Difficult 30% | Neutral 20% | Easy 30% | Very easy 20% | N/A |
| How would you rate your ability to enter and exit the pool using the FIN? | Very Difficult | Difficult | Neutral 10% | Easy 20% | Very easy 70% | N/A |
| How would you rate your ability to enter and exit the pool using the Swim Ankle (including foot position change)? | Very Difficult | Difficult 10% | Neutral 40% | Easy 40% | Very easy 10% | N/A |
| Please rank the following methods in order of your preference for entering and exiting the pool (1 = most preferred, 3 = least preferred): | FIN 100% | Ankle | No prosthesis (residual limb only) | |||
| Please rank the following methods in order of your preference for transitioning from walking to swimming and swimming to walking, in the pool (1 = most preferred, 3 = least preferred): | FIN 90% | Ankle 10% | No prosthesis (residual limb only) | |||
| Please rank the following methods in order of your preference for treading water (1 = most preferred, 3 = least preferred): | FIN 70% | Ankle 30% | No prosthesis (residual limb only) | |||
| Please rank the following methods in order of your preference for swimming one lap (1 = most preferred, 3 = least preferred): | FIN 80% | Ankle 20% | No prosthesis (residual limb only) | |||
| Overall, how satisfied are you with the FIN? | Not at all satisfied | Somewhat satisfied | Moderately satisfied 10% | Very satisfied 30% | Extremely satisfied 60% | |
| Overall, how satisfied are you with the Swim Ankle? | Not at all satisfied 20% | Somewhat satisfied 10% | Moderately satisfied 20% | Very satisfied 30% | Extremely satisfied 20% | |
Custom survey for participants was created using a Likert‐scale model. The percentage of participants who responded to each choice is shown to the right of each question. Each participant (N = 10 total) was asked to answer questions below about their experiences on the testing day using either the Swim Ankle or the novel device. For questions asked about performing activities without a prosthesis, since only Task 6 (25 m lap) was performed without a prosthesis, respondents were instructed to answer based on their typical past experiences outside of the study. N/A: not applicable.
As a way to quantify exertion, vital signs were taken using an automated blood pressure machine twice for each condition: at baseline before starting tasks and upon exiting the pool at the completion of the tasks (Figure 3). Blood pressure was within normal range for 9 of 10 participants, with one outlier due to a medication compliance issue.
Figure 3.
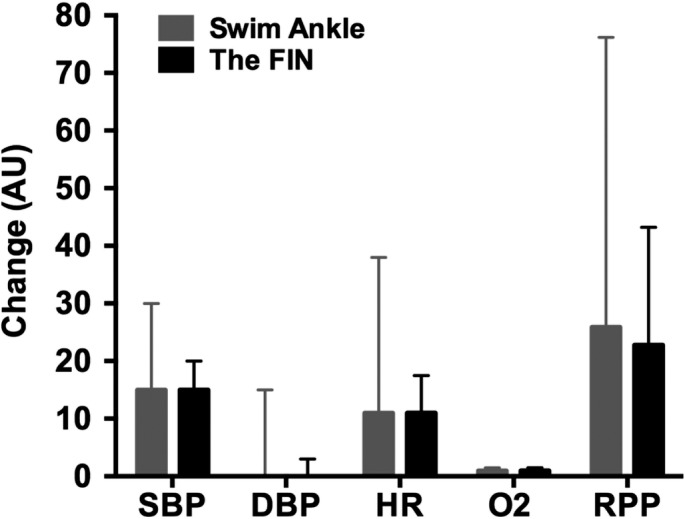
Changes in Vital Signs Before and After Each Task: SBP = systolic blood pressure; DBP = diastolic blood pressure; HR = heart rate; O2 = oxygen saturation; RPP = Rate Pressure Product, calculated as product of SBP x HR. RPP % change comparing groups. Bars show median and error bars show interquartile ranges (s). Y axis units are change in vital sign measurements. Units for each measure are indicated on the X axis. Stars indicate P value ranges: * = .01 to .05, ** = .001 to .01, *** = .0001 to .001.
Task 1 Ramp Test Into Pool
Each participant was seated on a bench placed 3 feet away from the pool and asked to enter the pool using a ramp that was 4.5 m long, anchored where the pool was 4 feet deep. Participants were asked to enter the pool via the ramp wearing either the Swim Ankle or the novel 3D printed amphibious lower limb prosthesis and were timed during this task. All participants were able to enter the pool via the ramp using either the Swim Ankle or the novel 3D printed amphibious lower limb prosthesis.
Task 2 Leisure Activities in Pool
Each participant was asked to spend 5 minutes of free time in the pool to experience the different prosthesis conditions in a setting typical of recreational pool use. Specifically, participants were asked to demonstrate their ability to complete a walk‐to‐swim‐to‐walk sequence during this time.
Task 3 Treading Water
Participants were then asked to perform the basic safety skill of treading water. After 5 minutes of leisure activities, participants were asked, if comfortable, to move one arm's length away from the pool edge and tread water for 60 seconds in an area of the pool that was 6 feet deep. A lifeguard and study team member who could swim remained within an arm's length of the participant during this task.
Task 4 Ladder Test Out
Participants were then asked to exit the pool wearing one of the prostheses using a vertical ladder fixed to the side of the pool within 3 feet of water. The time to complete this task was recorded.
Task 5 Ladder Test Into Pool
Participants were then asked to enter the pool wearing one of the prostheses using a vertical ladder fixed to the side of the pool within 3 feet of water. The time to complete this task was recorded.
Task 6 Lap Swim (25 m)
Participants were asked to swim a 25‐m lap at a self‐selected comfortable pace using a self‐selected stroke with the Swim Ankle and the novel 3D printed amphibious lower limb prosthesis. Two observers timed the lap and the average time was recorded.
Task 7 Ramp Test Out of Pool
After the lap was completed, participants were asked to exit the pool via a ramp (used in Task 1). The time to exit the pool was recorded.
Task 8 Customized Survey
After completing the functional tasks, a customized Likert‐scale survey was completed to query ease of use and likability of the different test conditions and prostheses (Table 1, Figure 4). We also recorded verbal impressions of participants or captured comments written next to survey responses.
Figure 4.
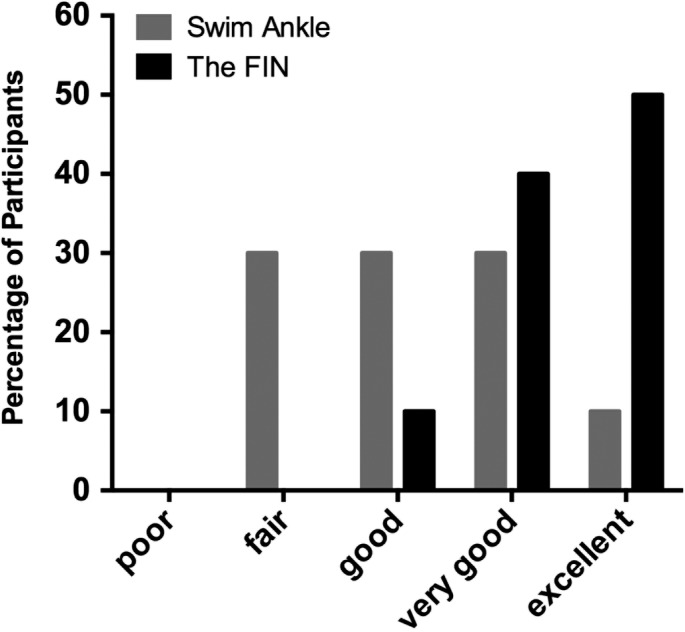
The novel 3D printed amphibious lower limb prosthesis is likeable by first‐time users: Scores from custom survey formulated using a Likert‐like scale. Bars show the possible responses to the questions: “How would you rate your quality of swimming with The FIN?” or “How would you rate your quality of swimming with the Swim Ankle?” The Y‐axis shows the percentage of participants who responded with each choice.
Data Analysis
Descriptive statistics were calculated using Prism GraphPad. Data are provided as median and interquartile range. Significant differences in the time to complete each task using either the novel 3D printed amphibious lower limb prosthesis or the standard Swim Ankle were determined using the Wilcoxon matched‐pairs signed‐rank test, with significance set at P < .05.
Participants completed the tasks on one of three testing days offered: N = 5 (day 1), N = 2 (day 2), N = 3 (day 3), where they were asked to use the novel 3D printed amphibious lower limb prosthesis for the first time. Each participant was asked to complete tasks typical of a recreational swimmer in a pool under two conditions: using the novel 3D printed amphibious lower limb prosthesis (Figure 1) or the Swim Ankle (Figure 1). Participants served as their own comparison and the choice of which prosthesis was used first was randomized to correct for potential fatigue bias. All participants were advised to complete tasks at their own pace and not to exert themselves.
A board‐certified physiatrist inspected residual limb skin integrity of participants before beginning each round of tasks and again when all tasks were completed. Skin was inspected for redness (yes/no) and skin breakdown (yes/no). If skin breakdown was noted, a description was recorded. Only one participant had a skin change, which was described as medial patellar redness; this was noted after he had completed trials with the novel 3D printed amphibious lower limb prosthesis and without a prosthesis, but before starting with the Swim Ankle.
Participants self‐identified as recreational swimmers. At all times, multiple lifeguards and physicians were present and a member of the study team who could swim was 1 foot away from the participant. Participants were instructed to stop or rest as desired at any time and to resume the activity or task when they felt comfortable to do so. Participants were asked to choose their preferred method to enter and exit the pool during the round of tasks without a prosthesis. If a participant declined to perform a task or round of tasks, then any remaining data collected from the participant were used. Namely, the tasks were not meant to be completed in a competitive manner, but rather were meant to measure comfort and ease of use. The time to complete each task was recorded as an indicator of ease of use.
Results
Basic clinical and demographic information for participants is shown in Table 1. Participants (N = 10%, 80% male) were individuals living with lower limb amputation for at least 2 years and had an average time from amputation of 14.5 ± 3.10 years (mean ± SEM). The average age of participants was 49.5 ± 4.80 (mean ± SEM), and the range was 29 to 82 years.
Baseline vital signs were obtained for all participants on the testing day and were found to be within normal range, with the exception of a single participant who reported missing his blood pressure medication. Blood pressure data for this participant were excluded from the averages presented and were judged by a board‐certified physiatrist to be within an appropriate range for the participant to engage in recreational physical activity at a comfortable pace.
Vital sign changes were not significantly different from each other with the different devices. The average change in heart rate was comparable for the Swim Ankle and the novel 3D printed amphibious lower limb prosthesis (median, IQR 11, 36 and 11, 16 beats P = .445). The average change in O2 saturation was comparable for the Swim Ankle and the novel 3D printed amphibious lower limb prosthesis (median, IQR: 1, 1.5 and 1, 2, P = .769) (Figure 3). The average percent change in rate pressure product (RPP) was 39.5% for the Swim Ankle, and 21.1% for the novel 3D printed amphibious lower limb prosthesis. The novel 3D printed amphibious lower limb prosthesis had the least change in RPP, but this change was not statistically significant (Figure 3).
Task 1 Ramp Test Into Pool
The average time to complete this task was similar when participants used the Swim Ankle or the novel 3D printed amphibious lower limb prosthesis, respectively (median, IQR: 13.6 seconds, 5.7 vs 15.0 seconds, 5.9 (median, IQR) (95% confidence interval [CI] −1.9 to 1.03; P = .530) (Figure 2).
Task 2 Leisure Activities in Pool
All participants completed leisure activities in the pool in each condition.
Task 3 Treading Water
All participants were comfortable completing the water treading test under all conditions (Figure 2).
Task 4 Ladder Test Out
All participants completed the task. The average time to exit the pool via the ladder was shorter for participants when they used the novel 3D printed amphibious lower limb prosthesis than when they used the Swim Ankle (median, IQR: 16.1, 5.5 vs 22.8, 8.6 seconds (95% CI 3.3 to 21.2; P = .008, respectively, Figure 2).
Task 5 Ladder Test Into Pool
All participants were able to enter the pool using the vertical ladder in both conditions. The average time to enter the pool via the vertical ladder was shorter for participants with the novel 3D printed amphibious lower limb prosthesis than with the Swim Ankle (median, IQR: 14.8, 6.7 vs 23.0, 17.9 seconds, 95% CI −0.57 to 23.29; P = .008, respectively, Figure 2).
Task 6 Lap Swim (25 m)
All participants completed the 25‐m lap swim. Although not statistically significant, the average swim time was comparable with either the novel 3D printed amphibious lower limb prosthesis or the Swim Ankle (43.51 ± 7.22, 40.41 ± 5.77 seconds, respectively, mean ± SEM, Figure 2). One participant did not complete the 25‐m swim (Task 6) with the Swim Ankle and one participant lost the Swim Ankle due to improper fitting with his own sleeve, which he requested to use, despite being advised against it.
Task 7 Ramp Test Out of Pool
All participants completed the ramp test. The average time to exit the pool via the ramp was significantly shorter with the novel 3D printed amphibious lower limb prosthesis as compared to the Swim Ankle: 14.24 ± 0.88 and 22.05 ± 1.32 seconds (mean ± SEM) respectively (95% CI 4.97 to 10.80, P = .004).
Task 8 Customized Survey
After completing the functional tasks, a customized Likert‐scale survey was completed to query ease of use and likability of the different test conditions and prostheses (Table 1, Figure 4). We also recorded verbal impressions of participants or captured comments written next to survey responses. Survey data demonstrated that most participants preferred the novel 3D printed amphibious lower limb prosthesis compared to the Swim Ankle in the areas of weight, comfort, energy efficiency, balance, swimming quality, overall satisfaction, and discomfort. Respondents were also instructed to answer the questions posed about performing activities without a prosthesis based on their typical past experiences outside of the study. Participants preferred the novel 3D printed amphibious lower limb prosthesis over the other conditions for entering and exiting the pool, transitioning between settings, treading water, and swimming. The complete survey and responses are shown in Table 1. An example of responses to the questions of how participants rated their quality of swimming with the novel 3D printed amphibious lower limb prosthesis or the Swim Ankle is shown in Figure 4.
Qualitative Data
Participants had positive impressions of using the novel 3D printed amphibious lower limb prosthesis. Participant A stated: “The FIN provides me with security and comfort and confidence.” Participant B stated: “The FIN is tight—it is easier to walk through the water, it is comfortable.” There were several negative comments about using the traditional fixed angle foot prosthesis. Participant C: “It was a little inconvenient to move the ankle straight for swimming and then transition to straight to swim. I can see a problem if I was at the shore of the ocean.” Participant D: “Had to take time to switch ankle before stepping on ladder.” Participant E stated: “If the lever on the Swim Ankle had a rubber coating it would make it a little user friendly.” Participant F stated that “the Swim Ankle is heavier compared to the FIN.” The two participants who did so felt that swimming without a prosthesis required additional energy. Participant G said “It's not uncomfortable; it is just very tiresome. Using a lot of my strength to push myself.” Participant H stated: “It takes more energy to swim with no prosthetic.”
Discussion
Persons with lower limb amputation encounter barriers to participation in physical activity including: difficulty arranging transportation, inaccessible fitness facilities, societal attitudes, climate, overall physical environment, and income.5, 9, 16, 17 These limitations play a role in preventing persons with lower limb amputation from participating in swimming, a physical activity likely to be recommended for this population. Currently, widely available swim prostheses are difficult or impossible to use on land for overground walking or for transitioning between land and water.
In this pilot study, participants did not exhibit a statistically significant change in heart rate or RPP when using the novel 3D printed amphibious lower limb prosthesis or Swim Ankle, with the caveat that this pilot study was not powered to detect these changes (Figure 4). Only one participant had an RPP >22 000, which may be an indicator of myocardial ischemia.18 All other rate pressure product measurements were below 22 000 before and after each activity, demonstrating that the novel 3D printed amphibious lower limb prosthesis did not cause an additional cardiac burden, with the caveat that this pilot study was not powered to detect these changes.
Time to exit the pool via ladder or ramp was significantly shorter when using the novel 3D printed amphibious lower limb prosthesis as compared to the Swim Ankle, indicating ease of use. This may be attributed to the fixed foot position of the novel 3D printed amphibious lower limb prosthesis, eliminating the need to adjust the foot position from transitioning between a walking stance and swimming, as needed with the Swim Ankle. The time to complete a 25 m lap was comparable when using the novel 3D printed amphibious lower limb prosthesis or Swim Ankle.
The weight of the novel 3D printed amphibious lower limb prosthesis is greater than that of the Swim Ankle (~795 vs 695 g, respectively). From verbal comments and written survey responses, most participants perceived that the weight of the novel 3D printed amphibious lower limb prosthesis was “appropriate” or “light” and that it allowed for “minor improvement” in the ability to swim in the pool. The responses to the questions on weight for the Swim Ankle prosthesis were more varied (Table 1). The quantity and design of the conical‐shaped holes within the build of the novel 3D printed amphibious lower limb prosthesis allows for passage of water, coordinating resistance and turbulence, while propelling an individual forward. As such, the novel 3D printed amphibious lower limb prosthesis may play a role in canceling out drag forces of the overall prosthetic. It is possible that this force cancellation/distribution along the entire length of the pylon contributed to the perception that the novel 3D printed amphibious lower limb prosthesis was lighter, as individuals may have felt forces and pressures on their residual limb in different areas and pressures when compared to the Swim Ankle.
Using a customized Likert‐scale survey, this pilot study evaluated the likability and ease of the novel 3D printed amphibious lower limb prosthesis. Participants rated the novel 3D printed amphibious lower limb prosthesis higher (more likable/usable) in each task than they did the Swim Ankle or when not using a prosthetic (this condition was not elected by most participants during the study except for the 25‐m lap swim, but participants were asked to rate their general impressions in the survey) (Figure 5). This was further affirmed by positive qualitative statements: “The FIN provides me with security and comfort and confidence.” “The FIN is tight‐ it is easier to walk through the water, it is comfortable.” Most participants subjectively felt it took “very little energy” or only “some energy” to use the novel 3D printed amphibious lower limb prosthesis to swim a lap and to tread water (Table 1).
This study has several expected limitations. This was a small, unblinded, pilot study with a sample size of convenience to assess likability and ease of use of a novel 3D printed swim prosthesis. In this initial pilot study, we did not collect information from participants on cause of amputation, use of assistive device for general mobility, or functional mobility level. Thus, the data here are intended to support the necessity of future studies that collect this and additional information in order to determine the generalizability of the results of this study. Participants were asked to use the novel 3D printed amphibious lower limb prosthesis for the first time on the day of the study and were given 5 minutes to adjust. Therefore, parameters measured and experiences may change with repeated use. Future studies could also examine the use of the novel 3D printed amphibious lower limb prosthesis beyond recreational activities to include relevant activities of daily living, such as bathing or community ambulation. A larger prospective study is necessary to make broader conclusions about use of the novel 3D printed amphibious lower limb prosthesis by individuals with lower limb amputations. Although double‐blinding in studies and trials of assistive devices is challenging, some aspects of the trial could be blinded, such as when obtaining vital signs, tabulating surveys, and collecting qualitative data.
Conclusions
Despite these limitations, this pilot study shows that the experimental device, the novel 3D printed amphibious lower limb prosthesis, was well liked and easy to use by a small number of participants in a recreational setting. This suggests that there may be advantages to using this device, a hypothesis that needs to be tested further in a larger definitive clinical trial.
Acknowledgments
The authors wish to thank Reid Oreste, Christian Arty, Anish Varghese MS, and Erica Sais for their assistance on trial days and the participants.
References
- 1. Ziegler‐Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the united states: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422‐429. [DOI] [PubMed] [Google Scholar]
- 2. Owings MF, Kozak LJ. Ambulatory and inpatient procedures in the United States, 1996. Vital Heal Stat 13. 1998;139:1‐119. [PubMed] [Google Scholar]
- 3. O'Donovan G, Blazevich AJ, Boreham C, et al. The ABC of physical activity for health: a consensus statement from the British association of sport and exercise sciences. J Sports Sci. 2010;28:573‐591. [DOI] [PubMed] [Google Scholar]
- 4. Deans S, Burns D, McGarry A, Murray K, Mutrie N. Motivations and barriers to prosthesis users participation in physical activity, exercise and sport: a review of the literature. Prosthet Orthot Int. 2012;36:260‐269. [DOI] [PubMed] [Google Scholar]
- 5. Blauwet CA, Iezzoni LI. From the paralympics to public health: increasing physical activity through legislative and policy initiatives. PM R. 2014;6:S4‐S10. [DOI] [PubMed] [Google Scholar]
- 6. Blauwet CA, Yang HY, Cruz SA, et al. Functional and environmental factors are associated with sustained participation in adaptive sports. PM R. 2017;9:668‐675. [DOI] [PubMed] [Google Scholar]
- 7. Altman B, Bernstein A. Disability and Health in the United States 2001‐2005. Hyattsville, MD: National Center for Health Statistics; 2008. [Google Scholar]
- 8. Jaarsma EA, Dekker R, Dijkstra PU, Geertzen JHB, Koopmans SA. Barriers to and facilitators of sports participation in people with visual impairments. Adapt Phys Activ Q. 2014;31:240‐264. [DOI] [PubMed] [Google Scholar]
- 9. Gallagher P, O'Donovan MA, Doyle A, Desmond D. Environmental barriers, activity limitations and participation restrictions experienced by people with major limb amputation. Prosthet Orthot Int. 2011;35:278‐284. [DOI] [PubMed] [Google Scholar]
- 10. Kars C, Hofman M, Geertzen JHB, Pepping GJ, Dekker R. Participation in sports by lower limb amputees in the Province of Drenthe, the Netherlands. Prosthet Orthot Int. 2009;33:356‐367. [DOI] [PubMed] [Google Scholar]
- 11. Kegel B, Carpenter ML, Burgess EM. Functional capabilities of lower extremity amputees. Arch Phys Med Rehabil. 1978;59(3):109‐120. [PubMed] [Google Scholar]
- 12. McAuley E, Rudolph D. Physical activity, aging, and psychological well‐being. J Aging Phys Act. 2016;3(1):67‐96. [Google Scholar]
- 13. Kegel B, Webster JC, Burgess EM. Recreational activities of lower extremity amputees: a survey. Arch Phys Med Rehabil. 1980;61(6):258‐264. [PubMed] [Google Scholar]
- 14. Highsmith MJ, Kahle JT, Lewandowski A, et al. Economic evaluations of interventions for transtibial amputees: a scoping review of comparative studies. Technol Innov. 2016;18:85‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Blough DK, Hubbard S, McFarland LV, Smith DG, Gambel JM, Reiber GE. Prosthetic cost projections for servicemembers with major limb loss from vietnam and OIF/OEF. J Rehabil Res Dev. 2010;47:387. [DOI] [PubMed] [Google Scholar]
- 16. Jaarsma EA, Dijkstra PU, Geertzen JHB, Dekker R. Barriers to and facilitators of sports participation for people with physical disabilities: a systematic review. Scand J Med Sci Sport. 2014;24:871‐881. [DOI] [PubMed] [Google Scholar]
- 17. Jaarsma EA, Geertzen JHB, de Jong R, Dijkstra PU, Dekker R. Barriers and facilitators of sports in Dutch Paralympic athletes: an explorative study. Scand J Med Sci Sport. 2014;24:830‐836. [DOI] [PubMed] [Google Scholar]
- 18. Sembulingam P, Ilango S. Rate pressure product as a determinant of physical fitness in normal young adults. IOSR J Dent Med Sci Ver II. 2015;14(4):2279‐2861. [Google Scholar]


